Abstract
Background. Syphilis has made a rapid resurgence in China, especially among high-risk groups including female sex workers (FSWs).
Methods. Two cities in each of 3 provinces in South China were chosen and allocated to intervention or control arms. The intervention consisted of enhancing community-based syphilis screening outreach intervention with comprehensive sexually transmitted infection services at designated clinics while the control maintained routine intervention activities. Generalized linear modeling was used to examine effect of the intervention on incident syphilis infection.
Results. A total of 8275 women were eligible, and 3597 women enrolled (n = 2011 in control arm, n = 1586 in intervention arm) in the study. The median follow-up duration was 375 days (interquartile range, 267–475). Syphilis incidence density in the intervention group was reduced by 70% (95% confidence interval, 53%–81%) compared with the incidence in the control arm. The syphilis prevention intervention benefits were robust among FSWs at low-tier venues, individuals with less than high school education, migrants, and women who did not report condom use during the last episode of sex.
Conclusions. Integrated sexually transmitted infection and human immunodeficiency virus prevention strategies substantially reduce syphilis incidence among FSWs, especially among those at low-tier venues. This intervention suggests the need for scaling up comprehensive FSW programs in China.
Unsafe commercial sex is a major public health problem in China, driving a resurgent syphilis epidemic [1] and expanding the sexual transmission of human immunodeficiency virus (HIV) infection [2]. Several studies among female sex workers (FSWs) in South China show high prevalence and incidence of syphilis and other sexually transmitted infections (STIs) [3–6]. Based on conservative estimates, China has >6 000 000 FSWs, [7] so the expansion of STI/HIV among FSWs has important public health consequences. Furthermore, there are great variations in sexual risk among FSWs from different types of venues in China, and FSWs at low-tier venues (defined as those who solicited clients on the street or public outdoor places) in China have a higher syphilis burden [3, 5]. The higher sexual risk associated with FSWs at low-tier venues may be related to greater numbers of clients per day, [3] less condom self-efficacy with clients that can pay extra for unsafe sex, or more migration [8, 9]. Although this group of FSWs is thought to have higher sexual risks, they are under-represented in both epidemiological studies and interventions.
Designing effective STI/HIV interventions for FSWs in China has been challenging because of FSW migration, mistrust of clinics, and limited health outreach programs [10, 11]. The compelling need for high-quality sexual health services and promising pilot STI/HIV programs in South China [12] have renewed interest in structural FSW programs. This study examined the effect of an integrated comprehensive structural STI/HIV intervention on incident syphilis and HIV infection in 6 cities of South China.
MATERIALS AND METHODS
Study Design and Participants
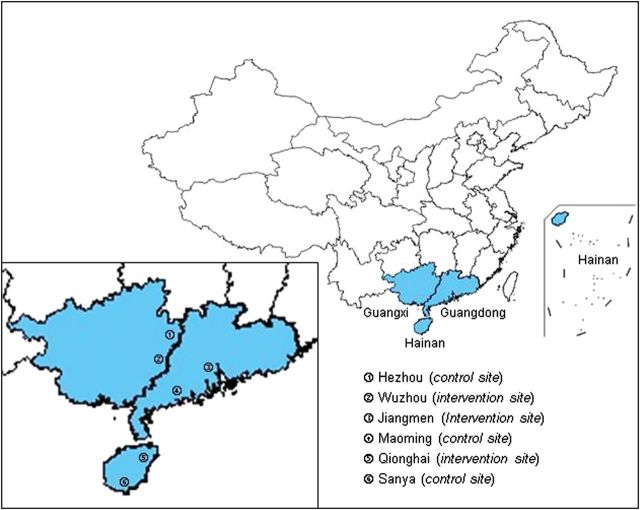
Reported primary and secondary syphilis cases have increased over the past 5 years in many parts of South China [13–15]. The study took place from June 2009 to March 2011 in 6 southern cities: Jiangmen and Maoming in Guangdong Province, Wuzhou and Hezhou in Guangxi Province, and Qionghai and Sanya in Hainan Province (Figure 1). These 6 cities were chosen because of their capacity to conduct research, supportive local health bureaus, spatial mapping of sex venues and sex worker estimates, and high prevalence of syphilis. The 2 study sites in each study province were allocated to an intervention arm or control arm. A convenience sampling strategy was used to recruit potential participants, with quotas for each tier of FSWs based on estimated total numbers of FSWs in each city. Ethics approval was obtained from the Chinese Academy of Medical Sciences Institute of Dermatology Medical Ethics Committee associated with the National STD Control Center in Nanjing, China.
Figure 1.
Geographic locations of the 6 study sites in 3 provinces.
