Abstract
Background:
The aim of this study was to evaluate intraocular pressure (IOP) and hemodynamic responses following insertion of laryngeal mask airway (LMA) or endotracheal tube (ETT) after anesthesia induction with propofol and remifentanil in cataract surgery.
Materials and Methods:
In a randomized controlled study, 50 adults scheduled for elective cataract extraction procedure under general anesthesia were allocated to LMA insertion (n = 25) or ETT (n = 25) groups. IOP, systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were measured after insertion of the airway device every minute up to 5 min.
Results:
There were no significant differences between LMA and ETT groups in SBP, DBP, HR, and IOP immediately after airway instrumentation up to 5 min, except in 4th min in DBP, 2nd min in HR, and 5th min in IOP (7.9 ± 2.3 mmHg in LMA and 9.4 ± 2.5 mmHg in ETT group; P = 0.030). There was good surgeon satisfaction for providing acceptable surgical field in both groups (88% in LMA and 80% in ETT group; P = 0.702).
Conclusion:
Propofol combined with remifentanil provides good and excellent conditions for insertion of LMA or ETT with minimal hemodynamic disturbances in cataract surgery. Considering LMA insertion is less traumatic than ETT, using LMA may be better than ETT for airway securing in these patients.
Keywords: Cataract surgery, hemodynamic responses, laryngeal mask airway, propofol, remifentanil
INTRODUCTION
Cataract surgery with lens implantation is one of the most commonly performed elective operations in the adults. On the other hand, in 2007-2008, among US adults aged 320 years, an estimated 49.7% had at least one of the cardiovascular disease risk factors.[1] The stress response to intubation, which entails laryngoscopy, is associated with a rise in intraocular pressure (IOP) mainly due to increased ocular blood flow.[2] These stress responses are hypertension, myocardial ischemia, or cerebrovascular disease.[3] The laryngeal mask airway (LMA) has seen increasing use in patients undergoing cataract extraction and lens implantation.[4] This is the result of a desire to limit the rise in IOP because there is minimal laryngo-tracheal stimulation associated with LMA placement. If at this time the IOP is increased, the intraocular contents are forced toward the incision. The iris, lens, or vitreous may prolapse either immediately or when the surgeon attempts to move the lens.[2]
Many studies have shown the effect of different combinations of anesthetic drugs including hypnotics and opioids on reducing the side effect of tracheal intubation on patients’ hemodynamic parameters.[5–9] Motiang et al.[2] and Siddiqui et al.[10] used propofol and isoflurane pulse nitrous oxide and compared the hemodynamic and IOP changes in cataract patients, while Whitford et al.[11] administered propofol with enflurane for cataract surgery. Eltzschig et al.[12] induced anesthesia with sevoflurane and remifentanil for strabismus surgery and compared IOP changes between endotracheal intubation (ETT) and LMA. Some investigators evaluated IOP changes between ETT and LMA placement in non-ocular surgeries using different anesthetic regimens.[13,14] In a recent study, Ismail et al.[3] compared IOP and hemodynamic responses to insertion of the i-gel, LMA, or ETT in non-ophthalmic procedures using thiopental and fentanyl.
We did not find any prospective and controlled trial that used the combination of propofol and remifentanil for inducing anesthesia in cataract surgery to compare the IOP and hemodynamic changes between ETT and LMA. Thus, this randomized controlled clinical trial was aimed to evaluate IOP change and hemodynamic responses in cataract surgery patients using ETT or LMA techniques using this special drug combination and to find a technique which is associated with minimal changes.
MATERIALS AND METHODS
After obtaining ethics approval and informed written consent, 50 adult patients of American Society of Anesthesiologists physical status I-III were recruited in the study. They ranged in age from 18 to 82 years, had normal IOP, and were scheduled for unilateral cataract extraction under general anesthesia. Patients presenting with the following conditions were excluded from selection: glaucoma, diabetes mellitus, severe respiratory disease, uncontrolled hypertension, and known allergy to any of the drugs to be used. The patients were randomized into two groups of ETT and LMA, with 25 patients in each [Figure 1]. According to Motiang and Rantloane's study[2] that measured IOP 20 seconds after placement of LMA (7.2 ± 4.2 mmHg) and ETT (3.85 ± 3.1 mmHg) and considering a = 0.05 and study power = 80% by using an online sample size calculator (available in URL: http://www.stat.ubc.ca/~rollin/stats/ssize/n2.html), the sample size was calculated to be 25 patients for each group separately. The randomization process was done by using an online software (URL: http://www.graphpad.com).[14] Our study was single blinded [the patients were unaware of the type of airway management, but the anesthesiologist selected (randomly) ETT or LMA].
