Abstract
Background:
Non-adherence to anti-tuberculosis (TB) treatment adversely affects treatment success rate. It increases disease morbidity and mortality. Also, it contributes significantly to the development of drug resistance.
Aim:
To identify risk factors for non-adherence to anti-TB treatment by new pulmonary TB patients.
Subjects and Methods:
It is a prospective cohort study at 21 TB treatment centres in E ward of Mumbai Municipal Corporation. All sputum smear positive new pulmonary TB patients initiated on treatment regimen of short course chemotherapy fro 1st January to 30th June of a calendar year were enrolled and followed up till any final outcome as per revised national TB control program. Non-adherence was defined as interruption of anti-TB treatment for ≥ 1 month. The factors were identified by univariate and logistic regression analysis.
Results:
We studied 156 newly diagnosed pulmonary TB patients. Out of these 78 (50%) were non-adherent to anti-tuberculosis treatment (ATT). Independent risk factors for non-adherence were identified as male gender (P = 0.035) and lack of knowledge of importance of regular treatment (P = 0.001). Being female sex worker (FSW) was also an absolute risk factor for non-adherence.
Conclusions:
There is immense need for continuous, effective and reinforcing health education to the patient and his family. Special groups like males in the age group of 15-49 years, patients who do not have any family support like migrants, FSW need special attention to ensure adherence to ATT.
Keywords: Adherence, Anti-tuberculosis treatment, Non-adherence
Introduction
Tuberculosis (TB) is a global health concern.[1] In low- and middle-income countries it is fuelled bypoverty, population increase and infection with human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS).[2] South East Asia Region carries about 40% of the global TB burden. India is the highest TB burden country in the world andaccounts for more than 25% of the world's incident cases.[3] More than 1000 Indians die of TB every day.[4]
World Health Organisation (WHO) has recommended directly observed treatment short course (DOTS) strategy for global TB control which is accepted worldwide.[5] Direct observation and regular home visits by treatment providers are provisions to increase treatment completion under DOTS. Based on DOTS strategy, India's revised national tuberculosis control program (RNTCP) was launched in 1997. Though treatment completion rate reported by RNTCP is satisfactory, recently there is growing concern of emergence of drug resistant strains of TB bacillus. Incomplete anti-tuberculosis treatment (ATT) is the reason for emergence of multi-drug resistant strains of TB bacillus that emerged in the early 1990s, extensively drug-resistant strains emerged in 2006 and now totally drug-resistant strains emerged in 2012 in India.[6] ATT based on DOTS alone do not always promote Treatment adherence.[7] ATT has multiple drugs and usually of at least 6 months’ duration. Patients on ATT may have unpleasant side effects of the drugs.[2] As a result, many TB patients start ATT but do not finish it.[8] Inadequate ATT may result in relapse and contribute to increase in morbidity, mortality, cost, duration of ATT and drug resistance at both individual and community level.[7,9]
Treatment providers have important role in completion and success of ATT. But, TB patients do not always co-operate with DOTS providers. They can decide about their treatment when away from the provider. Such decisions made by patients themselves can adversely affect treatment completion and its success.[2] Treatment behaviour is influenced by many factors such as socio-cultural, economic background, perceived health benefits and subjective experience of illness.[2]
Treatment adherence is the extent to which patients’ history of therapeutic drug intake coincides with prescribed treatment. It requires patient's agreement to providers’ recommendations.[7] Treatment adherence reflects active role of TB patients in self-management of treatment and extent of patient provider interaction (PPI).[2] Poor adherence to ATT may lead to treatment failure[10–13] while strict adherence to ATT help to achieve desired treatment success and help to minimize emergence of drug resistant strains.[14–16]
Stigma, illness representation and wide range other factors interact impacting treatment adherence.[17] These factors are needed to be identified early in their management. It will enable health care providers to take measures so that such patients will continue their treatment without interruption.[2]
Thus, treatment adherence by TB patients is a complex and multifaceted behavioural issue that needs to be understood better.[18] The TB literature is written almost entirely from a biomedical perspective.[17] Recent studies to show why people interrupt and may stop taking ATT are still scarce.[2] Lack of a comprehensive and holistic understanding of barriers to and facilitators of, treatment adherence is currently a major obstacle to find effective solutions.[19] Behavioural and social research for ATT adherence is important particularly when epidemiology of the disease has changed.[2]
In the present study, we tried to identify risk factors for non-adherence to ATT by NSP TB patients. If untreated, NSP TB patients are more likely to die compared to smear negative TB patients. Also, if untreated each NSP TB patient can infect 10-15 people per year.[15] Thus, they put community at greater risk of TB transmission. Their ATT initiation as well as completion with treatment adherence is utmost important. Hence, we prospectively followed up a cohort of NSP TB patients to study risk factors for non-adherence to ATT.