All women aged ≥ 15 years who reported exchanging money or gifts for vaginal, oral, or anal sex with a man in the past year were eligible to participate. Women at entertainment centers and women who provided hand jobs or massages were not included unless they reported selling sex as defined above. The following were exclusion criteria for participation: unwillingness to provide informed consent; positive test for HIV by enzyme-linked immunosorbent assay (ELISA) (for the HIV incidence cohort only); and positive test for Treponema pallidum by ELISA (for the syphilis incidence cohort only). Eligible individuals were assessed by the local investigators for study eligibility at sex venues and interviewed by the same investigators for collecting sociodemographic and behavioral data. Sex worker typologies were defined based on a modification of earlier anthropological analyses of Chinese sex workers [16]. In this study, FSWs were categorized into 3 tiers according to the venues where they solicited clients. The high-tier was defined as those who solicited clients in karaoke bars or hotels; the middle-tier was defined as those who solicited clients in hair salons or barber shops, massage parlors, foot bathing shops, roadside shops, guesthouses, or roadside restaurants; the low-tier was defined as those who solicited clients on the street or at public outdoor places.
Comparability of Intervention and Control Study Arms
The 6 cities were all urban areas in South China with at least 150 000 people. Each of these cities is a destination for rural-to-urban migrants and geographically separated by at least 250 km from other cities. All cities had existing public STI clinical services that provide standardized diagnosis and treatment according to national guidelines as well as conventional health outreach program targeting FSWs. Prior FSW interventions [3] at the intervention arm were comparable with the control arm of the study that focused on syphilis/HIV testing, condom use, and harm reduction.
Syphilis and HIV Testing
All women who agreed to participate in this study had whole blood drawn either in the clinic or onsite at a sex venue every 3 months. Blood specimens were stored temporarily before delivering to the local qualified STI and HIV laboratories for testing. Specimens were screened using a T. pallidum ELISA (Wantai) and HIV ELISA (Wantai). Positive T. pallidum tests were confirmed with a nontreponemal TRUST test (Rongsheng) to determine those positive for both treponemal and nontreponemal tests, and syphilis seroconversion was defined as changing from negative ELISA to positive ELISA and positive TRUST. Positive HIV tests were confirmed with a Western blot, and HIV seroconversion was defined as changing from negative ELISA to positive ELISA and positive Western blot. All syphilis and HIV infections were managed according to national guidelines.
Intervention and Control Conditions
Women in the control group received routine health outreach programs (ie, provision of condoms and health education materials), whereas the intervention group additionally received a comprehensive structural prevention package that included the following: health promotion though television and newspaper to increase awareness and health-seeking behaviors; regular syphilis screening for those who did not get any screening in the previous 3 months through monthly outreach services at the settings to include FSWs outside of the cohort; and strengthened connection between outreach and clinical STI services through enhanced referral services (Table 1).
Table 1.
Activities Conducted as Intervention Measures in the Intervention Arm
| Intervention Item | Contents |
|---|---|
| Health promotion | In addition to routine practice of providing HIV and STI information during special events such as World AIDS Day, regular deliveries of the news about this study project through local television programs and newspapers, emphasizing provision of free syphilis testing and treatment |
| Deliveries of STI-specific health education materials in sex venues through regular outreach services | |
| Syphilis screening | On-site screening of syphilis with point-of-care tests |
| Provision of screening results | |
| Referral services | Provision of free gynecologic exams and reproductive services |
| Referral of FSWs with positive screening results to the designated STI clinics | |
| Referral of FSWs with any STI symptoms to the designated STI clinics | |
| STI services | Provision of free diagnosis and treatment of syphilis to FSWs referred from sex venues at the designated STI clinics |
| Provision of free diagnosis and treatment of syphilis to all other patients attending the designated STI clinics, including male clients of FSWs |
Abbreviations: FSW, female sex worker; HIV, human immunodeficiency virus; STI, sexually transmitted infection.
Baseline and Follow-Up Survey
The baseline survey questionnaire consisted of 17 items that have been used before among South Chinese FSWs [17] and included questions about sociodemographics, sexual behaviors, and other STI/HIV risk behaviors. Women who were followed for at least 2 visits and filled out a survey at each visit were included in the final analysis.
Follow-Up and Endpoints
Women were followed in the clinic or community, receiving phone calls monthly and syphilis/HIV testing every 3 months. In our sample, 98.4% of all women had a cell phone number. Given the high rates of migration among FSW in China, we used several methods to increase follow-up: monthly calls by health outreach workers including $8 worth of call time for each connection; free health tests such as hepatitis B virus testing and gynecological examination; subsidies to cover the cost of transportation to clinics; and free cosmetic products and skin lotions. Women who changed their phone numbers were encouraged to provide their new phone numbers to the project. Women who did not have cell phones either shared cell phones or provided a landline phone number for contact.
