Abstract
Background:
Clinical guidelines have increasingly been used as tools for applying new knowledge and research findings. Although, efforts have been made to produce clinical guidelines in Iran, it is not clear whether they have been used by physicians and what factors are associated with them?.
Methods:
Four hundred and forty three practicing physicians in Tehran were selected from private clinics through weighted random sampling. The data collection tool was a questionnaire on familiarity and attitude toward clinical guidelines. The descriptive and analytical findings were analyzed with t-tests, Chi2, logistic and linear multivariate regression by SPSS, version 16.
Results:
31.8% of physicians were familiar with clinical guidelines. Based on the logistic regression model physicians’ familiarity with clinical guidelines was positively and significantly associated with ‘working experience in a health service delivery point’ OR = 2.13 (95% CI, 1.17-3.90), ‘familiarity with therapeutic protocols’ OR = 2.09 (95% CI, 1.22-3.57) and ‘holding a specialty degree’ OR = 2.51 (95% CI, 1.24-5.07). The mean overall attitude scores in the ‘usefulness’, ‘reliability’, and ‘problems and barriers’ domains were, respectively, 78.9 (SD = 16.5), 78.9 (SD = 19.7) and 50.4 (SD = 15.9) out of a total of 100 scores in each domain. No significant association was observed between attitude domains and other independent variables using multivariate linear regression.
Conclusions:
Little familiarity with clinical guidelines may represent weakness in of production and distribution of domestic evidence. Although, physicians considered guidelines as useful and reliable tools, but problems such as difficult access to guidelines and lack of facilities to apply them were stated as well.
Keywords: Attitude, clinical guidelines, evidence-based medicine, physician
INTRODUCTION
In the ideal situation, evidence should be the grounds on which a person makes decisions. In the medical profession too, new diseases and novel therapeutic techniques demand that a physician be aware and up-to-date with new evidence-based findings. Evidence-based practice ensures that the patient is receiving the correct treatment; the physician is dealing with human life, and incorrect management can prove fatal.[1] On the other hand, statistics show that there is a significant gap between clinical services and scientific evidence. In a study conducted in the US, 30 to 40% of patients had not received effective treatment. Another Australian study showed that 20 to 25% of patients received unnecessary care that sometimes even proved harmful.[2,3] The use of guidelines to apply new knowledge and research findings has greatly increased.[4]
An important approach in preparation of clinical guidelines is the collaboration among all its stakeholders, including patients, physicians, health specialists and executives; this collaboration is necessary for its finalization.[5] According to Lomas, guidelines should “represent the best available solution” to allow their use at the bedside.[6] Many efforts are made by health organizations to encourage the use of CPGs, but in spite of these efforts the use of CPGs at the bedside is limited.[7]
Barriers in attitude and behavior such as lack of trust in available guidelines have led to their low agreeability and prevented their use by physicians.[4,8] Some physicians believe guidelines limit a physician's free thinking and autonomy in certain cases, and limit their innovation at the bedside.[9,10] Naturally, all these barriers potentially limit the willingness to apply CPGs at the bedside. In America, there is a tendency to improve the quality of care and reduce costs, hence hundreds of guidelines have been designed and distributed and up-to-dated.[11] In the UK, more than a decade ago, the large numbers of CPGs produced have been mentioned as a limiting factor in using guidelines.[12] In Iran however, the circumstances have been different. Even though physicians may consult foreign guidelines for their practice or being up-to-date, the preparation and distribution of CPGs has been scarce. To correct this situation, in the past few years certain measures have been taken; one of these goals falls under Iran's fourth development program for the years 2005-2009: preparation and execution of 50 CPGs for general physicians and 20 specific guidelines for each specialty, based on the burden of disease.[13] At the same time certain efforts were made to create infrastructures for compiling valid scientific guidelines to meet the country's demands; educational workshops were held for guideline synthesis and systematic review of clinical evidence,[14,15] compilation and distribution of valid tools for critical appraisal of guidelines (AGREE),[16] design of structures for compilation of guidelines at the level of the ministry of health, and identification and announcement of CPGs to researchers and research funders in the country. On the whole, the numbers of domestic guidelines compiled and distributed in the country do not exceed tens; also, their distribution has been limited. However, there is no information on their application by physicians. Hence, this research can help reduce the barriers to implementation of guidelines by studying physicians’ familiarity and attitude in this field and identifying its strengths and weaknesses.