Subjects and Methods
Study was conducted in E ward of Mumbai Municipal Corporation (MMC) in Maharashtra state of India. Vast employment opportunities in Mumbai create a social crisis due to continuous migration of rural population all over the country. For administrative purpose MMC is divided into 6 zones, zone 1-6. Each zone has 3-5 wards named alphabetically. Zone 1 has 5 wards-A, B, C, D, and E. There is a continuous migration of rural population to Mumbai for employment.
DOTS under RNTCP are an integral part of the public health system in India. TB diagnostic services and treatments are provided free of cost at DOTS centres, TB dispensaries and hospitals run by government. It is also provided through public private partnerships.
Mumbai is the largest megacity in India with a population >18 million. MMC has total 298 DOTS centres where TB patients are treated by government free of cost based on DOTS strategy under RNTCP. 21 of these DOTS centres are located in E ward which has a population of >5 lacs.
Ward E is one of the most densely populated wards in MMC with highest number of decades-old slum and chawl settlements. The ward also includes the country's largest red-light area, Kamathipura. Along with number of small cottage industries, it has large tracts of Mumbai Port Trust Land, number of ship breaking and metal scrap selling units. It employs huge number of workers in overcrowded conditions with lack of sanitation. Majority of them are migrants from rural areas.
The study was approved by Ethical committee, Grant Medical College, Byculla, Mumbai and by Member secretary, Mumbai district TB control society.
We recruited all NSP TB patients initiated on category one (cat-I) treatment regimen of DOTS from 01 January to 30 June of a calendar tear. They were followed up till any final outcome of RNTCP.[20] Follow-up of lasted recruited case ended in February of the following year.
We defined non-adherence to ATT as interruption of ATT by recruited patient for ≥1 month.[21] Other definitions were followed as per RNTCP.[20]
Data collection was done by pre-tested structured interview schedule and questionnaires. They were pre-tested on 10 TB patients. Suitable modifications were done to achieve final structured interview schedule and questionnaires.
When the case was initiated cat-I DOTS regimen, investigator contacted the patient to fill up the proforma which included socio-demographic characteristics of patients, history of addictions, family history and support etc., Verbal consent of the case was taken to participate in the study. As per RNTCP, patients were contacted by treatment providers after they missed a single dose. But, sometimes they were unable to put them back on ATT because of various reasons. Such patients who did not return for treatment for >1 month, were identified from treatment cards at DOTS centres. They were contacted at their residence, work-place, by visits or telephone or they were called at DOTS centre with the help of treatment providers. Reasons for non-adherence were noted. Questionnaire was administered to find factors responsible for non-adherence and to assess knowledge regarding ATT they were taking. At the same time, patients were counselled by treatment providers and investigator to continue the treatment. Same questionnaire was administered to treatment adherent patients at the completion of the treatment.
Data analysis was done by SPSS (Chicago, Illinois, USA) 11.5 and STATA 8.0 softwares. For analysis of categorical data, frequencies were established; Pearson's Chi squared test was used as test of significance. When expected value in 2 × 2 table was <5, Fisher's Exact test was used as a test of significance. When expected value in n × n table was <5, Likelihood Ratio test was used as a test of significance. Logistic regression analysis of risk factors implicated in univariate analysis was done to find out independent risk factors.[22] Regression model was tested for goodness of fit by Hosmer and Lemeshow goodness of fit test with P = 0.2652. Similarly, pseudo R2 for the model was 0.4921. Receiver output characteristic curve showed area under receiver output curve as 0.9527. It showed regression model used was of excellent fit.
Results
Total 157 NSP TB patients were initiated on cat-I DOTS regimen in selected study area during assigned study period. As one eligible case was not willing to participate in study, we recruited 156 patients in the study. 67.30% (105/156) were males and 32.70% (51/156) were females. Average age of patients recruited was 32.99 years. 66.66% (104/156) were in the age group of 20-49 years. 53.8% (84/156, 59 males, 13 females) were migrated to Mumbai since average 5.68 years for food, job or shelter. 22.6% (19/84) were from various places in Maharashtra, 38.1% (32/84) were from UP and 9.5% (8/84) were from Bihar.
Overall 50% (78/156) were non-adherent to ATT that is they interrupted treatment for ≥1 month. 50% (78/156) were treatment adherent till final outcome of RNTCP.
Out of 78 treatment adherent patients, 2 were transferred out and 4 died during the course of treatment, they were not available for second interview. So, further analysis was done for 78 treatment non-adherent and 72 treatment adherent patients [Figure 1].
