Abstract
Background:
Estimates of health problems of the elderly in developing countries are required from time to time to predict trends in disease burden and plan health care for the elderly. Developing countries have a poor track record of equitable distribution of health care. Marginalized groups living in urban slums and rural villages have poor penetration of health services.
Aims:
To identify the geriatric health problems in samples drawn from a slum and a village, and also to explore any gender and urban–rural difference morbidity.
Subject and Methods:
A community-based cross-sectional study was carried out by house to house survey of all people aged over 60 years in an urban slum and a village in the field practice area of a teaching hospital. The total elderly population in these two areas was 407, with an almost equal representation from urban slum and rural area. Information (most of them self-reported) was collected in a pre-tested instrument, which has been used earlier in a World Health Organization multicentric study in India. Categorical variables were summarized by percentages. Associations were explored with odds ratio (OR) and 95% confidence intervals (CIs).
Results:
Female elders outnumbered the male elders; widows outnumbered widowers. Tobacco use was very high at 58.97% (240/407). Visual impairment (including uncorrected presbyopia) was the most common handicap with prevalence of 83.29% (339/407), with males more affected than females (OR = 2.52, 95% CI 1.32-4.87). Uncorrected hearing impairment was also common. Urinary complaints were also more common in males (OR = 1.68, 95% CI = 0.93-3.04). More rural elders were living alone than their urban counterpart (OR = 2.87, 95% CI 1.23-6.86). History of weight loss was higher in the rural areas, while tendency to obesity was higher in the urban areas. An appreciable number 29.2% (119/407) had unoperated cataract. Prevalence of hypertension was 30.7% (125/407); 12% (49/407) had diabetes; 7.6% (31/407) gave history of ischemic heart disease, males more than females (OR = 3.75, 95% CI 1.62-8.82). A large proportion, 32.6%, (133/407) had dental problems. Almost half of the population gave history of depression.
Conclusion:
A large number of unmet health needs, such as unoperated cataract, uncontrolled hypertension, uncorrected hearing impairment and tobacco use, exist in marginalized groups. Health interventions for these are needed in developing countries. Preventive services such as tobacco cessation campaigns among the elderly should also get priority.
Keywords: Cross-sectional, Elderly, Geriatric medicine and Asia, Health problems
Introduction
One of the biggest social changes brought about by improved standards of living is population aging. By 2050, older people will outnumber children under the age of 14 years.[1] Vast numbers of older people live in developing countries where health services are not equitably distributed. Moreover, health in old age is associated with health in earlier years of life, from womb to tomb. Intrauterine growth retardation for example increases the risk of diseases of the circulatory system and diabetes in later life.[1] Later in the life cycle, obese children track their risk of developing chronic diseases such as diabetes, circulatory disease, cancer, respiratory and musculo-skeletal disorders right up to old age. Rapidly developing countries with galloping economies are facing both extremes–child malnutrition among the deprived and child obesity among the nouveau riche. This phenomenon will manifest in a higher burden of non-communicable diseases in old age in the coming decades. Repeated cross-sectional surveys among the geriatric population can give an estimate of the future challenges facing geriatric medicine.
Studies in developed countries have identified certain key issues. Tomstad et al.,[2] in their study among older people reported a higher risk of under-nutrition among elders living alone. However, their study had a response rate of only 35.1% among the 450 elderly people approached. Foottit and Anderson[3] in their study on a sample of 325 elders living in the community in Australia found that perceived wellness was influenced by hearing, mobility, memory, chronic disease, exercise, gambling and single status. Harris and Grootjans[4] have suggested an ecological approach to understand the needs of the elderly. Therefore, country-specific studies of health and social problems in the elderly are needed.
Recent studies in India have brought out some of the health and social problems of the aged. However, some had small sample sizes and were limited to only urban areas,[5–7] while others with larger samples were clinic based.[8]
Considering the increasing burden of geriatric health and social problems in India, the World Health Organization (WHO) in collaboration with the Government of India carried out a cross-sectional, community-based study of the elderly population 60 years and above at 10 different sites in different states and union territories of India.[9] Using a structured questionnaire, 1000 subjects with an equal number from rural and urban area were studied at each center. However, although this study had good precision due to the large sample size, the study was representative of the whole population and not specific for any particular section of society.
