Abstract
Objectives:
Maladaptive cognitive schemas can lead to biases during clinical assessment or psychotherapeutic interventions. This study aimed to explore the cognitive schemas among mental health professionals.
Materials and Methods:
100 mental health professionals, of both genders, equally divided between psychiatrists, psychologists, social workers, and psychiatric nurses, were approached and administered the Young Schema Questionnaire - Short Form after written informed consent.
Results:
Males had higher maladaptive schemas than female respondents across all schema domains, viz., disconnection/rejection, impaired autonomy, impaired limits, other-directedness, and overvigilance (P ≤ 0.05). Psychiatrists had higher maladaptive schemas than psychologists (P ≤ 0.05). Age was weakly but positively corelated with the schemas of self-sacrifice (P = 0.038) and unrelenting standards (P = 0.002)
Conclusions:
Mental health professionals also may have maladaptive schemas, which needs to be addressed through schema therapy.
Keywords: Cognitive schemas, core beliefs, mental health professionals
INTRODUCTION
Individuals interpret their experiences in preexisting frames of reference through which they interpret and judge things. Such frames of references or schemas are cognitive frameworks that represent our knowledge of and assumptions about the world.[1] They determine which stimuli receive attention, are encoded in memory, or are remembered in specific situations. Schemas are developed through experiences and act something like mental scaffolds, providing us with basic frameworks for processing new information and relating it to existing knowledge. Once schemas are formed, they exert strong effects on the way information is processed and interpreted. These effects, in turn, can lead to important errors and distortions in memory.[2]
Young[3,4] extended Beck's original model of cognitive schemas by identifying maladaptive schemas, which are assumed to be responsible for distorted thinking about the world, oneself, and one's relationship with others. Originally, Young[3] proposed 16 schemas based on clinical experiences. He believed that these maladaptive schemas result from the interaction between the individual's emotional temperament and aversive early life experiences and that subsequent adult psychopathology arises from initiation and maintenance of these established core beliefs.[3–5] Since these schemas influence what we attend to and how we interpret things, they can bias and distort our thoughts, perceptions, and behaviors. It is the operation of schemas that, in part, accounts for the fact that, in many cases, we are more likely to notice and remember information that supports our beliefs about the world than information that challenges them. They can therefore lead to biases and blind spots in information processing during clinical assessment or psychotherapeutic interventions.
Previous studies have evaluated cognitive schemas among both the general population and those with various psychiatric illnesses.[6–9] But less attention have been paid toward mental health professionals’ own cognitive schemas. Dysfunctional cognitive schemas may lead to cognitive vulnerabilities among mental health professionals and influence their ability to process the patients’ information in an unbiased manner. This bias may be a substantial source of error in psychotherapeutic process ratings.[10] Further, psychotherapists may have discrepancies in reporting cognitive schemas of clients,[11] which may affect the quality of treatment they provide. This study therefore attempted to explore the cognitive schemas of mental health professionals with the help of a standardized questionnaire - The Young's Schema Questionnaire Short (YSQ-S) Form.[12]
MATERIALS AND METHODS
Trainee mental health professionals of both genders, in a tertiary postgraduate training institute (n = 100) in India were invited to participate and explained the nature of the study. From a base sample of 175, 100 participants were targeted who accepted the invitation. After written informed consent, all of the participants completed the short version of the YSQ-S.[12]
The YSQ-S contains 75 items, which break down into 15 subscales addressing the following core beliefs: abandonment (a belief that one will not be protected or supported by others), mistrust/abuse (a belief that others will hurt, manipulate, or take advantage of one), emotional deprivation (a belief that one's emotional needs will not be satisfied), functional dependence (the perception that one cannot cope without support from others), vulnerability to harm (the belief that one cannot control the threat of disaster), enmeshment (perceived emotional overinvolvement with others, due to fear that one will not cope alone); defectiveness/shame (perceived defects that make one unlovable and inferior), failure to achieve (perceived inadequacy, leading to failure to meet desired goals), subjugation (others’ desires are perceived as more important than one's own), emotional inhibition (emotional expression is seen to have aversive consequences), self-sacrifice (a belief that one should focus on others’ needs, rather than one's own), unrelenting standards (a belief that one should strive to achieve impossible goals), entitlement (perception that one can act without considering others), insufficient self-control (belief that one cannot or need not control impulses and feelings), and social isolation (perceiving oneself as different and isolated from others).
Each YSQ-S item is scored on a 6-point scale. The overall score for each scale is calculated from the mean of the five items in that scale. A higher score (range 1–6) reflects a more maladaptive, unhealthy core belief. On the YSQ-S, a score of 2 or more is considered maladaptive. The internal consistency of the 15 YSQ-S scales was broadly acceptable in all four groups. In a sub-sample of our study, Cronbach's alpha exceeded 0.70 in 56 cases.
Since mental health professionals may understand the nature of the questions and give misleading answers, the questions were first coded and then jumbled up. After all responses had been recorded, the data were decoded using the original code to give the correct scores on the YSQ-S. Statistical analysis was then done by means of T-test for continuous variables and the chi-squared test for categorical variables. Corelation analysis was then carried out to determine significant corelations between the independent variables and the schemas under study using Statistical Package for Social Sciences (SPPS) Version 13.