Statistical Analysis
The sample size was calculated to give 0.9 power to detect a risk reduction of 5% between the intervention and control arms in incidence of syphilis at 1 year, assuming a lost-to-follow-up rate of approximately 30% at 6 months. Total numbers of FSWs in each city were estimated prior to study launch based on mapping exercises. Because FSWs at low-tier venues are known to have higher sexual risk, this group was oversampled compared with those at middle and high-tier venues.
The primary outcome in the analysis was incident syphilis. Only 1 syphilis infection per patient was counted in the estimation of the syphilis outcome. Syphilis incidence was estimated by using the number of seroconversions within the follow-up period as the numerator and the cohort's total number of person-year exposure to the risk of syphilis transmission as the denominator. For those with seroconversion, half of the follow-up duration (between the 2 visits) was used as their contribution to the total risk exposure. The 95% confidence interval (CI) of the incidence was estimated using the Poisson method. Risk factors for syphilis seroconversion were identified by generalized linear modeling. Adjusted relative risk (RR) with 95% CIs was estimated. A P value ≤ 5% was considered statistically significant. Kaplan-Meier analysis was used to compare cumulative proportion of syphilis-free over time between the intervention and control groups. All analyses were done with SPSS 18.0.
RESULTS
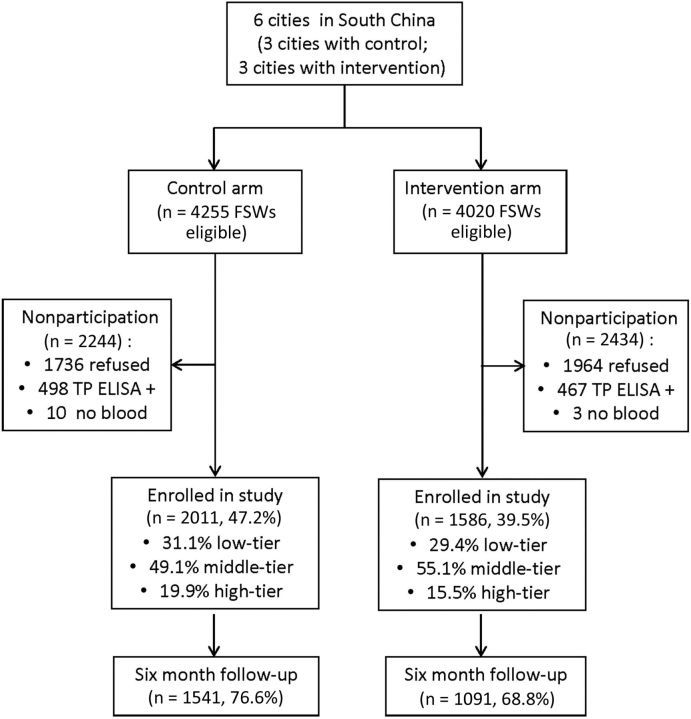
A total of 8275 FSWs were approached to participate in the syphilis cohort (Figure 2). The study overenrolled FSWs at low-tier venues, who represented 23.4% of all FSWs at baseline. A total of 3597 syphilis-negative women were enrolled in the syphilis cohort (n = 2011 in control cities, n = 1586 in intervention cities). Among those who were eligible, 52.7% (2244 of 4255) of those in the control arm and 60.5% (2434 of 4020) of those in the intervention arm did not participate in the study. Reasons for not participating in the syphilis cohort included refusal (3700, 79.1%), syphilis infection at baseline (965, 20.6%), and no blood sample (13, 0.3%). In the control arm, 76.6% of participants completed the 6-month follow-up, and 68.8% of the participants in the intervention arm completed the 6-month follow-up. The overall retention rate was 50.2% at 12 months, and the median follow-up period among all FSWs was 375 days (interquartile range, 267-475 days).
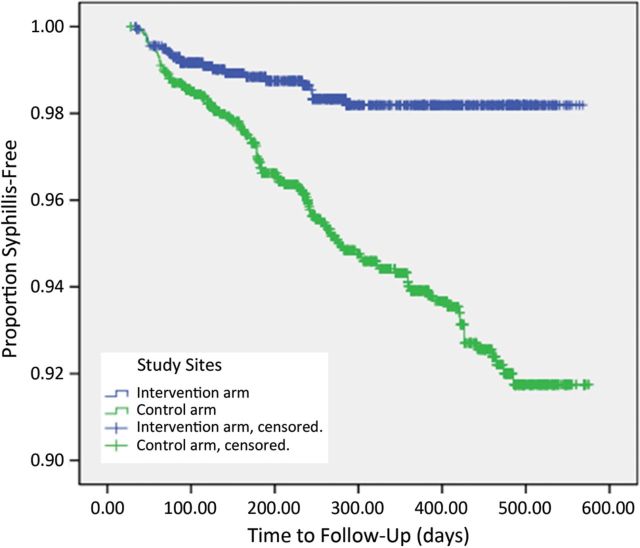
Figure 3.
