Abstract
Background:
Migraine and allergic rhinitis (AR) are two common causes of headache and facial pain that inflammatory mediators with vasoactive function play important roles in both of them. The aim of this research was to determine the prevalence of migraine in AR patients.
Materials and Methods:
In a cross-sectional comparative study performed from June to December 2010 in patients with AR sign and symptoms referred to ear, nose, throat (ENT) clinic of a university hospital in Iran-Rasht, 46 patients with positive skin prick test were compared with 60 subject without AR signs and symptoms and with negative skin test. In both the groups, history of migraine according to IHS (International Headache Society ) criteria were investigated. Analysis of data was performed by chi-sqaure and Fisher exact test by using SPSS16. Odds ratio were estimated for determining the chance of migraine in AR.
Results:
In case group (14 male, 37 female; mean age: 31.17 ± 8.31 years) and control group (23 male, 32 female; mean age: 37.58 ± 12.63 years), the prevalence of migraine was 37% and 5%, respectively. The differences in prevalence of migraine and migraine without aura between cases and controls were significant (P = 0.001). The chance of migraine in AR was 8.227 folds (95% CI: 2.38-28.42). In subjects older than 40 years old, the difference of prevalence of migraine was significant, contrary to subjects younger than 30 years old and between 30 and 39 years old.
Conclusions:
There is a correlation between migraine especially without aura and AR and this correlation is more powerful with increasing age.
Keywords: Allergic rhinitis, migraine, skin prick test test
INTRODUCTION
Ear, nose, throat (ENT) and allergy - immunology specialists frequently encounter with diagnosis of migraine headache in their patients. According to the high prevalence of migraine and allergic rhinitis (AR) in populations,[1,2] it is obvious that a noticeable proportion of the patients suffer from both conditions. But, is there any relationship between these two conditions?
Migraine is the second most common type of primary headaches that affects 18% of females and 6% of males (totally 12% of general population).[1,2] Migraine is accompanied with a mixture of neurologic, gastrointestinal, and autonomic signs and symptoms[3] and because of lack of any standard biologic marker for diagnosis of migraine, its diagnosis is based on clinical characteristics of the attacks.[1] On the other hand, allergic diseases in the upper aerodigestive tract are common, and allergy is the primary or secondary cause of complaints in 50% of patients who refer to ENT clinics and majority of patients referred to allergy clinics.[4] AR has been observed in 10%–30% of adults and up to 40% of pediatric population of United States.[2,5] In a study conducted in 2005 by use of standard questionnaire for AR, the prevalence of this disease was 14.3% in 6-7 years old and 28.2% in 12-13 years old children of Guilan province of Iran.[6]
In daily practice, we often encounter with patients who suffer from headaches assumed to have paranasal sinuses origin because of promotion with temperature changes, bilateral location, exposure to allergens, and their incidence in frontal regions[7]; but in further investigations, a noticeable proportion of self-diagnosed and doctor-diagnosed sinus headaches meet the International Headache Society (IHS) criteria for migraines, and those migraines misdiagnosed as sinus headaches respond to sumatriptan better than placebo.[8]
Obviously, many inflammatory mediators with vasoactive functions participate in these diseases, and it seems that there are some pathphysiologic similarities between these two common conditions.
Many studies have paid to the relationship between these two diseases from different perspectives, including statistical witnesses, clinical similarities, similar mechanisms and mediators, and response to similar treatments.[9–16]
In this study, we aimed to determine the prevalence of migraine, with and without aura, in AR patients compared with subjects without this.
MATERIALS AND METHODS
After approving the proposal of the research in research office and ethical committee of Guilan University of Medical Sciences (research project no. 1443), a comparative, cross-sectional study was performed in a referral- university hospital. With a significance level of 5%, the test power of 80%, and clinically difference equal to 30% (P1 = 34%, P2 = 4%), the sample size was determined to be 46 cases and 46 control subjects.
