Abstract
Studies have shown that a large proportion of traffic accidents around the world are related to inadequate or disordered sleep. Recent surveys have linked driver fatigue to 16% to 20% of serious highway accidents in the UK, Australia, and Brazil. Fatigue as a result of sleep disorders (especially obstructive sleep apnea), excessive workload and lack of physical and mental rest, have been shown to be major contributing factors in motor vehicle accidents. A number of behavioral, physiological, and psychometric tests are being used increasingly to evaluate the impact of fatigue on driver performance. These include the oculography, polysomnography, actigraphy, the maintenance of wakefulness test, and others. Various strategies have been proposed for preventing or reducing the impact of fatigue on motor vehicle accidents. These have included: Educational programs emphasizing the importance of restorative sleep and the need for drivers to recognize the presence of fatigue symptoms, and to determine when to stop to sleep; The use of exercise to increase alertness and to promote restorative sleep; The use of substances or drugs to promote sleep or alertness (i.e. caffeine, modafinil, melatonin and others), as well as specific sleep disorders treatment; The use of CPAP therapy for reducing excessive sleepiness among drivers who have been diagnosed with obstructive sleep apnea. The evidence cited in this review justifies the call for all efforts to be undertaken that may increase awareness of inadequate sleep as a cause of traffic accidents. It is strongly recommended that, for the purpose of promoting highway safety and saving lives, all disorders that cause excessive sleepiness should be investigated and monitored.
Keywords: Alertness, fatigue, rest, sleep, traffic accident
INTRODUCTION
Sleep disorders have been linked to a number of generalized health and behavioral disorders, including reduced efficiency while operating a motor vehicle. In recent years, a number of studies have shown consistent linkages between lack of sleep, circadian rhythm disorders (CRSDs), and fatigue, on the one hand, and psychosocial problems, behavioral disorders, and motor vehicle accidents on the other. Furthermore, reduced or inadequate sleep is per se considered as a risk factor for several chronic disorders, including hypertension,[1] obesity,[2,3] type II diabetes,[4,5] coronary disorders,[6] cancer, and premature death.[7,8] A number of specific health and sleep problems have now been shown to have adverse consequences during waking hours. These problems include: (a) Sleep deprivation or chronic sleep restriction;[9,10] (b) Excessive daytime somnolence;[11,12] (c) Tiredness and/or fatigue;[13–15] (d) High body mass index (BMI);[16] (e) obstructive sleep apnea (OSA) associated with alcohol consumption;[17] and f) other sleep disorders.[16,18,19]
Globally, thousands of accidents occur due to lack of sleep, tiredness, and fatigue. An awareness of this linkage has increasingly prompted public health concerns regarding the possible role of inadequate sleep in road accidents and fatalities.[11,15,20,21] These concerns have in turn resulted in recommendations for specific preventive steps and public education. In several countries, various contributors to traffic accidents have been discussed and considered closely. In 2004 and 2010, the UN General Assembly and World Health Organization (WHO) reviewed the costs of traffic accidents, and unanimously approved a policy statement urging that in the years 2011 to 2020 increased attention be given to the issue of road safety,[22] with the aim of halting or reversing the trend of increasing accidents and deaths worldwide. Member states were invited to perform activities in the areas of road safety, infrastructure, vehicle safety, road users’ behavior, reduction of accidents, traffic education and clinical care post-crash. The recommended activities were to conform to the following five target areas of concern: 1. Road safety management; 2. Safer roads and mobility; 3. Safer vehicles; 4. Safer road users; 5. Post-crash response. The purpose of these efforts was to change public behavior concerning road safety and to influence the attitudes of government policy makers. More specifically, these activities aimed to increase local government enforcement of road laws, to involve public health sectors, to increase awareness of vehicle manufacturers and to educate local communities. Studies have shown that a large proportion of traffic accidents around the world are related to inadequate or disordered sleep, with its resulting decrease in driver alertness being associated with serious injuries and deaths. In view of the direct implications of these associations for public health and safety, the present review sought to examine them more closely. The aim of this review was hopefully to promote greater understanding of driver sleepiness and to suggest possible strategies for dealing with the problem.
The seriousness of traffic accidents for public health and safety has been pointed out by a number of surveys and governmental statistics. These have shown that a large number of injuries and deaths have been caused by automobile accidents.[23] In a worldwide survey, WHO[23] tallied the road traffic injury fatality rates (per 10.000 population) of major global regions: South-East Asia region (16,6); African region (32,2); Eastern Mediterranean region (32,2); region of the Americas (15,8); European region (13,4) and Western Pacific region (15,6). India and China have the highest traffic accident rates in the world: 105,725 and 89, 455 people died in 2006, respectively.[23] In 2008, 39,000 people in the European Union lost their lives in traffic related accidents; the European countries with the highest rates of traffic fatalities were mostly eastern countries, namely, Lithuania (14.8/100,000 inhabitants), Poland (14.3/100,000 inhabitants) and Romania (14.2/100,000).[24] In 2008, out of all deaths in Argentina, 3,988 were found to be due to traffic accidents.[25] In the US, 37,261 deaths were the result of car accidents. In a study by Seaht et al. traffic accidents in Tehran accounted for 17.3% of all accidents and mortality was 26.6 per 1000 people per year.[26] In Brazil, there were 158,893 traffic accidents in 2009, with 93,851 injuries and 7,376 deaths.[27] The Brazilian National Health System (Sistema Único de Saúde - SUS) found that, out of nine million hospital admissions, 8.1% were due to external causes, and of these external causes, 15% were due to motor vehicle accidents. Several studies have underscored the need for urgency in developing methods to prevent errors associated with traffic accidents and for designing practical tests of driver fatigue, which is the root cause of these accidents.[10,15,28] Various authors have emphasized the vital importance of directing the attention of society and governments worldwide to the issue of “sleepy driving” (falling asleep while driving) and the threat it represents to public safety. It has been concluded that the need for adequate legislation in this regard is absolutely essential.[29–31]
Fatigue, sleep disorders, excessive sleepiness and accidents
Fatigue as a result of sleep disorders, excessive workload and lack of physical and mental rest, are known to be major contributors to motor vehicle accidents. It has been estimated that in the USA 56,000 accidents a year are related to inadequate sleep.[32] In the UK, 20% of highway accidents and up to one quarter of fatal and serious accidents are known to have occurred because of driver fatigue.[20,33] In Australia, it has been shown that driver fatigue is responsible for 17% of all accidents, 30% of which resulted in deaths.[34,35] In 2010, 41% of a sample of U.S. drivers who responded to a telephone survey admitted to having “fallen asleep or nodded off” at the wheel.[36] In general, fatigue is reported by Brazilian drivers to be the cause of approximately 20% of the accidents and over 30% of the 24,000 deaths that occur annually on Brazilian highways. In 2008, the Brazilian Federal Highway Police reported that nearly 2,400 accidents had been caused by sleep problems.[37]
