Abstract
Background:
Obstructive sleep apnea (OSA) is a common but usually under-diagnosed sleep disorder. Objective diagnosis is based on polysomnography, which is an expensive test. We assessed the reliability and diagnostic accuracy of the Berlin questionnaire (BQ) in diagnosis of OSA in Iranian sleep clinic patients.
Methods:
A cross-sectional linguistic validation study was conducted on consecutive Iranian patients with Persian language attending one sleep clinic in Isfahan (Iran) were studied. Patients completed the Persian BQ (contains 10 questions in 3 categories), developed by forward-backward translation method. The patients underwent an overnight polysomnographic study at the clinic. Apneas/hypopnea index of >5/Hour was considered for diagnosis of OSA.
Results:
One hundred and fifty seven patients (55.4% male, mean age = 52.3 ± 13.6 years) were evaluated. Sleep study confirmed OSA diagnosis in 91.7% of the studied patients. The reliability analysis of the BQ categories showed alpha Cronbach's as 0.70 and 0.50 for category 1 and category 2, respectively. BQ categories 1-3 were positive respectively in 88.5%, 67.5%, and 66.9% of the patients. The BQ and sleep study were in agreement for 82.1% of the cases. The sensitivity, specificity, positive and negative predictive values, and positive, and negative likelihood ratio of the BQ were calculated as 84.0%, 61.5%, 96.0%, 25.8%, 2.18%, and 0.26% respectively.
Conclusions:
BQ is useful as a screening test for diagnosing OSA in Iranian patients with sleep complaints; however, the test cannot be used for rolling out the OSA. Further studies on editing, modifying, and applying the BQ in a larger sample of patients are warranted in our society.
Keywords: Apnea hypopnea index, Berlin questionnaire, obstructive sleep apnea, Persian version of Berlin questionnaire, reliability and validity
INTRODUCTION
Obstructive sleep apnea (OSA) is a common sleep disorder with the prevalence of about 5% in Iranian population.[1] It is well known as an independent risk-factor for serious cardiovascular related diseases, including systemic hypertension, coronary artery disease, stroke, and pulmonary hypertension.[2–7] Moreover, it has economic impacts on societies by increasing the daytime sleepiness, leading to car accidents and work disability.[2,8]
Diagnosis of OSA is complex, and it is under-diagnosed most of the times, especially by primary care physicians who regularly visit the patients;[9] about 75% of even severe OSA patients are diagnosed.[10] Therefore, a sensitive and inexpensive test is required to diagnose OSA. Currently, polysomnography is the gold standard tool for diagnosis of OSA; however, because of its expensiveness and the limitations of its access it cannot be used regularly as the screening test.[11] Recently, a systematic review compared different instruments’ accuracies and showed the Wisconsin and the Berlin questionnaire (BQ) to have the highest sensitivity and specificity, respectively.[11] The BQ is an instrument, which can indicate the presence of sleep apnea by addressing the presence and frequency of snoring behavior, wake time sleepiness or fatigue, and history of obesity or hypertension.[12] The questionnaire has demonstrated the Cronbach's correlations of 0.86-0.92 with sensitivity of 86%, specificity of 77%, positive predictive value (PPV) of 89%, negative predictive value (NPV) of 72%, and a likelihood ratio of 3.79.[12]
With more than 400 citations, BQ is one of the most applied instruments for screening patients for OSA and is translated and validated in different populations.[13] To the best of our knowledge, there is no report to evaluate the validity and reliability of the Persian version of the BQ. Therefore, the aim of this study was to assess the reliability and diagnostic accuracy of the Persian version of the BQ in diagnosis of OSA in Iranian sleep clinic patients.
METHODS
Translation process
At first, the translation and back translation of the original version of the Berlin sleep questionnaire were conducted. Back translation was reviewed by two pulmonologist in order to achieve a modified version of the original copy. Then one translator and one researcher checked and agreed upon the provided version of the Berlin sleep questionnaire as a representative of the original version in terms of wording and content.
Patients and settings
A cross-sectional linguistic validation study was conducted on consecutive Iranian patients with Persian language attending the Bamdad Sleep Clinic in Isfahan (Iran) during the period, from September 2010 through October 2011. Patients with history of chronic anxiolytic/sedative drug use, those with renal, hepatic, cardiovascular or associated respiratory diseases, or upper respiratory tract infections within the past 4 weeks, as well as those who were critically ill or pregnant were excluded from the study. The study was approved by the ethics committee of the Isfahan University of Medical Sciences, and all patients signed an inform consent before entering the study.