From the patients referred to the ENT clinic of Amiralmomenin Hospital in Iran-Rasht with and without clinical symptoms and signs of AR, we took written informed consents to do skin prick test (SPT) in a standard safe setting. Inclusion criteria for cases group were: positive skin test, at least one positive allergic symptom (nasal congestion, rhinorrhea, sneezing, snoring or mouth breathing, throat drainage, and itchy/watery eyes), and one aspect of the physical examination consistent with AR (allergic shiners, nasal crease, pale or boggy turbinate, mucous discharge in the nasal passage or postnasal area, or hypertrophy of posterior nasopharyngeal/oropharyngeal wall lymphoid tissues).[1,2,17] Those cases under 15 years old, pregnant cases, immunodeficient patients, and cases with known skin diseases such as psoriasis or lichen planus were not included in the study. Occurrence of dermographism was exclusion criteria. The subjects must discontinue medications such as steroids, antihistaminic medications, and tricyclic antidepressants for a defined period before entering the study. None of cases and controls was referred specifically for work-up of headache in ENT clinic.
The SPT was done by use of standard criteria and manufacturer recommendations (Allergopharma, Reinbek, Germany) in emergency ward of the hospital by an expert immunologist (RJS) who was blinded about clinical condition of the subjects. After cleaning the forearm of the subjects, one drop from the commercial solution of eight common mixtures of allergens including Grasses, Trees I, Trees II, Weed, D. farinae, D. Pteronysinus, Cladosporium, Cat and Dog epithelia (totally 23 allergens along with positive and negative controls – i.e., histamine and distinct water, respectively) were put on the skin of forearm, separately. Then the skin was pricked through the drops by use of a sterile lancet for entering a little of the allergens into the epidermis of the skin. The responses were measured 15 min later and dermal reaction above 3 mm was assumed as positive response according to the manufacturer guidelines. Those subjects who did not react to histamine drop, were assumed as “anergic” subjects, and those subjects who reacted positively to distinct water drop, were assumed as “dermographism” and both of these two situations were of exclusion criteria of the study. Those subjects who had clinical symptoms and signs of AR and positive SPT were grouped as cases, and those who had not clinical symptoms and signs of AR with negative SPT were enrolled in control group. A neurologist (AS) who was blinded for clinic and SPT results of the subjects, visited the subjects of two groups and investigated the symptoms and signs of migraine (with and without aura) in them according to IHS criteria.[18] Finally, the data were analyzed by chi-square and Fischer exact test in SPSS version 16 and the prevalence of migraine in case and control groups was determined. The odd ratio was estimated for determining the chance of migraine and its subtypes in AR.
RESULTS
From more than 80 subjects with clinical signs and symptoms of AR, 47 subjects had positive skin test, and from 65 persons without history or symptoms and signs of AR, 62 persons had negative skin test. One case from the first group and 2 subjects from the second group were excluded from the study because of occurrence of dermographism.
Finally, a total of 46 and 60 persons were enrolled in case group and control group, respectively.
The former consisted of 14 (30.4%) men and 32 (69.6%) women and the latter 23 (38.3%) men and 37 (61.7%) women (P = 0.419). The mean ( ± SD) of ages in cases was 31.17 ± 8.31 years (18–47 years old) and of controls was 37.58 ± 12.63 years (20-65 years old).
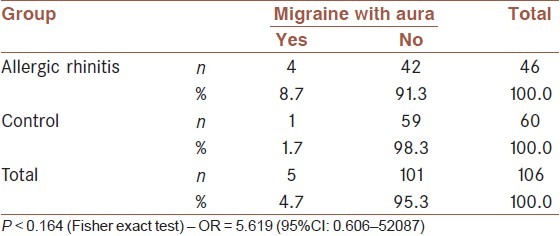
In case group, a total of 17 cases (37%) of the patients fulfilled the criteria of migraine (13 cases without aura and 4 cases with aura) but in control group, only 3 subjects (5%) had the criteria of migraine (2 without and 1 with aura). According to chi-square test, the statistical difference between these two groups was significant in the prevalence of migraine as a whole, and migraine without aura (P < 0.001 in both conditions), but Fisher's exact test did not show significant difference in frequency of migraine with aura (P = 0.164) [Tables 1 and 2]. Odd ratio for involving by migraine without aura in a population with AR was 11.42 (95% CI: 2.43-53.76) and for migraine with aura was 5.619 (0.61-52.09).