METHODS
Population under study
The sample size of this cross-sectional study was 385 using Zα at 95% confidence interval = 1.96 and assuming that 50% of physicians are familiar with the guidelines. Physicians considering cases would drop out, 443 privately practicing physicians in four different fields were included from 22 municipality zones: 350 general physicians, 47 pediatricians, 35 internal specialists, and 11 infectious disease specialists. The physicians were chosen randomly from the Medical council and deputies of Tehran's medical universities, proportional to the size in the main population. respectively; 175,140 and 128 physicians from Shahid Beheshti, Iran (former) and Tehran universities were selected. The team of questioners consisted of 17 questioners (each questioner was responsible for collecting data from a maximum of 30 physicians). These individuals were trained in an educational session that lasted 4 h. During this session they were briefed on the study's objectives, their job descriptions and rights. Also, any confusion was obviated; they were taught how to avoid interview errors, and taught how to take a uniform impression of specific terminology. Finally, they were handed the ‘questioner's guide’ and questionnaires were completed by them. They would visit the clinic at the most thrice in case of non-cooperation (if the clinic was very crowded or the physician was absent). Tokens of gratitude were given to the physicians for their participation.
Data collection tool
The data collection tool was a questionnaire consisting of three sections. The first section was related to familiarity with CPGs. It contained questions on the possession, study and application of CPGs and therapeutic protocols. The second section consisted of 22 items on attitude toward the usefulness, reliability, and possible difficulties and barriers of application of CPGs in the form of a Likert scale ranging from “completely agree” to “completely disagree”. This section was adopted from Elovainio et al.'s scale in UK[17] for its validity and reliability. The third section consisted of background variables and potential confounders including sex, age, duration of clinical practice, cumulative grade point average (GPA) gained in medicine (considered in percent here), the average number of patients examined in a week, working experience in a health service delivery point, simultaneous activity in another medical center such as public or private hospitals and clinics or university-in addition to a private clinic, holding a specialty degree and familiarity with therapeutic protocols. Therapeutic protocols are a set of detailed compulsory rules laid out for a specific clinical condition.
‘Health service delivery points’ are public health units in which general medical, dental, para-clinical and outpatient health services are delivered.
The validity and reliability of the attitude section of the questionnaire were determined as follows:
To ensure the validity of the tool the English questionnaire[17] was translated into Persian by two experts. Then the accuracy of the Persian version was reviewed. The content validity of the three sections of familiarity, attitude and background variables was determined by consulting 5 experts on the appropriateness, relevancy and adequacy of the questions. The attitude section's items were altered considering the structural and cultural circumstances of the country; 7 items were omitted and 2 were added. Eventually, 22 items remained in the attitude section that were classified into three domains: 1-physicians’ attitude toward the usefulness of guidelines, 2-physicians’ attitude toward the reliability of guidelines, 3-physicians’ attitude toward the difficulties of applying guidelines. The face validity of the questionnaire was evaluated by 10 expert physicians for its sequence and appearance, and necessary modifications were implemented. The reliability of the questionnaire was evaluated by test-retest on 20 physicians at a two-week interval. The intra-class correlation coefficient (ICC) of the questions was between 63 to 92% (median: 78%). To ensure the accuracy of the tool and to examine possible executive difficulties, a pilot study was performed on 20 physicians. Cronbach's alpha was calculated separately for the three attitude domains, attitude toward the usefulness of CPGs (6 items), reliability of CPGs (4 items), and problems and barriers associated with them (12 items). Cronbach's alpha was 80%, 90% and 74% respectively, which indicate acceptable internal validity for the attitude domains.
Statistical analysis
In analyzing the data of the first section of the questionnaire, those physicians who claimed they were familiar with CPGs and using them, and had at least seen one domestically designed or foreign CPG were considered familiar with CPGs. The second section of the questionnaire (attitude) was assessed in physicians familiar with CPGs only. Two approaches were taken here:
For every item a Likert scale of 1-5 was used ranging from ‘completely disagree’ to ‘completely agree’; options 4 or 5 were considered positive, 3 was considered neutral, and 1 or 2 were considered negative.
