Abstract
Background:
‘Mai suya’ is a common job in the most northern Nigeria in which there is significant exposures to wood smoke and oil fumes. The respiratory impact of these dual exposures on workers engaged in this work has not been previously documented, hence this study was carried out.
Aim:
The aim is to study the prevalence, patterns and respiratory function assessment among this group.
Subject and Methods:
This is a case controlled study involving mai suya and workers who are not exposed to wood smoke and oil fumes in an occupational setting. All consenting mai suya and matched controls were recruited. Both groups underwent an interviewer administered questionnaire followed by on spot spirometric test measuring forced expiratory volume in one second (FEV1), forced vital capacity (FVC), peak expiratory flow rate (PEFR). Results are presented using descriptive statistics. Chi square was used to test for association between respiratory symptoms and the job categories. Student's t-test was used to compare values of continuous variables. Odd ratios were determined for the risk of respiratory symptoms and exposure to wood smoke and oil fumes.
Results:
Both groups are similar in their demographic characters except in their smoking status, so current smokers were excluded from further analysis. The test group had significantly increased occurrence of chest tightness: 59% (19/32), nasal congestion: 37% (12/32), cough: 32% (10/32), and wheeze: 12% (4/32) compared with the control group, odds ratio (OR) 3.1, 95% confidence interval CI (0.1-5.8), P value 0.04, OR 1.2,95% CI (1.04-1.8), P value = 0.02, OR 0.9 95% CI (0.9-1.4), P value = 0.3, and OR 1.2,95% CI (1-1.3), P value = 0.04, respectively. Occurrences of some respiratory symptoms were associated with duration on the job, while a positive family history of asthma is not associated with increased occurrence of symptoms. The mean (SD) FEV1 and FVC were significantly lower among the test group compared with the control group; 2.5L/s (0.55) versus 3.02L/s (0.51), P value = 0.007 and 2.7L (0.7) versus 3.16L (0.51), P value = 0.04.
Conclusion:
Mai suya’ have increased risk of respiratory symptoms and altered pulmonary functions. There is a need for protective equipment and periodic evaluation.
Keywords: Function, Mai suya, Oil fumes, Pulmonary
Introduction
Domestic and industrial exposure to wood smoke and oil fumes occurs commonly and is associated with possible risk of harmful effects. Wood smoke and cooking oil fumes is a complex mixture of substances.[1] Both contains toxic products as well as carcinogens such as aldehydes, alkanoic, polycyclic aromatic hydrocarbons, and others.[1–3] Wood smoke also contain other substances such as benzopyrenes, phenols, and oxides of nitrogen and sulphur.[4] These products can cause significant airways irritation and are also carcinogenic.[3–7] Therefore, individuals exposed to these two emissions are more likely to have increased risk and occurrence of both respiratory and nonrespiratory diseases.
In northern Nigeria, a very common and important aspect of economic and social life is the roasting of fresh meat by men. These men are popularly called mai suya.
Fresh meats are salted and are roasted by heat from burning wood. The meat is turned periodically and cooking oil added. These procedures generate a lot of toxic fumes from the oil and smoke from the wood. Rodolfo, et al. and Erhabor, et al. have documented the occurrence of obstructive airways disease among women exposed to wood smoke in Bogota and Ife respectively.[8,9] Even short-term exposure to wood smoke has been associated with increased risk of respiratory symptoms and decreased lung function in an experimental setting.[10] Simpson, et al. reported a case study of a young nonsmoking man who developed chronic airflow limitation after inhalation of overheated cooking oil fumes.[11]
Though some works have been done to assess respiratory symptoms and ventilatory functions in some population group but none has been done among this significant group in the society.[12–15] This is an age long job for which the Northern part of the country is known for. Because of its wide acceptability even among other ethnic groups in Nigeria, there are increasing selling points in other parts of the country.
In this study, we aim to study the prevalence of respiratory symptoms and lung function abnormalities among these workers who are exposed to smoke from burning wood, meat and fumes emanating from cooking oil. We hypothesized that there is no difference in respiratory symptoms and lung function parameters between mai suya and other workers who are not so exposed. It is envisaged that the results of this study will provide baseline data for personal health control measures, especially regarding wood smoke and cooking oil fumes and subsequent evaluation of any intervention measure.