Figure 1.
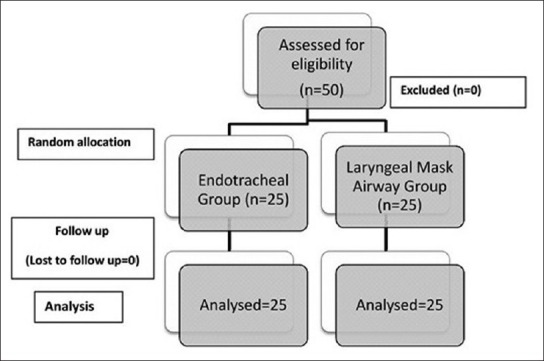
Randomized patients’ flow diagram
In the LMA group, the airway was secured with an LMA (size 4 in men and size 3 in women), while the ETT group represented patients in whom the airway was secured with a tracheal tube with appropriate size after which the cuff was inflated, avoiding leak. One attending anesthesiologist did laryngoscopy and ETT or placement of LMA in all the studied patients. All the patients were in grade I or II of laryngoscopy and there was not any case of difficult intubation. There was not any case of difficult intubation or repeated intubation; duration of laryngoscopy and intubation in all patients was less than 15 seconds. The cuffed tracheal tube used in women was of internal diameter (ID) 7.5 mm and in men the ID was 8.5 mm. The anesthesiologist filled the tracheal tube cuff until there was no air leakage in inspiratory pressure of 25 cmH2O.
Anesthesia was induced with propofol (2–2.5 mg/kg) and remifentanil (0.6–1 μg/kg) titrated to loss of eyelash reflex and this was followed by an intubating dose of atracurium (0.5 mg/kg). ETT or LMA placement proceeded 3 min thereafter. Anesthesia was maintained as a continuous infusion of remifentanil (0.17 μg/kg/min) and propofol 50–150 μg/kg/min. Ventilation of the lungs was controlled on volume control mode and adjusted to maintain EtCO2 at 32–35 mmHg. Monitoring consisted of continuous three-lead electrocardiography, non-invasive blood pressure, pulse oximetry, and capnography. A Schiotz tonometer was used to measure IOP after instillation of one drop of 0.5% tetracaine in the non-operated eye pre-induction. Repeat measurements were undertaken in 15th–30th second, 1st, 2nd, 3rd, 4th, and 5th min after the airway was secured.
Hemodynamic parameters including heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and IOP were compared between groups after airway instrumentation. We corrected the fluctuations in blood pressure more than 20% of basal value range. Hypertension was treated with nitroglycerin infusion and hypotension was corrected by volume infusion and/or administration of IV ephedrin 5–10 mg bolus doses. The dose of nitroglycerin was 0.05–0.5 μg/kg/min adjusted to the patient's need to control the blood pressure rise to >20% of pre-induction value.
The data were analyzed using SPSS for Windows statistical package v.18.0 (SPSS Inc., Chicago, IL, USA). Continuous variables in the two groups were compared using independent samples t-test and categorical parameters were analyzed by Chi-square test. A P-value ≤0.05 was considered statistically significant.
RESULTS
Patients’ clinical parameters in LMA and ETT groups are shown in Table 1. There was a statistically significant difference in sex distribution in the two study groups (P = 0.023). In the LMA group, 19 patients had laryngoscopy grade of I and 6 patients were of grade II; in the ETT group, 21 patients were of grade I and 4 patients were of grade II (P = 0.725). In the LMA group, two patients experienced hypertension and three faced mild hypotension that was treated as mentioned in Materials and Methods section. In the ETT group, four patients had increase and two patients had decrease in blood pressure that was corrected. There was not any significant difference in the number of patients who needed correction of blood pressure changes during operation [Table 1].
Table 1.