Souza et al. concluded that Brazilian truck drivers in Mato Grosso do Sul had increased alcohol consumption, bad sleeping habits and sleep restriction, excessive driving duration and poor quality of life; these behavioural factors were reflected in the poor scores of Epworth Sleepiness Scale (ESS) and the Pittsburgh Sleep Quality Index (PSQI) scales.[38] Both excessive daytime sleepiness and age were additionally found to correlate with traffic accidents. Silva-Junior et al. interviewed Brazilian truck drivers and found that 18.3% stated that they snored, 48.3% consumed alcohol while driving, and that 35% used stimulants, Further, the investigations found that and that these factors were involved in 34% of the reported accidents.[39]
Vakulin et al. surveyed 38 untreated individuals with OSA and found that, compared to a control group, the OSA respondents were more likely to have had at least one accident resulting from falling asleep at the wheel if they additionally experienced in combination with sleep restriction (OR = 4.0 [1.8-8.8]) or had consumed alcohol (OR = 2.3 [1.0-5.1]).[17]
Dawson et al.[40] compared the effects of blood alcohol concentration with sleep deprivation and found that 17-19 h of sleep deprivation resulted in task performance decrements that were equivalent to the effects of a 0.05% blood alcohol concentration, while further increases in sleep deprivation (20-25 h of wakefulness) were as damaging to driving performance as a blood alcohol concentration of 0.10%.[41]
Sagaspe et al. carried out telephone interviews with 4,774 French drivers and found that 11.8% of the sample had ESS scores of ≥ 11, 28.6% reported experiencing sleepiness at the wheel severe enough to require stopping, feeling sleepy during night-time (46.8%) and daytime of driving (39.4%), having a near-miss accident during the previous year (10.7%) (of which 46% of the incidents were reportedly sleep-related), and of having a driving accident (5.8%) (of which 5.2% of were sleep related).[42] The authors also found that among the factors linked to motor vehicle accidents or near-miss accidents, the ones having the strongest associations were male gender (1.22-1.87, P < 0.001), being a younger driver (1.41-2.44, P < 0.001), frequently reporting feeling sleepy (OR 1.67, 1.29-2.15, P < 0.001), having a sensitivity to caffeine, experiencing episodes of anxiety-depression (OR 1.82, 1.27-2.62, P < 0.001) and having at least one episode of severe sleepiness at the wheel in the previous year (5.20-8.12, P < 0.001). Other factors linked to an elevated risk of having a motor vehicle accident were being unmarried (0.99-1.96, P < 0.05), being in the age range of 18 to 30 (1.51-3.00, P < 0.001), being a professional driver (OR 1.52, 1.08-2.13, P < 0.05), having a sensitivity to caffeine (1.11-1.85, P < 0.01) and at least one episode of severe sleepiness at the wheel in the previous year (1.57-2.64, P < 0.001).
Komada et al. found that values of apnea hypopnea index (AHI ≥ 40) and ESS (ESS ≥ 11 and ESS ≥ 16) of 616 Japanese drivers were correlated with an increased risk of dozing off at the wheel, as well as a higher risk of being involved in motor vehicle accidents.[43]
Studies have shown that, compared to normal individuals, individuals with OSA have a higher risk of falling asleep while driving and are three times more likely to cause accidents.[16,18,44]
Shiomi et al. and George reported that, among sleep disorders, OSA represented the highest risk factor for sleepiness and accidents.[45,46] The partial or total obstruction of the upper airway that is associated with severe oxyhemoglobin desaturation is a cause of hypoxemia, hypercapnia, sleep fragmentation, ES, and cognitive impairments.[45,47] Among the impairments caused by OSA are those which involve frontal lobe executive functions, essential for decision making while driving. It has been recently demonstrated that these critical functions do not improve following CPAP treatment.[48]
In one study it was found that, compared to a group without OSA (AHI = 0 to 5), patients with OSA had a greater relative risk of having an accident (1.6 to 2.9), and a greater rate of having an accident in which there was a personal injury (3.0 to 4.8). It was found further that the increase in the risks and rates of accidents was proportional to the seriousness of sleep apnea.[49]
Vakulin et al. showed that OSA patients had performance impairments in a driving simulator when compared with the control group. The authors also reported that after three months of CPAP treatment, the OSA group had improved their driving performance.[50]
A systematic review and meta-analysis of the relationships among OSA, CPAP and accidents found that CPAP use reduced the accident risk of drivers with moderate to severe OSA (RR = 0.278, 95% CI: 0:22 to 0:35, P < 0.001), and, additionally, decreased self reported sleepiness, one of the symptoms of OSA.[16] Venelle et al. interviewed 677 drivers and found that 12% reported having OSA symptoms and having fallen asleep at the wheel, and that among these 7% were involved in accidents.[51]
Tippin et al. compared normal drivers with those who had OSA and demonstrated that the OSA group had reduced peripheral vision (80.7 ± 14.8% vs. 86.7 ± 8.8%, P = 0.03) and reported feeling greater sleepiness at the wheel (Stanford Sleep Scale = 4.2 ± 1.2 vs. 3.6 ± 1.2, P = 0.03).[52] The authors also showed that an association existed between increased sleepiness and decreased heart rate in OSA patients (r = -0.49, P = 0.01).
Philip et al. surveyed 35,004 drivers, and found that 5.2% had OSA, 2.3% had restless legs syndrome, 9.3% insomnia, 0.1% narcolepsy and hypersomnia, and 4.4% had multiple disorders.[19] Of these drivers, 7.2% reported having had at least one accident in the previous year, 5.8% of which were related to sleep. These results are reflected in related findings that the highest risk of having a motor vehicle accident was associated with narcolepsy or hypersomnia [OR = 8.78 (1.97-39.06)], OSA [OR = 2.09 (1.06-4.13)], insomnia [(OR = 1.78 (1.01-3.14)] and others multiple sleep disorders [OR = 1.46 1.20-1.78)]. Accidents caused by sleepiness occurred primarily on highways (77.6%) and on long trips (63.8%) and more frequently at night (40.9%) than during the day (29.4%).
Powell et al. found an association between sleep disorders (narcolepsy, insomnia, and OSA) and accidents caused by sleepiness, as well as an association between sleepiness and near miss accidents.[53] Donjacour et al. concluded that untreated narcolepsy can impair driving performance and increase the risk of traffic accidents.[54]
Vanlaar et al. evaluated 750 drivers and found that 14.5% reported sleepiness while driving, and, further, that 2% of the respondents had been involved in accidents caused by sleepy driving.[15]
A study conducted by Pérez-Chada et al. of 770 Argentinian truck drivers found that 80% were overweight, 71.9% snored (of those, 4.7% reported apnea), 37.8% were hypertensive, 86.9% had insomnia, 13.9% had ESS scores above 10, and 43.8% became sleepy while driving.[55] Those suffering from apnea had higher scores on the ESS, were more likely to be overweight and a higher prevalence of hypertension. In this population, snoring, ESS scores > 10, and driving for long hours were associated with sleepiness at the wheel, as well as an increased likelihood of having accidents or near misses. The risk of accidents among drivers who reported having sleep apnea was 54.3%.