Figure 1.
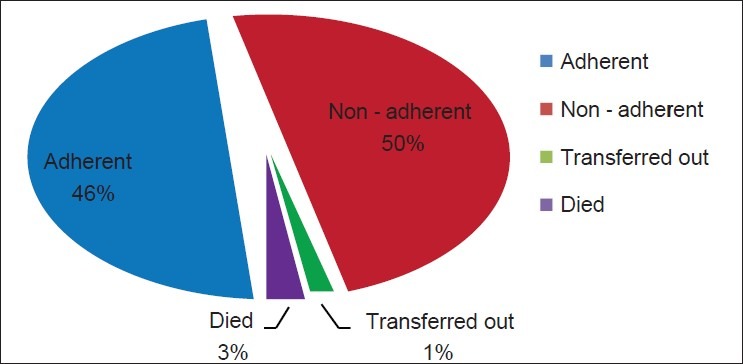
Distrubution of cases by patients treatment outcome
Out of 78 non-adherent patients, 40 (51.3%) interrupted the treatment for ≥1 month during intensive phase (IP) or extended intensive phase, before starting continuation phase (CP) [Table 1]. Majority of them (27 out of 40) did so because they started to feel better. Thirteen out of these 40 patients knew that duration of treatment was only 2 months and all were non-adherent at completion of IP. These patients were contacted by DOTS providers to continue and complete the desired ATT. It helped to decrease defaulters.
Table 1.
Onset of non-adherence during the treatment
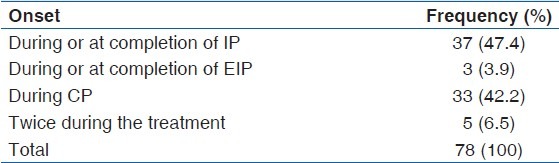
42.3% (33/78) of non-adherent patients interrupted ATT during CP for ≥1 month and 6.5% (5/78) interrupted ATT for ≥1 month for 2 times during the course of the treatment.
Univariate analysis showed [Table 2] that patients, who were between 15 years and 49 years of age group, males, migrants and patients who were employed were more likely to be non-adherent. The crude odds ratios (95% CIs) were 