Abstract
Background:
Treatment of childhood obesity is difficult, and successful management may differ in various areas with different cultural backgrounds. The present study was conducted to assess the effect of lifestyle modification family-based intervention in young Iranian children.
Methods:
This field trial study was conducted in 2011 among 156 obese children in Tehran, Iran. They were randomly assigned to intervention and control groups. At baseline, anthropometric measurements and biochemical analysis were performed. The second and third phases consisted of training sessions for parents of the intervention group. At the fourth phase, there was no training program. In all four phases, questionnaires on demographic characteristics, lifestyle and food frequency were completed by interviewing with mothers, and biochemical analysis was repeated at the end of the study.
Results:
During the second and third phases of the study, weight and height increased significantly in both groups, although weight increased more slowly, and waist and hip circumferences was decreased in the intervention group. Serum triglycerides and cholesterol decreased significantly in the intervention group (P < 0.05). Analysis of food group consumption showed that in the intervention group, not only consumption of milk, dairy and nuts group increased significantly but also the corresponding figure decreased for bread and cereals, sugar and confectionery ingredients; moreover, the family's oil and fat consumption decreased significantly (P < 0.05). Watching TV and playing on the computer decreased significantly in the intervention group; however, walking time increased significantly in both groups (P < 0.05).
Conclusions:
The family-based lifestyle program had limited but desirable effects on anthropometric and metabolic outcomes of the obese children. We suggest that a longer period of intervention may have more favorable results.
Keywords: Children, family-based intervention, obesity
INTRODUCTION
Nowadays, obesity has accelerated at an alarming rate in children worldwide.[1,2] Obesity, which is caused by imbalance between energy intake and energy expenditure, can be multifactorial (unhealthy lifestyle, genetic, economical, cultural and social status).[3] Analysis of 144 studies in different countries during 2010 showed that 43 million preschool children were overweight or obese. In Asia, prevalence of overweight and obesity in preschool children was 4.9% in 2010.[4] Recent reports indicate that over 15% of children living in Iran and neighboring countries are overweight or obese.[5–9] According to a national report, it was estimated that 4.4% of school children of Iran were obese.[10] Following this, the prevalence of obesity in preschool children was recorded as 4.8% in boys and 4.5% in girls in Tehran.[11]
Childhood obesity increases the risk of adulthood obesity. It is reported that 80% of obese children become obese adults,[12] which can bring about non-communicable diseases, academically unsuccessful, socially inept and behavioral problems.[13–15]
Hence, a valuable strategy to promote healthy lifestyle from early childhood is behavioral lifestyle modification, focused on dietary and activity habits by parental involvement as the primary agents. Thus, alarming and motivating them for stability of lifestyle changes is crucial.[16–20] As long as family bonding has a vital role in the child's behavioral modeling, and also school age is the most appropriate time for acquiring knowledge and habits, and because of there being limited research on obesity in preschool children, this study was the only one taken specifically on 7-year-old obese children to evaluate a family-based behavioral intervention to promote physical activity and healthy dietary habits in Tehran in 2011.
METHODS
This was a field trial study conducted in a random sample of 7-year-old obese children (n = 156) who were selected from nine health centers of three districts in the north of Tehran. The Ethics Committee of National Nutrition and Food Technology Research Institute approved the study.
Participants
Five hundred and fifty obese children were introduced by nine health centers based on study criteria (child age 7 years old, ≥95th percentile of body mass index (BMI) for age and willing to participate). Afterwards, a trained member of the research team called them to describe the study and to confirm an initial screening for eligibility. Children got a code number and were randomly divided into two groups; intervention (n = 70) and control (n = 86). Then, based on timetable schedule, they were invited to fieldwork (National Nutrition and Food Technology Research Institute) for secondary screening.
Parents and children who expressed their interest were assigned and then they completed the consent form. Ultimately, based on exclusion criteria (mental retardation, psychiatric symptoms, current obesity treatment, chronic disease and use of medication), 156 obese children were recruited.