Patients’ clinical parameters in laryngeal mask airway and endotracheal intubation groups
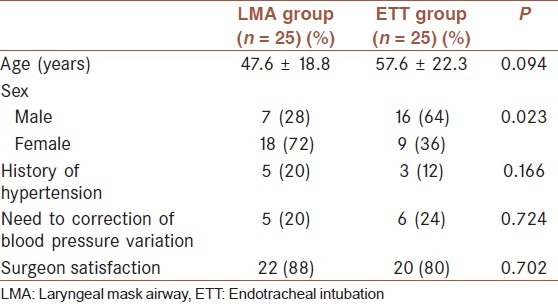
Hemodynamic changes of patients in the two study groups are illustrated in Figures 2 and 3. Overall, there were no significant differences in the two groups considering SBP, DBP, and HR changes 5 min after intubation. In both groups, there was a minimal increase in IOP through the operation, but there was statistically significant difference only in 5th min after intubation between the LMA (7.9 ± 2.3 mmHg) and ETT (9.4 ± 2.5 mmHg) groups (P = 0.030) [Figure 4]. There was a similar trend of change (minimal increase after airway securing) with no significant difference in peripheral O2 saturation in both groups [Figure 5].
Figure 2.
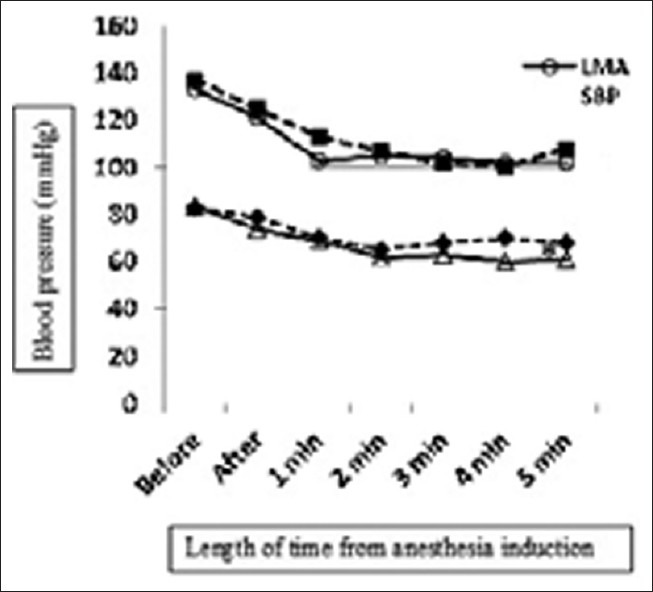
Comparison of systolic and diastolic blood pressure in laryngeal mask airway and endotracheal intubation groups (*P < 0.05)
Figure 3.
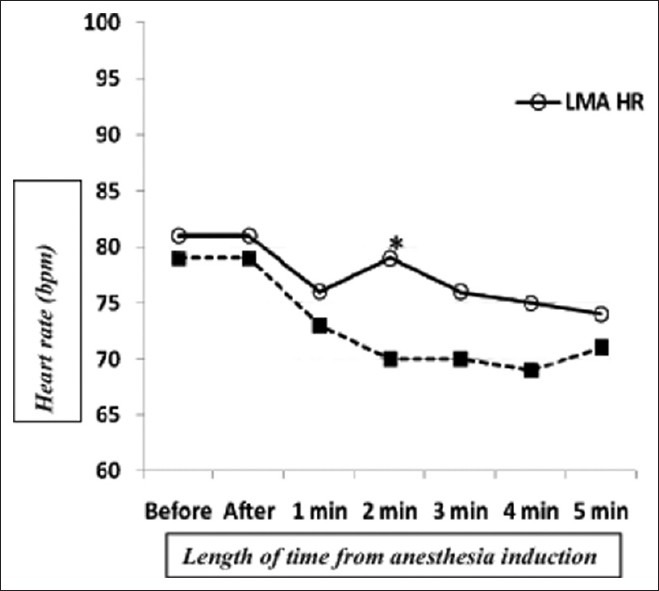
Heart rate variation in laryngeal mask airway and endotracheal intubation groups (*P < 0.05)
Figure 4.
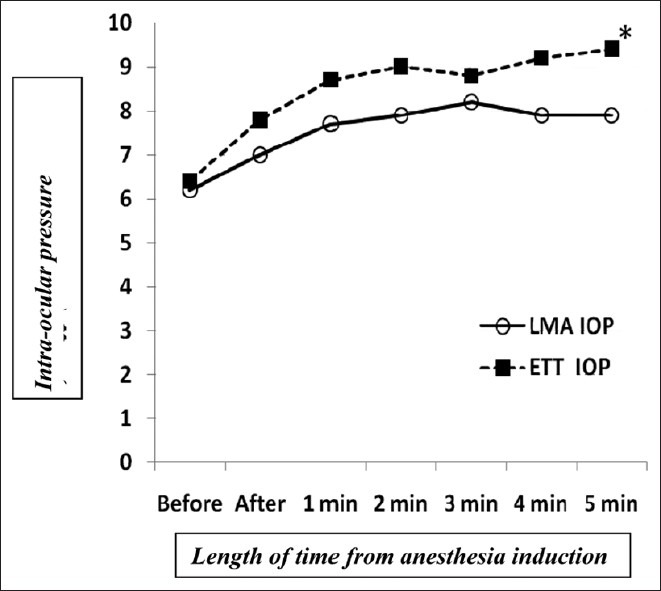
Variation of intraocular pressure in laryngeal mask airway and endotracheal intubation groups (*P < 0.05)
Figure 5.