1.561 (0.926-2.629), 2.510 (1.508-4.176), 1.969 (1.376-2.817) 1.632 (1.172-2.273) respectively. Patients who were educated till at least high-school and from poor socio-economic strata (SES) were also more likely to be non-adherent [Table 2].
Table 2.
Univariate analysis of association between selected factors and treatment adherence
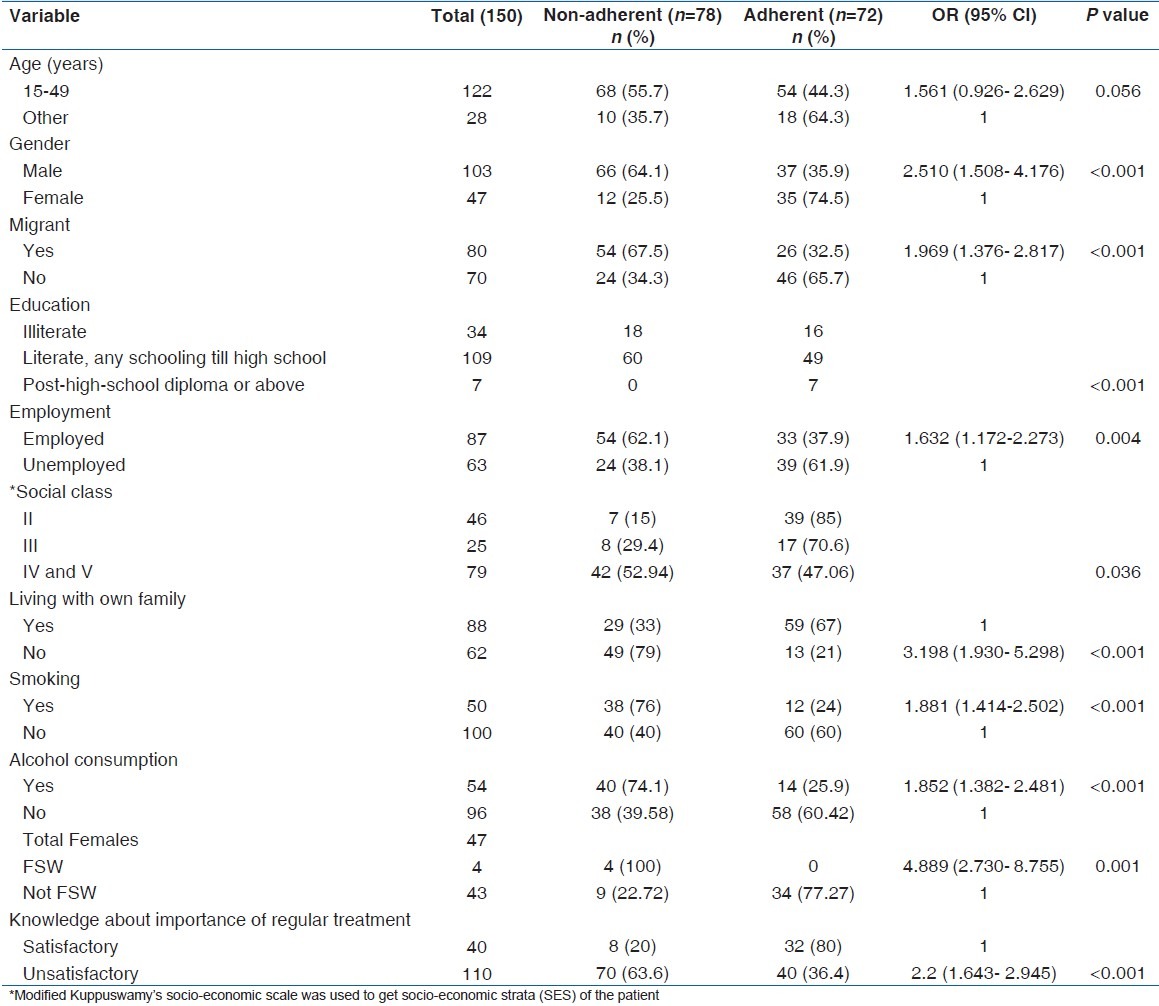
In multivariate analysis [Table 3], gender as male (P = 0.035) and unsatisfactory knowledge of importance of regular treatment (P < 0.001) were independent risk factors associated with non-adherence [Table 3]. 66 (64.1%) out of 103 males were non-adherent while only 12 (25.5%) out of 47 females were observed to be non-adherent. And, out of 40 patients who knew that regular treatment is must for cure of TB, 32 (80%) were treatment adherent while out of 110 patients who didn’t know importance of regular treatment, only 40 (36.4%) were treatment adherent [Figures 2 and 3].
Table 3.
Multiple logistic regression model to determine the factors predicting treatment non-adherence
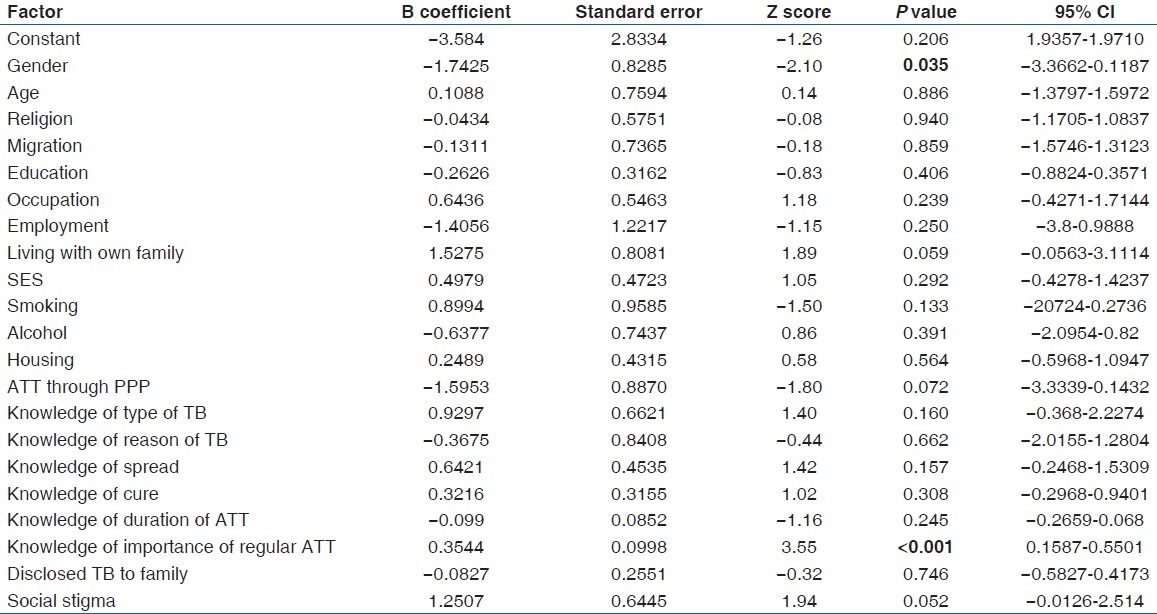
Figure 2.