Kaplan–Meier curves for the intervention and control arms.
Figure 2.
Flow chart of the female sex worker (FSW) intervention with a focus on the syphilis incidence cohort. TP ELISA + , positive Treponema pallidum enzyme-linked immunosorbent assay.
The baseline prevalence rates of syphilis were found to be 2.8% (95% CI, 1.9%–3.7%), 4.5% (95% CI, 3.6%–5.4%), and 12.4% (95% CI, 10.4%–14.4%) among FSWs at high-, middle-, and low-tier venues, respectively. The baseline sociodemographic characteristics, behaviors, and biomarkers of the intervention and control groups for the syphilis cohort are reported in Table 1. Women in the intervention group reported less-frequent condom use and less married status than control group women, and the group contained more migrants at baseline than the control group (Table 1). Age, ethnicity, and other sociodemographic variables were comparable between the intervention and control groups. Within the syphilis cohort (n = 3597), 2 of 2011 women in the control group had HIV infection at baseline compared with 5 of 1586 women in the intervention group (P = .28). The distribution of FSWs at low- and middle- or high-tier venues in this trial were comparable in the control and intervention groups (Tables 2 and 3).
Table 2.
Baseline Sociodemographic, Sexual Behavior, and HIV Prevalence Among Female Sex Workers (FSWs) in the Syphilis Cohort (n = 3597)a
| Variables | Control Group (n = 2011) | Intervention Group (n = 1586) | P Value |
|---|---|---|---|
| Age in years, mean ± SD | 26.2 | 27.3 | |
| Ethnicity | |||
| Han | 1703 (84.7) | 1316 (83.0) | .18 |
| Non-Han | 308 (15.3) | 270 (17.0) | |
| Education | |||
| Primary school | 354 (17.6) | 328 (20.7) | .06 |
| Middle school | 1404 (69.8) | 1059 (66.8) | |
| ≥High school | 253 (12.6) | 199 (12.5) | |
| Marital status | |||
| Married | 1350 (67.1) | 906 (57.1) | <.01 |
| Unmarried | 661 (32.9) | 680 (42.9) | |
| Resident status | |||
| Migrantb | 1398 (69.5) | 1197 (75.5) | <.01 |
| Nonmigrant | 613 (30.5) | 389 (24.5) | |
| Self-reported condom use with client at last sex | |||
| Yes | 1548 (77.0) | 1009 (63.6) | <.01 |
| No | 368 (18.3) | 480 (30.3) | |
| Drug use | |||
| Yes | 109 (5.4) | 73 (4.6) | .30 |
| No | 1902 (94.6) | 1513 (95.4) | |
| FSW typologyc | |||
| Low-tier | 623 (31.0) | 466 (29.4) | .32 |
| Middle- or high-tier | 1388 (69.0) | 1120 (70.6) | |
| HIV infectiond | |||
| Positive | 2 (0.1) | 5 (0.3) | .28 |
| Negative | 2009 (99.9) | 1581 (99.7) |
Data are no. (%) unless otherwise indicated.
Abbreviations: HIV, human immunodeficiency virus; SD, standard deviation.
a Missing data accounted for <5% of each variable with the exception of condom use at last sex (224, 5.6%) and condom use frequency (247, 6.1%).
b Migrant defined as not having a local city registration permit.
c FSW typology defined by sex venue as described in the text.
d HIV infection defined by positive enzyme-linked immunosorbent assay and positive Western blot.
Table 3.
Baseline Syphilis Prevalence by Female Sex Worker Type in Control and Intervention Groups
| Variable | Intervention Arm, No. (%) | Control Arm, No. (%) | P Value | |
|---|---|---|---|---|
| City | City | |||
| Wuzhou | 40/852 (4.7) | Hezhou | 100/826 (12.1) | .001 |
| Jiangmen | 17/534 (3.2) | Maoming | 42/825 (5.1) | .09 |
| Qionghai | 32/630 (5.1) | Sanya | 27/809 (3.3) | .10 |
| Tiera | Tier | |||
| High-tier | 19/591 (3.2) | High tier | 21/824 (2.6) | .46 |
| Middle-tier | 24/928 (2.6) | Middle-tier | 67/1108 (6.1) | .001 |
| Low-tier | 46/497 (9.3) | Low-tier | 81/528 (15.3) | .003 |
a Tier defined by sex venue as described in the text.