The present study explored the health problems of the elderly among particular marginalized groups belonging to lower socio-economic status who lived in urban slum and rural areas with a view not only to identify some of the health and social issues peculiar to these underprivileged groups but also to determine whether there is any rural-urban and gender difference.
Subject and Methods
Study site
The study was carried out in both the urban and the rural field practice areas of a medical college in Pune, India. An urban slum was selected in the urban field practice area located at a distance of 3 km from the college and a village was selected in the rural field practice area about 25 km from the college. Both the urban and the rural field practice areas have health centers under administrative and technical control of the Department, with availability of medical officers, paramedical workers, lab technician and medico-social workers who carry out home visits. Besides, interns are attached to these health centers on a rotating basis for internship training in community medicine.
Study design
A community-based cross-sectional study design was used.
Sample size calculation
Sample size calculation was done using software EPI info (WHO/CDC Atlanta). A default prevalence of morbidity at 50% was taken with worst possible estimate at 45% on one side and 95% confidence interval. Using these inputs, the sample size calculated was 384 subjects.
Selection of study subjects
It was decided to select the slum (with a population of 12,000) nearest to the urban health center for survey in the urban area. In the rural area, Markal village (population 5000) nearest to the rural health center was selected for the survey. House to house survey was carried out of all the eligible elderly population (above 60 years). In case the sample size could not be met, it was decided beforehand, to extend the survey to the adjacent slum/village. However, survey of one slum and one village, respectively, yielded more than the required number of study subjects, i.e., 407 (203 in urban area and 204 in rural areas).
Study instrument
The tool for data collection used was developed by the WHO for study of health status of elderly people in a multicenter study in India.[9] The same was adapted in the present study after some adaptations after a pilot study.
Pilot study
A pilot study was carried out over a period of 1 month. Data was collected from 50 subjects. Difficulties in data collection and ambiguities in the questionnaire were resolved. Modifications in the study instrument were done as indicated by the pilot study. The data of the pilot study were not included in the final analysis.
Data collection
Data were collected by house to house survey. All people of both genders over 60 years of age staying in the selected slum/village were interviewed after informed consent. In case of any difficulty in communication with the elder, help of other family members was taken. Presence of morbidity was elicited by self-reporting, supplemented by history, clinical examination and scrutiny of relevant medical documents, if present. Respondents newly detected with any medical condition were taken to the respective health center run by the college for free medical care. For those requiring specialized treatment, arrangements for their follow-up were made at the medical college.
Data entry and statistical analysis
Data were entered in a Microsoft Excel file and statistical analysis was done using Epi Info 2002 (WHO/CDC). Categorical variables were summarized by proportions and percentages. Association between categorical variables was explored by Chi square and odds ratio (OR) with 95% confidence intervals (CIs) where applicable. Continuous variables were summarized by mean and standard deviation (SD), and association tested by parametric tests.
Ethical issues
Ethical clearance from the institutional ethics committee was obtained before conducting the study. Besides, informed consent was taken from each study participant.
Results
Urban-rural difference in prevalence of elderly
A survey of 12,000 people in the urban slum yielded 203 elderly individuals over the age of 60 years, giving a prevalence of 1.69% (203/12000). While in the village, 204 out of the 5000 people surveyed were over 60 years, giving a proportion of elderly more than twice, 4.06% (204/5000) in the rural area compared with the urban slum.
Gender
Of the total of 407 elders surveyed in the slum and village, 38.33% (156/407) were males and 61.67% (252/407) were females. There was no difference in gender distribution of the elderly surveyed between the rural and urban subjects. The proportion of females among the elderly population was 61.76% (126/204) in the rural area and 61.57% (125/203) in the urban area.