Study design
The study was designed in four phases as follows [Figure 1].
Figure 1.
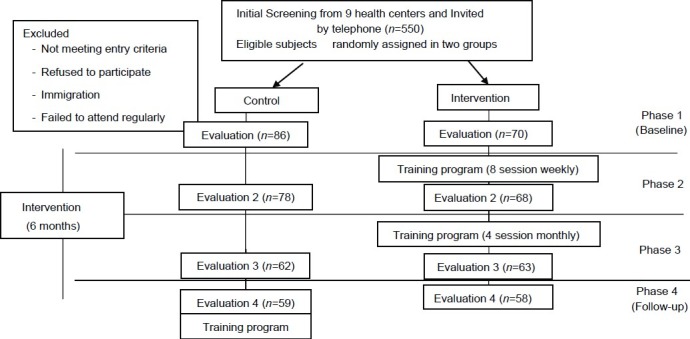
Study design
Phase 1 (Baseline)
In this phase, we measured anthropometric indices and completed socio-demographic and semi-quantitative food frequency questionnaires (FFQ).[21] For each subject, these evaluations were repeated at three phases later. In addition, biochemical analysis was only done at phases 1 and 4 because of ethical obligations.
Anthropometric measurements
Weight, height and waist and hip circumference were measured by trained experts. Weight was measured to the nearest 0.1 kg using a calibrated and certified portable digital scale (Beurer, made in Germany) with lightly dressed, without shoes and empty pockets. Height was determined on a standing position, barefoot using a portable height gauge (Seca) with accuracy of 0.1 cm. Then, the BMI was calculated (kg/m2). Children with BMI over the 95th percentile for age were identified as obese children.[22,23]
The waist circumference was measured at the smallest area between the edge of the lower chest and iliac crest bone.[13,23,24] Hip circumference was measured at the maximum level over light clothing and at the widest girth of the hip using an unstretched tape meter without any pressure to the body surface. These measurements were recorded to the nearest 0.1 cm.[25,26] Before the examination, the scale was calibrated and the mean of the two measurements was recorded.
Biochemical analysis
For blood sampling, subjects were asked to be 12 h overnight fasting and were invited to a health center near the fieldwork. Blood (5 cc) was taken from the cubical vein after confirming the 12-h fasting with parents. Also, parents were allowed to accompany their child during sampling. The fasting blood glucose, triglyceride (TG), total cholesterol[27] low-density lipoprotein-cholesterol (LDL-C) and high-density lipoprotein-cholesterol (HDL-C) concentrations were analyzed on fresh blood (on the day it was collected) using a commercial kit based on the enzymatic method (Pars Azmoon, Iran) with an auto-analyzer (Selectra E, Vita lab, Netherlands). Validity and reliability of measurement instruments were evaluated. After collecting blood samples, the children were served a healthy breakfast and a gift.
Questionnaires
Questionnaires on socio-demographic characteristics and FFQ were completed by interviewing with trained dieticians who are experienced in working with obese children. Socio-demographic questionnaire included family number, parents’ occupation and education, birth weight, duration of breastfeeding, gestational diabetes, history of obesity in family, walking to school, play with computer game and watching TV.
The validated FFQ was used to assess typical food intake over the previous year and, currently, included 168 items. For converting portion sizes to grams, household measures was used.[28]
Phases 2 and 3: (Family-based intervention)
An applicable 12-session training program for 6 months was designed with parents in the intervention group.
Parents attended to eight sessions weekly, for the first 2 months, then four sessions remained, which were held monthly. Each session lasts 4 h and started with a review of parent progress in implementing the strategies developed for changing their child's eating or exercise habits. Parents were intimated by group leaders about the successes, challenges and barriers encountered as they attempted to make lifestyle changes as well as the possible strategies for overcoming various challenges during the previous session.