The score obtained for attitude toward CPG was calculated by summing up the scores of the three domains’ items (for negatively scored items, scoring was done reversely). Each domain's scores were considered between 0-100 as follows;
(the mean score of each domain-the minimum possible score) × (100/the maximum score – the minimum score)
A higher score represented a more positive attitude toward CPG. Data were entered by two persons independently. Univariate analysis was performed. Multivariate logistic and linear regressions were used for variables that had a P value lower than 0.2 in the univariate analysis by the enter method.
Ethical considerations
Individuals participated in the study voluntarily and with consent. Necessary arrangements with the physicians were made with prior appointments, and questionnaires were completed anonymously.
This study has the approval of Tehran University of Medical Science's ethical committee.
RESULTS
Participants’ characteristics
Among 443 questionnaires, 393 (88.9%) were completed. Fifty physicians were contacted thrice and refused to cooperate. Analysis of the demographic data of this group showed that their sex and age distribution were not significantly different from the physicians who had participated in the study. Also, 10 out of 393 physicians were excluded from the study because of conflicting responses. Eventually, 383 persons’ data were analyzed. Seventy one point nine percent (71.9%) were male and 28.1% were female. Their mean age was 47.59 years (SD = 11.66). The minimum and maximum ages were 27 and 82 respectively. The duration of clinical practice was between 1 and 58 with a mean = 16.39 (SD = 11.36). Thirty one point eight percent (122 persons) were familiar with CPGs. On the whole, only 30.8% of physicians studied CPGs, and only 28.6% claimed they used these evidence-based recommendations. There were significant associations between familiarity with CPGs and working experience in a health service delivery point (OR = 1.86; 95%CI, 1.12-3.08 (, simultaneous activity in a private hospital (OR = 2.02; 95%CI, 1.15-3.56), familiarity with therapeutic protocols (OR = 2.61; 95%CI,1.67-4.06) and holding a specialty degree (OR = 2.16; 95% CI,1.35-3.46), in the univariate analysis [Table 1].