Age distribution
The overall mean age in elderly females was 68.68 years (SD 8.3 years), and in males it was 70.1 years (SD 7.3 years). The combined average of all elderly was 69.2 years (SD 8.04 years). The maximum age among females was 110 years, while for males it was 94 years. The mean age of the rural population was 70.5 years (SD 8.3 years), while that of the urban population was 67.9 years (SD 7.5 years). Majority of the elderly, 56.01% (228/407) were in the age group of 60–69 years, i.e. in the category of “young – old.”
Religion
Hindus constituted 79.6% (324/407), Buddhist 17.2% (70/407), Muslims 2% (8/407) and Christian 1.5% (5/407) of the population.
Educational status
Among the total elderly, 42.8% (174/407) were illiterate, 38.1% (155/407) had received primary education,17.2% (70/407) had received secondary education while only 1.9% (8/407) had received education up to the graduate level. The proportion of illiterates was much more among females 52.6% (132/251) as compared with males 26.9% (42/156), which was statistically significant (OR = 3.01, 95% CI 1.91-4.75). Similarly, rural illiteracy was higher 51.96% (106/204) than urban illiteracy33.5% ((68/203) (OR = 2.15, 95% CI 1.41-3.27).
Marital status
Of all the elderly surveyed in the rural and urban areas, 51.1% (208/407) were married at the time of the survey. The percentage of those currently married (with living spouse) was higher in males, 75% (117/156) than in females, 36.2% (91/251), which was statistically significant (OR = 5.27, 95% CI 3.31-8.44). There were a higher number of female widows, 60.2% (151/251) than male widowers, 20.5% (32/156).
Living arrangements
In the survey, it was found that 96.31% (392/407) of the elders lived with their spouse and/or their children, while 8.1% (33/407) lived alone. Proportion living alone was more in rural areas 11.76% (24/204) compared with urban areas, 4.43% (9/203), which was statistically significant (OR = 2.87, 95% CI 1.23-6.86).
Occupation
Of the total elders in the study, 253/407 (45.7%) were not working, nor drawing any pension, while 80/407 (19.6%) were pensioners, 74/407 (17.3%) were employed mostly as in odd jobs.
Socioeconomic status
Majority of the old population, 45.6% (185/407), belonged to the lower socioeconomic status (Class IV); 22.7% (92/407) belonged to Class III; 25.9% (106/407) belonged to Class V; while only 0.5% (2/407) and 5.4% (22/407) of the elderly belonged to Class I and Class II, respectively.
Addictions
Tobacco use
Among the selected sample, 58.97% (240/407) were using some or the other form of tobacco. Prevalence was 55.38% (139/251)in females and 64.74% (101/156) in males. More than half of the tobacco users were addicted to tobacco chewing in various forms. There was no urban rural difference in tobacco use habit.
Alcohol use
This had a very low prevalence-only 2.7% (11/407) of the study sample took alcohol.
Visual impairment
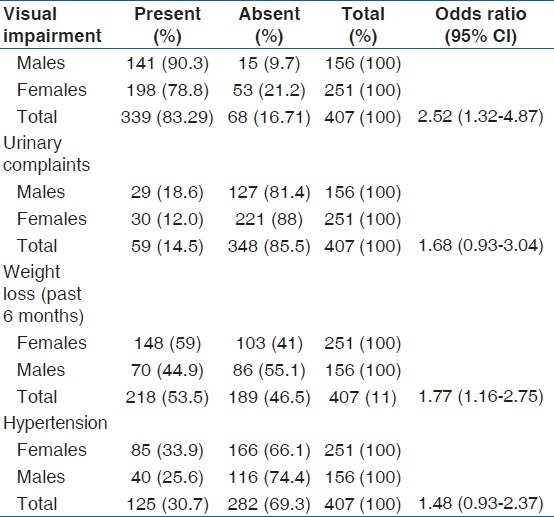
This was common. Of the 407 subjects, 339 (83.29%) had visual impairment. Overall, visual impairment was significantly higher in males than in females (OR = 2.52, 95% CI 1.32-4.87) [Table 1]. There was no urban rural difference.
Table 1.