The second segment of the session focused on the specific topic of the day. Sessions’ topics such as learning about the reasons of the childhood obesity, receiving nutritional information (e.g., food pyramid, food choices, food labels, food preparation and cooking, eating habits, regular meals, controlling environments that stimulate overeating, special dietary consideration during holidays, vacations and at the restaurants) and guidelines for physical activity and reducing sedentary behaviors (e.g., reduce watching television and playing computer games, use stairs instead of elevators and play outside instead of inside).
Phase 4
According to the study design for this phase, the intervention group did not perform any type of training, educational and follow-up programs. While for the control group, training programs (two sessions) were conducted according to the ethical obligations.
Statistical analysis
After rechecking all the data, statistical analyses were performed using Excel, Access and SPSS software package (version 16; [SPSS] Statistical Package for the Social Sciences Inc., Chicago, IL, USA). Chi-square, Student's t-test, Fisher, Paired-t-test and Friedman test were used to compare the ratios and the means of the groups. Because we measured our variables 4 times during the study, a repeated measurement ANOVA was used to compare data among several times. In this analysis, time effect, group effect and interaction between them were assessed, but, because the group effect was not significant, only the other two P values were mentioned. Statistical significance was established at P value <0.05.
RESULTS
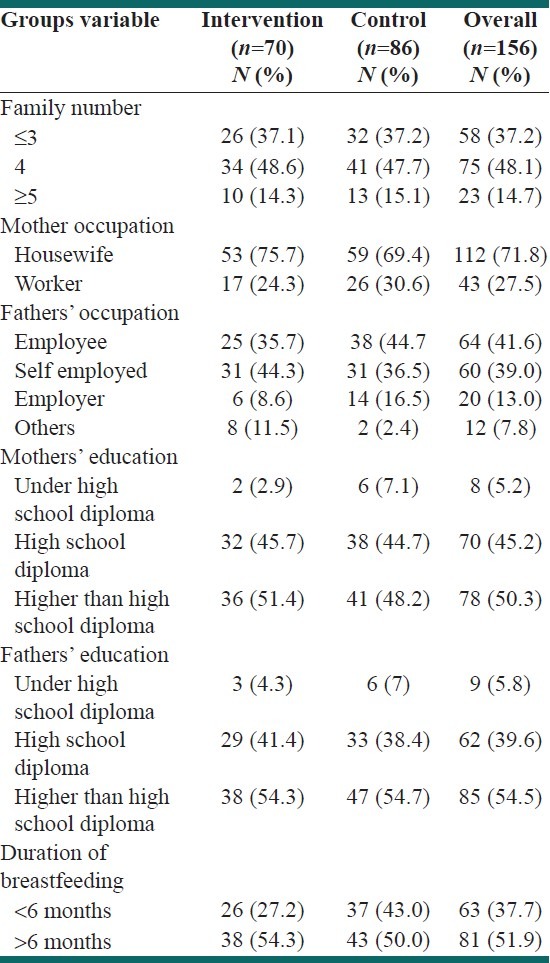
The participants in this study were 156 obese children (80 girls and 76 boys). Family characteristics are shown in Table 1. According to this table, most children were from families with four members per household (48%). The educational level of majority of the parents was higher than diploma. Most of the mothers and fathers were housewife and employee, 72% and 42%, respectively. The mean of children's birth weight was 3290 ± 620 g, and more than half of them were breastfed for more than 6 months (52%). Moreover, only 5% of the mothers gestational diabetes and 44% of the children had a history of obesity in their family. Two study groups were broadly similar at baseline, and these variables were not significantly different between them.
Table 1.
Characteristics of the study participants
Evaluation of physical activities and sedentary behaviors of children showed that walking time increased and watching TV and playing computer decreased significantly in intervention group especially during the 2nd and 3rd phases.
The results of repeated measurement analysis showed that walking, watching TV and playing with computer increased significantly in both groups, but each of these variables was managed better in the intervention group than in the control group; however, the interaction of time and group was not significant.
Evaluation of anthropometric indices in obese children showed that although weight, height and BMI increased significantly in both groups, this increase was lower in the intervention group compared with the control group, especially at the second and third phases. In addition, decline in waist and hip circumferences were also seen during the intervention phases [Table 2].