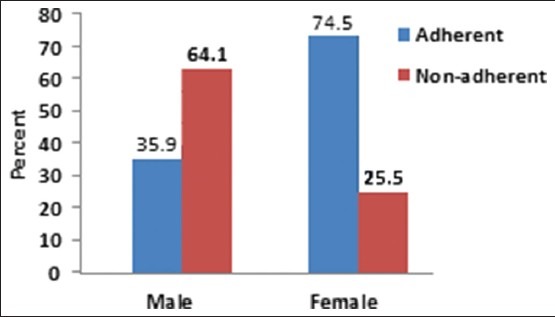
Gender & Non-adherence
Figure 3.
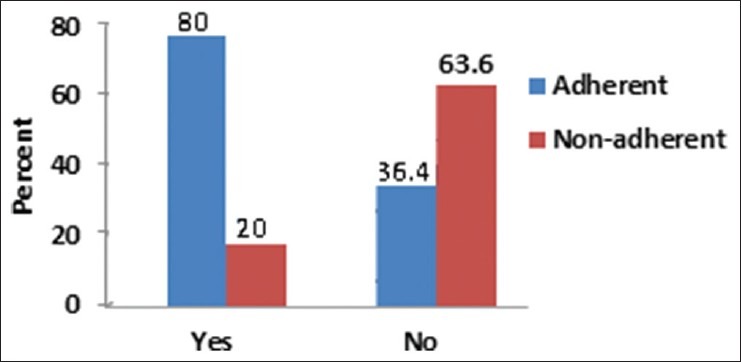
Knowledge of importance of regular treatment & non-adherence
To be a female sex worker (FSW) was observed as absolute risk factor for non-adherence as all 4 FSWs among patients were non-adherent to ATT [Figure 4].
Figure 4.
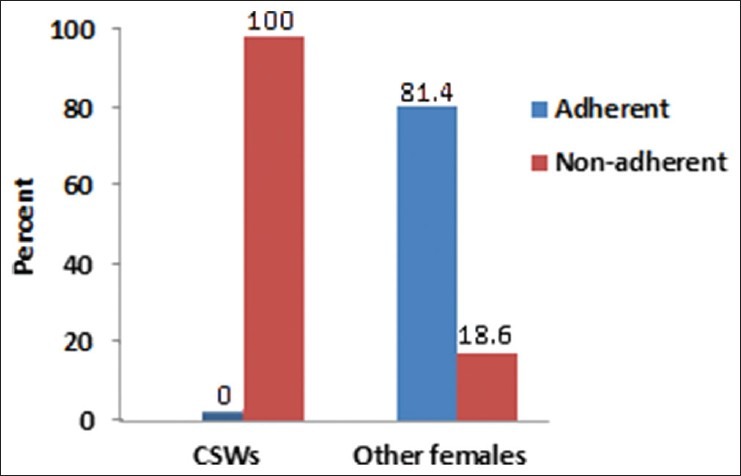
CSWs & non-adherence
Other significant variables implicated by univariate analysis had no such association after logistic regression. They could have been associated with non-adherence due to interaction and confounding.
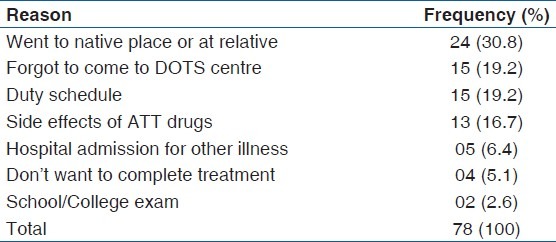
Patients listed various reasons for non-adherence to ATT [Table 4]. The main reasons for non-adherence [Table 4] were patient went to native place or at relative 30.8% (24/78), Forgot to come to DOTS centre 19.2% (15/78), has to go for work 19.2% (15/78), side effects of drugs 16.7% (13/78).
Table 4.
Reasons for non-adherence listed by patients
Discussion
In-spite of activities under RNTCP to improve ATT adherence, present study found 50% (78/156) patients as non-adherent. DOTS providers tried to contact them as per RNTCP norms that is within one day of missing a dose during IP and within a week of missing a weekly collection of drugs during CP. But, inspite of all efforts they were unable to trace them and/or put them back on ATT for ≥1 month.
We found females as more treatment adherent as reported by several studies.[21,23,24] Majority of non-adherent patients were males 15-49 years in age group. Most of them were from lower SES, migrants and people residing in unstable living conditions like cottage industry workers, FSWs. Poor knowledge of importance of regular treatment for TB cure also predicted non-adherence well.