Association between gender and morbidity
Hearing impairment
Self-reported hearing impairment was 63.1%, (257/407) with no appreciable urban rural difference. Males had a higher proportion of hearing impairment, 65.4% (102/156) compared with females, 61.8% (155/251), which was statistically not significant. In spite of the high prevalence of hearing loss, use of hearing aids was very low–only 1.47% (6/257) of the hearing impaired were using a hearing aid.
Urinary problems
Overall, 14.5% (59/407) of the elderly had urinary symptoms. Males had higher self-reported urinary problems18.6% (29/156) compared with females 12.0% (30/251) [Table 1].
Weight loss
A total of 53.6% (218/407) elderly reported weight loss in the last 6 months. Female elderly had a higher rate of weight loss, 59% (148/251) compared with males, 44.9% (70/156) [Table 1]. Rural elderly had a high percentage, 58.82% (120/204) as compared with the urban elderly population, 48.27% (98/203) [Table 2]. These differences were statistically significant.
Table 2.
Rural urban difference in morbidity
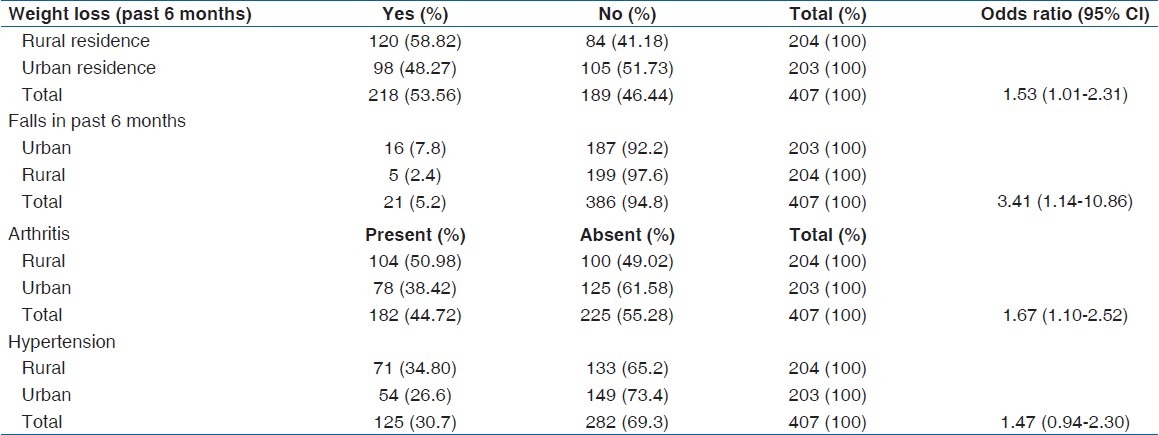
Falls
In the study sample, 5.2% (21/407) reported history of falls in the last 6 months. The incidence of falls was almost three times higher in urban areas 7.8% (16/203) as compared with rural areas, 2.4% (5/204), OR = 3.41, 95% CI 1.14–10.86 [Table 2].
Body mass index
Of all the elderly examined, 20.4% (83/407) had Body mass index (BMI) below 18.5, while 26.1% (106/407) had BMI above 25. The percentage of lower BMI was higher in rural (22.8%, 47/204) than in urban areas (17.7%, 36/203). More males (21.1%, 33/156) had lower BMI than females (19.9%, 50/251). Overweight/obesity was higher in the urban areas, with more than 31.2% (63/203) having BMI above 25 compared with the rural area, where 20.8% (43/204) had BMI over 25 (P < 0.01). Gender-wise overweight/obesity was more common in females, 27.8% (70/251) than in males, 23.12% (36/156).
Depression
Self-reported history of depression was 52.3% (213/407). Higher prevalence of depression was observed in the urban (56.6%, 114/203) than in the rural elderly population (48.0%, 98/204), which was statistically significant. The highest prevalence of self-reported depression was noted in the urban female elderly, 84/125 and rural male elderly, 52/78 (67.2% in each); it was lowest in urban males (39.7%, 31/78) and in between in rural females (54.8%, 69/126).