Among the FSWs in the intervention cities, 90.9%–91.8% (90.0%–90.4% of FSWs at high-tier, 90.7%–94.1% of middle-tier, and 93.0%–95.5% of low-tier venues) were covered by the comprehensive structural prevention provided by the outreach team. Of them, 75.4%–87.8% (72.8%–86.0% of FSWs at high-tier, 84.5%–88.9% of middle-tier, and 71.4%–86.0% of low-tier venues) were screened for syphilis, and 79.5%–100.0% of infected cases (60.7%–100.0% of FSWs at high-tier, 87.1%–100.0% of middle-tier, and 91.7%–100.0% of low-tier venues) were treated for syphilis.
A total of 132 incident syphilis infections were detected over the course of the study, with 109 in the control group and 23 in the intervention group, giving syphilis incidence densities of 1.85 per 100 person-years (95% CI, 1.79–1.94 per 100 person-years) in the intervention group and 6.14 per 100 person-years (95% CI, 6.09–6.19 per 100 person-years) in the control group. The highest incidence density of 8.87 per 100 person-years (95% CI, 8.76–8.98 per 100 person-years) was found among FSWs at low-tier venues in the control group. Syphilis incidence in the intervention group was reduced by 70% compared with the control group (adjusted RR, 0.30; 95% CI, .19–.47). The result of Kaplan-Meier analysis on cumulative proportions of syphilis-free FSWs between the intervention and control groups are shown in Figure 3. Correlates of incident syphilis are shown in Table 4. The effect of the intervention was unrelated to the cities (P < .05 for all city pairs). A significant syphilis incidence reduction in the intervention group compared with the control group was noted among those aged ≤45 years, all education levels, married and unmarried individuals, FSWs at low- and middle-tier venues, migrants, Han and non-Han ethnicities, and those who reported different levels of condom use. A significant syphilis incidence reduction could not be detected among individuals aged ≥46 years, drug users, FSWs at high-tier venues, and nonmigrants, although there were only 38 women aged ≥46 years old and 173 drug users.
Table 4.
Factors Associated With Incident Syphilis From a Generalized Linear Model
| Control Arm |
Intervention Arm |
|||||
|---|---|---|---|---|---|---|
| Person-Years | Rate per 100 Person-Years (95% CI) | Person-Years | Rate per 100 Person-Years (95% CI) | Relative Risk Reduction (95% CI) | P Value | |
| Overall | 1775 | 6.14 (6.09–6.19) | 1241 | 1.85 (1.79–1.91) | 70 (53–81) | <.001 |
| Age, years | ||||||
| 15–30 | 1397 | 5.37 (5.31–5.43) | 914 | 1.86 (1.79–1.93) | 65 (41–79) | <.001 |
| 31–45 | 352 | 8.81 (8.69–8.93) | 316 | 1.58 (1.45–1.71) | 82 (54–93) | <.001 |
| ≥46 | 26 | 11.54 (11.15–11.93) | 11 | 9.09 (8.40–9.78) | 22 (0–92) | .83 |
| Education | ||||||
| ≤Primary | 287 | 9.41 (9.28–9.54) | 265 | 1.51 (1.38–1.64) | 84 (51–94) | .001 |
| Middle | 1257 | 5.65 (5.59–5.71) | 835 | 1.68 (1.60–1.76) | 70 (47–83) | <.001 |
| ≥High School | 231 | 4.76 (4.63–4.89) | 141 | 3.55 (3.35–3.75) | 25 ( 0–74) | <.001 |
| Marital status | ||||||
| Married | 562 | 8.90 (8.81–8.99) | 542 | 2.40 (2.31–2.49) | 73 (50–85) | <.001 |
| Unmarried | 1213 | 4.86 (4.80–4.92) | 699 | 1.43 (1.35–1.51) | 71 (42–85) | <.001 |
| FSW tiera | ||||||
| Low | 462 | 8.87 (8.76–8.98) | 382 | 3.40 (3.29–3.51) | 62 (28–79) | .003 |
| Middle | 886 | 7.34 (7.27–7.41) | 707 | 1.27 (1.19–1.35) | 83 (65–91) | <.001 |
| High | 427 | 0.70 (.61–.79) | 152 | 0.66 (.46–.86) | 6 (0–90) | .96 |
| Resident status | ||||||
| Migrantb | 1282 | 6.55 (6.49–6.61) | 924 | 1.52 (1.45–1.59) | 77 (59–87) | <.001 |
| Nonmigrant | 493 | 5.07 (4.97–5.17) | 317 | 2.84 (2.72–2.96) | 44 (0–74) | .14 |
| Ethnicity | ||||||
| Han | 1514 | 5.75 (5.70–5.80) | 1013 | 1.88 (1.81–1.95) | 67 (46–80) | <.001 |
| Non-Han | 261 | 8.43 (8.30–8.56) | 228 | 1.75 (1.61–1.89) | 79 (39–93) | .004 |
| Last condom usec | ||||||
| Yes | 1388 | 6.12 (6.06–6.18) | 761 | 1.97 (1.89–2.05) | 68 (44–81) | <.001 |
| No | 307 | 5.86 (5.74–5.98) | 403 | 1.74 (1.63–1.85) | 70 (29–88) | .006 |
| Refuse to answer | 80 | 7.50 (7.26–7.74) | 77 | 1.30 (1.05–1.55) | 83 (0–98) | .11 |
| Condom use frequencyd | ||||||