Many studies on defaulters who are inherently non-adherent, observed that majority of them were in the age group of 35-55 years.[14,25] In the present study we found that more younger male TB patients, in 15-49 years of age group were more non-adherent.
People in this age group may migrate to a megacity like Mumbai for various employment opportunities. TB patients domiciled at treatment place used to be more treatment adherent than migrants.[26] Migration may force them to live alone or without family, to get minimal social support and to live in overcrowded and unhygienic environment.
Thus, migration affects stability of residence and it can adversely affect adherence.[7,27] More than half, 70.51% (55/78) of non-adherent patients were migrants with majority of males (49 out of 55). 30.8% patients went to native place and became non-adherent. In such cases treatment providers should be trained to collect information regarding native place, names and contact details of family members of nearest relatives, name of DOTS centre for that area and its in-charge officer. By using newer technology like use of SMS on mobile number of the patient, patient can be reminded about his dose of ATT. Patient may not inform to DOTS provider while leaving the area for long duration. Hence, there should provisions to trace such patients like tracing a mobile number for the same name and provision for use of single mobile number all over the country. It can also be linked to Unique Identify (UID)/Adhar card of the patient. UID is a scheme launched by the Unique Identification Authority, Planning Commission Government of India, to provide a UID or Adhar card with individual biometrics to every citizen. This scheme is envisaged to establish proof of identify of all individuals and is envisaged to particularly help migrant people.
We had 4 FSWs in our study. All of them were non-adherent to ATT during IP that is even before sputum conversion. They were not traceable to treatment providers. Underlying cause may be migration, lack of freedom, discrimination due to prostitution and TB and/or cost and time required to come to DOTS centre.[28] There were more than 45000 Nepali girls and FSWs in India in 1996 and about 5000-7000 are sent to India every year.[29] Their unstable living conditions with poor access to health care and lack of needed social support force them to be non-adherent to long term treatment like ATT.[28] To be treatment adherent, they need newer strategies under RNTCP to evolve like providing job, shelter and food to them till at least treatment completion.
19.2% non-adherence was due to forgetfulness of patients to go to DOTS clinic and take medicine. Such ignorance on part of patients reflect inadequate dissemination of information and education regarding TB and importance of its treatment by DOTS providers. Other 19.2% non-adherence was due to timing at occupational site of the worker. It emphasizes need to evolve strategies at work place and slums through peer outreach system linked with RNTCP.
As TB patient feels better after few weeks of treatment initiation and may tend to leave the treatment as he assumes that TB is cured.[2] We found 37 out of 78 non-adherent patients did so before starting CP. They reported that they were informed that treatment duration will be decided after 2 months of initial treatment. As, sputum smear was negative after 2 months, it was unexpected for them to be back on treatment for more period of time. It also denotes improper management of RNTCP. Treatment providers should spend adequate time to inform and educate TB patient regarding importance of regular treatment, correct duration of the treatment and laboratory diagnosis. In the same way, Sophia et al., observed that knowledge about correct duration of treatment was significantly lower among non-adherent group.[21]
We found lack of knowledge of importance of regular ATT as second independent risk factor for non-adherence. Correct knowledge about TB and its treatment improves adherence to ATT.[30] Defaulters are found to have less or no knowledge about TB disease and its treatment,[21] and non-adherent patients are potential defaulters.
Education overall increases knowledge and health awareness and treatment seeking behavior of the individual.[31] Literate individuals are more likely to complete the treatment.[21] We observed that patients who have completed at least high school education were strictly treatment adherent. We noted decrease in trend of non-adherence as level of education increased.
Several studies report that non-adherence is associated with low SES.[21,32] We also found that as social class became higher, treatment adherence increased.
Family support received by patients play important role in improving treatment adherence. Lack of family and social support predicts poor treatment adherence.[9,21,33] In our study, patients not living with own family were observed to be more non-adherent to the treatment as compared to patients living with family.
Alcohol consumption is well known risk factor for non-adherence.[7] We had 54 alcoholics in our study. They were significantly more non-adherent than non-alcoholics. Among alcoholics, regular alcoholics were highest to be non-adherent than occasional or past alcoholics. As, smoking is most of the times associated with alcoholism, it can also predict poor treatment adherence.[24] Out of 156 patients, we had 50 smokers. Majority of them (60%) were non-adherent to the treatment.