Anemia
This had a high prevalence –49.6% (202/407). It was higher in the rural elderly (60.7%, 124/204) as compared with the urban elderly (38.4%, 78/203); it was higher in females (56.6%, 142/251) than in males (38.5%, 60/156).
Arthritis
Overall, 44.7% (182/407) of the elderly population was found to suffer from arthritis, which was more prevalent in the rural (50.98%, 104/204) than in the urban areas (38.42%,78/203). This difference was statistically significant [Table 2].
Hypertension
The prevalence of known hypertension was reported in 125/407 (30.7%) of the total study population. This prevalence was higher in females compared with males, the difference missing statistical significance marginally [Table 1]. It was higher in the rural elderly population (34.8%, 71/204) than in the urban elderly population (26.6%, 54/203)–the difference again missing statistical significance marginally [Table 2].
Dental problems
One hundred and thirty-three (32.6%, 133/407) of the elderly were having dental problems. The percentage was higher in the urban area (38.4%, 78/203) compared with the rural area (27%, 55/204). There was no appreciable male female difference.
Cataract
Eighty-nine (29.2%, 89/407) elderly had cataract. The prevalence of cataract was higher in the urban area (25.12%, 51/203) compared with the rural area (18.6%, 38/204). There was no difference in prevalence between males and females.
Diabetes
Among those interviewed, 12% (49/407) reported having diabetes. The prevalence of self-reported diabetes mellitus was higher among the urban elderly population (15.7%, 32/203) than among the rural elderly (8.3%, 17/204), which was statistically significant (OR = 2.06, 95% CI 1.06–4.03). There was no appreciable difference between the genders.
Ischemic heart disease
In the present study, 7.6% (31/407) of the elderly population reported Ischemic Heart Disease (IHD). More males (13.5%, 21/156) reported history of IHD compared with females (4.0%, 10/251). The difference was statistically significant (OR = 3.75, 95% CI 1.62-8.82). A higher proportion of urban elders (9.8%, 20/203) suffered from IHD compared with their rural counterpart (5.4%, 11/204).
Asthma
History of asthma was given by 5.9% (24/407) of the study subjects, being more prevalent in the rural elderly (6.37%, 13/204) than in the urban elderly (5.4%, 11/203)–there was no appreciable difference between the genders.
Malignancy
In the survey, 1.71% (7/407) of the elderly were known cases of malignancy. The prevalence of malignancy was higher in the urban elderly (2.46%, 5/203) than in the rural elderly (0.98%, 2/204)–more females (1.99%, 5/251) gave history of malignancy compared with males (1.28%, 2/156). However, the absolute number of cases was very few in the sample for any conclusions.
Parkinson's disease
This was present in 1.5% (6/407) of the study population, more in the rural (1.96%, 4/204) than in the urban (0.9%, 2/203) elderly. There was no appreciable gender difference.
Paralytic attack
In the study sample, 3.19% (13/407) had reported an episode of paralytic attack, with no appreciable rural urban difference. Among males, a higher proportion (5.1%, 8/156) reported stroke than females (1.9%, 5/251).
Discussion
Rapid urbanization leads to more elderly people being left behind to fend for themselves in rural areas when the young migrate to the city in search of greener pastures. This is reflected in the higher proportion of elderly in the rural area compared with the urban area, and also higher mean age of the rural elderly as brought out in the present study.
The higher rural illiteracy coupled with a higher mean age of the rural elderly add to the challenge of geriatric health issues in this group, as literacy has a positive impact on overall health. Similarly, the higher rate of widows compared with widowers, one of the findings of the present study, has potential to adversely affect the health of elderly women, as women in the Indian culture (particularly of the past generation) are heavily dependent for emotional and social support on their husbands. An appreciable number not employed or drawing pension, thus not being economically independent, increases the burden of dependency. The WHO study[9] carried out at 10 sites all over India, covering 10,035 individuals over 60 years of age from rural and urban areas, indicated that widows, particularly in rural areas, outnumbered widowers.