Subject and Methods
The study was carried out in Kebbi, Kebbi State Nigeria. This is one of the States in the Northern Nigeria inhabited by various tribes, predominantly the Hausas and Fulanis. Apart from cow rearing, other major occupation of the men folk is selling roasted meat, called suya. Consent of the Director of Clinical Services, Federal Medical Center, Kebbi was obtained for the study as there was no Ethical Committee in the hospital at the time of conducting the study. We also discussed with the chairman of the mai suya and community leaders in the locality, who assisted in disseminating the information, on the aims and possible benefits of the study.
We recruited all consecutive and consenting mai suya who are currently engaged in the work and who is not incapacitated in any way. However any worker who has been treated for tuberculosis, or who is a known patients with asthma were not to be excluded. They were taken through an interviewer administered questionnaire which seeks to evaluate for respiratory symptoms.
The questionnaire contained some items from the Medical Research Council (MRC) Chronic respiratory questionnaire.[16]
Lung function was done with a portable office spirometer GP MS07 Gold standard transducer spirometer (Micro Medical limited, Rochester, Kent, UK). This was continuously calibrated and correcting factor used in the final results. The following parameters were measured, forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and peak expiratory flow rate (PEFR). Consented workers underwent an interviewer administered questionnaire followed by spirometric test. Some of the workers were evaluated at their stalls in the evening.
The interviewers were recruited from the pool of Health assistant at the Federal Medical Center, Kebbi after undergoing some periods of training while the spirometry was performed by a Physician. Controls were age and sex-matched individuals whose works did not entail exposure to fumes or smokes. They must also not have worked as a mai suya before or in any other job with exposure to wood smoke or oil fumes. Overall, 48 mai suya were recruited from 15 different selling points, at two local communities in Kebbi.
Statistical analysis
We performed a descriptive statistics for the sociodemographic characteristics and frequency of respiratory symptoms among both the workers and the control. Because of the cofounding effect of smoking on respiratory tract and because the two groups were significantly different in their smoking status, current smokers were excluded from further analysis. Chi square was used to test for association between respiratory symptoms and the job categories. Odd ratio was used to determine the risk of respiratory symptoms in exposed workers. Student's t-test was used to test for association between the means of numerical variables such as age, PEFR, FVC, and FEV1 values. The analysis was done using SPSS version 12 (SPSS Inc., Chicago, Illinois, USA), with significant level at <0.05.
Results
Study characteristics
The sociodemographic and some other characteristics of the study subjects is as shown in Table 1. The two groups were identical in age, marital status, and gender. They were all male. The mean for the test group, i.e., ‘Mai suya’ was 30.44 (6.7) versus 29.17 (9.7) years for the control, P value = 0.5. Six percent (3/48) of the test group and 12% (4/32) of the control group reported a positive family history of asthma, P value = 0.3. However, none among the study participants has ever been diagnosed with asthma.
Table 1.
Characteristic of study subjects
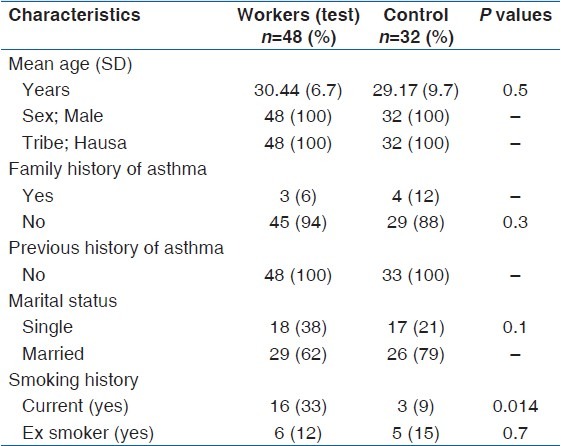
They were however statistically different in their smoking history with 33% (16/48) and 9% (3/32) of the test and control groups being current smokers respectively, P value = 0.014 [Table 1].