RESULTS
A total of 100 mental health professionals, divided equally into males (49%) and females (51%), were assessed for cognitive schemas. The mean (SD) age of the respondents was 24.9 (± 3.9) years with an average psychiatric work experience of 2.8 (± 2.0) years. A third of the respondents were trainee psychiatrists (30%), another third were trainee psychologists (33%), and the rest were trainee social workers and psychiatric nurses (37%).
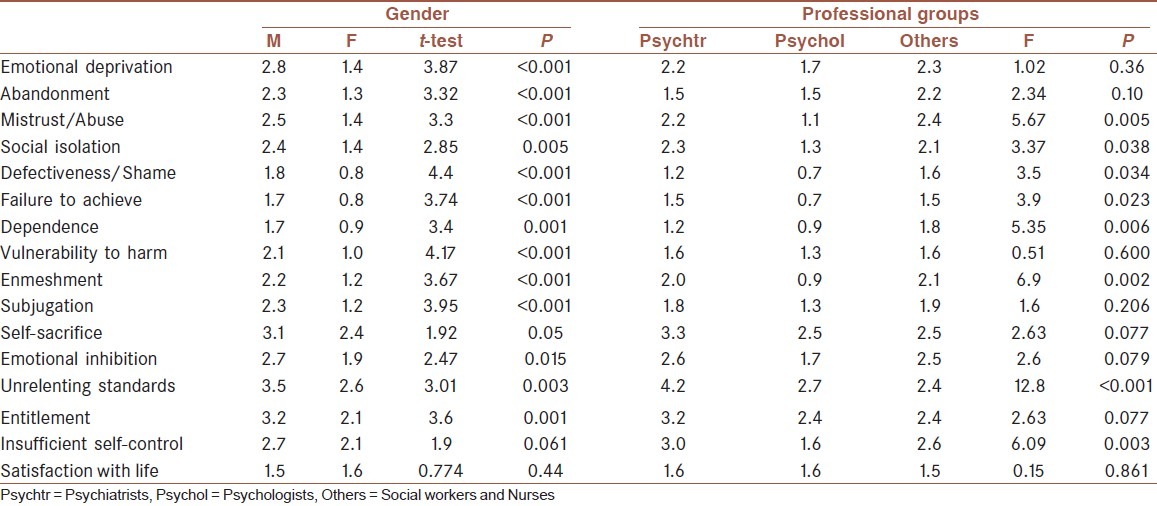
On the cognitive schemas, maladaptive scores were reported in the schemas of emotional deprivation, self-sacrifice, emotional inhibition, unrelenting standards, entitlement and insufficient self-control [Table 1]. When compared across genders, males reported higher maladaptive schemas on almost all domains with the exception of insufficient self-control and satisfaction with life which were almost equal between both sexes [Table 2]. When compared across professional groups, maladaptive schemas were reported in the domains of mistrust/abuse (psychiatrists = others > psychologists; LSD = 1.311; P = 0.002), social isolation (psychiatrists and others > psychologists; LSD: 0.996; P = 0.019), enmeshment (psychiatrists and others > psychologists; LSD = 1.141; P = 0.001), unrelenting standards (psychiatrists > psychologists and others; LSD = 1.439; P < 0.001), and insufficient self-control (psychiatrists and others > psychologists; LSD = 1.33; P = 0.001).
Table 1.
Characteristics of cognitive schemas among all respondents
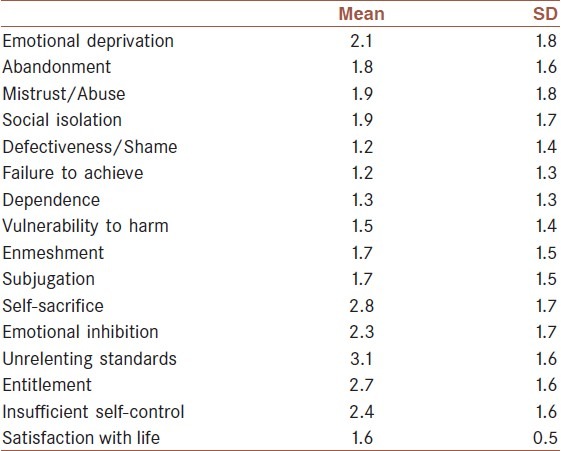
Table 2.
Comparisons of cognitive schemas between gender and professional groups
Corelation analyses revealed a weak but positive corelation of age with the schemas of self-sacrifice (Pearson's R = 0.208; P = 0.038) and unrelenting standards (Pearson's R = 0.305; P = 0.002) and a negative corelation with abandonment (Pearson's R = 0.213; P = 0.033).