| 100% | 1131 | 4.95 (4.89–5.01) | 325 | 1.54 (1.41–1.67) | 69 (22–87) | .01 |
| Not 100% | 553 | 8.14 (8.05–8.23) | 831 | 2.05 (1.98–2.12) | 75 (56–86) | <.001 |
| Refuse to answer | 92 | 8.70 (8.48–8.92) | 85 | 1.18 (.94–1.42) | 87 (0–98) | .06 |
| Drug usee | ||||||
| Yes | 83 | 9.64 (9.39–9.89) | 50 | 2.00 (1.67–2.33) | 79 (0–98) | .14 |
| No | 1692 | 5.97 (5.92–6.02) | 1191 | 1.85 (1.79–1.91) | 69 (51–80) | <.001 |
Abbreviations: CI, confidence interval; FSW, female sex worker.
a Tier defined by sex venue and fee per client as described in the text.
b Migrant defined as not having a local city registration permit.
c During the last episode of sexual intercourse, used a condom.
d Defined as women reporting 100% condom use or not in the past 12 months.
e Used any form of drugs in the past 12 months.
This study also analyzed incident HIV infection, finding no significant difference when comparing the control and intervention groups, although the incidence in the intervention group was slightly less than that in the control group (adjusted RR, 0.35; 95% CI, .03–3.13; P = .35). A total of 5 incident HIV infections were detected, with 4 in the control group (out of 2219 HIV-negative individuals) and 1 in the intervention group (out of 1801 individuals). The majority (4 of 5) of the incident HIV cases were found among FSWs at low-tier venues, 1 in the intervention group and 3 in the control group.
An analysis of loss to follow-up found no significant difference in syphilis infection between women who were present and those lost to follow-up at 6 months (P = .94).
DISCUSSION
This is one of the largest FSW interventions and the first in China to have sufficient follow-up to measure syphilis and HIV incidence. This study represents a marked departure from earlier FSW interventions in China by virtue of its higher recruitment rate, improved retention, measurement of syphilis and HIV incidence, and oversampling of FSWs from low-tier sex venues [3, 18–20]. One study reported approaching 13 785 FSWs but enrolling only 977 (7.1%), [18] making our enrollment rate of 49.3% (3597 of 7297) a substantial improvement. Despite the importance of better understanding FSW STI and HIV needs and testing interventions, this is, to our knowledge, only the second Chinese FSW cohort described in the English literature [21]. This study is also important because it provides a more robust understanding of the sexual risk and social composition of FSWs at low-tier sex venues, a group that has been difficult to accurately study in China [11] and that is less well represented in current surveillance and intervention programs in China.
There are several aspects of the community intervention that may have contributed to its effectiveness. First, whereas most traditional FSW interventions have focused on condom use and increasing individual HIV knowledge, [20] this community structural intervention focused on creating mutual trust and sustainable connections between sex venues and STI clinics. Especially in local contexts where private clinics may not have standardized STI services or licensed doctors, [22] re-establishing trust and relationships with local standardized STI clinics may have been a powerful force in preventing syphilis. The referral systems established at intervention sites may have facilitated this trust. Second, although sexual health was the focus of our measured outcomes, these components were only a portion of a broader comprehensive package of health and well-being services that included free gynecological exams and reproductive services at sex venues. Third, implementing concomitant programs for male STI patients in each of the cities may have provided greater leverage for FSWs to mandate condom use with clients.
This study further demonstrates a higher sexual risk of syphilis infection and probably HIV infection as well among FSWs at low-tier venues, which has implications for surveillance and intervention programs in FSWs. This trend has been observed in several other studies [3, 5], but previous studies have been limited by their small sample sizes and cross-sectional designs.