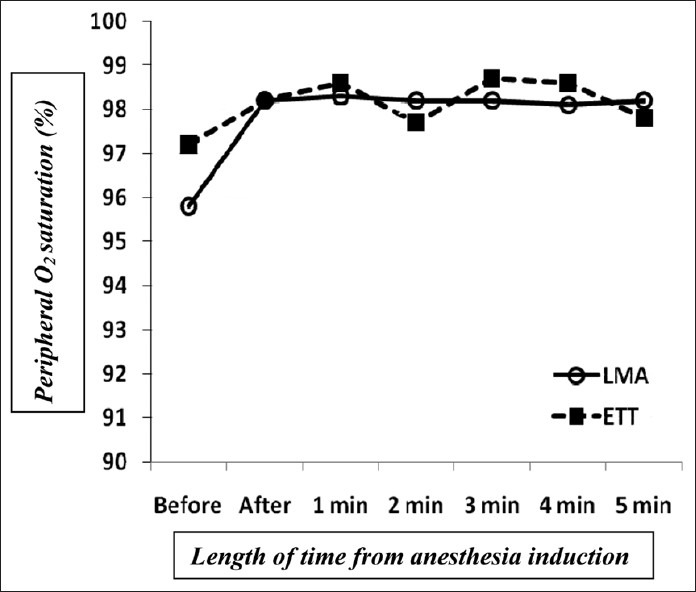
Comparison of peripheral O2 saturation in laryngeal mask airway (LMA) and endotracheal intubation groups
DISCUSSION
Most of the patients undergoing cataract extraction surgery are old, and therefore at an increased risk of adverse hemodynamic responses for airway manipulation.[1] ETT may be associated with tachycardia, hypertension, and an increase in IOP. LMA insertion is less traumatic than ETT and may provoke less sympathetic stimulation.[13,15] However, during insertion of the LMA, there is less likelihood of a blood pressure response or coughing than with conventional tracheal intubation. As a result, the increase in IOP may be diminished.[2,13]
Many studies have compared hemodynamic changes between LMA and ETT in ophthalmic surgeries; some researchers found differences and preferred LMA to ETT,[12,16–18] but others did not find any difference between LMA and ETT.[17,19] In most studies on cataract[2,11] and other ophthalmic surgeries[12,16] with various anesthetic drug combinations, there was higher increase in IOP in ETT group than in LMA group. However, Akhtar et al.[20] used propofol anesthesia and did not find significant difference in IOP in LMA and ETT groups in ophthalmic operation. Hltzschig et al.[19] administered sevoflurane and remifentanil combination and also did not find significant difference in IOP in LMA and ETT groups in strabismus surgery.
The difference in sex distribution in our study occurred by chance and it seems there is not any pathophysiologic relationship between patient gender and ease of tracheal intubation in our studied population. In our study, we used propofol and remifentanil for inducing and maintaining anesthesia both for LMA and ETT insertion. Overall, we did not find significant differences between LMA and ETT groups in SBP, DBP, HR, and IOP immediately after airway instrumentation up to 5 min, except in the 4th min in DBP, 2nd min in HR, and 5th min in IOP. Even these transient statistically significant differences in some parameters were not clinically important. “Propofol-remifentanil” is a hypnotic-analgesic combination, and if used by an experienced hand - anesthesiologist - it provides adequate anesthesia depth with acceptable hemodynamics. So, insertion of either LMA or ETT leads to minimal and similar decrease in SBP, DBP, and HR, and minimal increase in IOP in both study groups [Figures 2 and 3]. The number of patients who needed intervention to correct blood pressure variation was not different in both groups [Table 1]. Although there was good surgeon satisfaction for providing acceptable surgical field (88% in LMA group and 80% in ETT group), both study groups were similar in this point of view. Thus, we find no difference in hemodynamic and IOP changes with LMA or ETT in airway management using propofol and remifentanil for anesthesia in cataract surgery.