Table 2.
The trend of anthropometric indices of obese children in 4 phases
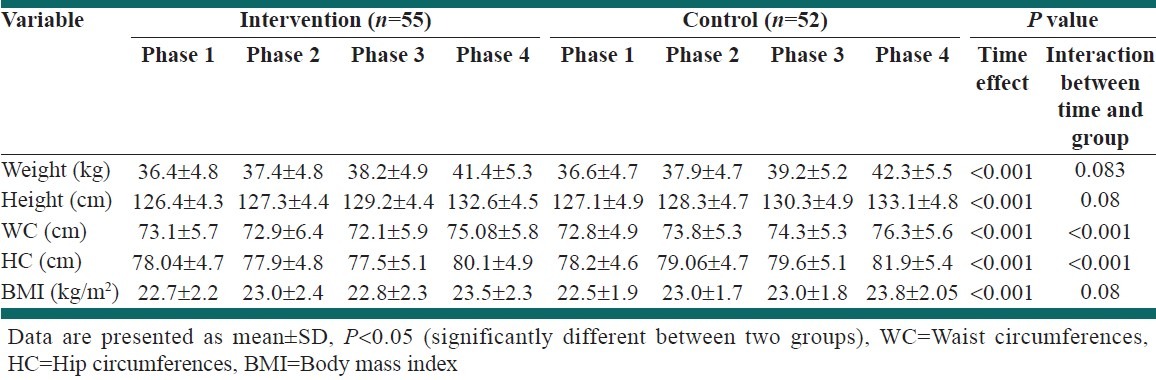
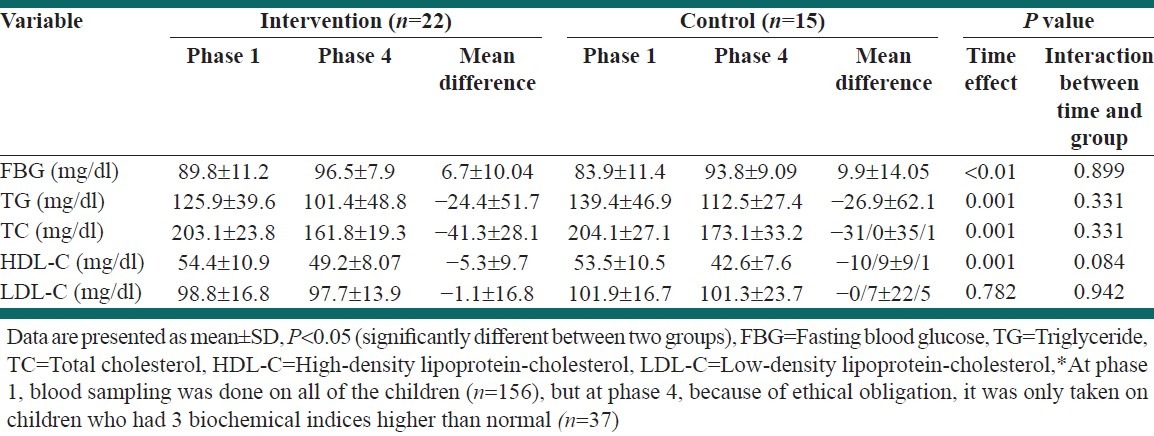
As shown in Table 3, among biochemical indices, although positive trends of TG and cholesterol were observed, interaction between the two groups was not significant.
Table 3.
The trend of biochemical indices of obese children in phases 1 and 4
Evaluation of FFQ showed that consumption of milk and fruit increased significantly in the intervention group (P < 0.05). Consumption of bread and sugar and jam decreased significantly in both groups [Table 4]. In contrast different types of fat and oil decreased significantly in the intervention families rather than in controls (P < 0.05) [Figure 2].
Table 4.