The overall follow-up rates in our study (73.1% of FSWs at 6 months and 50.2% of FSWs at 12 months) are far better than those for the other FSW cohort in China, which was able to follow 53% at approximately 6 months [21]. Higher FSW retention rates in our study may be partly attributed to the gains from mobile phone use, such as text message appointment reminders and health behavior promotion. Mobile phones have been used among STI and HIV risk groups in other contexts to promote retention and behavior change [23]. Although other research has suggested that online methods could be used for STI and HIV prevention in China, [24] our experience found higher levels of mobile phone use among FSWs, especially FSWs at low-tier venues.
This study has several limitations. First, the study was only implemented in 6 urban regions located in South China, and care must be taken when generalizing the findings to other areas. At the same time, other research has suggested that China's primary and secondary syphilis cases are substantially greater in urban regions than in rural areas [13, 15] Second, although every effort was made to make the intervention and control groups as comparable as possible, they were not identical. The intervention group had a higher syphilis prevalence than the control group at baseline. Third, we cannot know with certainty which aspects of the structural intervention were essential drivers of behavior change and syphilis prevention. Although no measures of FSW condom negotiation were measured, FSW condom use increased over time. Furthermore, there was some flexibility provided to the 3 intervention sites to allow the program to adapt to local circumstances and needs.
This research study demonstrates the efficacy and potential public health benefits in prevention and control of syphilis through providing expanded comprehensive structural interventions for FSWs in South China. However, there are still many unanswered questions, such as feasibility in scaling up of the structural interventions and the cost-effectiveness of these strategies, in this field that require further investigation in order to translate the evidence from this multicity study to national or local policies and to bring the findings of the study to the millions of FSWs across China. The new National Syphilis Control Plan [25] in China holds great promise for realizing these goals.
Notes
Acknowledgments. The authors wish to acknowledge the following members of the study team: Guo-Cheng Zhang, Zhi-Ju Zheng, Feng-Qin Ge, Wan-Hui Wei, Mei-Qin Shi, Hong-Chun Wang, Xue-Qin Dai, Ming-Ying Zhong,Yan Han, Shao-Chun Chen, Ning-Xiao Cao, Pei-Wen Sun, and Ping Yang from the National Center for STD Control in Nanjing; JianZhong, Jie Lin, Bing-Jian Liang, Yi-Hai Chen, Shu-Jun Ye, Gui-ping Rao, Feng Li, Gui-Biao Huang,Lin-Lin Tan, Yun-Ming Hu, and ZiZeng from the Guangxi sites; He-Ping Zheng, Cheng Wang, Xu-Qi Ren, Zheng-Jun Zhu, Guang-Wei Wu, He-Kun Lu, Mei-Lin Chen, Shu-Jie Huang, Hai-Qing Yang, Wei-Guang Dong, Wei-Jun Deng, and Qi-Shan Chen from the Guangdong sites; Yu-Jun Xu, Na Zhong, Hai-Wei Xu, You-Shu Lin, Li-Ming Wang, Hua-Bo Li, Ji-Wen Zheng, He-Fa Fan, Ling Wang, Ling He, Shi-Zhou Ling, Xue-Liang Wang, and Ying-Liang Chen from the Hainan sites; and Geng-Feng Fu from the Jiangsu Center for Disease Control.
Financial support. This work was supported by the Mega Project of China National Science Research for the 11th Five-Year Plan (2008ZX10001–005) from the Ministry of Health and the Ministry of Sciences and Technology in China.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Tucker JD, Chen XS, Peeling RW. Syphilis and social upheaval in China. N Engl J Med. 2010;362:1658–61. doi: 10.1056/NEJMp0911149. [DOI] [PubMed] [Google Scholar]
- 2.Wang N, Wang L, Wu Z, et al. Estimating the number of people living with HIV/AIDS in China: 2003–09. Int J Epidemiol. 2010;39(Suppl 2):ii21–8. doi: 10.1093/ije/dyq209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Q, Yang P, Gong XD, Jiang J, Yang B. Syphilis prevalence and high risk behaviors among female sex workers in different settings. China J AIDS STDs. 2009;15:398–400. [Google Scholar]
- 4.Li Y, Detels R, Lin P, et al. Prevalence of HIV and STIs and associated risk factors among female sex workers in Guangdong Province, China. J Acquir Immune Defic Syndr. 2010;53(Suppl 1):S48–53. doi: 10.1097/QAI.0b013e3181c7d72f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang H, Zhi X, Chen X-S, Cohen MS. Systematic review and meta-analysis of syphilis seroprevalence among female sex workers in China. 2010 NIH Fogarty International Clinical Scholar Conference (Bethesda, MD). Bethesda, MD, National Institutes of Health. [Google Scholar]
