Abstract
Our objective was to examine the impact of a videobooklet patient decision aid supplemented by an interactive values clarification exercise on decisional conflict in patients with knee osteoarthritis (OA) considering total knee arthroplasy. 208 patients participated in the study (mean age 63 years; 68% female; 66% White). Participants were randomized to 1 of 3 groups: (1) Educational booklet on OA management (control); (2) Patient decision aid (videobooklet) on OA management; and (3) Patient decision aid (videobooklet) + adaptive conjoint analysis ACA tool. The ACA tool enables patients to consider competing attributes (i.e. specific risks/benefits) by asking them to rate a series of paired-comparisons. The primary outcome was the decisional conflict scale ranging from 0 to 100. Differences between groups were analyzed using analysis of variance (ANOVA) and Tukey's honestly significant difference tests. Overall, decisional conflict decreased significantly in all groups (p<0.05). The largest reduction in decisional conflict was observed for participants in the videobooklet decision aid group (21 points). Statistically significant differences in pre vs. post-intervention total scores favored the videobooklet group compared to the control group (21 vs. 10) and to the videobooklet plus ACA group (21 vs. 14; p<0.001). Changes in the decisional conflict score for the control compared to the videobooklet decision aid + ACA group were not significantly different. In our study, an audiovisual patient decision aid decreased decisional conflict more than printed material alone, or than the addition of a more complex computer-based ACA tool requiring more intense cognitive involvement and explicit value choices.
Current treatments for knee osteoarthritis (OA) alleviate symptoms, but do not affect disease progression. For patients with pain and disability unresponsive to medical treatment, total knee arthroplasty (TKA) results in substantial pain relief and functional improvement.1 In 2006, the rate of TKA in the US was more than double that of the previous decade,2 and is expected to continue to rise with advanced aging of the population.3
Despite its benefits, TKA is not without risks. Perioperative complications can occur, and furthermore, prosthesis failure may require surgical revision. Because TKA is an elective procedure and patients must carefully weigh potential benefits and risks, the decision-making process is complex and uncertainty is common. Decisions are strongly related to patients' pre-existing preferences and values and the patient-physician relationship.4,5 Furthermore, some groups such as African Americans and older patients are less likely to choose surgery over conservative therapy.6-10 Qualitative research has demonstrated that patients' misperceptions of surgery in general, misunderstanding of the etiology of OA and its progressive nature, low expectations of TKA outcomes and fear of surgical complications all influence patients' preferences for this procedure. 5,11-13
Clear communication between the patient and physician leading to mutual understanding of the risks and benefits of treatment options for OA increase patient confidence and may lead to higher satisfaction with decision.13 However, the clinical encounter is usually short, and often there is not sufficient time to discuss in-depth the complex issues that patients must understand to clarify their values and make a decision. Patient decision aids can reduce the level of uncertainty or ‘decisional conflict’.14 These tools increase patients' knowledge about the risks and benefits of therapeutic alternatives, help them clarify their values and preferences, and prepare them for the encounter with their physician and deciding on a course of action.14,15
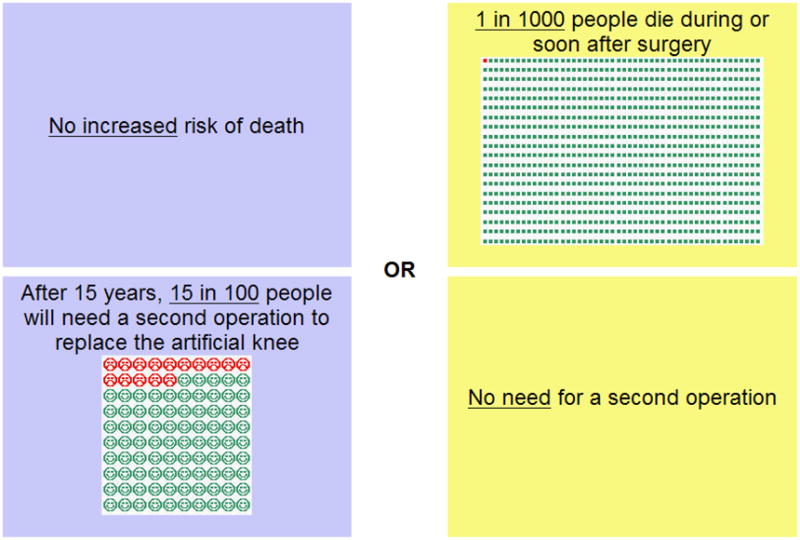
Conjoint analysis has been used for over a decade to explore patient preferences in healthcare.16 This approach enables patients to evaluate tradeoffs between two or more scenarios which present different levels of attributes (risks and benefits) related to the health or therapeutic problem presented to them. Adaptive conjoint analysis (ACA) is a specific type of conjoint analysis that has been explored extensively by Fraenkel et al. to describe patient preferences and values impacting decision-making in rheumatic conditions.17-19 ACA collects and analyzes preference data using an interactive computer program (Sawtooth Software ®). ACA is unique in that it uses an individual respondent's answers to update and refine questions through a series of paired-comparisons (see Figure 1). In addition, because it forces respondents to cognitively engage in the choice between alternatives with competing risks and benefits, it is considered a values clarification exercise of the various attributes pertinent to the decision. The assumption is that the interactive exercise provides the patient with a “deeper insight into his or her own constellation of decision-relevant values.”20
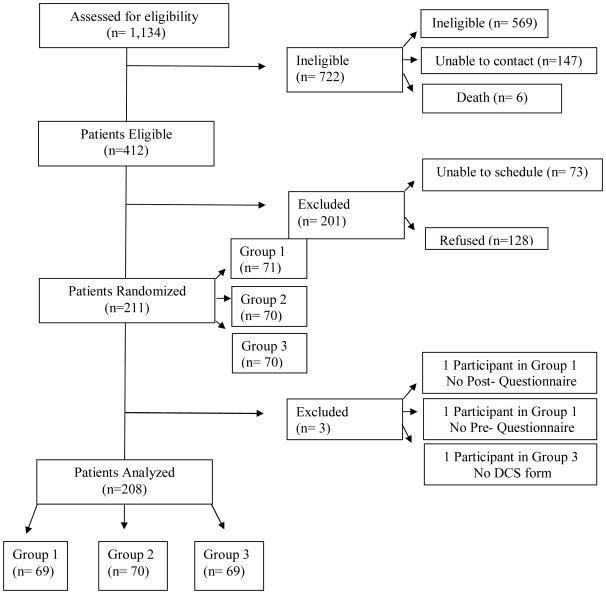
Figure 1. CONSORT diagram of participants.