The trend of food consumption (g/day/person) of obese children in 4 phases
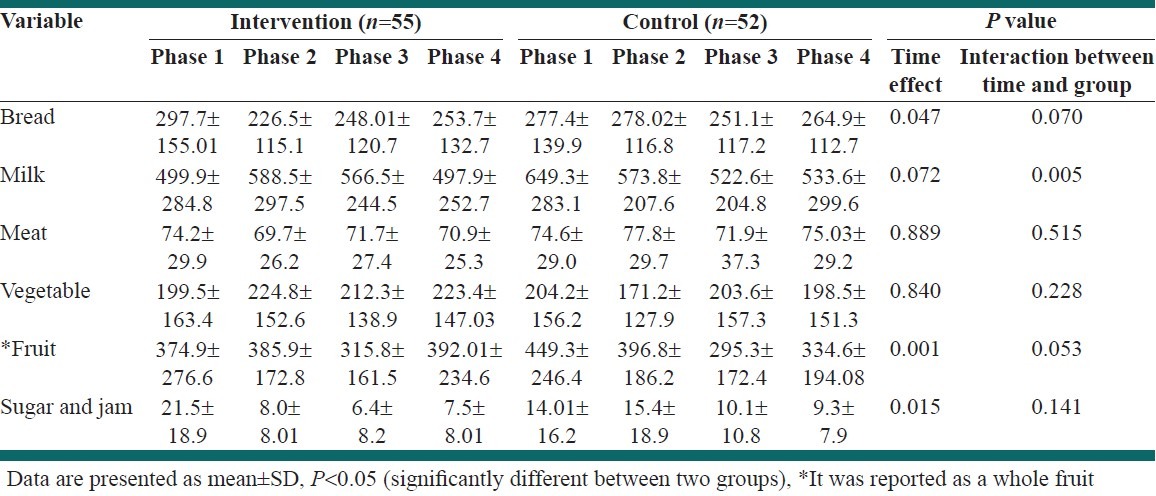
Figure 2.
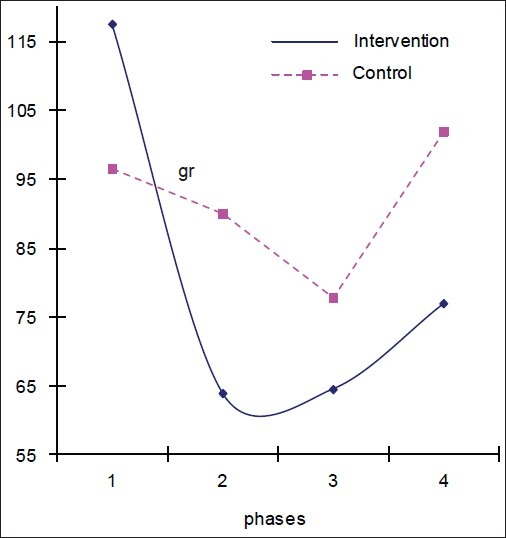
The trend of familys’ fat and oil consumption
DISCUSSION
The results of this family-based intervention for controlling excess weight among young children showed a combination of variables, nutrition behaviors, physical activity and parental involvement as the primary agents of change, and indicated that these can be effective in preventing childhood obesity. In this study, in phases 2 and 3, waist and hip circumferences decreased in the intervention group compared with the control group. However, at the end of the study, these indices and BMI increased. But, this increment was lower in the intervention group than in the control group, like Flodmark et al. study.[29] Family-based studies[30–33] have also shown that the combination of exercise and behavioral modification can be effective for reducing waist circumference and BMI in the intervention group rather than in the control group. The reason of this success was educational program for parents and children with free sport classes and cooperation of school staff. Unlike our results, in another family-based study that was conducted for 2 years, BMI declined significantly in the intervention group.[18]
In this study, children's physical activity increased and sedentary behaviors were managed at close to the standard range.[30] Similarly, after family-based interventions in the Sacher,[31] Epstein,[32] Muller[33] and Robinson[34] studies, children's physical activity was increased and sedentary behaviors decreased by regulating the time of television viewing.