Lic and Summala evaluated a sample of truck drivers from two companies in Finland. Out of the total 11% had already had at least one accident because of sleepiness while driving, 33% snored during sleep, 8% reported having respiratory disorders, and more than 50% were obese.[56]
De Pinho et al. found that out of 300 truck drivers evaluated, 46.3% experienced poor sleep quality, 46% had excessive sleepiness, and 40% were chronically sleep-deprived. Snoring was present in 18.3% of the drivers.[57] Excessive sleepiness (ES) was the cause of the majority of accidents reported by the drivers (26.5%) while the reported frequency of ES was even greater among drivers who had a history of accidents.
A number of studies of shift workers, especially professional drivers, have documented the occurrence of changes in sleep architecture over time. The associated symptoms, including poor quality of sleep, fragmentation due to OSA, and sleep deprivation and/or restriction, were thought to explain the ES, fatigue, health deficits, possible driving errors, and serious accidents.[9,13,23,58,59]
Most European countries now have specific traffic laws for sleep disorders and diseases. Several U.S. states, as well as Canada and Australia, have established laws that prohibit drivers with OSA or narcolepsy from driving a car and/or obtaining a drivers license unless their condition is medically controlled.[60] In 2007, 128,467 traffic accidents were recorded in Brazil, with 42,508 being caused by inattention and 3,367 being caused by sleepy driving. In 2008 there were 60,370 confirmed deaths due to accidents, with 36,666 deaths resulting from traffic accidents.[37,61] In Brazil, due to the high rate of traffic accidents caused by sleepiness, a resolution was adopted by Departamento Nacional de Trβnsito (DENATRAN) in 2008 (Resolution CONTRAN/DENATRAN 267/2008) to reduce the number of accidents caused by sleepiness, fatigue, sleep respiratory disorders and changes in biological rhythms.[31]
Sleep medication
Some studies have shown that individuals with insomnia and those who were taking various sleep medications had an increased risk of accidents due to fatigue symptoms, reduced alertness and sleepiness at the wheel.[62–64] Over the past 30 years, on-road driving research conducted in the Netherlands examined the effects on driving of various medicinal drugs.[65] Participants were evaluated during a 100-km driving test on a public highway. They were instructed to drive with a steady lateral position and constant speed (95 km/h). The standard deviation of lateral position (SDLP), i.e. the weaving of the car, was the primary outcome measure of the test.[66] A study of unmedicated healthy volunteers concluded that prolonged nighttime highway driving is associated with increased driver sleepiness, and that this was further associated with progressively increasing SDLP values.[29] After 2 to 3 h of driving, performance impairments are comparable to those seen in drivers who have consumed alcohol and have a blood alcohol concentration (BAC) or 0.05%, i.e. the legal limit for driving in many countries. As a result of these findings it has been recommended that drivers take regular breaks when driving. It has been shown effective if during these breaks drivers consume caffeinated beverages such as coffee or energy drinks in order to increase their alertness.[67,68]
Several driving studies have examined the residual effects of hypnotic drugs. In these studies, participants received treatment at bedtime and were tested the following morning. The results of these studies showed that benzodiazepine hypnotics and zopiclone significantly impair driving performance, whereas zolpidem and zaleplon seem relatively safe.[69–71] Ramelteon, a melatonin receptor agonist, also significantly impaired next morning driving performance.[72]
The findings of these studies are in line with epidemiological evidence showing increased accident risks among those who use benzodiazepine hypnotics and zopiclone[73] and are also generally consistent with other findings cited in this paper showing that a number of sleep disorders can reduce daytime alertness, and thus have adverse effects on driving performance.
Sleep, sleepiness and sleep disorders monitoring
The various types of evaluations and their respective instruments that are commonly used to study sleep disorders, sleepiness, and wakefulness-rest activity are listed below [Table 1]:
Table 1.
Various methods and instruments for evaluating drowsiness and daytime sleepiness
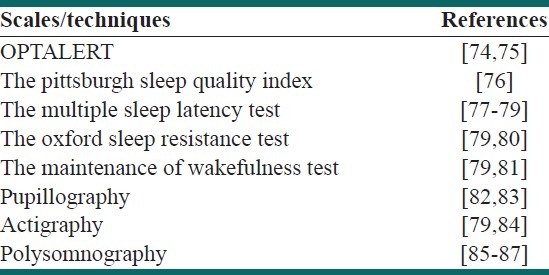
OPTALERT (System of Infrared Reflectance Oculography): This is a new method for monitoring eye and eyelid movements by infrared reflectance oculography. The method uses transducers attached to a glass frame to measure drivers’ drowsiness continuously on a new scale (Johns Drowsiness Scale-JDS) during driving task.[74,75]
The Pittsburgh sleep quality index (PSQI),[76] includes issues related to sleepiness during daily activities and daily life, sleep, and sleep disorders;
The multiple sleep latency test (MLST),[77–79] assesses the propensity to sleep in a comfortable position, a factor that is commonly used in the diagnosis of narcolepsy;
The oxford sleep resistance test (OSLER),[79,80] determines the onset of sleep;
The maintenance of wakefulness test (MWT),[79,81] assesses the individual's ability to stay awake;
Pupillography, which evaluates the diameter and variability of the pupil and the relationship of these variables to subjective sleepiness complaints;[82,83]
Actigraphy, assesses the activity-rest periods and circadian rhythm disorders of shift workers and may be used to infer hypersomnia and/or fatigue;[79,84]
Polysomnography (PSG) (the “gold standard” for diagnosing OSA) is the most commonly used test to evaluate sleep and its disorders. It includes measures based on the electroencephalogram (EEG), mentonian and lower limb electromyography (EMG), electrooculogram (EOG), electrocardiogram (ECG), pulse oximetry, oro-nasal airflow, respiratory effort measurements, blood gas, snoring, and body position. (It has been noted however that while PSG can contribute importantly to an overall assessment of sleep quality, it is not a specific instrument for assessing sleepiness).[85–87] The clinical diagnosis of OSA is made with protocols used by a physician who specializes in sleep disorders.
These survey instruments and physiological tests are very important for accurately diagnosing sleep disorders and their symptoms so that driver errors and accidents, which may affect public health, can be avoided.
Prevention and therapeutic strategies
Rodenstein summarized several studies dealing with the financial consequences of a-related accidents and concluded that the resulting cost to the public was $ 16 billion per year.[18] It has been projected that CPAP treatment could reduce these costs to $11 billion per year. Further, it has been calculated that 567,000 crashes and 980 traffic deaths could be prevented with OSA treatment by CPAP.[88] These projections underscore the urgency of the need to develop policies for preventing accidents and promoting the health of drivers who are affected by sleep disorders or other conditions that restrict sleep. The preventive or therapeutic interventions should be emphasized to minimize the deleterious effects of drowsy driving and to educate drivers about the risks of economic loss, poor quality of life and death. Figure 1 summarizes of the causes and preventing strategies of sleepiness during driving. Due to the high prevalence of OSA and sleepiness among drivers, some studies have recommended that educational activities related to drowsy driving and how OSA may be an important cause of traffic accidents be made a requirement for the licensure of professional drivers.[18,89,90]
Figure 1.