We conducted a prospective, three arm randomized controlled trial (RCT) to compare ACA coupled with a videobooklet patient decision aid to the videbooklet alone and to standard educational materials regarding patients' decisional conflict associated with TKA for knee OA.
Methods
Participant recruitment
Participants were recruited using multiple methods including advertisements in several local newspapers, on Facebook®, and by contacting participants of a previous research study. Participants were considered eligible if: (i) a physician had told them they had OA of the knee diagnosed with an X-ray at least two years before screening; (ii) their knee OA interfered with their activities of daily living; (iii) they experienced pain (at least 4 on a 1-10 scale) on most days in the last 3 months; and (iv) they had ever considered or talked to a doctor about TKA. Patients were excluded if they had rheumatoid arthritis, had not had X-rays of their knees, had undergone TKA or were currently scheduled for TKA, if they were not comfortable reading and communicating in English, or if they were not comfortable answering questions on a computer using a mouse. After providing informed consent patients were scheduled to participate in the trial. The study was approved by the Institutional Review Board of the University of Texas MD Anderson Cancer Center and Baylor College of Medicine.
ACA Program
Eight attributes were selected via consensus by two rheumatologists (MSA and LF) to evaluate patient preferences for TKA surgery. Characteristics of attributes associated with TKA were then reviewed in the literature to determine four levels for each characteristic chosen (Table 1). Characteristics of knee pain and function were derived from items from the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), specifically ‘having little or no pain when you walk,’ ‘having little or no pain at night,’ and ‘being able to do activities like shopping or golfing with little or no difficulty.’ Due to recent research regarding the presentation of risk perception,21-23 we utilized frequency format to describe risk and added verbal descriptions generating a combined frame presented in the introduction and continued throughout the program. In addition, we utilized visual pictographs to enable understanding of risk and generate affective response.
Table 1. Attributes and levels utilized for ACA program.
| Level | ||||
|---|---|---|---|---|
|
| ||||
| Attribute | 1 | 2 | 3 | 4 |
|
| ||||
| Risk of a serious complication (lung clot, pneumonia, or heart attack) | No increased risk | 1 in 100 | 5 in 100 | 10 in 100 |
| Extremely rare risk of death from surgery | No increased risk | 1 in 1000 | 5 in 1000 | 10 in 1000 |
| Need for another operation after 15 years | No need | 2 in 100 | 8 in 100 | 15 in 100 |
| Number of days in the hospital | No days in the hospital | 3 days | 5 days | 15 days |
| Need for rehabilitation and walking aids | No need | 4 weeks | 6 weeks | 12 weeks |
| Having little or no pain when you walk | Same amount of pain | 5 out of 10 | 7 out of 10 | 9 out of 10 |
| Having little or no pain at night | Same amount of pain | 5 out of 10 | 7 out of 10 | 9 out of 10 |
| Being able to do activities like shopping or golfing with little or no difficulty 6 months from now | Same amount of difficulty | 5 out of 10 | 7 out of 10 | 9 out of 10 |
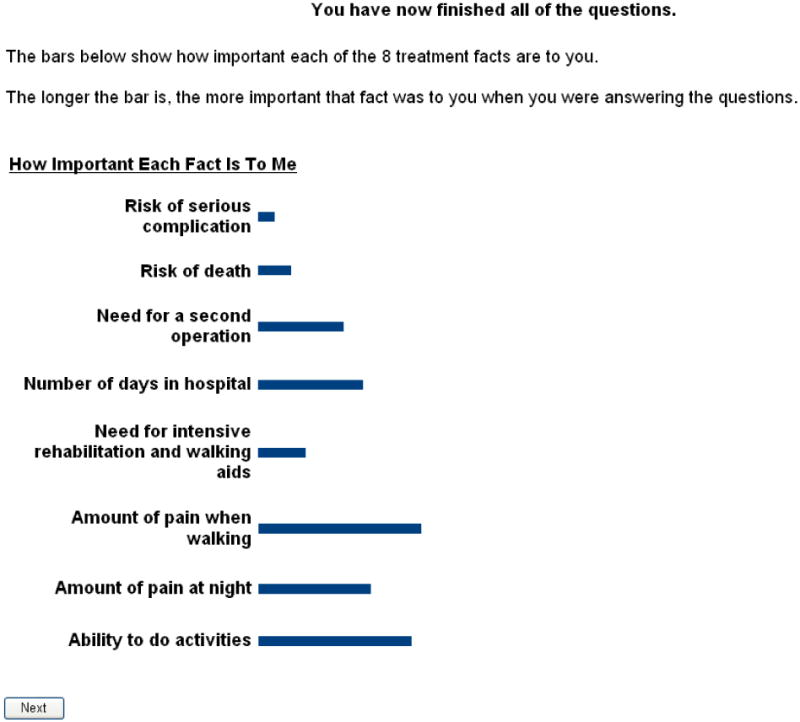
Patients were first presented with a list of the eight characteristics and were told to choose only one as being the most important thing to them ‘when thinking about knee replacement surgery.’ They then were led to a screen where they ranked each of the seven other attributes on a scale from 1-10 (‘not nearly as important’ to ‘just as important’) compared to the first chosen attribute.18 These rankings are used by the software to generate an initial estimate of each subject's values. Next participants were presented with two treatment choices (described to be ‘exactly the same except for the differences [provided]’) and asked to select their preference (weighted scale ranging from ‘strongly prefer left’ to ‘strongly prefer right’) (See Figure 1). Each treatment option provided was described with the same two attributes at two different levels. Lastly, participants were presented with results of the program's calculation of how important each fact was to them. These were presented with bar graphs, the longer bars representing increased importance (See example Figure 2). These results were explained by the research assistant, printed and given to the participants.