Prevalence of respiratory symptoms among study participants
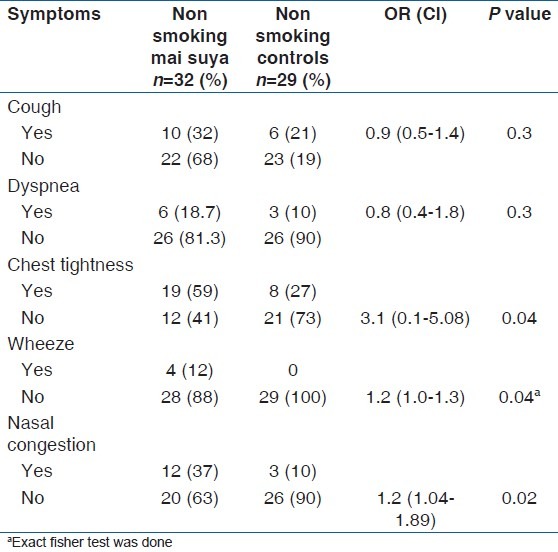
The self-reported prevalences of respiratory symptoms were analyzed among the study participants. In order to eliminate the confounding effect of smoking as the groups were significantly different in their smoking status and giving the effect of smoking on respiratory tract, only participants who were not current smokers were included in this analysis as shown in Table 2. The commonest/most frequently reported symptoms was cough, it was present in 59% (19/32) of the test group and 27% (8/29) of the control, odds ratio; 3.1, 95% CI (0.1–5.8), P value = 0.04. Thirty seven percent (12/32) of the Mai Suyas’ reported nasal congestion compared with 10% (3/29) of the control, odds ratio; 1.2, 95% CI (1.04-1.82), P value = 0.02. Cough was reported in 32% (10/32) and 21% (6/29) of the test and control, respectively, but this was not statistically significant, P value = 0.3. Eighteen percent (6/32) of the Mai Suyas and 10% (3/29) of the control reported dyspnea, P value = 0.3. However, none of the control reported any occurrence of wheeze while 12% (4/32) of the Mai Suyas’ reported wheeze, P value = 0.04.
Table 2.
Prevalence of respiratory symptoms among nonsmokers
Analysis of the association between respiratory symptoms mai suyas
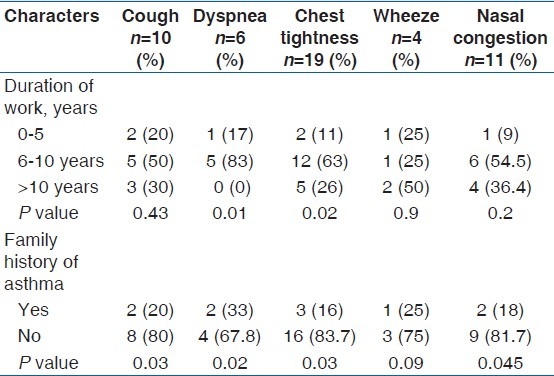
The association between respiratory symptoms among mai suyas who are non smokers was also apparent in the trend analysis as shown in Table 3. Dyspnoea and chest tightness were significantly associated with number of years at work. Individuals who have been engaged in the job for between 6 and 10 years have the highest frequency of dyspnea and chest tightness, 83% (5) and 63% (12/19), P values = 0.01 and 0.02, respectively. Though wheeze was associated with those who have worked for 10 years and above, 50% (2/4) versus 25% (1/4) each for others, P value = 0.9. Individuals with no known family history of asthma had increased association and occurrence of cough; 80% (8/10), dyspnea; 67.8% (4/6), Chest tightness; 83.7% (16/19) and nasal congestion; 81% (9/11).
Table 3.
Factors associated with respiratory symptoms among non smoking Mai suyas
Spirometric study the subjects
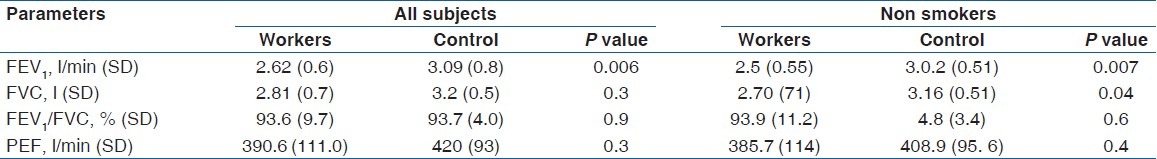
Table 4 shows the lung function results of study subjects. As shown, the mean FEV1 (L/s) was significantly lower among the test group compared with the control group irrespective of the smoking status, 2.62 (0.6) vs. 3.09 (0.8), P value = 0.006 and 2.5 (0.55) and 3.02 (0.51) among nonsmokers, P value = 0.007. However, the mean FVC (L) was significantly lower among Mai suyas who are not smoking compared with nonsmoking control, 2.7 (0.7) and 3.16 (0.51), respectively, P value = 0.004.
Table 4.
Lung function results among study subjects
Discussion
This study looks at the respiratory symptoms and function among Mai Suyas’ which could be described as a form a traditional barbecues workers whose main job is to roast fresh meat in the open. This is also an age long means of meat preserving apart from the use as a delicacies. These individuals are usually exposed to a mixture of wood smoke and fumes from oils or other additives to the meat.