Living alone, which can be taken as a surrogate measure of loneliness, was higher in the rural area (11.76%) compared with the urban area (4.43%). This may be due to reverse migration of elders from urban to rural areas, after they lose their jobs due to age. Loneliness can be a strong risk factor for undernutrition among older people.[2] This may perhaps be the reason for the higher prevalence of weight loss and anemia in the rural elderly compared with the urban elderly in the present study.
The higher tobacco use in the present study should be a cause of concern. Tobacco habits take shape in adolescence and early adulthood, and tend to continue into old age. Anti-tobacco campaigns are of relatively recent onset, and may have missed out the present elderly when they were adolescents/young adults. The prevalence of tobacco use in the elderly in the present study is much higher than in other studies.[7,9] This lifestyle factor puts the elderly at greater risk for most non-communicable diseases. Tobacco cessation campaigns among the elderly should be worthwhile, because tobacco cessation is beneficial in chronic users also. It has been reported that even people who quit past 60 years of age live longer than those who continue to smoke.[10]
We observed a very high prevalence of visual impairment (83.29%) in our study population, even higher that that found in the WHO multicentric study, which reported poor vision in 45.4% in the elderly. In our study, the problem with near vision due to uncorrected presbyopia was also included as visual impairment, which may have contributed to the high prevalence of visual impairment. More than a quarter of the surveyed also had unoperated cataract, adding to the burden of visual impairment. In many developing countries like India, there is only one eye specialist for a million population.[11] Increasingly, therefore, health care leans on the use of auxiliary health personnel to fill the deficiency. In India, this gap is filled by village health guides, ophthalmic assistants (who can prescribe spectacles for refractive errors and presbyopia), multipurpose workers and voluntary agencies. Secondary eye care involves definitive management of common blinding conditions such as cataract, which accounts for 62.6% of blindness in India.[12] The eye camp approach to make cataract surgery available has been highly successful, and has received wide popular support. Apart from cataract surgery, these camps undertake general health surveys for the early detection of visual defects as well as the education of the masses. It seems from the study findings that in the surveyed areas, such services have not made much impact.
Hearing problems were almost three times higher in the present study sample than that reported by the WHO multicentric study.[9] Only 1.47% of the hearing impaired used hearing aid. There is need for evaluation and management of hearing problems among the elderly.
Prevalence of urinary problems (14.5%) was identical to the findings of the WHO multicentric study.[9] The higher prevalence in urinary problems in males, also reported in earlier studies,[9] is likely to be due to the presence of benign prostatic hypertrophy.
Falls and fractures are common geriatric problems. We found a higher prevalence of falls in the urban area, while the WHO study reported a higher prevalence in rural areas. Fall prevention measures, which include correction of visual and hearing impairments, are indicated in the elderly.
While percentage of aged with abnormally low BMI was higher in rural areas, indicating malnutrition, overweight/obesity was higher in the urban area, indicating impact of urbanization and sedentary lifestyle even in the elderly. Sedentary lifestyle with associated obesity will increase the incidence of many non-communicable diseases in the elderly, such as coronary heart disease, diabetes and osteoarthritis. In our study, this is reflected by higher prevalence of coronary heart disease and diabetes in urban elders compared with rural elders. The higher prevalence of malignancy in the urban population compared with the rural population may be due to the combined effect of lifestyle and environmental factors. Other non-communicable diseases such as asthma, Parkinson's disease and stroke did not show any urban–rural difference.
Self-reported depression caused significant morbidity in the elderly. More than half of the elderly reported feelings of depression in the past 6 months. Mental health care and psychological rehabilitation should be part of health care of the elderly.
Dental problems is a common accompaniment of ageing and, in India, a largely unmet one. Remote areas lack dental health personnel. While planning health care for the elderly, dental component should also be considered.
The study has the following limitations
Sample size: This was calculated for only estimating the prevalence of morbidity. The sample size calculation was not done to elicit various associations. These were done only as exploratory exercises. A larger sample size would be required to establish these associations adequately. Therefore, most of the deductions are more speculative than empirical.