The polysomnographic study was scored according to the American Academy of Sleep Medicine guideline. Apneas/hypopnea was scored when the baseline amplitude of respiration reduced 50% or more, or oxygen saturation reduces for at least 3%, either lasting for a minimum of 10 s. An apneas/hypopnea index (AHI) of >5 was considered for diagnosis of OSA and respiratory disturbance index (RDI) ≥15 indicating sleep-disordered breathing (SDB).[14]
Data collection
Data on demographic characteristics, (including age and gender) and weight and height were collected from patients’ documents files. Patients completed the BQ, which contains 10questions in 3 categories; 1st category includes five items on snoring, 2nd category includes three items on daytime somnolence, and the 3rd category includes two items on the history of hypertension and/or body mass index (BMI) >30 kg/m2. Illiterate and low-educated patients filled out the questionnaire with the assistance of an investigator. Having high-risk sleep apnea was considered if scores were positive on two or more of the three categories and those who identified as low-risk of having sleep apnea had positive scores on less than two categories. Pilot study was performed on 10 patients to examine the clearance of the questionnaire.
The patients underwent an overnight polysomnographic study at the clinic. All the patients had more than 90% effective sleep.
Statistical analysis
Data were analyzed using the SPSS software for windows version 16.0. Reliability of the Persian BQ was assessed with Cronbach's alpha of each category. Predictive parameters of the BQ, and its categories, (including sensitivity, specificity, PPV, and NPV were calculated by considering AHI > 5 as the gold standard.
RESULTS
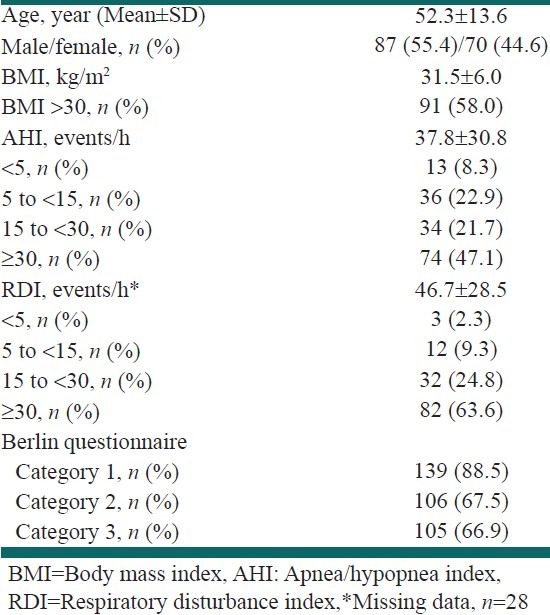
One hundred and fifty seven patients (55.4% male) with ages between 16 years and 89 years (52.3 ± 13.6 years) were evaluated in the sleep clinic during the study. Studied population characteristics are presented in Table 1. Sleep study confirmed OSA diagnosis in 91.7% of the studied patients. RDI was available for 129 patients in whom 88.3% had RDI ≥ 15 indicating SDB. BQ categories 1-3 were positive respectively in 88.5%, 67.5%, and 66.9% of the patients.
Table 1.
General population characteristics
BQ performance
The reliability analysis of the BQ categories showed alpha Cronbach's as 0.70 and 0.50 for category 1 and category 2, respectively. Descriptive scale analysis of the 2nd category showed that item 9 has an item-total correlation of 0.213 and increased the alpha to 0.552 if item deleted
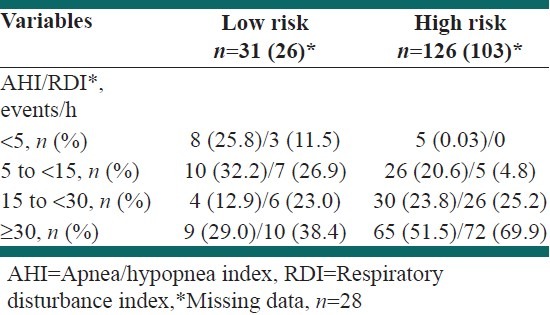
The BQ and AHI were in agreement for 82.1% of the cases. The BQ identified 80.3% (n = 126) of the patients as being in the high-risk group for OSA. In subjects with a high-risk score, OSA diagnosis was confirmed by sleep study in 96.0% (PPV, n = 121). Mild, moderate, and severe OSA based on sleep study was present in 20.6%, 23.8%, and 51.5% of the patients in the high-risk group based on BQ. Of the subjects in the low-risk group, 32.2%, 12.9%, and 29.0% had mild, moderate, and severe OSA, followed by those 25.8% (n = 8), in whom OSA was excluded by sleep study NPV. Data regarding BQ in comparison with RDI are also provided [Table 2].
