Abstract
Objective
The emergency department (ED) is an inherently high-risk setting. Early death after an ED evaluation is a rare and devastating outcome which the understanding of can potentially help improve patient care and outcomes. Using administrative data from an integrated health system, we describe characteristics and predictors of patients who experience 7-day death after ED discharge.
Methods
Administrative data from 12 hospitals were used to identify death after discharge in adults age 18 or older within 7 days of ED presentation from 1/1/07 to 12/31/08. Patients who were non members of the health system, in hospice care, or seen at out of network EDs were excluded. Predictors of 7-day post-discharge death were identified using multivariable logistic regression.
Results
The study cohort contained a total of 475,829 members with 728,312 discharges from Kaiser Permanente Southern California (KPSC) EDs in 2007 and 2008. Death within 7 days of discharge occurred in 357 cases (0.05%). Increasing age, male gender, and number of pre-existing co-morbidities were associated with increased risk of death. The top 3 primary discharge diagnoses predictive of 7-day death after discharge include non-infectious lung disease (OR 7.1, 95% CI 2.9-17.4), renal disease (OR 5.6, 95% CI 2.2-14.2), and ischemic heart disease (OR 3.8, 95%CI 1.0-13.6).
Conclusions
Our study suggests that 50 in 100,000 patients in the U.S. die within 7-days after discharge from an emergency department. Our study is the first to identify potentially “high risk” discharge diagnoses in patients who suffer a short-term death after discharge.
INTRODUCTION
Background
Recent attention to quality improvement and patient safety has highlighted the importance of improving emergency care.1 The emergency department (ED) is an inherently high-risk setting2, and early death after ED discharge is an adverse event which may signal opportunities to improve care. An estimated 30,000 patients experience early death after ED discharge annually in the United States.3-4 Two prior case series of early death after ED discharge in the United States are an important contribution but are limited by small sample size and lack of a control population.4-5 Studies of this phenomenon conducted in Iceland and Canada may not be generalizable to the US population due to differences in healthcare systems and populations.6-7 The major barrier to studying this important public health problem in the United States has been the lack of large datasets that link information about patient co-morbidities, acute ED illness presentation, and ED care to post-ED discharge outcomes.
Importance
Although early death after ED discharge events in the US population may have important medico-legal and patient safety implications, there is little systematic understanding of such events. With increasing ED crowding8-14, illness complexity of the aging population, and pressures to reduce unnecessary hospitalizations, it is likely that underlying factors contributing to potentially avoidable ED post discharge death will intensify.6
Goal of This Investigation
We studied data from an integrated health care system including 12 emergency departments to identify the patterns and predictors of 7-day mortality following ED discharge. To the best of our knowledge, this is the first population-based, controlled study on early death after ED discharge in the United States.
METHODS
Study Design
We conducted a retrospective cohort study of member visits to any of 12 emergency departments within an integrated health system beginning in January 2007 and ending in December 2008. All adult patients seen and discharged from an ED to home or a non-acute care facility were eligible. Patients who died within or en route to the ED were excluded along with patients in hospice care. Death within 7 days of the ED visit was identified using the California Vital Statistics files and the Social Security Death Index. Predictors of short-term mortality following discharge were identified using multivariable logistic regression using a generalized estimating equation. The study protocol was reviewed and approved by the Institutional Review Board of Kaiser Permanente Southern California and the University of California at Los Angeles.
Setting
We examined administrative data of members of Kaiser Permanente Southern California (KPSC), an integrated health system which provides comprehensive care to 3.1 million members throughout Southern California. Health care is delivered at over 100 outpatient clinics and emergency services provided at 12 medical centers. All members have similar health care benefits, including coverage of emergency services both within and outside the health system. Electronic administrative databases track all health care encounters within the health system. A claims reimbursement system tracks health care encounters at outside facilities. Detailed information on diagnoses and procedures are available regardless of setting. Laboratory, pharmacy and other specialized databases provide information on clinical care including the use of hospice services. All members are assigned a unique medical record number which is used for data linkage.
Selection of Participants
Study subjects were members of Kaiser Permanente Southern California with at least 1 emergency department visit and discharge from 1st Jan 2007 to 31st Dec 2008. A subject had to be a member of the health plan at the time of the ED visit; however, no minimum health plan enrollment period was required. Subjects were restricted to age 18 years and older due to the low incidence of post-discharge complications in children. Subjects discharged home, to a skilled nursing facility, or to a rehabilitation facility were included in the analysis.
Subjects admitted to an inpatient ward or inpatient observation bed were excluded. Patients who died en route or within the ED were also excluded. We excluded patients who were in hospice care on the basis that such care indicates knowledge of impending death and an intention to provide end-of-life therapy rather than more aggressive treatment. Visits by non-health plan members to health plan EDs were excluded, as we did not have comorbidity data on such patients. Visits to non-KPSC emergency departments were also excluded due to the inability to identify a primary ED discharge diagnosis among all the diagnosis claims for non-KPSC ED visits. Quality of administrative data was validated by blinded manual chart review of 20 cases which demonstrated 100% agreement between the chart and the electronic records for discharge diagnosis, disposition, and mortality.
Methods of Measurement
Demographic information on age, sex, income, ethnicity and race were obtained from administrative databases. We collected data on the presence of 17 comorbid conditions as defined by the Charlson classification system.15 For this purpose, we obtained ICD diagnosis codes from all inpatient, outpatient, and emergency department health plan encounters during the entire duration of membership and prior to the index ED visit.