Table 1.
Comparing the prevalence of migraine without aura in patients with allergic rhinitis and nonallergic group
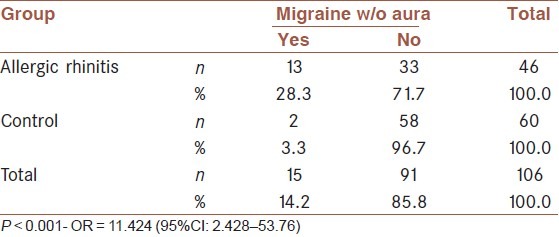
Table 2.
Comparing the prevalence of migraine with aura in patients with allergic rhinitis and nonallergic group
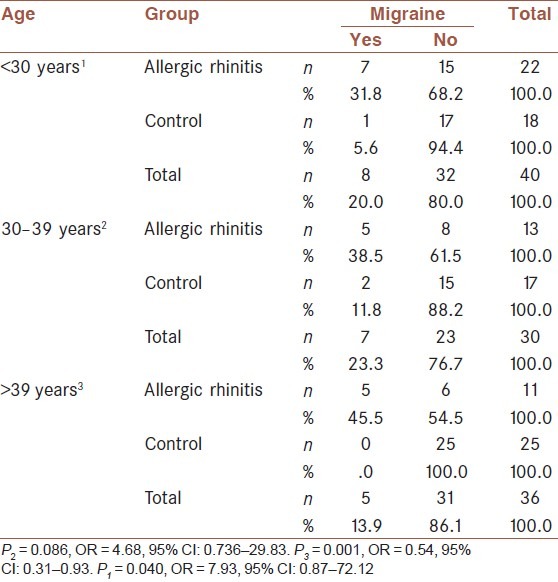
The data were analyzed in male and female groups separately, and the results were similar to the whole subjects [Table 3]. Also analysis of data was done in separate age groups (i.e., age below 30, 30-39 years old, and above 40 years old). Especially, in group above 40 years old, the difference of migraine frequency in cases and controls was significant (P < 0.001) [Table 4].
Table 3.
Comparing the prevalence of migraine in patients with allergic rhinitis and nonallergic group according to sex
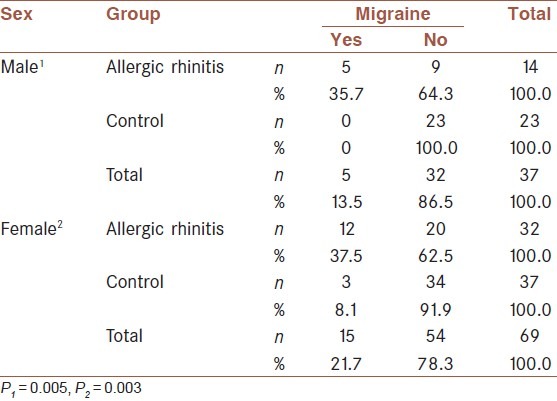
Table 4.
Comparing the prevalence of migraine in patients with allergic rhinitis and nonallergic group according to age
For omitting the effects of age and sex parameters, the Mantel-Haenszel common odd ratio and P value for the occurrence of migraine in AR were estimated (OR: 8.227, 95% CI: 2.381-28.424, P = 0.001).
DISCUSSION
In our study, 46 patients were in AR group and 60 subjects were included in control group. A total of 37% of the cases and 5% of the controls were affected by migraine (P = 0.001). The majority of migraines were without aura, and the incidence of migraine without aura between the cases and controls was different significantly (P < 0.05). The results of analysis in male and female groups were similar to the whole subjects, but considering the age, only among patients older than 40 years the difference of migraine prevalence was statistically significant. By omitting the effects of age and sex parameters the chance of migraine in allergic group was 8.227 folds (95% CI: 2.381–28.424, P = 0.001).