DISCUSSION
Schema theory postulates that all individuals have maladaptive schemas, which are core themes or patterns that we keep repeating throughout our lives. Young,[5] in his model of cognitive schemas, theorized that there are 18 maladaptive schemas which can be grouped into 5 broad schema domains, on the basis of which core needs the schema is related to. These schema domains correspond to the basic emotional needs of a child. If these needs are not met, maladaptive schemas develop which lead to recurring patterns of reactions to life events[5]. Hence, there is a need that clinicians, especially therapists, who deal with patients and clients very closely, have little or no maladaptive schemas which may bias or prejudice their responses to their clients.
This study on mental health professionals marks probably one of the first studies to demonstrate maladaptive schemas among this important therapeutic group. This study reported that certain maladaptive schemas may exist even among mental health professionals, although they are scattered across different domains. However, two schema domains stand out as maladaptive - that of impaired limits and overvigilance/inhibition. The first believes one to be of a superior nature and the second demands maintenance of exacting standards to maintain that superiority. Both these together would suggest that our study sample felt that they were superior to the others around them and expected to maintain this superiority by following different standards.
When compared across genders, surprisingly we found higher maladaptive schemas among males when compared to females across all schema domains, viz., disconnection/rejection, impaired autonomy, impaired limits, other-directedness, and overvigilance. Similar results have however been reported[13] in earlier studies. Yet, males had equal satisfaction with life when compared to females, perhaps because they did not consider these schemas to be maladaptive and actually fitting in with their gender roles. Once again, the surprising finding of psychiatrists having more maladaptive schemas than their psychology counterparts may be due to a better psychological and psychotherapeutic alignment among psychologists compared to a greater biological belief among most psychiatrists.
Age had a positive corelation with self-sacrifice which implied that an increasing age perhaps led to an increasing sensitivity to the feelings and needs of others, often at the cost of one's own gratification. A negative corelation of abandonment with age implied that the older one got, the lesser the feeling of being abandoned as one started to become more self-sufficient across all spheres of life.
The authors believe that addressing negative schemas is essential since it may bias and prejudice clinical reasoning and judgment and can affect the therapeutic relationship. Therefore, therapists in training should also be exposed to schema therapy in order to address their own shortcomings which may prejudice their therapeutic interventions and lead to a failure of psychotherapy. Such therapies may help therapists identify and adjust their own maladaptive schemas for a better psychotherapeutic experience.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Beck AT. Depression: Causes and treatment. Philadelphia: University of Pennsylvania Press; 1967. [Google Scholar]
- 2.Beck AT. Beyond belief: A theory of modes, personality, and psychopathology.In: , editor. In: Salkovskis P, editor. Frontiers of cognitive therapy. New York: Guilford; 1996. pp. 1–25. [Google Scholar]
- 3.Young JE. Cognitive Therapy for Personality Disorder: A Schema-Focused Approach. Sarasota, FL: Professional Resource Exchange, Inc; 1990. [Google Scholar]
- 4.Young JE. Cognitive Therapy for Personality Disorders: A Schema-Focused Approach. 2nd ed. Sarasota, FL: Professional Resource Exchange; 1994. [Google Scholar]
- 5.Young JE, Klosko JS, Weishaar M. Schema Therapy: A Practitioner's Guide. New York: Guilford Publications; 2003. [Google Scholar]
- 6.Kempke S, Luyten P. Psychodynamic and cognitive-behavioral approaches of obsessive-compulsive disorder: Is it time to work through our ambivalence? Bull Menninger Clin. 2007;71:291–311. doi: 10.1521/bumc.2007.71.4.291. [DOI] [PubMed] [Google Scholar]
- 7.Pincus T, Morley S. Cognitive-processing bias in chronic pain: A review and integration. Psychol Bull. 2001;127:599–617. doi: 10.1037/0033-2909.127.5.599. [DOI] [PubMed] [Google Scholar]
- 8.Gladstone G, Parker G. Depressogenic cognitive schemas: Enduring beliefs or mood state artefacts? Aus NZ J Psychiatry. 2001;35:210–6. doi: 10.1046/j.1440-1614.2001.00883.x. [DOI] [PubMed] [Google Scholar]
- 9.Bosmans G, Braet C, Van Vlierberghe L. Attachment and symptoms of psychopathology: Early maladaptive schemas as a cognitive link? Clin Psychol Psychother. 2010;17:374–85. doi: 10.1002/cpp.667. [DOI] [PubMed] [Google Scholar]
- 10.Markin DR, Kivlighan DM., Jr Bias in psychotherapist ratings of client transference and insight. Psychotherapy (Chic) 2007;44:300–15. doi: 10.1037/0033-3204.44.3.300. [DOI] [PubMed] [Google Scholar]
- 11.Lobbestael J, Arntz A, Löbbes A, Cima M. A comparative study of patients and therapists’ reports of schema modes. J Behav Ther Exp Psychiatry. 2009;40:571–9. doi: 10.1016/j.jbtep.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Young JE. The Young Schema Questionnaire: Short Form. [Last cited in 1998]. Available from: http://www.schematherapy.com/id54.htm .
- 13.Estevez A, Calvete E, Calvete E, Estévez A. Substance use in adolescents: The role of stress, impulsivity, and schemas related to lack of limits. Adicciones. 2009;21:49–56. [PubMed] [Google Scholar]