Figure 2. Screenshot of ACA program.
We also examined the participants' preferred treatment before and after the intervention. We generated a dichotomized variable indicating certainty in treatment choice (i.e. chose preferred treatment as ‘knee replacement surgery’ or ‘pills and physical therapy’ versus ‘unsure’).
Procedures
Study participants were randomized into one of the three intervention arms using a computer-generated random list with unequal blocks, and numbered, sealed, opaque envelopes to ensure allocation concealment. Patients were randomized after completing the baseline assessment, and only then was the assigned envelope opened to allocate patient to group.
Subjects randomized to Group 1 (“Control”) were given a printed booklet about treatment choices for knee OA, including medical management and surgery published by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).24 Participants were asked to read the booklet which took approximately 20 minutes.
Subjects randomized to Group 2 (“Videobooklet”) were given a videobooklet decision aid developed by Health Dialog with the Foundation for Informed Medical Decision-Making (FIMDM) entitled “Treatment Choices for Knee Osteoarthritis” including a DVD and a booklet to follow along while viewing the DVD. The Shared Decision-making® video was approximately 45 minutes long and meets criteria created by the International Patient Decision Aids Standards (IPDAS) Collaboration in the areas of content, development process and effectiveness.25
Subjects randomized to Group 3 (“Videobooklet + ACA”) were given the same videobooklet decision aid to watch and read first. Afterwards they received a brief training session regarding the computer-based ACA tool and then completed the ACA tool, which took an additional 15 minutes.
On the day of the scheduled intervention, after randomization, participants assigned to the control group were taken to a room where they were provided with the educational book and upon completion of the reading they completed the post-intervention questionnaires. Participants in the videobooklet and videobooklet+ACA groups remained together and viewed the video. Once the video was finished, the groups were again divided and the videobooklet group was taken to a separate room where they completed their post-intervention questionnaires. The videobooklet+ACA group was given instruction on the ACA program by the study coordinator. A demo ACA program using the same instructions and introduction screens as the program used by the individual patients was presented to the participants while the coordinator explained the exercise. Participants were allowed to ask questions about the program during the demo. Upon completion of the demo, participants were led to individual computers, where they completed the ACA program on their own. The study coordinator was available to answer questions about use. After participants completed the program, they were given post-intervention questionnaires to complete.
Measures
Primary Outcome Measure
The decisional conflict scale developed by O'Connor was adapted for knee OA to evaluate participants' uncertainty with their treatment options.15 Patients were first asked ‘which treatment option they preferred: knee replacement surgery; pills and physical therapy, possibly occasional knee joint injections; or unsure.' The total score ranges from 0 (no decisional conflict) to 100 (extremely high decisional conflict). The decisional conflict scale has five 0-100 subscales: (i) uncertainty, (ii) informed, (iii) values clarity, (iv) support; and (v) effective decision. For all subscales higher scores indicate greater decisional conflict. The decisional conflict scale was administered before the intervention and immediately after. O'Connor has generated thresholds of meaningful differences. A score of less than 25 of 100 is ‘associated with implementing decisions’ and a score greater than 37.5 of 100 is ‘associated with decision delay or feeling unsure about implementation.’ The total score was used as the primary outcome measure, and the subscale scores were used as secondary outcome measures.26
Covariates
Demographic information collected included self-reported age, race/ethnicity, gender, education, marital status and employment status. Comorbidities were assessed using participants' self-reported checklist of conditions generated from the conditions present in the Charlson comorbidity index.27 Body mass index (BMI) was calculated from self-reported height and weight. The Knee injury and Osteoarthritis Outcome Score (KOOS) was utilized to measure knee pain and symptoms and the effects of the arthritis on participants' activities of daily living, sports and recreational activities and quality of life.28 Patients also indicated in which knee they had OA (right, left or both) and the year in which they were first diagnosed with OA.