Migraine and AR have many clinical similarities. It was seen that among patients with sinus headache referred to otolaryngology clinics, up to 75% may have histories compatible with the migraine criterion.[13] Even in a tertiary care rhinology setting, Perry et al. found that radiography-normal and endoscopy-normal headache patients had a 58% incidence of migraine.[14] Similarly, Eross et al. reported a series of 100 consecutive self-diagnosed “sinus headache” patients and found that 86% were diagnosed as migraine or probable migraine using IHS criteria, and only 3% were found to have rhinosinusitis-attributable headaches. They also found that many migraine or probable migraine patients reported “headache triggers” such as weather changes, seasonal variation, and exposure to allergens.[7]
The reasons for this correlation may be pathophysiological resemblance between these disorders. Different studies introduced immunologic mediators such as IgE (immunoglobulin E), histamine, tumor necrosis factor-α (TNF-α), calcitonin gene related peptide (CGRP), vasoactive intestinal peptide (VIP), D2 and F2 prostaglandins, interleukin–1 (IL-1), tryptase, and also activation of mast cells and secondary release of nitric oxide in both conditions.[2,17,19–23]
In a comparative study that was performed by Ku and colleagues in cases older than 4 years, in AR group, 26 patients (34%) had headaches that met the IHS criteria for migraines, whereas only 2 patients (4%) in the non-AR group had headaches that met the criteria. Fisher's exact test showed P <0.0001, the odds ratio was calculated and found to be 14.39 (95%CI: 3.23-63.34). However, the wide confidence interval indicates that the estimation has low precision. This may be due to the relatively small number of patients in the study. They also performed a parallel study in all of the patients in the pediatric and internal medicine clinics without skin testing.[17]
Jackson and Dial have reported that 49 of 100 patients referred to their otolaryngology office for sinus headache had previously unrecognized migraine. Among them, only 13% had migraine alone, 19% (of the patients with migraine) had AR as well, 11% had sinusitis, and 6% had both AR and sinusitis.[24]
Migraine attacks may have secondary nasal parasympathetic signs. Cady and Schreiber reported objective endoscopic evidence of nasal congestion and rhinorrhea during migraine attack.[25]
In one study that was performed in Iran in 2009, among 104 patients who have sinus headaches, either self-ascribed or physician diagnosed, 72 patients (69.2%) did not have any positive sino-nasal findings in the nasal endoscopy and the computed tomography scanning. The response rate to the treatment with sodium valproate for 3 months in these patients was as follows: significant improvement in 44 patients (61.1%), partial response (9.7%), no response (15.3%), and 10 patients (13.9%) withdrew or failed to follow-up. According to Wilcoxon test, the patients’ response rate to sodium valproate was statistically significant (P = 0.001).[26]
In another study that was performed by Vincent et al. in 2010, they investigated the prevalence of migraine headache in AR patients (but not compared with a control group) and also investigated the relation between the severity of allergy/atopy with severity and frequency of migraine and the effect of immunotherapy on these parameters. Patients were categorized into high (more than 45% positive allergy tests) and low (less than 45% positive allergy tests) atopic groups based on the number of allergy tests that were positive for the frequency and disability analyses. Their study suggested that the association of allergy with migraine headaches depended upon age, degree of allergic sensitization, administration of immunotherapy, and the type of headache outcome measure that were studied. The administration of immunotherapy was associated with a decreased prevalence, frequency, and disability of migraine headache in younger subjects,[27] while in our study the correlation between migraine and AR was more significant in patients older than 40 years old. This result may be due to either the small sample size in this age group, or the increased prevalence of both disorders with increasing age, although according to the evidences, the incidence of migraine decreases with increasing age. Albeit, because of many differences in study design and the variables in two studies, the results of our study are not comparable with results of this one, and it is better to consider “severity” of migraine and AR in future studies.