- 6.Gao L, Che Z, Lu Y. A cross-sectional study on STD/HIV among 270 female sex workers. J Dermatol Venereol. 2008;30:39–42. [Google Scholar]
- 7.Ministry of Health of the People's Republic of China. Beijing: 2010. China 2010 UNGASS Country Progress Report. [Google Scholar]
- 8.Yang X, Xia G. Gender, work, and HIV risk: determinants of risky sexual behavior among female entertainment workers in China. AIDS Educ Prev. 2006;18:333–47. doi: 10.1521/aeap.2006.18.4.333. [DOI] [PubMed] [Google Scholar]
- 9.Yang X, Xia G, Li X, Latkin C, Celentano D. Social influence and individual risk factors of HIV unsafe sex among female entertainment workers in China. AIDS Educ Prev. 2010;22:69–86. doi: 10.1521/aeap.2010.22.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weeks MR, Liao S, Li F, et al. Challenges, strategies, and lessons learned from a participatory community intervention study to promote female condoms among rural sex workers in Southern China. AIDS Educ Prev. 2010;22:252–71. doi: 10.1521/aeap.2010.22.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tucker JD. The social context of sexual HIV prevention among female sex workers in China. Int J Epidemiol. 2011;40:1421–2. doi: 10.1093/ije/dyr021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tucker JD, Yang LG, Yang B, et al. A twin response to twin epidemics: integrated HIV/syphilis testing at STI clinics in South China. J Acquir Immune Defic Syndr. 2011;57:e106–11. doi: 10.1097/QAI.0b013e31821d3694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen ZQ, Zhang GC, Gong XD, et al. Syphilis in China: results of a national surveillance programme. Lancet. 2007;369:132–8. doi: 10.1016/S0140-6736(07)60074-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tan N, Messina JP, Yang L, et al. A spatial analysis of county-level variation in syphilis and gonorrhea in Guangdong Province. China PloS ONE. 2011;6:e19648. doi: 10.1371/journal.pone.0019648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang LG, Tucker JD, Yang B, et al. Primary syphilis cases in Guangdong Province 1995–2008: opportunities for linking syphilis control and regional development. BMC Public Health. 2010;10:793. doi: 10.1186/1471-2458-10-793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang Y, Henderson GE, Pan S, Cohen MS. HIV/AIDS risk among brothel-based female sex workers in China: assessing the terms, content, and knowledge of sex work. Sex Transm Dis. 2004;31:695–700. doi: 10.1097/01.olq.0000143107.06988.ea. [DOI] [PubMed] [Google Scholar]
- 17.Chen XS, Yin YP, Tucker JD, et al. Detection of acute and established HIV infections in sexually transmitted disease clinics in Guangxi, China: implications for screening and prevention of HIV infection. J Infect Dis. 2007;196:1654–61. doi: 10.1086/522008. [DOI] [PubMed] [Google Scholar]
- 18.Rou K, Wu Z, Sullivan SG, et al. A five-city trial of a behavioural intervention to reduce sexually transmitted disease/HIV risk among sex workers in China. AIDS. 2007;21(Suppl 8):S95–101. doi: 10.1097/01.aids.0000304703.77755.c7. [DOI] [PubMed] [Google Scholar]
- 19.Wu Z, Rou K, Jia M, Duan S, Sullivan SG. The first community-based sexually transmitted disease/HIV intervention trial for female sex workers in China. AIDS. 2007;21(Suppl 8):S89–94. doi: 10.1097/01.aids.0000304702.70131.fa. [DOI] [PubMed] [Google Scholar]
- 20.Hong Y, Li X. HIV/AIDS behavioral interventions in China: a literature review and recommendation for future research. AIDS Behav. 2009;13:603–13. doi: 10.1007/s10461-008-9483-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma S, Dukers NH, van den Hoek A, et al. Decreasing STD incidence and increasing condom use among Chinese sex workers following a short term intervention: a prospective cohort study. Sex Transm Infect. 2002;78:110–4. doi: 10.1136/sti.78.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tucker JD, Yang LG, Zhu ZJ, et al. Integrated syphilis/HIV screening in China: a qualitative analysis. BMC Health Services Research. 2010;10:58. doi: 10.1186/1472-6963-10-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swendeman D, Rotheram-Borus MJ. Innovation in sexually transmitted disease and HIV prevention: internet and mobile phone delivery vehicles for global diffusion. Curr Opin Psychiatry. 2010;23:139–44. doi: 10.1097/YCO.0b013e328336656a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hong Y, Li X, Fang X, Lin X, Zhang C. Internet use among female sex workers in China: implications for HIV/STI prevention. AIDS Behav. 2011;15:273–82. doi: 10.1007/s10461-010-9846-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beijing. 2010. China Ministry of Health. National Program of Syphilis Prevention and Control in China (Years 2010–2020) http://www.china.com.cn/policy/txt/2010-06/21/content_20305839.htm , accessed 24 July 2012. [Google Scholar]