Table 2.
Relationship between Berlin questionnaire score and Apnea/hypopnea index
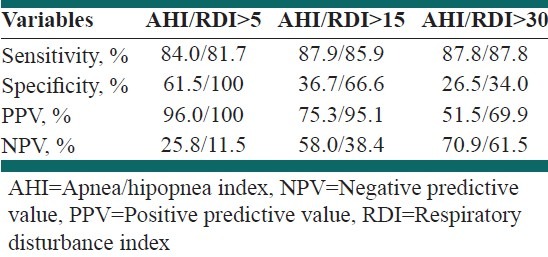
The sensitivity and the specificity of the whole BQ for OSA diagnosis with AHI > 5 were 84.0% and 61.5%, respectively with PPV of 96.0%, NPV of 25.8%, positive likelihood ratio of 2.18 and negative likelihood ratio of 0.26. Considering RDI > 5 as the standard, the sensitivity and the specificity of the whole BQ were 81.7% and 100%, respectively [Table 3]. The BQ sensitivity and specificity were respectively as 82.1% and 100% in men and 86.6% and 50% in women. For category 1, the sensitivity and specificity were 91.6% and 46.1%, and for category 2 they were 68.0% and 38.4%, respectively. In 67.5% of the cases, the two categories were in agreement
Table 3.
Predictive parameters of the Berlin questionnaire
DISCUSSIONS
Our study was aimed to evaluate the validity and reliability of the Persian version of the BQ in Iranian patients attending to sleep on clinic. The questionnaire reliability was appropriate for the first category (Cronbach's alpha, 0.70), but was not appropriate for the second category (Cronbach's alpha, 0.50). It might be due to (1) translation and scoring errors and/or (2) the ninth item, (which is about nodding off or falling asleep while driving a vehicle), as far as the old population admitted to the sleep clinic did not drive regularly, and thus, this question was not appropriate to evaluate their daytime sleepiness. Indeed the item-scale correlation of this item was not appropriate and its deletion increased the internal consistency of the category, similar to the original study (from 0.63 to 0.86).[12] Furthermore, the strong homogeneity of our studied patients could contribute to a low alpha. However, as the second category reliability is confirmed by the original study,[12] and other linguistic validation studies,[13] translation errors should also be considered in our study.
Among our study population that more than 90% of them were diagnosed as high-risk for OSA, the Persian BQ had acceptable sensitivity of 84% and PPV of 96%, however, specificity of 61.5% and NPV of 25.8% for diagnosing OSA with AHI > 5 as the gold standard. Predictive parameters of BQ have been very different in previous studies. Regarding the studies conducted on patients without history/complaints of sleep disorders, the original study in primary care setting found a sensitivity of 86%, specificity of 77%, PPV of 88%, and NPV of 72% against RDI > 5[12] and another study in preoperative surgical patients showed a sensitivity of 68.9% and specificity of 56.4% (PPV 779% and NPV 44.9%).[15] Furthermore, a Norwegian population-based study found a sensitivity and specificity of 37.2% and 84.0%, respectively (PPV 61.3% and NPV 66.2%) against AHI ≥ 5.[16] With regard to the studies on patients with sleep complaints, the Arabic BQ has a sensitivity of 97% and specificity of 90% (PPV 96% and NPV 93%) against AHI > 5[13] while the Portuguese BQ showed sensitivity of 72.1% and specificity of 50% (PPV 87.7% and NPV 26.7%) against AHI > 5 in respiratory/sleep clinic patients[17] Ahmadi et al., with retrospective chart review study of sleep clinic patients, found a sensitivity of 68% and specificity of 46% (PPV 48% and NPV 65%) against RDI > 10[18] Among patients with cardiovascular problems, BQ showed a sensitivity of 68% to 70% and specificity of 34% to 48% (PPV 56-68% and NPV 50-64%) against AHI ≥ 5.[19,20] These differences may be due to differences in studied population and the factors that may conflict with OSA sign and symptoms, including complicated health conditions of cardiovascular patients (that may cause sleep disturbances), and also patients underling diseases such as hypertension and obesity. Difference between studies regarding the gold standard, RDI versus AHI, is also of great importance in this regard as the RDI is more broaden than the AHI.