Table 1.
Participants’ characteristics and relation between physicians’ familiarity with clinical guidelines and independent variables (N=383)
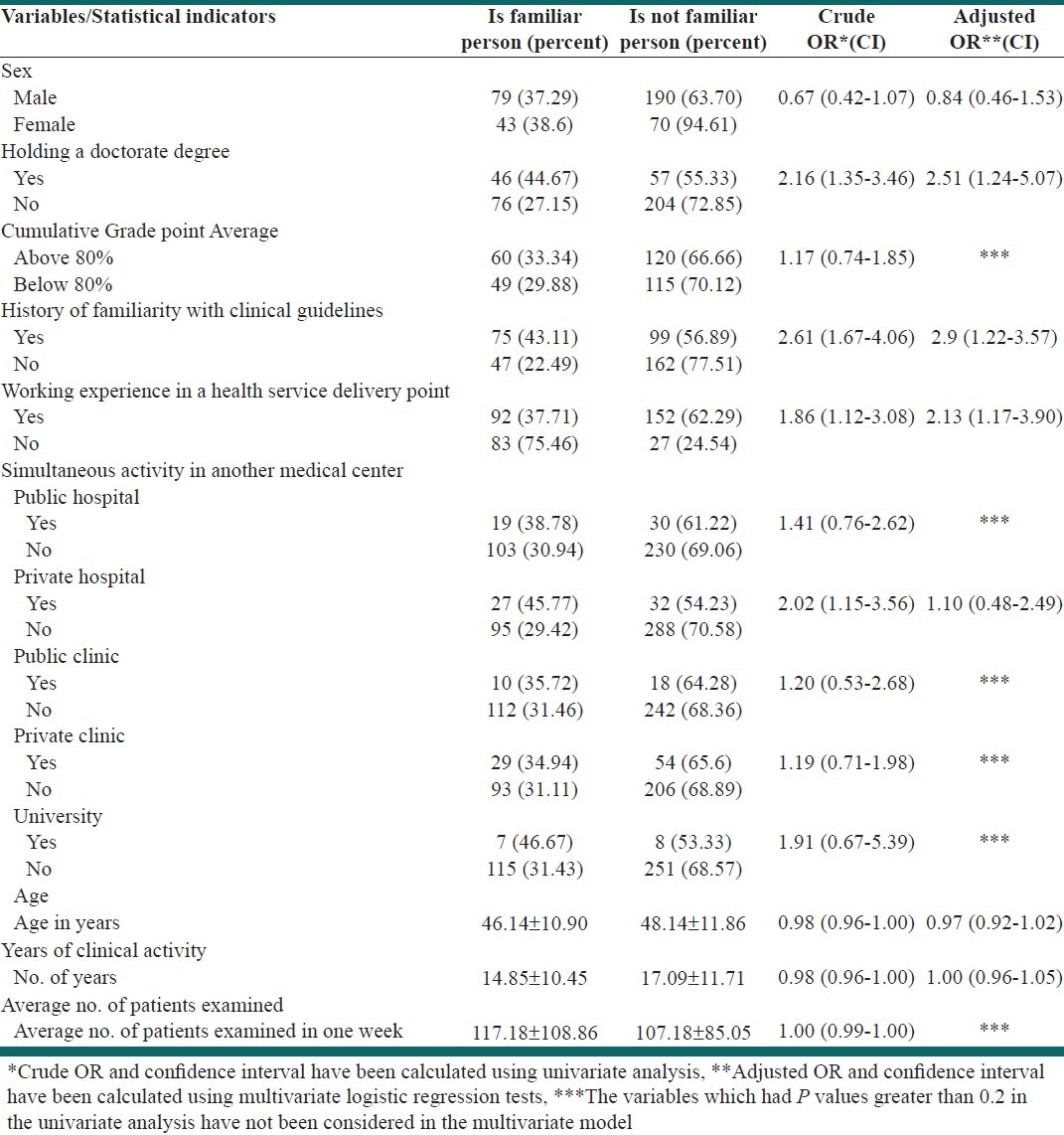
Based on the multivariate logistic regression, considering familiarity with CPGs as the dependent variable and independent variables with a significance level lower than 0.2 in the univariate analysis, using the enter method, there was a positive and significant association between working experience in a health service delivery point OR = 2.13, 95% CI: 1.17-3.90, familiarity with therapeutic protocols OR = 2.09, 95% CI: 1.22-3.57, and holding a specialty degree OR = 2.51, 95% CI: 1.24-5.07, but no significant association existed with other variables [Table 1].
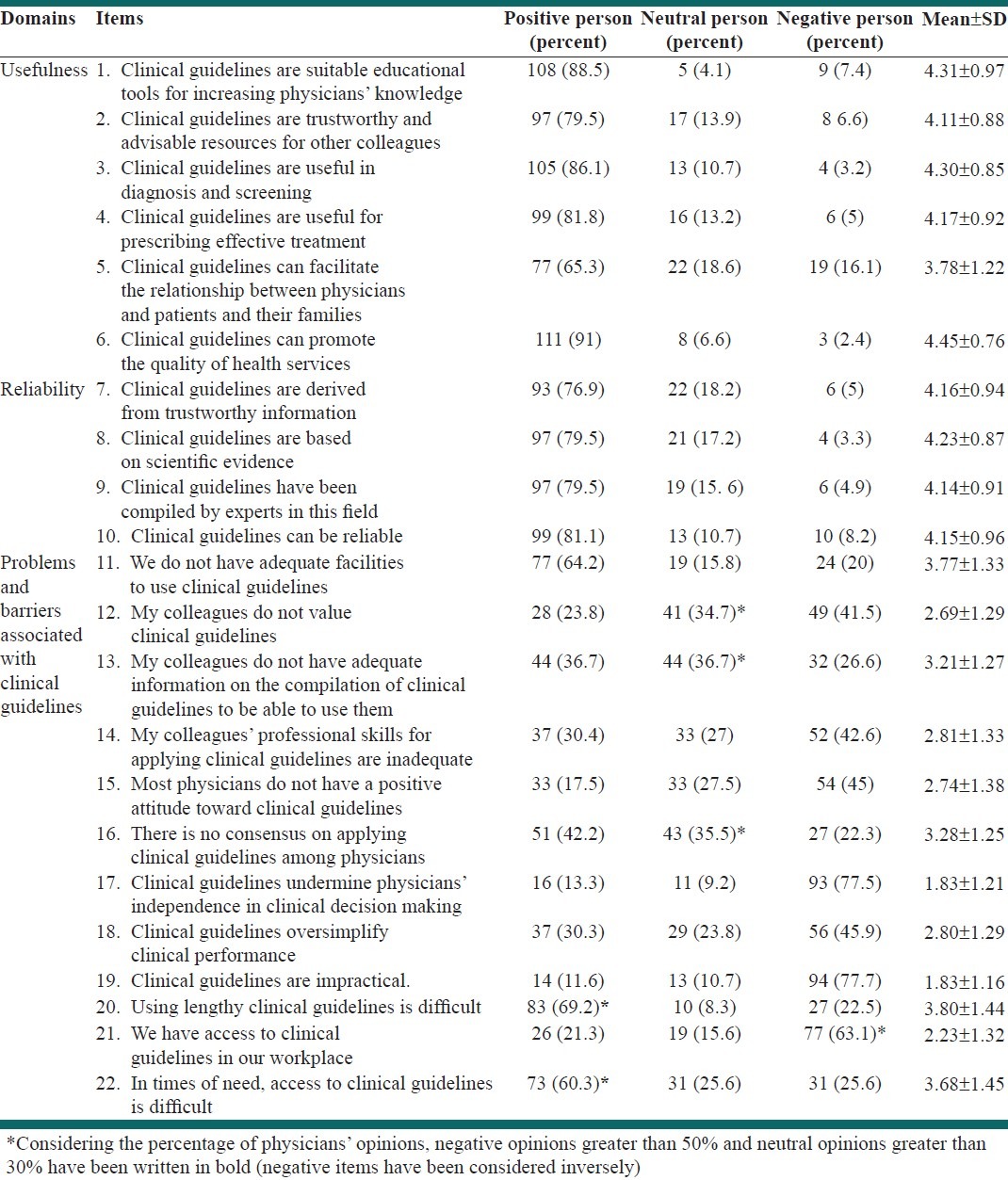
To study the attitude of physicians familiar with CPGs, the frequency of positive, neutral and negative attitudes, their means and standard deviations were calculated for each item [Table 2]. The overall attitude scores in the domains ‘usefulness’, ‘reliability’ and ‘absence of barriers and difficulties’ were 78.9 (SD = 16.5), 78.9 (SD = 19.7) and 50.4 (SD = 15.9) respectively, out of a total of 100 scores in each domain. The univariate analysis showed a positive and significant association between attitude toward difficulties in applying guidelines and being familiar with therapeutic protocols (P = 0.003), but there was no statistically significant association between the other two domains and the other variables. No statistically significant association was present in the attitude domains in linear multivariate regression analysis.
Table 2.
Physicians’ attitude toward clinical guidelines. Mean and standard deviations of scores are include
DISCUSSION
In Iran the limited distribution of CPGs has been ineffective and physicians have not had adequate access to guidelines. In this study, we have analyzed the findings in two sections of familiarity and attitude toward CPGs. In the familiarity section, only 31.8% of physicians were familiar with CPGs.