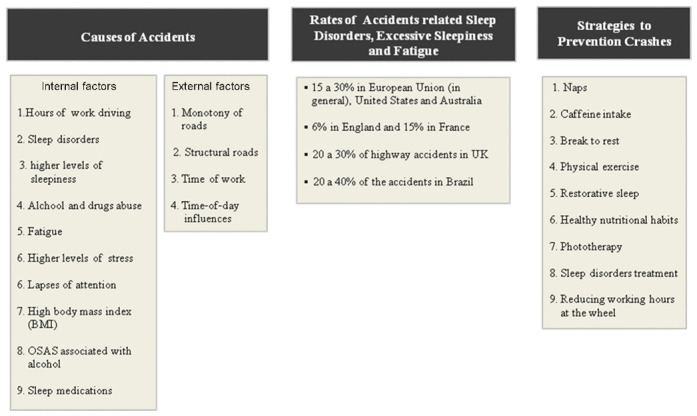
A summary of the causes and preventing strategies of sleepiness during driving
The literature highlights the importance of restorative sleep and the need for drivers to examine the external environment, to recognize the presence of fatigue symptoms, and to determine when to stop to sleep.[10,51] A number of prevention strategies have been proposed. Awareness programs based on educational lectures have now been developed. The aim of these is to promote behavioral change,[10,14,18,90] sleep hygiene strategies,[91,92] healthy nutritional habits,[93,94] exercise at certain times,[10,95,96] changes in behavior, drugs and alcohol abuse, time of driving and signs of fatigue,[10,14,15,45] stop driving to doze and scheduled naps.[97,98]
Some therapeutic interventions include phototherapy to promote alertness and vigilance, with different intensities for each individual,[86,99] substances or drugs to promote either sleepiness or alertness (i.e., caffeine, modafinil, melatonin and others), as well as specific sleep disorders treatment.[86,98]
Several studies report that naps, phototherapy and caffeine can be helpful for increasing awareness, alertness and memory consolidation.[98,100,101] Phototherapy using bright light is recommended for night shift workers with insomnia, excessive sleepiness and fatigue.[86,99] Mets et al. demonstrated that 80 mg of caffeine, comparable to a regular cup of coffee or a 250 ml can of Red Bull energy drink, reduces sleepiness and improves driver performance.[67,68] Similarly, Reyner and Horne found that 200 mg of caffeine reduced subjective sleepiness in the morning as well decreased accidents.[102] Asaoka et al. reported that Japanese non-professional drivers used naps and coffee intake as strategies for preventing sleepiness at the wheel and possible accidents.[103]
Lic and Summala reported that the most common strategy used by Argentinian drivers for avoiding sleepiness was to take a nap for 10 min (66.2%) followed by ingestion of yerba mate infusion with caffeine (53.1%).[56]
The National Sleep Foundation has recommended that for maintaining alertness and optimal driving performance that sleep be adequate to meet biological needs, should not be fragmented, that the sleep cycle should be synchronized, and that the sleeping environment should be free of disturbances.[104–107]
Another strategy reported in the scientific literature is physical exercise in the evening or during the workday to increase the alertness and vigilance of drivers who do shift work or who spend long periods of time behind the wheel. Exercise has been shown to increase alertness, reduce sleepiness and accidents by increasing body temperature, as well as to promote restorative sleep.[10,96]
The quality of sleep that an individual experiences, not only its quantity, is an important factor for enhancing ambient, physical and social functioning. Sleep that is refreshing, restorative sleep, is important for promoting homeostasis and thermoregulation, and is basic in memory consolidation and cognition, energy restoration and the cerebral energy metabolism. It is known that many individuals experience and “adequate” total sleep time (6 to 8 h) but do not have enough quality sleep due to repeated awakenings, and/or sleep disorders.[108–111]
Abe et al. reported that short duration (<6 h) of nocturnal sleep is associated with an increased risk of rear-end collisions and single-car accidents.[112]
It is known that among the numerous types of sleep disorders, excessive sleepiness is more prevalent among drivers with OSA. Thus, CPAP has been recommended as a “gold standard” therapeutic strategy for remediating OSA.[83,113,114] Yamamoto et al., Sassani et al., Barbe et al. and Komada et al. reported that OSA treatment with CPAP in particular reduces the number and risk of accidents and deaths, as well as improving mood, and reducing excessive sleepiness.[43,88,115,116]
CONCLUSIONS
This review has cited studies showing that sleep disorders such as narcolepsy, insomnia, periodic leg movement disorder, OSA, and a number of other common diseases are all associationed with excessive sleepiness, fatigue symptoms such as reduced driving skills, and cognitive deficits. These in turn have been linked to an increased risk of accidents and fatalities on the highway. Although, pharmacological treatment for insomnia is meant to improve sleep and thereby reducing daytime sleepiness, driving studies show that many sleep drugs may actually contribute to daytime sleepiness and the increased risk of accidents. The evidence summarized in this paper supports the conclusion that excessive sleepiness is a serious public health concern that directly affects the safety of all who drive motor vehicles. This evidence further supports the recommendation that all disorders which produce excessive sleepiness should be investigated and monitored so that highway accidents and associated injuries and loss of lives can be reduced.
ACKNOWLEDGEMENTS
The authors would like to thank the anonymous reviewers for their helpful and constructive comments that greatly contributed to improving the final version of the paper. They would also like to thank the Editors for their generous comments and support during the review process.