The characteristic of our study is not only performing the SPT as a standard test for AR diagnosis but also the blindness of immunologist and neurologist of the study to the clinical situation and SPT results of the cases and controls. Finally, there is a noticeable restriction in our study that our control subjects with negative SPT would be positive for other allergens that were not included in our kit (false negative).
CONCLUSIONS
The prevalence and chance of migraine, especially without aura, are more in patients with AR compared with control subjects. It seems that performing more studies (e.g. interventional studies, clinical trial, and studies in specific age groups) are needed in future.
ACKNOWLEDGMENTS
The authors thank a lot from ENT-HNS Research Centre of Guilan University of Medical Sciences that aided in performing this project.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Boes CJ, Capobianco DJ, Ctrer FM, Dodick DW, Garza I, Swanson JW. Headache and Other Craniofacial Pain. In: Bradley WG, Daroff RB, Fenichel GM, Jankovic J, editors. Neurology in clinical practice. 5th ed. Philadelphia, PA: Butterworth-Heinemann; 2008. pp. 2026–42. [Google Scholar]
- 2.Mehle ME. Allergy and migraine: Is there a connection? Curr Opin Otolaryngol Head Neck Surg. 2008;16:265–9. doi: 10.1097/MOO.0b013e3282f6a629. [DOI] [PubMed] [Google Scholar]
- 3.Silberstein SD, Lipton RB, Goadsby PJ. 2th ed. 2002. Headach in clinical practice; pp. 28–55. [Google Scholar]
- 4.Mabry RL, Marple BF. Allergic rhinitis. In: Cummings CW, Flint PW, Harker LA, Haughey BH, Richardson MA, Robbins KT, editors. Cumming's otolaryngology- head & neck surgery. 4th ed. Philadelphia: Mosby Co; 2005. pp. 981–9. [Google Scholar]
- 5.Wallace DV, Dykewicz MS, Bernstein DI, Blessing-Moore J, Cox L, Khan DA, et al. The diagnosis and Management of rhinitis: An updated practice parameter. J Allergy Clin Immunol. 2008;122(2 Suppl):S1–84. doi: 10.1016/j.jaci.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Abbasi Ranjbar Z. Prevalence of allergic rhinitis signs and symptoms in children of Rasht City, Iran. J Guilan Med University. 2005;53:56–62. [Google Scholar]
- 7.Eross E, Dodick D, Eross M. The sinus, allergy and migraine study. Headache. 2007;47:213–24. doi: 10.1111/j.1526-4610.2006.00688.x. [DOI] [PubMed] [Google Scholar]
- 8.Tepper SJ. New thoughts on sinus headache. Allergy Asthma Proc. 2004;25:95–6. [PubMed] [Google Scholar]
- 9.Davey G, Sedgwick P, Maier W, Visick G, Strachan DP, Anderson HR. Association between migraine and asthma: matched case-control study. Br J Gen Pract. 2002;52:723–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Mortimer MJ, Kay J, Gawkrodger DJ, Jaron A, Barker DC. The prevalence of headache and migraine in atopic children: An epidemiological study in general practice. Headache. 1993;33:427–31. doi: 10.1111/j.1526-4610.1993.hed3308427.x. [DOI] [PubMed] [Google Scholar]
- 11.Aamodt AH, Stovner LJ, Langhammer A, Hagen K, Zwart JA. Is headache related to asthma, hay fever, and chronic bronchitis? The Head-HUNT Study. Headache. 2007;47:204–12. doi: 10.1111/j.1526-4610.2006.00597.x. [DOI] [PubMed] [Google Scholar]
- 12.Gürkan F, Ece A, Haspolat K, Dikici B. Parental history of migraine and bronchial asthma in children. Allergol Immunopathol (Madr) 2000;28:15–7. [PubMed] [Google Scholar]