Because the school is the best place for providing an opportunity for education and increased physical activity, and children spend most of their time there, unfortunately, in our schools, the strategies to motivate and increase physical activity in children are powerless. Also, in the hours after school and on holidays, parents were unsupportive and did not have the ability to plan for promoting physical activity because of individual and environmental barriers such as urbanization, lack of safe and easy-access places, family funds, time (working mother, traffic) and pollution, and children had to choose the last option that is watching TV and playing on the computer.[35,36]
It seems that a positive trend was observed toward the intervention group to improvement in blood levels of some biochemical parameters, similar to the Jiang et al.[18] and Nemet et al.[37] studies that showed that total cholesterol and triglyceride were decreased in the intervention group.
In this study, the consumption of dairy products and fruits were increased significantly. In the Faghihi study,[38] the average consumption of milk and dairy group was significantly increased in the intervention group compared with the control group. Sugar and confectionery ingredients’ consumption also decreased relative to the baseline, which reflected the control and management of mothers, although the interaction between the two groups was not significant. Similar to the Epstein,[39] Gortmaker[40] and Sahota[41] studies an improvement in children's dietary habits was shown with increased fruit and vegetable consumption and balancing the intake of foods that contain high sugar. Evaluation of the total consumption of oils and fats group of households showed that it was significantly lower in the intervention group compared with the control group, similar with Armitage,[42] Himes[43] and Caballero[14] studies, which could be representative of the skills and consumption management of mothers.
There are several limitations in this study; first is that the majority of children suffered from severe obesity and thus lifestyle modification could have been more difficult to achieve. Otherwise, parents of the control group were keen to know more about this matter, and we did not see a significant difference between the two groups.
CONCLUSION
The family-based lifestyle program had limited effects on anthropometric and metabolic outcomes of obese children. We suggest that if interventions were performed in longer periods with a teamwork including a dietitian, psychologist, coach and all family members and school staff, weight control and lifestyle modification would have been more efficient. It is obvious that government policy and organization support are also effective ways to decrease childhood obesity and to have a healthy society in the future.
ACKNOWLEDGMENT
The authors would like to acknowledge the Research Council of National Nutrition and Food Technology Research Institute, Faculty of Nutrition Science and Food Technology and Shahid Beheshti University of Medical Sciences for financial support. The authors would also like to thank all parents and children for their valuable help in conducting this study.
Footnotes
Source of Support: National Nutrition and Food Technology Research Institute, Faculty of Nutrition Sciences and Food Technology, Shahid Beheshti University of Medical Sciences (Grant No: 2676)
Conflict of Interest: None declared
REFERENCES
- 1.Dattilo AM, Birch L, Krebs NF, Lake A, Taveras EM, Saavedra JM. Need for early interventions in the prevention of pediatric overweight: A review and upcoming directions. J Obes. 2012;2012:123023. doi: 10.1155/2012/123023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsiros MD, Sinn N, Coates AM, Howe PR, Buckley JD. Treatment of adolescent overweight and obesity. Eur J Pediatr. 2008;167:9–16. doi: 10.1007/s00431-007-0575-z. [DOI] [PubMed] [Google Scholar]
- 3.Karnik S, Kanekar A. Childhood obesity: A global public health crisis. Int J Prev Med. 2012;3:1–7. [PMC free article] [PubMed] [Google Scholar]