A study performed in Isfahan in 2007-2009 to assess physicians’ awareness on evidence-based medicine (EBM) showed that among 181 physicians of various specialties, less than half i.e., 41% stated they had used evidence-based findings in their clinical practice; 70% recognized absence of appropriate educational courses as a main barrier in applying EBM.[18] Evidence on the status of application of CPGs in developing countries was little.[19] For example, a study conducted in Malaysia in 1999 less than half (48.5%) private physicians knew what CPGs were, and only 22.7% used them in their clinical practice.[20] Another study conducted in India (2008) to examine physicians’ attitude toward EBM, physicians’ preference to use scientific references such as books, scientific journals and CPG were 100%, 86% and 44%, respectively.[21] However, in a study performed in Zimbabwe 72.6% of physicians were familiar with at least one CPG and 65.9% claimed they used CPGs in their clinical practice.[22] Among developed countries, a study conducted in Canada in 1997 showed that the rate of use of CPGs was lower as compared to other references such as reference books, articles, conference or workshops.[23] Anyhow, inadequate production and dissemination of CPGs may be one of the reasons behind physicians’ unfamiliarity with CPGs. In our study, most physicians stated they had access to limited number of CPGs, and used them in their clinical practice. Results from a study in USA showed that more than half of physicians had changed their clinical practice on the basis of CPGs and 3% stated they did not believe in CPGs at all and did not use them.[24] Based on our findings, familiarity with CPGs was significantly higher in specialists than in general physicians. A positive significant association was observed between working experience in a health service delivery point and percentage of familiarity with CPGs. Preparation and delivery of clinical protocols to health service delivery points is one of the District Health Centers’ duties. So it may explain why CPGs have been distributed more systematically to health service delivery points.