- 13.Mehle ME, Kremer PS. Sinus CT scan findings in ‘sinus headache’ migraineurs. Headache. 2008;48:67–71. doi: 10.1111/j.1526-4610.2007.00811.x. [DOI] [PubMed] [Google Scholar]
- 14.Perry BF, Login IS, Kountakis SE. Nonrhinologic headache in a tertiary rhinology practice. Otolaryngol Head Neck Surg. 2004;130:449–52. doi: 10.1016/j.otohns.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 15.de Souza Carvalho D, Fragoso YD, Coelho FM, Pereira MM. Asthma plus migraine in childhood and adolescence: Prophylactic benefits with leukotriene receptor antagonist. Headache. 2002;42:1044–7. doi: 10.1046/j.1526-4610.2002.02236.x. [DOI] [PubMed] [Google Scholar]
- 16.Riccioni G, Bucciarelli T, Mancini B, Di Ilio C, D’Orazio N. Antileukotriene drugs: Clinical application, effectiveness and safety. Curr Med Chem. 2007;14:1966–77. doi: 10.2174/092986707781368522. [DOI] [PubMed] [Google Scholar]
- 17.Ku M, Silverman B, Prifti N, Ying W, Persaud Y, Schneider A. Prevalence of migraine headaches in patients with allergic rhinitis. Ann Allergy Asthma Immunol. 2006;97:226–30. doi: 10.1016/S1081-1206(10)60018-X. [DOI] [PubMed] [Google Scholar]
- 18.International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias, and facial pain. Cephalalgia. 1988;8(suppl 7):1–96. [PubMed] [Google Scholar]
- 19.Gazerani P, Pourpak Z, Ahmadiani A, Hemmati A, Kazemnejad A. A correlation between migraine, histamine, and immunoglobulin E. Iran J Allergy Asthma Immunol. 2003;2:17–24. [PubMed] [Google Scholar]
- 20.Kemper RH, Meijler WJ, Korf J, Ter Horst GJ. Migraine and function of the immune system: A meta-analysis of clinical literature published between 1966 and1999. Cephalgia. 2001;21:549–57. doi: 10.1046/j.1468-2982.2001.00196.x. [DOI] [PubMed] [Google Scholar]
- 21.Bellamy JL, Cady RK, Durham PL. Salivary levels of CGRP and VIP in rhinosinusitis and migraine patients. Headache. 2006;46:24–33. doi: 10.1111/j.1526-4610.2006.00294.x. [DOI] [PubMed] [Google Scholar]
- 22.Schuller DE, Cadman TE, Jeffreys WH. Recurrent headaches: What every allergist should know. Ann Allergy Asthma Immunol. 1996;76:219–30. doi: 10.1016/S1081-1206(10)63430-8. [DOI] [PubMed] [Google Scholar]
- 23.Levy D, Burstein R, Strassman AM. Mast cell involvement in the pathophysiology of migraine headache: A hypothesis. Headache. 2006;46(Suppl 1):S13–8. doi: 10.1111/j.1526-4610.2006.00485.x. [DOI] [PubMed] [Google Scholar]
- 24.Jackson A, Dial A. Sinus headache in an ENT setting.Poster presented. Amer Acad Neurology Annual Meeting. 2004:9–16. [Google Scholar]
- 25.Cady RK, Schreiber CP. Sinus headache: A clinical conundrum. Otolaryngol Clin North Am. 2004;37:267–88. doi: 10.1016/S0030-6665(03)00181-6. [DOI] [PubMed] [Google Scholar]
- 26.Dadgarnia MH, Atighechi S, Baradaranfar MH. The response to sodium valproate of patients with sinus headaches with normal endoscopic and CT findings. Eur Arch Otorhinolaryngol. 2010;267:375–9. doi: 10.1007/s00405-009-1090-9. Epub 2009 Sep 16. [DOI] [PubMed] [Google Scholar]
- 27.Martin VT, Taylor F, Gebhardt B, Tomaszewski M, Ellison JS, Martin GV, et al. Allergy and Immunotherapy: Are they related to migraine headache? Headache. 2011;51:8–20. doi: 10.1111/j.1526-4610.2010.01792.x. [DOI] [PubMed] [Google Scholar]