Footnotes
Source of Support: Joris Verster received research support from Takeda Pharmaceuticals and Red Bull and has acted as a scientific advisor for Takeda, Sanofi-Aventis, Transcept, Sepracor, Red Bull, Deenox, Trimbos Institute, and CBD
Conflict of Interest: S. R. Pandi-Perumal is a stockholder and the President and Chief Executive Officer of Somnogen Canada Inc., a Canadian Corporation. He declared no competing interests that might be perceived to influence the content of this article. All remaining authors declare that they have no proprietary, financial, professional, nor any other personal interest of any kind in any product or services and/or company that could be construed or considered to be a potential conflict of interest that might have influenced the views expressed in this manuscript
REFERENCES
- 1.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 2.Mullington JM, Chan JL, Van Dongen HP, Szuba MP, Samaras J, Price NJ, et al. Sleep loss reduces diurnal rhythm amplitude of leptin in healthy men. J Neuroendocrinol. 2003;15:851–4. doi: 10.1046/j.1365-2826.2003.01069.x. [DOI] [PubMed] [Google Scholar]
- 3.Aldabal L, Bahammam AS. Metabolic, endocrine, and immune consequences of sleep deprivation. Open Respir Med J. 2011;5:31–43. doi: 10.2174/1874306401105010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 5.Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: A novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol. 2005;99:2008–19. doi: 10.1152/japplphysiol.00660.2005. [DOI] [PubMed] [Google Scholar]
- 6.Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 7.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 8.Liu Y, Tanaka H Fukuoka Heart Study Group. Overtime work, insufficient sleep and risk of non-fatal acute myocardial infarction in Japanese men. Occup Environ Med. 2002;59:447–51. doi: 10.1136/oem.59.7.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howard ME, Desai AV, Grunstein RR, Hukins C, Armstrong JG, Joffe D, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 10.Pandi-Perumal SR, Verster JC, Kayumov L, Lowe AD, Santana MG, Pires ML, et al. Sleep disorders, sleepiness and traffic safety: A public health menace. Braz J Med Biol Res. 2006;39:863–71. doi: 10.1590/s0100-879x2006000700003. [DOI] [PubMed] [Google Scholar]
- 11.Philip P. Sleepiness of Occupational Driver. Ind Health. 2005;43:30–3. doi: 10.2486/indhealth.43.30. [DOI] [PubMed] [Google Scholar]
- 12.Crummy F, Cameron PA, Swann P, Kossmann T, Naughton MT. Prevalence of sleepiness in surviving drivers of motor vehicle collisions. Intern Med J. 2008;38:769–75. doi: 10.1111/j.1445-5994.2008.01629.x. [DOI] [PubMed] [Google Scholar]
- 13.Philip P, Sagaspe P, Moore N, Taillard J, Charles A, Guilleminault C, et al. Fatigue, sleep restriction and driving performance. Accid Anal Prev. 2005;37:473–8. doi: 10.1016/j.aap.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 14.Nabi H, Guéguen A, Chiron M, Lafont S, Zins M, Lagarde E. Awareness of driving while sleepy and road traffic accidents: Prospective study in GAZEL cohort. Research. BMJ. 2006;333:75. doi: 10.1136/bmj.38863.638194.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vanlaar W, Simpson H, Mayhew D, Robertson R. Fatigued and drowsy driving: A survey of attitudes, opinions and behaviors. J Safety Res. 2008;39:303–9. doi: 10.1016/j.jsr.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: Systematic review and meta-analysis. J Clin Sleep Med. 2009;5:573–81. [PMC free article] [PubMed] [Google Scholar]
- 17.Vakulin A, Baulk SD, Catcheside PG, Antic NA, van den Heuvel CJ, Dorrian J, et al. Effects of alcohol and sleep restriction on simulated driving performance in untreated patients with obstructive sleep apnea. Ann Intern Med. 2009;151:447–55. doi: 10.7326/0003-4819-151-7-200910060-00005. [DOI] [PubMed] [Google Scholar]
- 18.Rodenstein D. Sleep apnea: Traffic and occupational accidents--individual risks, socioeconomic and legal implications. Respiration. 2009;78:241–8. doi: 10.1159/000222811. [DOI] [PubMed] [Google Scholar]
- 19.Philip P, Sagaspe P, Lagarde E, Leger D, Ohayon MM, Bioulac B, et al. Sleep disorders and accidental risk in a large group of regular registered highway drivers. Sleep Med. 2010;11:973–9. doi: 10.1016/j.sleep.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 20.Horne JA, Reyner LA. Driver sleepiness. J Sleep Res. 1995;4:23–9. doi: 10.1111/j.1365-2869.1995.tb00222.x. [DOI] [PubMed] [Google Scholar]
- 21.Driver fatigue and road accidents: A literature review and position paper. ROSPA. 2001. Feb, [Last accessed on 2012 Feb 06]. Available from: http://www.rospa.com/roadsafety/info/fatigue.pdf .
- 22.World Health Organization (WHO), 2010. [Last accessed on 2012 Feb 06];Global Plan for the Decade of Action for Road Safety 2011-2020, WHO, Geneva. Available from: http://www.roadsafetyfund.org/UnDecadeOfAction/Documents/global_plan_en.pdf . [Google Scholar]
- 23.World Health Organization (WHO), 2009. [Last accessed on 2012 Feb 06];Global status report on road safety time for action, WHO, Geneva. Available from: http://www.whqlibdoc.who.int/publications/2009/9789241563840_eng.pdf . [Google Scholar]
- 24.Bundesanstalt für StraBenwesen-BASt: Federal Highway Research Institute. [Last accessed on 2012 Feb 06]. Available from: http://www.bast.de/nn_76784/EN/e-Statistik/e-Unfalldaten-Downloads/e-getoetete-gesamt-ortslage,templateId=raw,property=publicationFile.pdf/e-getoetete-gesamt-ortslage.pdf .
- 25.Dead and injured in road traffic accidents by province. Country's total. Years: 2004-8. National Institute of Statistics and Census-INDEC. [Last accessed on 2012 Feb 06]. Available from: http://www.indec.gov.ar/nuevaweb/cuadros/8/ c030603.xls .
- 26.Sehat M, Naieni KH, Asadi-Lari M, Foroushani AR, Malek-Afzali H. Socioeconomic status and incidence of traffic accidents in metropolitan tehran: A populationbased study. Int J Prev Med. 2012;3:181–90. [PMC free article] [PubMed] [Google Scholar]
- 27.Statistical Yearbook of the Federal Highway 2009: Traffic Accidents and Actions to Combat Crime. National Department of Transport Infrastructure /The Brazilian Federal Highway Police. 2009. [Last accessed on 2012 Feb 06]. Available from: http://www.dnit.gov.br/rodovias/operacoes-rodoviarias/estatisticas-de-acidentes/anuario-2009.pdf .
- 28.Smolensky MH, Di Milia L, Ohayon MM, Philip P. Sleep disorders, medical conditions, and road accident risk. Accid Anal Prev. 2011;43:533–48. doi: 10.1016/j.aap.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 29.Verster JC, Taillard J, Sagaspe P, Olivier B, Philip P. Prolonged nocturnal driving can be as dangerous as severe alcohol-impaired driving. J Sleep Res. 2011;20:585–8. doi: 10.1111/j.1365-2869.2010.00901.x. [DOI] [PubMed] [Google Scholar]
- 30.Alonderis A, Barbe F, Bonsignore M, Calverley P, De Backer W, Diefenbach K, et al. Medico-legal implications of sleep apnoea syndrome: Driving license regulations in Europe. Sleep Med. 2008;9:362–75. doi: 10.1016/j.sleep.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 31.de Mello MT, Bittencourt LR, Cunha Rde C, Esteves AM, Tufik S. Sleep and transit in Brazil: New legislation. J Clin Sleep Med. 2009;5:164–6. [PMC free article] [PubMed] [Google Scholar]
- 32.An Analysis of the Significant Decline in Motor Vehicle Traffic Fatalities in 2008. NHTSA. 2010. [Last accessed on 2012 Feb 06]. Available from: http://www-nrd.nhtsa.dot.gov/Pubs/811346.pdf . [DOI] [PubMed]
- 33.Road safety Information: Driver fatigue and road accidents. ROSPA. 2011. [Last accessed on 2012 Feb 06]. Available from: http://www.rospa.com/roadsafety/info/driver_fatigue_2011.pdf .
- 34.Heavy vehicle driver fatigue final regulatory impact statement. National Transport Comission-NTC Australia. [Last accessed on 2012 Feb 06]. Available from: http://www.ntc.gov.au/filemedia/Reports/3HVDFHVDFRISFeb2007.pdf .
- 35.Road crash facts for South Australia. Government of South Australia/Department for transport, energy and Infrastructure. [Last accessed on 2012 Feb 06]. Available from: http://www.transport.sa.gov.au/pdfs/safety/road_crash/Crash_Facts.pdf .