Knowledge of importance of regular treatment shows the extent of PPI and impact of all health educational activities held at DOTS centre to which patient is exposed while being treated. There is immense need for continuous, effective and reinforcing health education to the patient and his family. Treatment providers should pay special attention to male patients in 15-49 year age group, from lower SES, migrants, habitual smokers, alcoholics. Special groups who do not have any family support like FSWs, migrated individuals living alone or without family need special attention and provisions under RNTCP, at least in study area. More patient-centered interventions and greater attention to structural barriers are needed to improve treatment adherence.
Training of RNTCP staff in interpersonal communication skills is needed to be enhanced to deal with TB patients. They should be adequately trained to disseminate correct knowledge about TB disease and its treatment to the TB patients. They should also be adequately trained and supervised about strict adherence to transferring out procedures.
RNTCP staff should screen all TB patients for factors predicting possible non-adherence since at the time of diagnosis and treatment initiation. Patients with such risk factor should be motivated to follow DOTS through counselling. Trained counsellors are needed to be appointed to counsel cases having a cock-tail combination of risk factors for non-adherence. It should be done with the help of relatives and/or person who has positive impact on patient's behaviour.
Study provided a good insight regarding risk factors for non-adherence to ATT. Most available studies with DOTS are retrospective in nature with patient interview at the end of the treatment. But, several factors shape the treatment behaviour from initiation till final outcome. They may not come into picture while interviewing patient at the end of the treatment.[21]
For logistic reasons the study is carried out in E ward of MMC. It may limit generalisability of the study. We tried to compensate this error by having a strict control on internal validity. As most of the data was qualitative, veracity of answers was checked by data triangulation.
Many studies report association of unemployment and non-adherence.[32] But, we found that unemployed patients were more treatment adherent. It may be due to time available to go to DOTS centre to take doses on proper time. Also, females contributed majority of unemployed group and as discussed earlier females are more treatment adherent. It may reflect role of social and family support when on ATT. We did not observe any association of non-adherence with religion or marital status.
15% (20/150) patients in the study were treated through public private partnership (PPP). Majority of them (17/20) were non-adherent to ATT.
Study identified many loopholes in supervision of ATT under DOTS given by private practitioners. Effective mechanisms have to be evolved to ensure treatment adherence through PPP approach.
Acknowledgments
We are grateful to Dr G T Ambe, Member Secretary, Mumbai District TB Control Society who permitted to carry out the study in Ward-E of Mumbai District.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Global tuberculosis control: Surveillance, planning, financing. Geneva: WHO; 2008. WHO. [Google Scholar]
- 2.Esther S. When TB treatment fails: A socio-behavioral account of patient adherence. Am Rev Respir Dis. 1993;147:1311–20. doi: 10.1164/ajrccm/147.5.1311. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Tuberculosis control in South-East Asia Region. Regional Report. 2012 [Google Scholar]
- 4.USAID-India. Health overview. 2011 [Google Scholar]
- 5.WHO. The origins of DOTS. Research for action: Understanding and controlling TB in India. 2000 [Google Scholar]
- 6.Coghlan A. Totally drug-resistant TB at large in India. New Scientist Health. 2012. Jan 12, Available at: http://www.newscientist.com/article/dn21350-totally-drugresistant-tbat-large-in-india.html .
- 7.WHO. Diseases specific reviews. Adherence to long term therapies: Evidence for action. 2003:123–8. [Google Scholar]
- 8.WHO. TB and DOTS. NGOs and TB control: Principles and examples for organizations joining fight against TB. 1999 [Google Scholar]
- 9.Pablos-Méndez A, Knirsch CA, Barr RG, Lerner BH, Frieden TR. Nonadherence in tuberculosis treatment: Predictors and consequences in New York city. Am J Med. 1997;102:164–70. doi: 10.1016/s0002-9343(96)00402-0. [DOI] [PubMed] [Google Scholar]