Selection of study sample: The slum/village nearest to the respective health centers in urban and rural areas was chosen for the survey. This may have some amount of selection bias in the sample. Slum/village nearest to the health center may have more access to health services, and their morbidity may be less compared with more remote slums or villages. This may, to some extent, limit external validity of the study.
Measurement errors in detection of morbidity: As this was a house to house survey, most morbidity was elicited by simple questions, self-reporting and clinical examination, without confirmation by sophisticated laboratory tests or other costly investigations. This may underestimate the morbidity because early or subclinical cases may be missed. This may have affected the internal validity of the study. Morbidity may have been underestimated.
Conclusion
In spite of the above limitations, the study has established that overall morbidity was high among the study population, with non-communicable and degenerative diseases comprising the major burden of disease. Hearing and visual impairments (mostly correctable) were high. There is much scope for behavior change communication for lifestyle factors such as tobacco use, which was found to be high in the study sample.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.WHO. World Health Day–toolkit for organizers. [Last cited on 2012]. Available from: http://www.who.int/world.health.day/2012/toolkit/background/en/index.html .
- 2.Tomstad ST, Soderhamn U, Espenes GA, Soderhamn O. Living alone, receiving help, helplessness, and inactivity are strongly related to risk of undernutrition among older home-dwelling people. Int J Gen Med. 2012;5:231–40. doi: 10.2147/IJGM.S28507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foottit J, Anderson D. Association between perception of wellness and health-related quality of life, co-morbidities, modifiable lifestyle factors and demographics in older Australians. Australas J Ageing. 2012;31:22–7. doi: 10.1111/j.1741-6612.2011.00526.x. [DOI] [PubMed] [Google Scholar]
- 4.Harris N, Grootjans J. The application of ecological thinking to better understand the needs of communities of older people. Australas J Ageing. 2012;31:17–21. doi: 10.1111/j.1741-6612.2010.00501.x. [DOI] [PubMed] [Google Scholar]
- 5.Pandve HT, Deshmukh P. Health survey among elderly population residing in an urban slum of Pune city. [Last accessed on 2012 Sep 07];J Indian Acad Geriatr. 2010 6:5–8. Available from: http://www.jiag.org/march2010/1.pdf . [Google Scholar]
- 6.Bhatia SP, Swami HM, Thakur JS, Bhatia V. A study of health problems and loneliness among the elderly in Chandigarh. [Last accessed on 2012 Sep 07];Indian J Community Med. 2007 32:255–8. Available from: http://www.ijcm.org.in/text.asp?2007/32/4/255/37689 . [Google Scholar]
- 7.Prakash R, Choudhury SK, Singh US. A Study of morbidity pattern among geriatric populaton in an urban area of Udaipur Rajasthan. [Last accessed on 2012 Sep 07];Indian J Community Med. 2004 29:35–40. Available from: http://www.ijcm.org.in/temp/IndianJCommunityMed29135.1484378_040723.pdf . [Google Scholar]
- 8.Lena A, Ashok K, Padma M, Kamath V, Kamath A. Health and social problems of the elderly: A cross sectional study in Udupi taluk, Karnatka. Indian J Community Med. 2009;34:131–4. doi: 10.4103/0970-0218.51236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization Collaborative Programme supported by the Government of India. Multicentric study to establish epidemiological data on health problems in elderly. [Last cited on 2007]. Available from: http://www.whoindia.org/LinkFiles/Health_Care_for_the_Elderly_Multicentric_study_healthcareelderly_exe.pdf .
- 10.Doll R, Peto R, Borcham J, Sutherland I. Mortality in relation to smoking: 50 years’ observation on male British doctors. BMJ. 2004;328:1519–27. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park K. Park's text book of preventive and social medicine. 21st ed. Jabalpur, India: M/S Banarsidas Bhanot; 2011. Blindness; pp. 370–4. [Google Scholar]
- 12.Park K. Visual Impairment and Blindness. In: Park K, editor. Park's textbook of preventive and social medicine. 22nd edition. Jabalpur, India: Banarsidas Bhanot; 2013. pp. 371–4. [Google Scholar]