Statistical analysis
All analyses were conducted according to group allocation. A sample size of 70 per group was calculated to be sufficient to estimate a moderate effect size (0.5) responsive to change in DCS before and after interventions26 with a two-tailed probability of type I error of 0.05, and a type two error of 0.20 (80% power). Chi-square and analysis of variance (ANOVA) were utilized to identify differences in patient characteristics for categorical and continuous variables respectively. We defined change in decisional conflict total score and subscale scores as the difference between the post-intervention and pre-intervention scores (so that a negative difference indicated a reduction in decisional conflict). Tukey's honestly significant difference post hoc test was utilized to examine differences between randomized groups. Statistically significant differences were defined at the p<0.05 level. We also conducted analysis of covariance (ANCOVA) to control for potential baseline differences among groups. Decisional conflict scale post-intervention scores were the dependent variable in the ANCOVA model with group as the independent variable and baseline scores as a covariate. All analyses were conducted in STATA version 10 (StataCorp, College Station, TX).
Results
Patient disposition
A total of 1,134 potential participants were contacted study staff; 64% were deemed ineligible after screening or were unable to be contacted after multiple attempts before the end of the recruitment period. Of the remaining eligible participants, 31% declined participation, and 18% were unable to attend the intervention session before the end of the recruitment period. A total of 210 participants were randomized into one of the three treatment groups. Two participants (one from the control group and one from the videobooklet+ACA group) did not turn in the post-intervention questionnaire and were excluded in this analysis, leaving a total of 208 participants in the analysis (Figure 3).
Figure 3. Example of ACA output.
Patient characteristics
Patient characteristics are described in Table 2. After randomization, no statistically significant differences existed among groups in participant demographic characteristics, KOOS pain, function or quality of life scores. Statistically significant differences (p=0.02), however were noted between the videobooklet group and the videobooklet+ACA in KOOS symptom scores, but not on the other KOOS subscales. The difference was small (5 points) with those in the videobooklet group reporting less knee symptoms.
Table 2. Participant Characteristics.
| Total (n=208) | Group 1 - Control (n=69) | Group 2 - Videobooklet (n=70) | Group 3 - Videobooklet + ACA (n=69) | |
|---|---|---|---|---|
|
| ||||
| Gender: Female | 141 (68%) | 48 (70) | 47 (67) | 46 (67) |
|
| ||||
| Age, years, mean (SD) | 62.8 (9.0) | 63.6 (8.6) | 62.6 (9.2) | 62.5 (9.4) |
|
| ||||
| White | 137 (66) | 49 (71) | 49 (70) | 39 (56) |
| Black | 49 (24) | 14 (20) | 17 (24) | 18 (26) |
| Hispanic | 15 (7) | 3 (4) | 2 (3) | 10 (14) |
| Other | 7 (3) | 3 (4) | 2 (3) | 2 (3) |
|
| ||||
| Less than bachelor's degree | 91 (44) | 30 (43) | 28 (40) | 33 (48) |
| Bachelor's or Advanced Degree | 117 (56) | 39 (56) | 42 (60) | 36 (52) |
|
| ||||
| Disabled | 13 (6) | 3 (4) | 6 (8) | 4 (6) |
| Employed | 76 (36) | 25 (36) | 24 (34) | 27 (39) |
| Retired | 85 (41) | 29 (42) | 28 (40) | 28 (40) |
| Something else | 34 (16) | 12 (17) | 12 (17) | 10 (14) |
|
| ||||
| Bilateral Knee Symptoms | 116 (56) | 42 (61) | 38 (54) | 36 (52) |
|
| ||||
| Disease Duration , years (SD) | 9.6 (8.2) | 10.6 (9.8) | 9.0 (6.6) | 9.2 (7.9) |
|
| ||||
| BMI | 32.9 (8.1) | 32.0 (7.9) | 34.3 (8.7) | 32.3 (7.7) |
|
| ||||
| Comorbidity Index | 0.9 (1.6) | 0.8 (1.6) | 1.1 (1.8) | 0.7 (1.3) |
|
| ||||
| KOOS Pain | 48.8 (17.5) | 50.0 (18.4) | 50.7 (15.2) | 45.7 (18.6) |
| KOOS Symptom * | 42.4 (11.2) | 41.6 (10.8) | 45.3 (11.5) | 40.3 (10.7) |
| KOOS Function in Daily Living | 51.9 (19.0) | 52.5 (17.7) | 54.4 (18.3) | 48.8 (20.6) |
| KOOS Function in Sports/Recreation | 25.5 (24.9) | 26.4 (25.5) | 26.4 (25.3) | 23.8 (24.1) |
| KOOS Quality of Life | 27.5 (17.7) | 29.2 (17.5) | 28.2 (16.6) | 25.0 (18.9) |
denotes p < 0.05, anova; Group 2 significantly higher than group 3 using Tukey's honestly significant difference. No other statistically significant differences by group.
Pre-post results after intervention
Prior to the intervention, a statistically significant difference was noted between the control and videobooklet groups in the effective decision subscale (Table 3). No statistically significant differences between groups were noted for the total score or the other subscales at baseline. Immediately after the intervention the decisional conflict scale total score and subscale scores were significantly lower in all three groups indicating a reduction in decisional conflict. Post hoc analyses of differences between groups indicated that both the videobooklet and videobooklet+ACA interventions had greater reductions in decisional conflict than the booklet alone (−21.0, −14.0, and −9.5 respectively, p<0.001). In addition, the reduction in decisional conflict was greater for the videobooklet group than the videobooklet+ACA group.