- 36.Tefft B. AAA Foundation for Traffic Safety. Washington, D.C: 2010. Asleep at the Wheel: The Prevalence and Impact of Drowsy Driving. [Google Scholar]
- 37.Statistics Operations. [Last accessed on 2012 Feb 06];The Brazilian Federal Highway Police. Available from: http:// www.dprf.gov.br/PortalInternet/estatistica.faces . [Google Scholar]
- 38.Souza JC, Paiva T, Reimao R. Sleep habits, sleepiness and accidents among truck drivers. Arq Neuropsiquiatr. 2005;63:925–30. doi: 10.1590/s0004-282x2005000600004. [DOI] [PubMed] [Google Scholar]
- 39.da Silva-Junior FP, de Pinho RS, de Mello MT, de Bruin VM, de Bruin PF. Risk factors for depression in truck drivers. Soc Psychiat Psychiat Epidem. 2009;44:125–9. doi: 10.1007/s00127-008-0412-3. [DOI] [PubMed] [Google Scholar]
- 40.Dawson D, Reid K. Fatigue, alcohol and performance impairment. Nature. 1997;388:235–7. doi: 10.1038/40775. [DOI] [PubMed] [Google Scholar]
- 41.Williamson AM, Feyer AM. Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med. 2000;57:649–55. doi: 10.1136/oem.57.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sagaspe P, Taillard J, Bayon V, Lagarde E, Moore N, Boussuge J, et al. Sleepiness, near-misses and driving accidents among a representative population of French drivers. J Sleep Res. 2010;19:578–84. doi: 10.1111/j.1365-2869.2009.00818.x. [DOI] [PubMed] [Google Scholar]
- 43.Komada Y, Nishida Y, Namba K, Abe T, Tsuiki S, Inoue Y. Elevated risk of motor vehicle accident for male drivers with obstructive sleep apnea syndrome in the Tokyo metropolitan area. Tohoku J Exp Med. 2009;219:11–6. doi: 10.1620/tjem.219.11. [DOI] [PubMed] [Google Scholar]
- 44.Amra B, Dorali R, Mortazavi S, Golshan M, Farajzadegan Z, Fietze I, et al. Sleep apnea symptoms and accident risk factors in Persian commercial vehicle drivers. Sleep Breath. 2012:187–91. doi: 10.1007/s11325-010-0473-x. [DOI] [PubMed] [Google Scholar]
- 45.George CF. Sleep apnea, alertness, and motor vehicle crashes. Am J Respir Crit Care Med. 2007;176:954–6. doi: 10.1164/rccm.200605-629PP. [DOI] [PubMed] [Google Scholar]
- 46.Shiomi T, Arita AT, Sasanabe R, Banno K, Yamakawa H, Hasegawa R, et al. Falling asleep while driving and automobile accidents among patients with obstructive sleep apnea-hypopnea syndrome. Psychiatry Clin Neurosci. 2002;56:333–4. doi: 10.1046/j.1440-1819.2002.01004.x. [DOI] [PubMed] [Google Scholar]
- 47.Hack M. Obstructive sleep apnoea: Accidents waiting to happen. [Last accessed on 2012 Feb 06];Airways J. 2004 2:37–8. Available from: http://www.welshsas.org/documents/AJ_Mar_37-38.pdf . [Google Scholar]
- 48.Prilipko O, Huynh N, Schwartz S, Tantrakul V, Kim JH, Peralta AR, et al. Task positive and default mode networks during a parametric working memory task in obstructive sleep apnea patients and healthy controls. Sleep. 2011;34:293–301A. doi: 10.1093/sleep/34.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mulgrew AT, Nasvadi G, Butt A, Cheema R, Fox N, Fleetham JA, et al. Risk and severity of motor vehicle crashes in patients with obstructive sleep apnoea/hypopnoea. Thorax. 2008;63:536–41. doi: 10.1136/thx.2007.085464. [DOI] [PubMed] [Google Scholar]
- 50.Vakulin A, Baulk SD, Catcheside PG, Antic NA, van den Heuvel CJ, Dorrian J, et al. Driving simulator performance remains impaired in patients with severe OSA after CPAP treatment. J Clin Sleep Med. 2011;7:246–53. doi: 10.5664/JCSM.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vennelle M, Engleman HM, Douglas NJ. Sleepiness and sleep-related accidents in commercial bus drivers. Sleep Breath. 2010;14:39–42. doi: 10.1007/s11325-009-0277-z. [DOI] [PubMed] [Google Scholar]
- 52.Tippin J, Sparks J, Rizzo M. Visual vigilance in drivers with obstructive sleep apnea. J Psychosom Res. 2009;67:143–51. doi: 10.1016/j.jpsychores.2009.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Powell NB, Schechtman KB, Riley RW, Guilleminault C, Chiang RP, Weaver EM. Sleepy driver near-misses may predict accident risks. Sleep. 2007;30:331–42. doi: 10.1093/sleep/30.3.331. [DOI] [PubMed] [Google Scholar]
- 54.Donjacour CE, Mets AJ, Verster JC. Driving and Traffic Safety. In: Goswami M, Pandi-Perumal SR, Thorpy MJ, editors. Narcolepsy: A Clinical guide. New York, USA: Springer Science; 2010. [Last accessed on 2012 Feb 06]. http://link.springer.com/chapter/10.1007/978-1-4419-0854-4_19 . [Google Scholar]
- 55.Pérez-Chada D, Videla AJ, O’Flaherty ME, Palermo P, Meoni J, Sarchi MI, et al. Sleep habits and accident risk among truck drivers: A cross-sectional study in Argentina. Sleep. 2005;28:1103–8. doi: 10.1093/sleep/28.9.1103. [DOI] [PubMed] [Google Scholar]
- 56.Hakkanen H, Summala H. Sleepiness at Work Among Commercial Truck Drivers. Sleep. 2000;23:49–57. [PubMed] [Google Scholar]
- 57.de Pinho RS, da Silva-Junior FP, Bastos JP, Maia WS, de Mello MT, de Bruin VM, et al. Hypersomnolence and accidents in truck drivers: A cross-sectional study. Chronobiol Int. 2006;23:963–71. doi: 10.1080/07420520600920759. [DOI] [PubMed] [Google Scholar]
- 58.de Mello MT, Esteves AM, Pires ML, Santos DC, Bittencourt LR, Silva RS, et al. Relationship between Brazilian airline pilot errors and time of day. Braz J Med Biol Res. 2008;41:1129–31. doi: 10.1590/s0100-879x2008001200014. [DOI] [PubMed] [Google Scholar]
- 59.Aguiar M, Valenca J, Felizardo M, Caeiro F, Moreira S, Staats R, et al. Obstructive sleep apnoea syndrome as a cause of road traffic accidents. Rev Port Pneumol. 2009;15:419–31. [PubMed] [Google Scholar]
- 60.Krieger J. Sleep apnoea and driving: How can this be dealt with? Eur Respir Rev. 2007;16:189–95. [Google Scholar]
- 61.The Brazilian Health Surveillance Secretariat/Ministry of Health of Brazil. [Last accessed on 2008]. Available from: http://www.datasus.gov.br .