Other factors that may affect the accuracy of BQ in diagnosing OSA are suggested as age, BMI, underling disease and the capability of the individuals to works. For example, among the young nurses for RDI ≥ 5 the validity parameters for BQ would be weaker than other populations, it seems to be due to lower prevalence rates of sleep apnea in this population. Moreover, the nurses expect to have poorer sleep quality because of their job situations. So this may affect their response to self-administered screening tests (BQ).[21] Other study demonstrated the sensitivity of 76.7% and specificity of 39.3% at a cut-off of AHI > 15, and lower accuracy of the test in older individuals, women (as our data confirm that as well) and patients with hypertension.[22] This was similar to our findings that the accuracy of BQ was better among men and women; however, the original study did not confirm a gender effect.[12] Regarding the BMI, the Arabian study, in which the participants were more obese than in our study (mean BMI of 41.2) found better predictive values, as the BMI is included in the third category of the BQ.[14]
According to our study, and similar to some other reports,[18,22] separate analysis of the BQ categories showed better sensitivity and specificity for the first versus the second category. Furthermore, Sharma et al. modified the item nine in the 2nd category and found higher sensitivity of 85% and specificity of 95% (PPV 96% and NPV 81%) for AHI > 5.[23] According to these results, it seems that this item needs modification and further studies are warranted in this regard.
There are some limitations to our study. The possibility of errors in translation may have effects on predictive values of the Persian BQ. Furthermore, our study sample was very homogenous and not large enough as there were only 13 cases that had not OSA based on sleep study. Therefore, further studies on editing, modifying, and applying the BQ in a larger sample of patients are warranted in our society.
CONCLUSIONS
According to high sensitivity and PPV of the test, the Persian BQ is useful as a screening test for diagnosing OSA in patients with sleep complaints. However, the test has very low specificity and NPV and thus, cannot be used for rolling out OSA among such patients. Further studies on editing, modifying, and applying the BQ in a larger sample of patients are warranted in our society
ACKNOWLEDGMENTS
This study was supported by the Isfahan University of Medical Sciences as a thesis for obtaining specialty degree in Internal Medicine. Authors are thankful to Bamdad Sleep Clinic staff for helping in data gathering, Dr. Ali Gholamrezaei for data analysis, and Dr. Leila Mirbagher for editing this report.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Amra B, Farajzadegan Z, Golshan M, Fietze I, Penzel T. Prevalence of sleep apnea-related symptoms in a Persian population. Sleep Breath. 2011;15:425–9. doi: 10.1007/s11325-010-0353-4. [DOI] [PubMed] [Google Scholar]
- 2.Terán-Santos J, Jiménez-Gómez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents Cooperative Group Burgos-Santander. N Engl J Med. 1999;340:847–51. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 3.Schäfer H, Koehler U, Ewig S, Hasper E, Tasci S, Lüderitz B. Obstructive sleep apnea as a risk marker in coronary artery disease. Cardiology. 1999;92:79–84. doi: 10.1159/000006952. [DOI] [PubMed] [Google Scholar]
- 4.Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000;283:1829–36. doi: 10.1001/jama.283.14.1829. [DOI] [PubMed] [Google Scholar]
- 5.Amra B, Bahaee FS, Amini M, Golshan M, Fietze I, Penzel T. Sleep Apnea Symptoms in Diabetics and their First Degree Relatives. Int J Prev Med. 2012;3:95–101. [PMC free article] [PubMed] [Google Scholar]
- 6.Hung J, Whitford EG, Parsons RW, Hillman DR. Association of sleep apnoea with myocardial infarction in men. Lancet. 1990;336:261–4. doi: 10.1016/0140-6736(90)91799-g. [DOI] [PubMed] [Google Scholar]