In the attitude section, examining the total scores in each of the three domains showed that the scores obtained in usefulness and reliability domains were closer to 100. However, in the absence of difficulties and barriers in application of CPGs’ domain, attitude was not very positive and scores were low. In a cross-sectional study in Isfahan (2007-2009), physicians’ overall attitude toward EBM was positive, and 70% believed that EBM promotes health service delivery.[18] Several studies from around the world showed that on the whole, physicians’ attitude toward CPGs is positive. For example, in the USA most family physicians thought using CPGs was useful and their mean attitude scores were higher than 3 (where scores ranged from 1 -5).[24] In the Malaysia study 64% of physicians thought CPGs were useful and almost 54% believed evidence-based CPGs could improve the process of patient care, and 41.6% believed that CPGs could lead to physicians’ greater satisfaction in clinical practice.[20] In the 2004, Zimbabwe study the overall attitude toward CPGs was acceptable, but 66.2% of physicians believed their flexibility in treatment was limited by guidelines.[22] In a systematic review in 2002, almost 30% (12 studies) agreed that guidelines are impractical and rigid for application at the bedside, but physicians’ opinions toward their usefulness was positive on the whole.[25] In addition to examining the scores obtained in the three attitude domains, the items also showed physicians’ positive opinion on CPGs in the first 10 items. We learnt that most physicians (88.5%) saw guidelines as a suitable educational tool for knowledge promotion, and 91% agreed that guidelines can promote the quality of healthcare. Sixty five point three percent agreed on the usefulness of guidelines in facilitating the physician-patient relationship.
Also, 86.1%, 81.8% and 79.5% of physicians recognized guidelines as useful for screening, diagnosis, treatment and advice to other colleagues respectively. These findings were similar to those of the mentioned systematic review; among the 30 English articles published 75% of clinical physicians (24 reviews) agreed that guidelines were useful resources for prescriptions, 71% (14 studies) believed that guidelines were useful educational tools, and 70% (16 studies) believed that guidelines helped improve quality of care.[25,23] Items 7-10 showed positive attitude toward e scientific accuracy of guidelines. These findings were in line with many other studies’ findings. For example, in a study conducted in Canada, more than 50% of physicians agreed that guidelines were reliable sources for prescriptions.[23,25–28] The acceptability and success of applying CPGs is associated with multiple factors. In a qualitative study in UK on the influential factors in applying guidelines, the following items were summarized in 7 main themes, including: 1. The acceptability of the subject and content, 2. The acceptability of the references, 3. Being presentable, 4. People's impact, 5. Organizational factors, 6. Disease characteristics, 7. Guideline dissemination strategies. Any shortcoming in either of these factors can play a part in the awareness, attitude, acceptance and application of clinical guidelines.[29] Upon examining the items on lack of barriers to application of guidelines, we found that a higher percentage of physicians had negative or neutral attitudes, the explanations of which are given below:
Thirty seven percent of physicians believed that they had insufficient information on the way guidelines are prepared, and 37% had no opinion (Table 2, item 13).
Only 22.3% agreed on using guidelines. Thirty one percent believed physicians weren’t skilled enough to use guidelines, (Table 2, items 11 and 14).
About 70% of physicians thought using lengthy guidelines was difficult (Table 2, item 13). In fact those guidelines are considered presentable that possess clarity, simplicity and discipline.[29]
Sixty five percent of physicians believed conditions were unfavorable for applying guidelines (Table 2, item 13). According to the evidence, the availability of resources and facilities in applying guidelines is a multidimensional process, therefore it requires the support of national organizations for its production and dissemination, and commercialization should be avoided.[29]
More than 60% of physicians agreed on the difficulty in accessing guidelines (Table 2, items 21 and 22). According to the evidence, difficult access to guidelines in times of need can be a result of dissemination strategies.[29]
On the basis of our findings, a higher percentage of physicians assessed their colleagues’ attitude toward guidelines as positive (41.5%), and did not see guidelines as impractical (77.7%), and didn’t see them as barriers to a physicians’ independence (77.5%).
The high response rate of the physicians was one of the positive aspects of this study. Although only one third of physicians were familiar with CPGs, in the attitude section we were able to examine the attitude of those physicians only (122 persons).