- 4.de Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92:1257–64. doi: 10.3945/ajcn.2010.29786. [DOI] [PubMed] [Google Scholar]
- 5.Discigil G, Tekin N, Soylemez A. Obesity in Turkish children and adolescents: Prevalence and non-nutritional correlates in an urban sample. Child Care Health Dev. 2009;35:153–8. doi: 10.1111/j.1365-2214.2008.00919.x. [DOI] [PubMed] [Google Scholar]
- 6.Kelishadi R. Childhood overweight, obesity, and the metabolic syndrome in developing countries. Epidemiol Rev. 2007;29:62–76. doi: 10.1093/epirev/mxm003. [DOI] [PubMed] [Google Scholar]
- 7.Maddah M, Nikooyeh B. Factors associated with overweight in children in Rasht, Iran: Gender, maternal education, skipping breakfast and parental obesity. Public Health Nutr. 2010;13:196–200. doi: 10.1017/S1368980009990589. [DOI] [PubMed] [Google Scholar]
- 8.Mirmiran P, Sherafat-Kazemzadeh R, Jalali-Farahani S, Azizi F. Childhood obesity in the Middle East: A review. East Mediterr Health J. 2010;16:1009–17. [PubMed] [Google Scholar]
- 9.The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304:2042–7. doi: 10.1001/jama.2010.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelishadi R, Ardalan G, Gheiratmand R, Majdzadeh R, Hosseini M, Gouya MM, et al. Thinness, overweight and obesity in a national sample of Iranian children and adolescents: CASPIAN Study. Child Care Health Dev. 2008;34:44–54. doi: 10.1111/j.1365-2214.2007.00744.x. [DOI] [PubMed] [Google Scholar]
- 11.Gaeini A, Kashef M, Samadi A, Fallahi A. Prevalence of underweight, overweight and obesity in preschool children of Tehran, Iran. J Res Med Sci. 2011;16:821–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Inter-relationships among childhood BMI, childhood height, and adult obesity: The Bogalusa Heart Study. Int J Obes Relat Metab Disord. 2004;28:10–6. doi: 10.1038/sj.ijo.0802544. [DOI] [PubMed] [Google Scholar]
- 13.CDC table for calculated body mass index values for selected heights and weights for ages 220 Years. 2000. [Last accessed on 2013 Feb 05]. Available from: http://www.cdc.gov/growthcharts .
- 14.Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T, et al. Pathways: A school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma M. School-based interventions for childhood and adolescent obesity. Obes Rev. 2006;7:261–9. doi: 10.1111/j.1467-789X.2006.00227.x. [DOI] [PubMed] [Google Scholar]
- 16.Dolinsky DH, Armstrong SC, Kinra S. The clinical treatment of childhood obesity. Indian J Pediatr. 2012 doi: 10.1007/s12098-012-0766-0. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Gruber KJ, Haldeman LA. Using the family to combat childhood and adult obesity. Prev Chronic Dis. 2009;6:a106. [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang JX, Xia XL, Greiner T, Lian GL, Rosenqvist U. A two year family based behaviour treatment for obese children. Arch Dis Child. 2005;90:1235–8. doi: 10.1136/adc.2005.071753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krishnamoorthy JS, Hart C, Jelallian E. The epidemic of childhood obesity: Review of research and implications for public policy 2006. Grantmakers for Children, Youth and Families. [Last assessed on 2012 May 25]. Available from: http://www.srcd.org/documents/publications/spr/20-2_childhood_obesity.pdf .
- 20.Sajjadi F, Kelishadi R, Maghroon M, Alikhasi H, Mohammadifard N, Saghafian F, et al. The effect of two nutritional methods in changes of anthropometric indexes in obese parents and their children. Zahedan J Res Med Sci. 2011;13:42–6. [Google Scholar]
- 21.Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13:654–62. doi: 10.1017/S1368980009991698. [DOI] [PubMed] [Google Scholar]
- 22.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: Methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- 23.Rosenbaum M, Leibel RL. The physiology of body weight regulation: Relevance to the etiology of obesity in children. Pediatrics. 1998;101:525–39. [PubMed] [Google Scholar]