Table 3. Multiple Comparison Group Differences of Decisional Conflict Scale Total and Subscale Scores.
| Variable | Group 1 - Control (n=69) Mean (SE) | Group 2 - Videobooklet (n=70) Mean (SE) | Group 3 - Videobooklet + ACA (n=69)Mean (SE) | p-value | Statistically significant comparisons* |
|---|---|---|---|---|---|
|
| |||||
| DCS Total Score Pre | 38.8 (2.2) | 42.7 (2.3) | 37.4 (2.0) | > 0.20 | None |
| DCS Total Score Post | 29.2 (2.0) | 21.6 (1.5) | 23.4 (1.8) | 0.009* | 1 vs 2 and 1 vs 3 |
| DCS Total Score Difference (Post-Pre)† | −9.5 (1.8) | −21.0 (2.2) | −14.0 (1.9) | <0.001* | 1 vs 2 and 2 vs 3 |
|
| |||||
| DCS Uncertainty Pre | 46.4 (3.1) | 52.5 (3.0) | 48.1 (2.9) | > 0.20 | None |
| DCS Uncertainty Post | 35.9 (2.7) | 29.8 (2.2) | 33.4 (2.8) | > 0.20 | None |
| DCS Uncertainty Difference (Post-Pre)† | −10.5 (2.4) | −22.7 (3.2) | −14.6 (3.0) | 0.01* | 1 vs 2 |
|
| |||||
| DCS Informed Pre | 41.4 (2.9) | 42.6 (2.8) | 37.1 (2.6) | > 0.20 | None |
| DCS Informed Post | 27.3 (2.0) | 15.4 (1.7) | 15.9 (1.9) | < 0.001* | 1 vs 2 and 1 vs 3 |
| DCS Informed Difference (Post-Pre)† | −14.1 (2.6) | −27.3 (2.7) | −21.1 (2.5) | 0.002* | 1 vs 2 |
|
| |||||
| DCS Values Clarity Pre | 38.5 (2.9) | 37.4 (2.5) | 32.2 (2.6) | >0.20 | None |
| DCS Values Clarity Post | 26.1 (2.3) | 16.9 (1.8) | 17.9 (1.8) | 0.002* | 1 vs 2 and 1 vs 3 |
| DCS Values Clarity Difference (Post-Pre)† | −12.4 (2.6) | −20.5 (2.7) | −14.4 (2.4) | 0.07 | 1 vs 2 |
|
| |||||
| DCS Support Pre | 32.5 (2.1) | 36.0 (2.4) | 32.8 (2.0) | > 0.20 | None |
| DCS Support Post | 25.0 (1.9) | 19.9 (1.7) | 20.5 (1.8) | 0.10 | None |
| DCS Support Difference (Post-Pre)† | −7.5 (2.1) | −16.1 (2.3) | −12.3 (1.9) | 0.02* | 1 vs 2 |
|
| |||||
| DCS Effective Decision Pre | 36.0 (2.4) | 44.4 (2.5) | 37.0 (2.1) | 0.02* | 1 vs 2 |
| DCS Effective Decision Post | 31.2 (2.3) | 25.1 (1.9) | 27.7 (2.2) | 0.12 | None |
| DCS Effective Decision Difference (Post-Pre)† | −4.7 (1.8) | −19.3 (2.6) | −9.3 (2.5) | < 0.001* | 1 vs 2 and 2 vs 3 |
DCS - Decisional Conflict Scale. Higher score denotes higher conflict. Range 0-100
Overall and within groups, post-intervention scores statistically significantly differed than pre-intervention scores p<0.05, anova
Tukey's honestly significant difference test, p < 0.05, anova
The overall baseline decisional conflict total score was approximately 40, indicating high decisional conflict and uncertainty. Results on the decisional conflict subscales demonstrated similar patterns, with both videobooklet groups showing significant reductions in decisional conflict compared to controls. The largest reduction was observed in the videobooklet alone group. Overall, the two decisional conflict subscales that improved the most were ‘informed’ and ‘uncertainty’. The mean difference in pre and post-intervention total and subscale decisional conflict scores varied from −4.5 to −27.3 out of 100. After the intervention, the overall decisional conflict total group mean score was slightly less than 25, suggesting patients were ready to implement a decision about treatment.
In the ANCOVA model, pre-intervention decisional conflict scores and randomized group were significantly associated with post-intervention decisional conflict total score. Due to statistically significant differences between groups in the KOOS symptom scores at baseline, an additional ANCOVA model was generated taking into account patients' self-reported symptoms measured by the KOOS. When added to the model, KOOS symptoms did not significantly contribute to a change in the decisional conflict total or subscale scores.
Among the 218 patients who indicated a specific preferred treatment before the intervention (either ‘knee replacement surgery’ or ‘pills and physical therapy, possibly occasional knee joint injections’), 87.5% continued to indicate a preferred choice after the intervention, while 12.5% became ‘unsure’ about their preferred treatment. Among the 80 patients who were initially were ‘unsure’ about their preferred treatment, 61.2% chose a treatment option while 38.8% remained ‘unsure’. We also examined if change in patient preferences about OA treatment could have an impact on decisional conflict after receipt of the decision aids. In order to further evaluate this possibility, we incorporated a dichotomized variable indicating change in preference in the pre vs. post-intervention decisional conflict scale total score into an ANCOVA model. The analysis demonstrated the change in preference itself was not statistically associated with decisional conflict scores.