- 7.Dyken ME, Somers VK, Yamada T, Ren ZY, Zimmerman MB. Investigating the relationship between stroke and obstructive sleep apnea. Stroke. 1996;27:401–7. doi: 10.1161/01.str.27.3.401. [DOI] [PubMed] [Google Scholar]
- 8.Reuveni H, Greenberg-Dotan S, Simon-Tuval T, Oksenberg A, Tarasiuk A. Elevated healthcare utilisation in young adult males with obstructive sleep apnoea. Eur Respir J. 2008;31:273–9. doi: 10.1183/09031936.00097907. [DOI] [PubMed] [Google Scholar]
- 9.Mold JW, Quattlebaum C, Schinnerer E, Boeckman L, Orr W, Hollabaugh K. Identification by primary care clinicians of patients with obstructive sleep apnea: A practice-based research network (PBRN) study. J Am Board Fam Med. 2011;24:138–45. doi: 10.3122/jabfm.2011.02.100095. [DOI] [PubMed] [Google Scholar]
- 10.Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto FJ, et al. Sleep disordered breathing and mortality: Eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anaesth. 2010;57:423–38. doi: 10.1007/s12630-010-9280-x. [DOI] [PubMed] [Google Scholar]
- 12.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 13.Saleh AB, Ahmad MA, Awadalla NJ. Development of Arabic version of Berlin questionnaire to identify obstructive sleep apnea at risk patients. Ann Thorac Med. 2011;6:212–6. doi: 10.4103/1817-1737.84775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sleep-related breathing disorders in adults: Recommendations for syndrome definition and measurement techniques in clinical research The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 15.Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. Validation of the Berlin questionnaire and American Society of Anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients. Anesthesiology. 2008;108:822–30. doi: 10.1097/ALN.0b013e31816d91b5. [DOI] [PubMed] [Google Scholar]
- 16.Hrubos-Strøm H, Randby A, Namtvedt SK, Kristiansen HA, Einvik G, Benth J, et al. A Norwegian population-based study on the risk and prevalence of obstructive sleep apnea. The Akershus Sleep Apnea Project (ASAP) J Sleep Res. 2011;20:162–70. doi: 10.1111/j.1365-2869.2010.00861.x. [DOI] [PubMed] [Google Scholar]
- 17.Vaz AP, Drummond M, Mota PC, Severo M, Almeida J, Winck JC. Translation of Berlin Questionnaire to Portuguese language and its application in OSA identification in a sleep disordered breathing clinic. Rev Port Pneumol. 2011;17:59–65. [PubMed] [Google Scholar]
- 18.Ahmadi N, Chung SA, Gibbs A, Shapiro CM. The Berlin questionnaire for sleep apnea in a sleep clinic population: Relationship to polysomnographic measurement of respiratory disturbance. Sleep Breath. 2008;12:39–45. doi: 10.1007/s11325-007-0125-y. [DOI] [PubMed] [Google Scholar]
- 19.Sert Kuniyoshi FH, Zellmer MR, Calvin AD, Lopez-Jimenez F, Albuquerque FN, van der Walt C, et al. Diagnostic accuracy of the Berlin Questionnaire in detecting sleep-disordered breathing in patients with a recent myocardial infarction. Chest. 2011;140:1192–7. doi: 10.1378/chest.10-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martinez D, da Silva RP, Klein C, Fiori CZ, Massierer D, Cassol CM, et al. High risk for sleep apnea in the Berlin questionnaire and coronary artery disease. Sleep Breath. 2012;16:89–94. doi: 10.1007/s11325-010-0460-2. [DOI] [PubMed] [Google Scholar]
- 21.Geiger-Brown J, Rogers VE, Han K, Trinkoff A, Bausell RB, Scharf SM. Occupational screening for sleep disorders in 12-h shift nurses using the Berlin Questionnaire. Sleep Breath. 2012 doi: 10.1007/s11325-012-0705-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Sforza E, Chouchou F, Pichot V, Herrmann F, Barthélémy JC, Roche F. Is the Berlin questionnaire a useful tool to diagnose obstructive sleep apnea in the elderly? Sleep Med. 2011;12:142–6. doi: 10.1016/j.sleep.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 23.Sharma SK, Vasudev C, Sinha S, Banga A, Pandey RM, Handa KK. Validation of the modified Berlin questionnaire to identify patients at risk for the obstructive sleep apnoea syndrome. Indian J Med Res. 2006;124:281–90. [PubMed] [Google Scholar]