- 62.Leger D, Massuel MA, Metlaine A SISYPHE Study Group. Professional correlates of insomnia. Sleep. 2006;29:171–8. [PubMed] [Google Scholar]
- 63.Daley M, Morin CM, LeBlanc M, Gregoire JP, Savard J, Baillargeon L. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10:427–38. doi: 10.1016/j.sleep.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 64.Williamson A, Lombardi DA, Folkard S, Stutts J, Courtney TK, Connor JL. The link between fatigue and safety. Accid Anal Prev. 2011;43:498–515. doi: 10.1016/j.aap.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 65.Verster JC, Roth T. The prevalence and nature of stopped on-the-road driving tests and the relationship with objective performance impairment. Accid Anal Prev. 2012;45:498–506. doi: 10.1016/j.aap.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 66.Verster JC, Roth T. Standard operation procedures for conducting the on-the-road driving test, and measurement of the standard deviation of lateral position (SDLP) Int J Gen Med. 2011;4:359–71. doi: 10.2147/IJGM.S19639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mets MA, Ketzer S, Blom C, van Gerven MH, van Willigenburg GM, Olivier B, et al. Positive effects of Red Bull (R) Energy Drink on driving performance during prolonged driving. Psychopharmacology (Berl) 2011;214:737–45. doi: 10.1007/s00213-010-2078-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mets M, Baas D, van Boven I, Olivier B, Verster J. Effects of coffee on driving performance during prolonged simulated highway driving. Psychopharmacology (Berl) 2012;222:337–42. doi: 10.1007/s00213-012-2647-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Verster JC, Veldhuijzen DS, Volkerts ER. Residual effects of sleep medication on driving ability. Sleep Med Rev. 2004;8:309–25. doi: 10.1016/j.smrv.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 70.Verster JC, Veldhuijzen DS, Patat A, Olivier B, Volkerts ER. Hypnotics and driving safety: Meta-analyses of randomized controlled trials applying the on-the-road driving test. Curr Drug Saf. 2006;1:63–71. doi: 10.2174/157488606775252674. [DOI] [PubMed] [Google Scholar]
- 71.Verster JC, Spence DW, Shahid A, Pandi-Perumal SR, Roth T. Zopiclone as positive control in studies examining the residual effects of hypnotic drugs on driving ability. Curr Drug Saf. 2011;6:209–18. doi: 10.2174/157488611798280933. [DOI] [PubMed] [Google Scholar]
- 72.Mets MA, de Vries JM, de Senerpont Domis LM, Volkerts ER, Olivier B, Verster JC. Next-day effects of ramelteon (8 mg), zopiclone (7.5 mg), and placebo on highway driving performance, memory functioning, psychomotor performance, and mood in healthy adult subjects. Sleep. 2011;34:1327–34. doi: 10.5665/SLEEP.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barbone F, McMahon AD, Davey PG, Morris AD, Reid IC, McDevitt DG, et al. Association of road-traffic accidents with benzodiazepine use. Lancet. 1998;352:1331–6. doi: 10.1016/s0140-6736(98)04087-2. [DOI] [PubMed] [Google Scholar]
- 74.Johns M, Tucker A, Chapman R, Crowley K, Michael N. Monitoring eye and eyelid movements by infrared reflectance oculography to measure drowsiness in drivers. [Last accessed on 2012 Feb 06];Somnologie. 2007 11:234–42. The manuscript is Available from: http://www.mwjohns.com/wp-content/uploads/2009/murray_papers/johns_et_al_2007_monitoring_eye_and_eyelid_movements_by_ir_reflectance_oculography_to_measure_drowsiness_in_drivers.pdf . [Google Scholar]
- 75.Johns M, Chapman R, Crowley K, Tucker A. A new method for assessing the risks of drowsiness while driving ;12:66-74. [Last accessed on 2012 Feb 06];Somnologie. 2008 12:66–14. The manuscript is Available from: http://www.mwjohns.com/wp-content/uploads/2009/murray_papers/johns_et_al_2008_a_new_method_for_assessing_the_risks_of_drowsiness_while_driving.pdf . [Google Scholar]
- 76.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 77.Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): A standard measure of sleepiness. Sleep. 1986;9:519–24. doi: 10.1093/sleep/9.4.519. [DOI] [PubMed] [Google Scholar]
- 78.Zwyghuizen-Doorenbos A, Roehrs T, Schaefer M, Roth T. Test-retest reliability of the MSLT. Sleep. 1988;11:562–5. doi: 10.1093/sleep/11.6.562. [DOI] [PubMed] [Google Scholar]
- 79.Mathis J, Hess CW. Sleepiness and vigilance tests. Swiss Med Wkly. 2009;139:214–9. doi: 10.4414/smw.2009.12498. [DOI] [PubMed] [Google Scholar]
- 80.Bennett LS, Stradling JR, Davies RJ. A behavioural test to assess daytime sleepiness in obstructive sleep apnoea. J Sleep Res. 1997;6:142–5. doi: 10.1046/j.1365-2869.1997.00039.x. [DOI] [PubMed] [Google Scholar]
- 81.Mitler MM, Gujavarty KS, Browman CP. Maintenance of wakefulness test: A polysomnographic technique for evaluation treatment efficacy in patients with excessive somnolence. Electroencephalogr Clin Neurophysiol. 1982;53:658–61. doi: 10.1016/0013-4694(82)90142-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wilhelm B, Giedke H, Ludtke H, Bittner E, Hofmann A, Wilhelm H. Daytime variations in central nervous system activation measured by a pupillographic sleepiness test. J Sleep Res. 2001;10:1–7. doi: 10.1046/j.1365-2869.2001.00239.x. [DOI] [PubMed] [Google Scholar]
- 83.Balkin TJ, Bliese PD, Belenky G, Sing H, Thorne DR, Thomas M, et al. Comparative utility of instruments for monitoring sleepiness-related performance decrements in the operational environment. J Sleep Res. 2004;13:219–27. doi: 10.1111/j.1365-2869.2004.00407.x. [DOI] [PubMed] [Google Scholar]
- 84.Sack RL, Auckley D, Auger RR, Carskadon MA, Wright KP, Jr, Vitiello MV, et al. Circadian rhythm sleep disorders: Part I, basic principles, shift work and jet lag disorders. An American academy of sleep medicine review. Sleep. 2007;30:1460–83. doi: 10.1093/sleep/30.11.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Iber C, Ancoli-Israel S, Chesson A, Jr, Quan S, Thomas M. The AASM manual for the scoring of sleep and associated events: Rules, terminology and technical specifications. Westchester: American Academy of Sleep Medicine; 2007. pp. 2–59. [Google Scholar]