Discussion
Patients with advanced knee OA are often faced with the decision about TKA. This decision can be difficult, particularly if patients do not clearly understand the benefits and risks of each option (undergoing surgery or continuing medical management alone). It is important to ensure patients are effectively informed and decisions are not guided by misperceptions and false beliefs. The decision process itself involves multiple health care providers and discussions regarding pros and cons of surgery and patient preferences.29
In this study, we examined the effect of a decision aid supplemented by an adaptive conjoint analysis program on decisional conflict regarding treatment options in individuals with knee OA. We used three different tools: (i) an educational booklet developed by the NIH, (ii) a videobooklet decision aid developed by the Foundation for Informed Decision Making and (iii) a computer-based adaptive conjoint analysis values clarification exercise with the videobooklet decision aid. Decisional conflict decreased among all patient groups receiving information about treatment options for OA. This finding was expected and supports theory in which information provided to patients about risks and benefits of treatment options decreases decisional conflict. Previous studies measuring change in the decisional conflict after decision aids range from −2.5 to −17.1.14
The magnitude of reduced decisional conflict in our cohort varied between groups. Those who received the control brochure had the smallest reduction in decisional conflict, while those who viewed the videobooklet had the greatest reduction in decisional conflict. Furthermore, those in the control group continued to have scores greater than 25, indicating the potential for high decisional conflict and uncertainty while those in the videobooklet and videobooklet+ACA group had scores below 25 indicating readiness to implement a decision. Both groups receiving the videobooklet intervention had increased improvement with respect to individuals receiving the booklet alone. The videobooklet decision aid not only described OA and the potential treatments like the control group, but also included outcomes of the options, communicated risks, benefits and uncertainties using audiovisual and graphical methods and suggested the patients take their own values into account when deciding about TKA. In addition, the videobooklet integrated testimonials of patients that had chosen surgical and non-surgical treatment options and emphasized communication with the patient's physician which may have added to its overall effectiveness when compared to the booklet.30-32 The various components of the decision aid provide a possible explanation to the greater magnitude in reduced decisional conflict found in our study compared to previous studies. Weng et al. utilized the same videobooklet produced by FIMDM to determine the effect of the decision aid on knowledge, expectations and decisional conflict. They found the video to be effective in creating realistic expectations. In addition, viewers of the video felt more confident in their knowledge of the efficacy of TKA treatment. In their cohort, the post-intervention decisional conflict score was 25.8 which is similar to our cohorts' final score of 25.33
Previous randomized control trials have compared patient decision aids to usual care and simple to complex decision aids. Few, to our knowledge, have been utilized in the area of decision-making for OA treatment, utilizing TKA as a treatment option. As summarized by O'Connor and colleagues in the 2009 Cochrane Review, 10 studies compared decision aids to usual care for a variety of decisions and evaluated decisional conflict.14 Decisional conflict decreased in all of the included studies when comparing the decision aid versus usual care. In the meta-analysis, O'Connor and colleagues also included a comparison of the impact of simple versus complex decision aids on decisional conflict. Their results indicated only one of seven studies demonstrated significant reductions in decisional conflict with detailed versus simple decision aids. This is comparable to our results in that we did not see a further decrease in decisional conflict among the videobooklet+ACA group when compared to the group that received the videobooklet only.14,34
Potential respondent fatigue could be one explanation to our findings: participants in the videobooklet group took approximately one hour to view the video and complete the questionnaires, while those in the videobooklet+ACA took on average two hours. To further investigate the potential effect of respondent fatigue on decisional conflict we evaluated scale reliability of the total decisional conflict post scores among the three groups, using Cronbach's alpha and mean to variance ratios, to determine if for those engaged in the videobooklet+ACA intervention variability increase (and reliability decreased) in their responses. The internal consistency was excellent and consistent between groups (0.96, 0.94 and 0.94 for control, videobooklet and videobooklet+ACA groups, respectively). Mean to variance ratios were 9.71, 7.76 and 9.60 for control, videobooklet and videobooklet+ACA groups, respectively. No statistically significant differences were observed in the mean to variance ratio between groups. This suggests that respondent fatigue did not have an impact on the reliability of the outcome measure.
Another potential explanation for the greater reduction in decisional conflict among the videobooklet only group is that the ACA exercise in addition to the information provided by the videobooklet was cognitively rigorous, and in fact reduced clarity about the decision, increasing uncertainty. It has been suggested that complex decisions do not always benefit from intense cognitive evaluation, and that in these circumstances ‘gist’ driven decisions may be more satisfying.35 We only assessed ACA in addition to the videobooklet decision aid. Previous studies in which patient preferences were elicited utilizing conjoint analysis alone demonstrate patients are able to evaluate multiple risks, benefits and uncertainties regarding specific treatment options.19 Fraenkel et al. utilized ACA to elicit preferences regarding treatment options for OA including non-steroidal anti-inflammatory drugs, cyclooxygenase-2 inhibitors, glucosamine and/or chondroitin, opioids or capsaicin. They found patients preferred topical capsaicin most likely due to due to low probability of adverse effects. Patients in this study however did not receive additional information about the decision from another decision aid. Fraenkel also did not include TKA as a potential treatment option. In addition, decisional conflict was not evaluated.
Although the content of the decision aids utilized in this study were comprehensive, additional specific content areas were not included. The aids utilized in this study did not include content regarding costs of the treatments. This may be an area of concern for many with OA considering the cost of TKA can be over U$S 100,000 for a person at end-stage OA and multiple comorbidities.36 It is important to note, also, the control group used in this study did not receive ‘standard of care.’ Rather, the control group received publically available educational materials about OA and treatment options, offering a reasonable comparison with the two decision aid groups.