From this study, these workers have increased frequency of respiratory symptoms compared with control. Occurrence of respiratory symptoms especially chest tightness and dyspnea are common among those who have spent 6-10 years on the job compared with wheeze which was present in those with 10 years and more on the job. Positive family history of asthma is not associated with increased occurrence and incidence of respiratory symptoms. Spirometric values were significantly lower among them compared with controls irrespective of the smoking status.
The commonest symptoms were chest tightness, nasal congestion and cough, with a frequency of 59%, 37%, and 32%, respectively. The frequency of chest tightness in this study was higher than previously reported findings among people exposed to only wood dust or wood smokes and detergent workers.[14,15] Because the test group and control were significantly different in their smoking status, we compared the prevalence of these symptoms among non smokers in both groups. Our findings revealed that Mai suyas have up to threefold risk of having chest tightness and about one half risk of having wheeze and nasal congestion. Interestingly, cough and dyspnea were not significantly different among non smoking workers and controls. We also found that those with no known family history of asthma, which may be a marker of pre-existing atopy in these workers also have increased occurrence of respiratory symptoms. All these findings are indicative of significant occurrence and risk of respiratory symptoms among these workers which is not accounted for by smoking cigarette and previous history of atopy or allergy.
It may, therefore, suggested that smokes from burning wood, fumes from oil, and other additives may be strong airway irritants which may act alone or with other factors to increase the occurrence of respiratory symptoms.[10] Additional often unrecognized cofactors such as dust and fumes from car exhaust which these workers may be exposed to may increase the occurrence of respiratory symptoms, as they commonly operates by the road side and popular junctions.
Other possible pathogenic mechanism is the occurrence of airway inflammation and subsequent development of bronchial hyperactivity.[17] Respiratory symptoms distributions were quite varied based on duration of job exposure. Medium term workers; i.e., those working for between 6 and 10 years seems to have the highest frequency of the symptoms. These are probably subjects who have settled down with the job and are doing it more regularly than others. This observation may also be explained in part by the fact that affected individuals may have resigned from the job due to disability. Regarding chest tightness, it was common among those working for more than ten years compared with those working for less than six years. This may really be indicative of development of bronchial hypersensitivity and atopy as result persistent exposure to toxic substances emanating from combustion of wood burning and oil fumes which eventually lead to obstructive airway disease.
Exposure to oil fumes and biomass smoke in these workers is associated with significant reduction in FEV1 and FVC after controlling for smoking. In non smokers, the spirometric results suggest mainly variable degree of airways obstruction. There is a possibility of some workers having a mixed spirometric abnormality as well evidenced by markedly reduced FVC. Other workers have documented obstructive airway disease (OAD) in both acute and chronic exposure to wood smoke and fumes from oil.[6,8,10]
Some limitations of the present study must be highlighted. This was an interviewer administered cross sectional study which may be subjected to error in interpretation of terms by the interviewer and also subject to accurate recall by the subjects. Also ability to accurately describe some of the symptoms to the participants may also affect their response. The interviewers were Health assistants that usually offered assistance, for example in interpreting for Physicians, as their normal and routine work. Additionally, initial training and explanation of terms were undertaken. So these may minimize problems due to interviewing the individuals. However, questionnaire based approach is mostly used tool in even asthma survey, though video based questionnaire is being encouraged especially in children.[18] Portable spirometer was used, though we did not think this should affect the result as it was calibrated, the best reading of three was recorded and a correcting factor used. Reversibility testing may have added additional information to the finding but was abandoned as most subjects were not willing to inhale bronchodilator.