- 10.Xu W, Lu W, Zhou Y, Zhu L, Shen H, Wang J. Adherence to anti-tuberculosis treatment among pulmonary tuberculosis patients: A qualitative and quantitative study. BMC Health Serv Res. 2009;9:169. doi: 10.1186/1472-6963-9-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burman WJ, Cohn DL, Rietmeijer CA, Judson FN, Sbarbaro JA, Reves RR. Nonadherence with directly observed therapy for tuberculosis. Epidemiology and effect on the outcome of treatment. Chest. 1997;111:1168–73. doi: 10.1378/chest.111.5.1168. [DOI] [PubMed] [Google Scholar]
- 12.Addington WW. Patient adherence: The most serious remaining problem in the control of tuberculosis in the United States. Chest. 1979;76(Suppl):S741–3. doi: 10.1378/chest.76.6_supplement.741. [DOI] [PubMed] [Google Scholar]
- 13.Fox W. Adherence of patients and physicians: Experience and lessons from tuberculosis-II. Br Med J (Clin Res Ed) 1983;287:101–5. doi: 10.1136/bmj.287.6385.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Central TB Division. TB India2012; RNTCP Annual Status Report. New Delhi: Central TB Division, Directorate General Health Services, Goverment Of India; 2012. pp. 21–6. [Google Scholar]
- 15.Wares DF, Singh S, Acharya AK, Dangi R. Non-adherence to tuberculosis treatment in the eastern Tarai of Nepal. Int J Tuberc Lung Dis. 2003;7:327–35. [PubMed] [Google Scholar]
- 16.Paramasivan CN, Venkataraman P. Drug resistance in tuberculosis in India. Indian J Med Res. 2004;120:377–86. [PubMed] [Google Scholar]
- 17.Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: A systematic review of qualitative research. PLoS Med. 2007;4:e238. doi: 10.1371/journal.pmed.0040238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sophia V, Balasangameswara VH, Jagannatha PS, Saroja VN, Kumar P. Defaults among tuberculosis patients treated under DOTS in Bangalore city: A research for solution. Ind J Tub. 2003;50:185–95. [Google Scholar]
- 19.Centers for Disease Control (CDC). Transmission of multidrug- resistant tuberculosis among immunocompromised persons in a correctional system–New York, 1991. MMWR Morb Mortal Wkly Rep. 1992;41:507–9. [PubMed] [Google Scholar]
- 20.Cramm JM, Finkenflügel HJ, Møller V, Nieboer AP. TB treatment initiation and adherence in a South African community influenced more by perceptions than by knowledge of tuberculosis. BMC Public Health. 2010;10:72. doi: 10.1186/1471-2458-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumareson J. Epidemiology. In: Narayan JP, editor. Tuberculosis: Epidemiology and Control. 1st ed. New Delhi: WHO Regional Office for South-East Asia; 2002. pp. 16–7. [Google Scholar]
- 22.Sophia V, Balasangameshwara VH, Srikantaramu N. Treatment dynamics and profile of patients under DTP: A prospective cohort study. Indian J Tuberc. 1999;46:239–49. [Google Scholar]
- 23.Dawson B, Trapp RG. Basic andclinical biostatistics. 4th Ed. New York: McGraw-Hill Companies; 2004. [Google Scholar]
- 24.Sophia V, Balasangameshwara VH, Jagannatha PS, Saroja VN, Shivashankar B, Jagota P. Retreatment outcome of smear positive PTB patients under DOTS in Bangalore city. Indian J Tuberc. 2002;49:195–203. [Google Scholar]
- 25.Central TB division. RNTCP at glance. 2006 [Google Scholar]
- 26.Deshmukh MD. Pulmonary tuberculosis and common chest diseases. 2nd edition. Bombay: Kothari Medical Publishing House; 1980. Historical aspects of TB. [Google Scholar]
- 27.Gad A, Mandii AMA, Shérif AARA, Gad ZM, Sallam S. Compliance with anti-tuberculosis drugs among TB patients in Alexandria. Egypt. 1997;2:244–50. [Google Scholar]
- 28.Bagchi S, Ambe G, Sathiakumar N. Determinants of poor adherence to anti-tuberculosis treatment in Mumbai, India. Int J Prev Med. 2010;1:223–32. [PMC free article] [PubMed] [Google Scholar]
- 29.Rao KN. History of Tuberculous. In: Rao KN, Vishwanathan R, Sen PK, Deshmuch MD, Bordia NL, Pamra SP, et al., editors. Text-book of Tuberculosis. The Tuberculosis Association of India. 2nd edition. 1981. pp. 3–15. [Google Scholar]
- 30.Culqui DR, Munayco E CV, Grijalva CG, Cayla JA, Horna-Campos O, Alva Ch K, et al. Factors associated with the non-completion of conventional anti-tuberculosis treatment in Peru. Arch Bronconeumol. 2012;48:150–5. doi: 10.1016/j.arbres.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 31.Geetakrishnan K. Case holding and treatment failures under a TB clinic operating in rural settings. Int J Tub. 1990;37:145–8. [Google Scholar]
- 32.Bhatia S, Dranyi T, Rowley D. Tuberculosis among Tibetan refugees in India. SocSci Med. 2002;54:423–32. doi: 10.1016/s0277-9536(01)00041-7. [DOI] [PubMed] [Google Scholar]
- 33.Prozsik, et al by CDC. Approaches to improve adherence to ATT. South Carolina and New York, 1986-1991. CDC. MMWR, weekly. 2005. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/00019521.htm .