Our participants were over the age of 55 years old, mostly female, and with high prevalence of obesity, characteristics that are representative of patients with knee OA at large.37 However, they were mostly White and educated and may not be representative of OA patients from ethnically diverse backgrounds, or low literacy levels, considering treatment options. Our recruitment methods may have generated volunteer bias. Less than 20% of the participants were recruited from the previous study and over 65% of our participants were recruited from newspaper ads. Recruitment from the waiting room of a physician visit may have generated a different population; however we feel our recruitment methods generated a more representative group of all patients with knee OA, not only those who were receiving current care for their OA.
Participants described experiences of friends or family members who had already undergone TKA. The experiences of others may influenced the decision-making process and affect toward surgical options, however we did not formally evaluate these influences. Future evaluations of treatment decision-making should incorporate experiences and heuristics.
The ACA program may have in fact increased decisional conflict after the delivery of the videobooklet. This however may not be a negative effect of the ACA program. It is important to consider the variation within our participant group in stage of decision regarding TKA. Although decisional conflict is generally assessed as a negative attribute of a decision, it is useful to think that decisional conflict may be expected for many in this population and they work through the decision. Those that viewed the videobooklet and participated in the ACA program were able to view the risks and the benefits of TKA specifically and may have delayed their decision or become uncertain regarding their preferences. This does not necessarily indicate they will not make a quality decision, or be satisfied with the decision; instead it suggests additional thought into the decision.
Our findings suggest that a comprehensive videobooklet including a decision aid significantly improved decisional conflict in patients with knee OA when considering multiple treatment options. Participating in the ACA exercise, however, did not contribute to additional reductions in decisional conflict. In addition, certainty about treatment decisions can vary after exposure to information, suggesting that early patient education about treatment options for OA during the discussion with the primary care physician or rheumatologist is needed. Long-term effectiveness of these tools on the quality of the decision, overall satisfaction with the decision, and final impact on preferences about TKA is yet to be determined.
Significance and Innovation.
Patient decision aids provide information to patients regarding risks and benefits of multiple treatment options and have been shown to reducing decisional conflict.
Reduction in decisional conflict or uncertainty is linked to improved satisfaction with the decision.
Comprehensive decision aids appear to reduced decisional conflict in OA patients considering TKA and could be used at point of care to facilitate informed patient decision-making.
Acknowledgments
Supported by the Agency for Healthcare Research and Quality (AHRQ) through the Center for Education and Research on Therapeutics (CERTs; U18 HS016093). Dr. Suarez-Almazor has a K24 career award from the National Institute for Arthritis, Musculoskeletal and Skin Disorders (NIAMS; AR53593-06) and is the Director of the Houston Center for Education and Research on Therapeutics funded by AHRQ. Dr Fraenkel was supported by a NIAMS K23 award (AR048826-05) for this work.
We are grateful to Mr. Vincent Richards who assisted us in the recruitment and follow-up of participants.
References
- 1.Jones CA, Beaupre LA, Johnston DWC, Suarez-Almazor ME. Total Joint Arthroplasties: Current Concepts of Patient Outcomes after Surgery. Rheumatic Disease Clinics of North America. 2007;33(1):71–86. doi: 10.1016/j.rdc.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Freid VM, Bernstein AB. Health care utilization among adults aged 55-64 years: how has it changed over the past 10 years? NCHS Data Brief. 2010:1–8. [PubMed] [Google Scholar]
- 3.Singh JA, Vessely MB, Harmsen WS, et al. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969-2008. Mayo Clin Proc. 2010;85:898–904. doi: 10.4065/mcp.2010.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz JN, Lyons N, Wolff LS, et al. Medical decision-making among Hispanics and non-Hispanic Whites with chronic back and knee pain: A qualitative study. BMC Musculoskelet Disord. 2011;12:78. doi: 10.1186/1471-2474-12-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Neill T, Jinks C, Ong BN. Decision-making regarding total knee replacement surgery: a qualitative meta-synthesis. BMC Health Services Research. 2007;7:52. doi: 10.1186/1472-6963-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kroll TL, Richardson M, Sharf BF, et al. “Keep on truckin” or “It's got you in this little vacuum”: race-based perceptions in decision-making for total knee arthroplasty. Journal of Rheumatology. 2007;34:1069–75. [PubMed] [Google Scholar]
- 7.Suarez-Almazor ME, Souchek J, Kelly PA, et al. Ethnic variation in knee replacement: patient preferences or uninformed disparity? Archives of Internal Medicine. 2005;165:1117–24. doi: 10.1001/archinte.165.10.1117. [DOI] [PubMed] [Google Scholar]
- 8.Byrne MM, Souchek J, Richardson M, et al. Racial/ethnic differences in preferences for total knee replacement surgery. Journal of Clinical Epidemiology. 2006;59:1078–86. doi: 10.1016/j.jclinepi.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Figaro MK, Russo PW, Allegrante JP, Figaro MK, Russo PW, Allegrante JP. Preferences for arthritis care among urban African Americans: “I don't want to be cut”. Health Psychology. 2004;23:324–9. doi: 10.1037/0278-6133.23.3.324. [DOI] [PubMed] [Google Scholar]