According to the viewpoint of experts in our country, CPGs are prepared and available in different domestic or foreign topics, but since we did not have any specific statistics on the mode of access and use of guidelines in the country, we studied the overall attitude toward them. Some physicians’ opinions may have been based on a specific type of guideline they have read, but the questions were general, therefore the results are not generalizable to each and every guideline; they are general. Data were collected through interviews, so questionnaires wouldn’t be completed inattentively by the physicians. Also, questioners were given necessary training not to leave any question unanswered and to prevent random and systematic errors.
On the whole, our findings showed that physicians thought CPGs were useful and reliable, but multiple problems and barriers were mentioned in the field of awareness and preparation of guidelines. This can represent weakness in creating domestic evidence; therefore compiling valid national guidelines that are more suitable to the country's demands can be a positive effort to familiarize physicians with them for their better application at the bedside. Based on this finding a fundamental solution to the application and follow-up of guidelines in the country can be to establish a ‘general standards office’ to prepare scientific contexts on the basis of existent evidence, and to create and disseminate national guidelines in the presence of all its# stakeholders and supervise them.
CONCLUSIONS
The low familiarity rate of CPGs is an important point, because, on one hand, it can represent the weakness in creating domestic evidence and creating CPGs and on the other hand it can indicate problems in notification at service providers’ level. Effective notification strategies and education planning for physicians seem to be helpful in this respect. The attitude section showed that physicians familiar with guidelines have a positive attitude toward their usefulness and reliability. Barriers such as the length of CPGs, difficulty of access to guidelines, and lack of facilities for using guidelines show the need to conduct studies on the barriers to production and dissemination of CPGs in the country.
ACKNOWLEDGMENTS
This study was part of a M.S. thesis supported by Tehran University of Medical Sciences (grant No: 87_04_74_8168). We would like to thank Katayoun Maleki for translating and scientifically editing the manuscript. We would also like to extend our gratitude to Zahra Mounesan, Maryam Mounesan and Ayat Ahmadi for helping us in the execution of the project.
Footnotes
Source of Support: Tehran University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.Jordan TJ. Understanding Medical Information: A User's Guide to Informatics and Decision-Making. 2002 [Google Scholar]
- 2.Schuster MA, McGlynn EA, Brook RH. How good is the quality of health care in the United States? Milbank Q. 1998:517–63. doi: 10.1111/1468-0009.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39:II46–54. doi: 10.1097/00005650-200108002-00003. [DOI] [PubMed] [Google Scholar]
- 4.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don’t physicians follow clinical practice guidelines. A framework for improvement? JAMA. 1999;282:1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 5.Woolf SH. Practice guidelines, a new reality in medicine: II. Methods of developing guidelines. Arch Intern Med. 1992;152:946–52. [PubMed] [Google Scholar]
- 6.Lomas J. Making clinical policy explicit: Legislative policy making and lessons for developing practice guidelines. Int J Technol Assess Health Care. 1993;9:11–25. doi: 10.1017/s0266462300002993. [DOI] [PubMed] [Google Scholar]
- 7.Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8:1–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 8.Lawler F, Viviani N. Patient and physician perspectives regarding treatment of diabetes: Compliance with practice guidelines. J Fam Pract. 1997;44:369–73. [PubMed] [Google Scholar]
- 9.Deutsch S, Denton M, Borenstein J. Clinical practice guidelines: A tool to help provide quality care. (61-4, 70, 73-4).Geriatrics. 1998;53:57. quiz 75. [PubMed] [Google Scholar]
- 10.Delamothe T. Wanted: Guidelines that doctors will follow. BMJ. 1993;307:218. doi: 10.1136/bmj.307.6898.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christakis DA, Rivara FP. Pediatricians’ awareness of and attitudes about four clinical practice guidelines. Pediatrics. 1998;101:825–30. doi: 10.1542/peds.101.5.825. [DOI] [PubMed] [Google Scholar]