Some investigators evaluated various doses and combinations of propofol and remifentanil in ophthalmic surgeries and compared LMA insertion with ETT, but none of them were performed in cataract extraction surgery.[5–9,21] In our study, we compared hemodynamic and IOP changes and surgeon satisfaction in both and the number of patients who needed normalization of the blood pressure changes, and found that in both LMA and ETT groups, propofol and remifentanil combination provided good anesthesia depth with acceptable hemodynamic profile in cataract operation. Regarding lower risk of airway complications with LMA (in comparison with ETT)[4] and newer versions of LMA,[22] and also expanding the experience of administration of propofol and remifentanil in LMA insertion and removal,[23] it seems using LMA may be better than ETT for airway securing in patients who are candidates for cataract surgery.
LIMITATIONS
In this study, we measured hemodynamic parameters in the first 5 min of operation only; it is better to measure these variables through the operation period and even in recovery period. Also, our study consisted of adult population. For determining airway differences between adults and children, it is useful to conduct another investigation in pediatric patients to compare the effect of this drug combination on IOP and hemodynamic parameters.
CONCLUSION
In this study, providing acceptable anesthesia using propofol and remifentanil combination, we did not find significant differences in hemodynamic and IOP values between patients with LMA and those with ETT. Thus, considering LMA insertion is less traumatic than ETT, using LMA may be better than ETT for airway securing in patients who are candidates for cataract surgery.
ACKNOWLEDGMENTS
The authors are grateful to Vice-Chancellor for Research, Birjand University of Medical Sciences, for providing financial support for the present study (research project number 221).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC); Million hearts: Strategies to reduce the prevalence of leading cardiovascular disease risk factors --- United States, 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1248–51. [PubMed] [Google Scholar]
- 2.Motiang MJ, Rantloane JL. Intraocular pressure changes in patients undergoing cataract extraction and lens implantation: Laryngeal mask airway versus endotracheal tube. South African Journal of Anesthesia and Analgesia. 2009;15:23–7. [Google Scholar]
- 3.Ismail SA, Bisher NA, Kandil HW, Mowafi HA, Atawia HA. Intraocular pressure and haemodynamic responses to insertion of the I-gel, laryngeal mask airway or endotracheal tube. Eur J Anaesthesiol. 2011;28:443–8. doi: 10.1097/EJA.0b013e328345a413. [DOI] [PubMed] [Google Scholar]
- 4.Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: A systematic review. J Oral Maxillofac Surg. 2010;68:2359–76. doi: 10.1016/j.joms.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Yazicioglu H, Muslu S, Yamak B, Erdemli O. Laryngeal mask airway insertion with remifentanil. Acta Anaesthesiol Belg. 2005;56:171–6. [PubMed] [Google Scholar]
- 6.Bouvet L, Da-Col X, Rimmelé T, Allaouchiche B, Chassard D, Boselli E. Optimal remifentanil dose for laryngeal mask airway insertion when co-administered with a single standard dose of propofol. Can J Anaesth. 2010;57:222–9. doi: 10.1007/s12630-009-9249-9. [DOI] [PubMed] [Google Scholar]
- 7.Jeon WJ, Kim KH, Suh JK, Cho SY. The use of remifentanil to facilitate the insertion of the Cobra perilaryngeal airway. Anesth Analg. 2009;108:1505–9. doi: 10.1213/ane.0b013e31819e0248. [DOI] [PubMed] [Google Scholar]
- 8.Hall AP, Thompson JP, Leslie NA, Fox AJ, Kumar N, Rowbotham DJ. Comparison of different doses of remifentanil on the cardiovascular response to laryngoscopy and tracheal intubation. Br J Anaesth. 2000;84:100–2. doi: 10.1093/oxfordjournals.bja.a013362. [DOI] [PubMed] [Google Scholar]
- 9.Ganatra SB, D’Mello J, Butani M, Jhamnani P. Conditions for insertion of the laryngeal mask airway: Comparisons between sevoflurane and propofol using fentanyl as aco-induction agent. A pilot study. Eur J Anaesthesiol. 2002;19:371–5. doi: 10.1017/s0265021502000601. [DOI] [PubMed] [Google Scholar]
- 10.Siddiqui NT, Khan FH. Haemodynamic response to Tracheal Intubation via intubating laryngeal mask airwayversus Direct Laryngoscopic Tracheal Intubation. J Pak Med Assoc. 2007;57:11–4. [PubMed] [Google Scholar]
- 11.Whitford AM, Hone SW, O’Hare B, Magner J, Eustace P. Intra-ocular pressure changes following laryngeal mask airway insertion: A comparative study. Anaesthesia. 1997;52:794–6. doi: 10.1111/j.1365-2044.1997.186-az0317.x. [DOI] [PubMed] [Google Scholar]
- 12.Ghai B, Sharma A, Akhtar S. Comparative evaluation of intraocular pressure changes subsequent to insertion of laryngeal mask airway and endotracheal tube. J Postgrad Med. 2001;47:181–4. [PubMed] [Google Scholar]
- 13.Kiliçkan L, Baykara N, Gürkan Y, Toker K. The effect on intraocular pressure of endotracheal intubation or laryngeal mask use during TIVA without the use of muscle relaxants. Acta Anaesthesiol Scand. 1999;43:343–6. doi: 10.1034/j.1399-6576.1999.430317.x. [DOI] [PubMed] [Google Scholar]
- 14.GraphPad Software, QuikCalcs online calculators for scientists, assign subjects to groups. [Last accessed on 2011 Sep 14]. Available from: http://www.graphpad.com/quickcalcs/randomize2.cfm .