- 10.Hamel MB, Toth M, Legedza A, et al. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Archives of Internal Medicine. 2008;168:1430–40. doi: 10.1001/archinte.168.13.1430. [DOI] [PubMed] [Google Scholar]
- 11.Wright JG, Santaguida PL, Young N, et al. Patient preferences before and after total knee arthroplasty. Journal of Clinical Epidemiology. 2010;63:774–82. doi: 10.1016/j.jclinepi.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 12.Suarez-Almazor ME, Richardson M, Kroll TL, et al. A qualitative analysis of decision-making for total knee replacement in patients with osteoarthritis. JCR: Journal of Clinical Rheumatology. 2010;16:158–63. doi: 10.1097/RHU.0b013e3181df4de4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Street RL, Jr, Richardson MN, Cox V, et al. (Mis)understanding in patient-health care provider communication about total knee replacement. Arthritis & Rheumatism. 2009;61:100–7. doi: 10.1002/art.24371. [DOI] [PubMed] [Google Scholar]
- 14.O'Connor AM, Bennett CL, Stacey D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009:CD001431. doi: 10.1002/14651858.CD001431.pub2. [DOI] [PubMed] [Google Scholar]
- 15.O'Connor AM. Validation of a decisional conflict scale. Medical Decision Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 16.Marshall D, Bridges JF, Hauber B, et al. Conjoint Analysis Applications in Health - How are Studies being Designed and Reported? An update on Current Practice in the Published Literature between 2005 and 2008. Patient. 2010;3:249–56. doi: 10.2165/11539650-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 17.Fraenkel L. Conjoint Analysis at the Individual Patient Level: Issues to Consider as We Move from a Research to a Clinical Tool. Patient. 2008;1:251–3. doi: 10.2165/1312067-200801040-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fraenkel L. Feasibility of Using Modified Adaptive Conjoint Analysis Importance Questions. Patient. 2010;3:209–15. doi: 10.2165/11318820-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fraenkel L, Bogardus ST, Concato J, Felson DT, Wittink DR. Patient preferences for treatment of rheumatoid arthritis. Ann Rheum Dis. 2004;63:1372–8. doi: 10.1136/ard.2003.019422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Llewellyn-Thomas HA. Values Clarification. In: Edwards A, Elwyn G, editors. Shared decision-making in healthcare: Achieving evidence-based patient choice. Second. Oxford University Press; 2009. [Google Scholar]
- 21.Fraenkel L, Rabidou N, Wittink D, Fried T. Improving informed decision-making for patients with knee pain. J Rheumatol. 2007;34:1894–8. [PubMed] [Google Scholar]
- 22.Kopec JA, Richardson CG, Llewellyn-Thomas H, et al. Probabilistic threshold technique showed that patients' preferences for specific trade-offs between pain relief and each side effect of treatment in osteoarthritis varied. Journal of Clinical Epidemiology. 2007;60:929–38. doi: 10.1016/j.jclinepi.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Peters E, Hart PS, Fraenkel L. Informing Patients: The Influence of Numeracy, Framing, and Format of Side Effect Information on Risk Perceptions. Medical Decision Making. 2010 doi: 10.1177/0272989X10391672. [DOI] [PubMed] [Google Scholar]
- 24.NIH. Handout on Health: Osteoarthritis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. 2006 [Google Scholar]
- 25.Treatment choices for Knee Osteoarthritis: Decision Aid Summary. 2010 Accessed at http://decisionaid.ohri.ca/AZsumm.php?ID?1087.
- 26.Ottawa: Ottawa Hospital Research Institute; 1993. User Manual - Decisional Conflict Scale (16 item statement format) [document on the Internet] [updated 2010] (Accessed at http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Decisional_Conflict.pdf. [Google Scholar]
- 27.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 28.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17. doi: 10.1186/1477-7525-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zikmund-Fisher BJ, Couper MP, Singer E, et al. Deficits and variations in patients' experience with making 9 common medical decisions: the DECISIONS survey. Med Decis Making. 2010;30:85S–95S. doi: 10.1177/0272989X10380466. [DOI] [PubMed] [Google Scholar]
- 30.Elwyn G, O'Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333:417. doi: 10.1136/bmj.38926.629329.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elwyn G, O'Connor AM, Bennett C, et al. Assessing the quality of decision support technologies using the International Patient Decision Aid Standards instrument (IPDASi) PLoS One. 2009;4:e4705. doi: 10.1371/journal.pone.0004705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spunt BS, Deyo RA, Taylor VM, Leek KM, Goldberg HI, Mulley AG. An interactive videodisc program for low back pain patients. Health Educ Res. 1996;11:535–41. doi: 10.1093/her/11.4.535. [DOI] [PubMed] [Google Scholar]
- 33.Weng HH, Kaplan RM, Boscardin WJ, et al. Development of a decision aid to address racial disparities in utilization of knee replacement surgery. Arthritis & Rheumatism. 2007;57:568–75. doi: 10.1002/art.22670. [DOI] [PubMed] [Google Scholar]
- 34.Ringash J. Review: decision aids increase patients' knowledge and realistic expectations and reduce decisional conflict. Evidence-Based Medicine. 2004;9:21. [Google Scholar]
- 35.Lloyd FJ, Reyna VF. Clinical gist and medical education: connecting the dots. JAMA. 2009;302:1332–3. doi: 10.1001/jama.2009.1383. [DOI] [PubMed] [Google Scholar]
- 36.Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–21. doi: 10.1001/archinternmed.2009.136. discussion 21-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arden N, Nevitt MC. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. 2006;20:3–25. doi: 10.1016/j.berh.2005.09.007. [DOI] [PubMed] [Google Scholar]