- 24.Kelishadi R, Ardalan G, Gheiratmand R, Adeli K, Delavari A, Majdzadeh R, et al. Paediatric metabolic syndrome and associated anthropometric indices: The CASPIAN Study. Acta Paediatr. 2006;95:1625–34. doi: 10.1080/08035250600750072. [DOI] [PubMed] [Google Scholar]
- 25.Azizi F, Esmaillzadeh A, Mirmiran P, Ainy E. Is there an independent association between waist-to-hip ratio and cardiovascular risk factors in overweight and obese women? Int J Cardiol. 2005;101:39–46. doi: 10.1016/j.ijcard.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Mirmiran P, Esmaillzadeh A, Azizi F. Detection of cardiovascular risk factors by anthropometric measures in Tehranian adults: Receiver operating characteristic (ROC) curve analysis. Eur J Clin Nutr. 2004;58:1110–8. doi: 10.1038/sj.ejcn.1601936. [DOI] [PubMed] [Google Scholar]
- 27.Phisical status: The use and interpretation of anthropometry. WHO Technical Report Series 854. Geneva: WHO; 1995. WHO Expert Commitee; pp. 1–439. [PubMed] [Google Scholar]
- 28.Ghaffarpour M, Houshiar-Rad A, Kianfar H. The manual for household measures, cooking yields factors and edible portion of foods. Tehran: Nashre Olume Keshavarzy; 1999. pp. 1–40. [Google Scholar]
- 29.Flodmark CE, Ohlsson T, Rydén O, Sveger T. Prevention of progression to severe obesity in a group of obese schoolchildren treated with family therapy. Pediatrics. 1993;91:880–4. [PubMed] [Google Scholar]
- 30.Committee on communications. Children, adolescents and television. American Academy of Pediatrics. Pediatrics. 1995;96:786–7. [PubMed] [Google Scholar]
- 31.Sacher PM, Kolotourou M, Chadwick PM, Cole TJ, Lawson MS, Lucas A, et al. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity (Silver Spring) 2010;18:S62–8. doi: 10.1038/oby.2009.433. [DOI] [PubMed] [Google Scholar]
- 32.Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162:239–45. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Müller MJ, Danielzik S, Pust S. School-and family-based interventions to prevent overweight in children. Proc Nutr Soc. 2005;64:24954. doi: 10.1079/pns2005424. [DOI] [PubMed] [Google Scholar]
- 34.Robinson TN. Does television cause childhood obesity? JAMA. 1998;279:959–60. doi: 10.1001/jama.279.12.959. [DOI] [PubMed] [Google Scholar]
- 35.Kelishadi R, Ghatrehsamani S, Hosseini M, Mirmoghtadaee P, Mansouri S, Poursafa P. Barriers to Physical Activity in a Population-based Sample of Children and Adolescents in Isfahan, Iran. Int J Prev Med. 2010;1:131–7. [PMC free article] [PubMed] [Google Scholar]
- 36.Gunnarsdottir T, Njardvik U, Olafsdottir AS, Craighead LW, Bjarnason R. The role of parental motivation in family-based treatment for childhood obesity. Obesity (Silver Spring) 2011;19:1654–62. doi: 10.1038/oby.2011.59. [DOI] [PubMed] [Google Scholar]
- 37.Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short-and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics. 2005;115:e443–9. doi: 10.1542/peds.2004-2172. [DOI] [PubMed] [Google Scholar]
- 38.Faghihi A, Anousheh M, Ahmadi F, Ghofranipour Rouchi F. The effect of boy students’ participation on consumtion of milk and dairy products by family in Janah, Hormozgan province. Med J Hormozgan Univ. 2007;10:349–56. [Google Scholar]
- 39.Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes Res. 2001;9:171–8. doi: 10.1038/oby.2001.18. [DOI] [PubMed] [Google Scholar]
- 40.Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–18. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 41.Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH, Cade J. Evaluation of implementation and effect of primary school based intervention to reduce risk factors for obesity. BMJ. 2001;323:1027–9. doi: 10.1136/bmj.323.7320.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Armitage CJ. Evidence that implementation intentions reduce dietary fat intake: A randomized trial. Health Psychol. 2004;23:319–23. doi: 10.1037/0278-6133.23.3.319. [DOI] [PubMed] [Google Scholar]
- 43.Himes JH, Ring K, Gittelsohn J, Cunningham-Sabo L, Weber J, Thompson J, et al. Impact of the pathways intervention on dietary intakes of American Indian schoolchildren. Prev Med. 2003;37:S55–61. doi: 10.1016/j.ypmed.2003.08.003. [DOI] [PubMed] [Google Scholar]