Despite these limitations, this study shows that Mai suyas have increased frequencies and risk of respiratory problems and reduced spirometric parameters. Enlightenment through their society is necessary in order to devise and encourage use of in expensive protective devices.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Naeher LP, Brauer M, Lipsett M, Zelikoff JT, Simpson CD, Koenig JQ, et al. Wood smoke health effects: A review. Inhal Toxicol. 2007;19:67–106. doi: 10.1080/08958370600985875. [DOI] [PubMed] [Google Scholar]
- 2.Jensen LK, Larsen A, Molhave L, Hansen MK, Knudsen B. Health evaluation of volatile organic compound (VOC) emissions from wood and wood based-materials. Arch Environ Health. 2001;56:419–32. doi: 10.1080/00039890109604477. [DOI] [PubMed] [Google Scholar]
- 3.Li S, Pan D, Wang G. Analysis of polycyclic aromatic hydrocarbons in cooking oil fumes. Arch Ennviron Health. 1994;49:119–22. doi: 10.1080/00039896.1994.9937464. [DOI] [PubMed] [Google Scholar]
- 4.Thiébaud HP, Knize MG, Kuzmicky PA, Hsieh DP, Felton JS. Airborne mutagens produced by frying beef, pork and a soy-basd food. Food Chem Toxicol. 1995;33:821–8. doi: 10.1016/0278-6915(95)00057-9. [DOI] [PubMed] [Google Scholar]
- 5.Tzanakis N, Kallergis K, Bouros DE, Samiou MF, Siafakas NM. Short term effects of wood smoke on the respiratory system among charcoal production workers. Chest. 2001;119:1260–5. doi: 10.1378/chest.119.4.1260. [DOI] [PubMed] [Google Scholar]
- 6.Pierson WE, Konenig JQ, Bardana EJ., Jr Potential adverse health effects of wood smoke. West J Med. 1989;151:339–42. [PMC free article] [PubMed] [Google Scholar]
- 7.Lyon France: 2006. [Last accessed on 2012 Jan 25]. International Agency for Research on Cancer: Monographs on the Evaluation of Carcinogenic risks to human indoor air pollution from household cooking and heating: Emissions from high temperature frying; p. 95. Available from: http://monographs.iarc.fr/ENG/Meetings/95.cooking.oils.pdf . [Google Scholar]
- 8.Dennis RJ, Maldonado D, Norman S, Baena E, Martinez G. Wood smoke exposure and risk for obstructive airways disease among women. Chest. 1996;109:115–9. doi: 10.1378/chest.109.1.115. [DOI] [PubMed] [Google Scholar]
- 9.Erhabor GE, Kolawole OA, Adewole OO. Chronic obstructive pulmonary disease in OAUTHC Ile-Ife: A ten-year review of hospital mortality. J Natl Med Assoc. 2002;94:1071–6. [PMC free article] [PubMed] [Google Scholar]
- 10.Svedahl S, Svendsen K, Qvenild T, Sjaastad AK, Hilt B. Short term exposure to cooking fumes and pulmonary function. J Occup Med Toxicol. 2009;4:4–9. doi: 10.1186/1745-6673-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Erhabor GE, Fatusi AO, Ndububa A. Pulmonary symptoms and functions in gas welder in Ile Ife. Nig Med Pract. 1992;24:99–101. [Google Scholar]
- 12.Ijadunola KT, Erhabor GE, Onayade AA, Ijadunola MY, Fatusi AO, Asuzu MC. Prevalence of respiratory symptoms among wheat flour workers in Ibadan, Nigeria. Am J Ind Med. 2004;45:251–9. doi: 10.1002/ajim.10344. [DOI] [PubMed] [Google Scholar]
- 13.Ige OM, Onadeko OB. Respiratory symptoms and ventilatory function of the sawmillers in Ibadan, Nigeria. Afr J Med Med Sci. 2000;29:101–4. [PubMed] [Google Scholar]
- 14.Ibhazehiebo K, Dimkpa U, Uche OK, Iyawe VI. Peak expiratory flow rate and respiratory symptoms following chronic domestic wood smoke exposure in women in Edo, Nigeria. Afr J Biomed. Res. 2007;10:33–9. [Google Scholar]
- 15.Babashani M, Iliyasu Z, Ukoli CO. Respiratory symptoms and pulomanry function impairement among detergent plant workers in Jos, Northern Nigeria. Niger J Med. 2008;17:423–7. doi: 10.4314/njm.v17i4.37426. [DOI] [PubMed] [Google Scholar]
- 16.Medical Research Council on the Aetiology of Chronic Bronchitis. Standardised questionnaire on respiratory symptoms. BMJ. 1960;2:1665. [Google Scholar]
- 17.Chan–Yeung M, Malo JL. Occupational asthma. N Eng J Med. 1995;333:107–110. doi: 10.1056/NEJM199507133330207. [DOI] [PubMed] [Google Scholar]
- 18.Yeh F, Rhodes ER, Tarpay M, Eicher JE. Advantages of video questionnaire in estimating asthma prevalence and risk factors for school children: Findings from an asthma survey in American Indian Youth. J Asthma. 2010;47:311–7. doi: 10.3109/02770903.2010.485663. [DOI] [PubMed] [Google Scholar]