- 12.Hibble A, Kanka D, Pencheon D, Pooles F. Guidelines in general practice: The new Tower of Babel? BMJ. 1998;317:862–3. doi: 10.1136/bmj.317.7162.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Assemblies DoC-oaSo. National Development Act “Fourth Economic, Social and Cultural Development Plan”. 2005:36–7. [Google Scholar]
- 14.Yousefi Nooraie R, Rashidian A, Nedjat S, Majdzadeh R, Mortaz Hedjri S, Etemadi A, et al. Promoting development and use of systematic reviews in a developing country. J Eval Clin Pract. 2009;15:1029–34. doi: 10.1111/j.1365-2753.2009.01184.x. [DOI] [PubMed] [Google Scholar]
- 15.Nedjat S, Nedjat S, Maleki K, Gholami J, Ashoorkhani M, Majdzadeh R. Methodologies and Messages in Iranian Articles on Maternal Care, Diabetes Mellitus, and Tuberculosis, Published in 2001-2006. Int J Prev Med. 2012;3:42–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Rashidian A, Yousefi-Nooraie R. Development of a Farsi translation of the AGREE instrument, and the effects of group discussion on improving the reliability of the scores. J Eval Clin Pract. 2012;18:676–81. doi: 10.1111/j.1365-2753.2011.01649.x. [DOI] [PubMed] [Google Scholar]
- 17.Elovainio M, Eccles M, Mäkelä M. Changing professional practice. Copenhagen: DSI, Danish Institute for Health Services Research and Development; 1999. Attitudes towards guidelines and a scale for measuring them; pp. 153–68. [Google Scholar]
- 18.Mozafarpour S, Sadeghizadeh A, Kabiri P, Taheri H, Attaei M, Khalighinezhad N. Evidence-based medical practice in developing countries: The case study of Iran. J Eval Clin Pract. 2011;17:651–6. doi: 10.1111/j.1365-2753.2011.01642.x. [DOI] [PubMed] [Google Scholar]
- 19.Zolala F, Haghdoost AA. A gap between policy and practice: A case study on maternal mortality reports, Kerman, Iran. Int J Prev Med. 2011;2:88–93. [PMC free article] [PubMed] [Google Scholar]
- 20.Lian PC, Marnoch G. Knowledge and attitudes of Malaysian private medical practitioners toward guidelines-based medicine. J Manag Med. 1999;13:178–89. doi: 10.1108/02689239910292071. [DOI] [PubMed] [Google Scholar]
- 21.Gavgani VZ, Mohan VV. Physicians’ Attitude towards evidence-based medical practice and health science library services. LIBRES. 2008;18 [Google Scholar]
- 22.Bhagat K, Nyazema N. General practitioners and clinical guidelines. East Afr Med J. 2004;78:30–4. doi: 10.4314/eamj.v78i1.9109. [DOI] [PubMed] [Google Scholar]
- 23.Hayward RS, Guyatt GH, Moore KA, McKibbon KA, Carter AO. Canadian physicians’ attitudes about and preferences regarding clinical practice guidelines. CMAJ. 1997;156:1715–23. [PMC free article] [PubMed] [Google Scholar]
- 24.Wolfe RM, Sharp LK, Wang RM. Family physicians’ opinions and attitudes to three clinical practice guidelines. J Am Board Fam Pract. 2004;17:150–7. doi: 10.3122/jabfm.17.2.150. [DOI] [PubMed] [Google Scholar]
- 25.Farquhar CM, Kofa EW, Slutsky JR. Clinicians’ attitudes to clinical practice guidelines: A systematic review. Med J Aust. 2002;177:502–6. doi: 10.5694/j.1326-5377.2002.tb04920.x. [DOI] [PubMed] [Google Scholar]
- 26.Flores G, Lee M, Bauchner H, Kastner B. Pediatricians’ attitudes, beliefs, and practices regarding clinical practice guidelines: A national survey. Pediatrics. 2000;105:496–501. doi: 10.1542/peds.105.3.496. [DOI] [PubMed] [Google Scholar]
- 27.Bochud M, Cornuz J, Vader JP, Kamm W, Burnand B. Are internists in an non-prescriptive setting favourable to guidelines. A survey in a Department of Internal Medicine in Switzerland? Swiss Med Wkly. 2002;132:201–6. doi: 10.4414/smw.2002.09853. [DOI] [PubMed] [Google Scholar]
- 28.Hobbs F, Erhardt L. Acceptance of guideline recommendations and perceived implementation of coronary heart disease prevention among primary care physicians in five European countries: The Reassessing European Attitudes about Cardiovascular Treatment (REACT) survey. Fam Pract. 2002;19:596–604. doi: 10.1093/fampra/19.6.596. [DOI] [PubMed] [Google Scholar]
- 29.Rashidian A, Eccles MP, Russell I. Falling on stony ground. A qualitative study of implementation of clinical guidelines’ prescribing recommendations in primary care? Health Policy. 2008;85:148–61. doi: 10.1016/j.healthpol.2007.07.011. [DOI] [PubMed] [Google Scholar]