- 86.Morgenthaler TI, Lee-Chiong T, Alessi C, Friedman L, Aurora RN, Boehlecke B, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American academy of sleep medicine. Report Standards Of Practice Committee Of The AASM. Sleep. 2007;30:1445–59. doi: 10.1093/sleep/30.11.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sack RL, Auckley D, Auger RR, Carskadon MA, Wright KP, Jr, Vitiello MV, et al. Circadian rhythm sleep disorders: Part II, advanced sleep phase disorder, delayed sleep phase disorder, free-running disorder, and irregular sleep-wake rhythm. An American Academy of Sleep Medicine review. Sleep. 2007;30:1484–501. doi: 10.1093/sleep/30.11.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27:453–8. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- 89.Hartenbaum N, Collop N, Rosen IM, Phillips B, George CF, Rowley JA, et al. Sleep apnea and commercial motor vehicle operators: Statement from the joint task force of the American college of chest physicians, the American college of occupational and environmental medicine, and the national sleep foundation. Chest. 2006;130:902–5. doi: 10.1378/chest.130.3.902. [DOI] [PubMed] [Google Scholar]
- 90.Rodenstein D Cost-B26 Action on Sleep Apnoea Syndrome. Driving in Europe: The need of a common policy for drivers with obstructive sleep apnoea syndrome. J Sleep Res. 2008;17:281–4. doi: 10.1111/j.1365-2869.2008.00669.x. [DOI] [PubMed] [Google Scholar]
- 91.Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. 2003;7:215–25. doi: 10.1053/smrv.2001.0246. [DOI] [PubMed] [Google Scholar]
- 92.Tufik S. I Consenso Brasileiro de Insônia 2003;3-45. [Last accessed on 2012 Feb 06];Hypnos. 2003 :3–45. Available from: http://www.ic.unicamp.br/~wainer/cursos/2s2008/ia/pdf_consenso.pdf . [Google Scholar]
- 93.Crispim CA, Zalcman I, Dattilo M, Padilha HG, Edwards B, Waterhouse J, et al. The influence of sleep and sleep loss upon food intake and metabolism. Nutr Res Rev. 2007;20:195–212. doi: 10.1017/S0954422407810651. [DOI] [PubMed] [Google Scholar]
- 94.Crispim C, Zalcman I, Dattilo M, Padilha H, Tufik S, Mello M. Shift work and nutritional aspects. [Last accessed on 2012 Feb 06];Nutrire. 2009 34:213–27. Available from: http://www.files.bvs.br/upload/S/1519-8928/2009/v34n2/a213-227.pdf . [Google Scholar]
- 95.Youngstedt SD. Effects of exercise on sleep. Clin Sports Med. 2005;24:355–65. doi: 10.1016/j.csm.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 96.Antunes H, Andersen M, Tufik S, Mello M. Privação de Sono e Exercício Físico. [Last accessed on 2012 Feb 06];Rev Bras Med Esporte. 2008 14:51–6. Available from: http://www.scielo.br/pdf/rbme/v14n1/a10v14n1.pdf . [Google Scholar]
- 97.Takahashi M. The role of prescribed napping in sleep medicine. Sleep Med Rev. 2003;7:227–35. doi: 10.1053/smrv.2002.0241. [DOI] [PubMed] [Google Scholar]
- 98.Sagaspe P, Taillard J, Chaumet G, Moore N, Bioulac B, Philip P. Aging and nocturnal driving: Better with coffee or a nap. A randomized study? Sleep. 2007;30:1808–13. doi: 10.1093/sleep/30.12.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gooley JJ. Treatment of circadian rhythm sleep disorders with light. Ann Acad Med. 2008;37:669–76. [PubMed] [Google Scholar]
- 100.Purnell MT, Feyer AM, Herbison GP. The impact of a nap opportunity during the night shift on the performance and alertness of 12-h shift workers. J Sleep Res. 2002;11:219–27. doi: 10.1046/j.1365-2869.2002.00309.x. [DOI] [PubMed] [Google Scholar]
- 101.Lahl O, Wispel C, Willigens B, Pietrowsky R. An ultra short episode of sleep is sufficient to promote declarative memory performance. J Sleep Res. 2008;17:3–10. doi: 10.1111/j.1365-2869.2008.00622.x. [DOI] [PubMed] [Google Scholar]
- 102.Reyner LA, Horne JA. Early morning driver sleepiness: Effectiveness of 200 mg caffeine. Psychophysiology. 2000;37:251–6. [PubMed] [Google Scholar]
- 103.Asaoka S, Abe T, Komada Y, Inoue Y. The factors associated with preferences for napping and drinking coffee as countermeasures for sleepiness at the wheel among Japanese drivers. Sleep Med. 2012;13:354–61. doi: 10.1016/j.sleep.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 104.National Sleep Foundation (NSF) Sleep Studies. [Last accessed on 2012 Feb 06]. Available from: http://www.sleepfoundation.org/article/sleep-topics/sleep-studies .
- 105.NSF. Fatigue and Excessive Sleepiness. [Last accessed on 2012 Feb 06]. Available from: http://www.sleepfoundation.org/article/sleep-related-problems/excessive-sleepiness-and-sleep .
- 106.NSF. Sleep Drive and Your Body Clock. [Last accessed on 2012 Feb 06]. Available from: http://www.sleepfoundation.org/article/sleep-topics/sleep-drive-and-your-body-clock .
- 107.NSF. Let Sleep Work for You. [Last accessed on 2012 Feb 06]. Available from: http://www.sleepfoundation.org/article/hot-topics/let-sleep-work-you .
- 108.Rial RV, Nicolau MC, Gamundi A, Akaarir M, Aparicio S, Garau C, et al. The trivial function of sleep. Sleep Med Rev. 2007;11:311–25. doi: 10.1016/j.smrv.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 109.Davies KA, Macfarlane GJ, Nicholl BI, Dickens C, Morriss R, Ray D, et al. Restorative sleep predicts the resolution of chronic widespread pain: Results from the EPIFUND study. Rheumatology (Oxford) 2008;47:1809–13. doi: 10.1093/rheumatology/ken389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Samuels C. Sleep, recovery, and performance: The new frontier in high-performance athletics. Phys Med Rehabil Clin N Am. 2009;20:149–59. doi: 10.1016/j.pmr.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 111.Oluwole OS. Sleep habits in Nigerian undergraduates. Acta Neurol Scand. 2010;121:1–6. doi: 10.1111/j.1600-0404.2009.01171.x. [DOI] [PubMed] [Google Scholar]
- 112.Abe T, Komada Y, Nishida Y, Hayashida K, Inoue Y. Short sleep duration and long spells of driving are associated with the occurrence of Japanese drivers’ rear-end collisions and single-car accidents. J Sleep Res. 2010;19:310–6. doi: 10.1111/j.1365-2869.2009.00806.x. [DOI] [PubMed] [Google Scholar]
- 113.Holmdahl C, Schollin IL, Alton M, Nilsson K. CPAP treatment in obstructive sleep apnoea: A randomised, controlled trial of follow-up with a focus on patient satisfaction. Sleep Med. 2009;10:869–74. doi: 10.1016/j.sleep.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 114.McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, et al. Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: A systematic review and economic analysis. Health Technol Assess. 2009;13:1–119. doi: 10.3310/hta13040. [DOI] [PubMed] [Google Scholar]
- 115.Yamamoto H, Akashiba T, Kosaka N, Ito D, Horie T. Long-term effects nasal continuous positive airway pressure on daytime sleepiness, mood and traffic accidents in patients with obstructive sleep apnoea. Respir Med. 2000;94:87–90. doi: 10.1053/rmed.1999.0698. [DOI] [PubMed] [Google Scholar]
- 116.Barbé F, Sunyer J, De La Peña A, Pericas J, Mayoralas LR, Antó JM, et al. Effect of Continuous Positive Airway Pressure on the Risk of Road Accidents in Sleep Apnea Patients. Respiration. 2007;74:44–9. doi: 10.1159/000094237. [DOI] [PubMed] [Google Scholar]