- 15.Denny NM, Gadelrab R. Complications following general anaesthesia for cataract surgery: A comparison of the laryngeal mask airway with tracheal intubation. J R Soc Med. 1993;86:521–2. [PMC free article] [PubMed] [Google Scholar]
- 16.Holden R, Morsman CD, Butler J, Clark GS, Hughes DS, Bacon PJ. Intra-ocular pressure changes using the laryngeal mask airway and tracheal tube. Anaesthesia. 1991;46:922–4. doi: 10.1111/j.1365-2044.1991.tb09847.x. [DOI] [PubMed] [Google Scholar]
- 17.Igboko JO, Desalu I, Akinsola FB, Kushimo OT. Intraocular pressure changes in a Nigerian population--effects of tracheal tube and laryngeal mask airway insertion andremoval. Niger Postgrad Med J. 2009;16:99–104. [PubMed] [Google Scholar]
- 18.Gulati M, Mohta M, Ahuja S, Gupta VP. Comparison of laryngeal mask airway with tracheal tube for ophthalmic surgery in paediatric patients. Anaesth Intensive Care. 2004;32:383–9. doi: 10.1177/0310057X0403200314. [DOI] [PubMed] [Google Scholar]
- 19.Eltzschig HK, Darsow R, Schroeder TH, Hettesheimer H, Guggenberger H. Effect of tracheal intubation or laryngeal mask airway insertion on intraocular pressure using balanced anesthesia with sevoflurane and remifentanil. J Clin Anesth. 2001;13:264–7. doi: 10.1016/s0952-8180(01)00259-8. [DOI] [PubMed] [Google Scholar]
- 20.Akhtar TM, McMurray P, Kerr WJ, Kenny GN. A comparison of laryngeal mask airway with tracheal tube for intra-ocular ophthalmic surgery. Anaesthesia. 1992;47:668–71. doi: 10.1111/j.1365-2044.1992.tb02387.x. [DOI] [PubMed] [Google Scholar]
- 21.Schäfer R, Klett J, Auffarth G, Polarz H, Völcker HE, Martin E, et al. Intraocular pressure more reduced during anesthesia with propofol than with sevoflurane: Both combined with remifentanil. Acta Anaesthesiol Scand. 2002;46:703–6. doi: 10.1034/j.1399-6576.2002.460612.x. [DOI] [PubMed] [Google Scholar]
- 22.Arslan ZI, Zdamar DO, Yildiz TS, Solak ZM, Toker KK. Tracheal intubation in morbidly obese patients: A comparison of the Intubating Laryngeal Mask AirwayÔ and Laryngeal Mask Airway CTrachÔ. Anaesthesia. 2012;67:261–5. doi: 10.1111/j.1365-2044.2011.06991.x. [DOI] [PubMed] [Google Scholar]
- 23.Ozkan D, Ergil J, Alptekin A, Aktürk N, Gümüs H. Target controlled remifentanil infusion for smooth laryngeal mask airway removal during emergence from desflurane-remifentanil anesthesia. J Anesth. 2012;26(3):369–74. doi: 10.1007/s00540-012-1346-1. [DOI] [PubMed] [Google Scholar]