To our knowledge, the literature lacks a thorough yet concise coding system of discharge diagnoses from acute care facilities that is representative of the most prevalent and clinically important conditions.16-18 Similar to the methods used for the creation of cause of death categories, our study group, composed of GZG, BCS, and SDS, apriori reviewed data on national3 and local ED visits, and used clinical judgment to classify the AHRQ CCS Multilevel diagnosis codes9 into 38 primary discharge diagnosis categories. The study group first composed the categories and then reviewed the codes individually. Following the individual review of the codes, the group met a second time to discuss residual unclassified diagnoses and a third time to arrive at the final ED discharge diagnosis groups. The 38 codes included a total of 5 symptom based discharge categories such as chest pain, abdominal pain and syncope. (See Appendix)
Outcome Measures
The primary outcome was all cause death occurring within 7-days after the start of the emergency department assessment. We chose the 7-day time frame because of its clinical relevance, implications for health policy decisions, and prior use in previous studies.4-7 Mortality data included the California vital statistics files for in-state deaths and the Social Security Death Index for out-of-state deaths. Occurrence of death was determined within the year of the ED visit regardless of subsequent health plan membership status. Cause of death was obtained from state death certificates (cause of death is not available from the Social Security Death Index) and was classified using a modified version of the Clinical Categorization Software (CCS).9 The CCS is developed by the Agency of Healthcare Research and Quality (AHRQ) to group all ICD codes into clinically meaningful categories. The CCS has aggregated ICD-10 codes for 259 mutually exclusive categories. Our study team used national19 and local mortality data, as well as clinical judgment, to further aggregate single level CCS codes into 21 cause-of death categories. (See Appendix)
Primary Data Analysis
We estimated the incidence of 7-day all cause mortality following discharge after an ED visit. The univariate associations of demographic characteristics, pre-existing comorbidities, and ED discharge diagnoses with death at 7 days were examined by the likelihood ratio test.
Predictors of 7-day death after discharge were identified through multivariable logistic regression using a generalized estimating equation for a binomial outcome. The unit of analysis was an ED visit. To account for clustering of ED visits by unique individuals, the models included person-level random effects. The model accounts for repeat users of the ED with a non-uniform number of visits to yield a more accurate estimate of the effect. To minimize the risk of model over-fitting, we reduced the number of primary discharge diagnoses to be included in the multivariate regression by using a univariate screen of p<0.2. The final model included age, gender, race, a Charlson comorbidity index score, and 24 primary discharge diagnosis groups. The Charlson index score included the number of comorbidities for each patient and was analyzed as a categorical variable (0,1,2,or 3+ comorbidities).20-22 All analyses were conducted at Kaiser Permanente Southern California’s Department of Research. Regression modeling was performed using PROC GENMOD in SAS EG 4.2 (Cary, NC).
RESULTS
Characteristics of Study Subjects
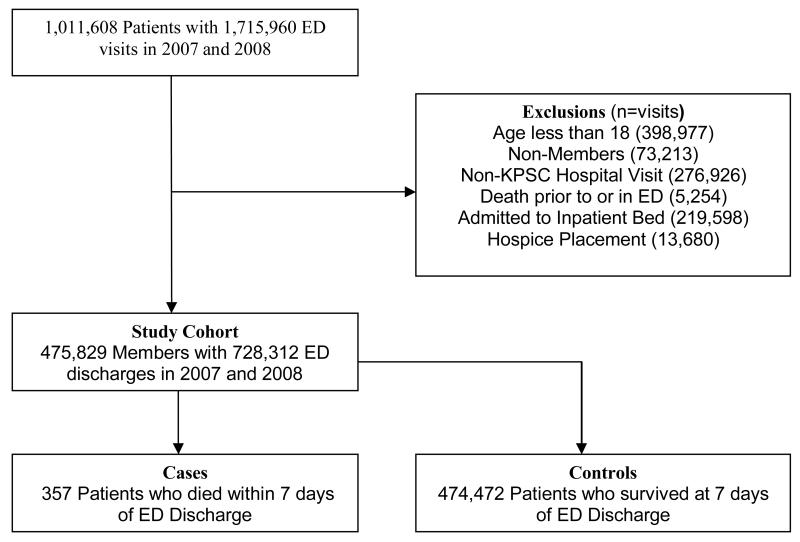
Over the two years, there were 1,011,608 patients who accounted for 1,715,960 visits to Southern California emergency departments (Figure 1). The study cohort contained 475,829 health plan members with 728,312 visits to emergency departments. The characteristics of the study cohort are presented in Table 1. The mean age of study cohort was 47 years (sd 18.3). A total of 357 patients died within 7 days after ED discharge with a mean age of 70.7 years (sd 15.6). More than 25% of patients who died within 7 days of ED discharge had at least one chronic and/or serious condition such as a previous myocardial infarction, congestive heart failure, peripheral vascular disease, pulmonary disease, renal disease, or diabetes with complications. Table 2 shows the causes of death at 7 days in decreasing frequency. Despite excluding hospice patients, the most common causes of death included malignancy (19.6%), coronary heart disease (17.3%), and non-atherosclerotic heart disease (11.3%). Table 3 provides visit level data on primary discharge diagnoses for the entire cohort and patients who experienced 7-day death after ED discharge. Results are presented with the most proximate ED visit linked to death.
Figure 1.
Flow diagram of study cohort
Table I.
Characteristics of the Study Cohort
| Characteristics | Total Cohort (N=475,829) |
Survived (N=475,472) |
Death within 7 days (N=357) |
|---|---|---|---|
| Age | |||
| 18-39 | 182,310 | 182,295 (38.3) | 15 (4.2) |
| 40-59 | 172,136 | 172,073 (36.2) | 63 (17.7) |
| 60-79 | 96,256 | 96,093 (20.2) | 163 (45.7) |
| 80+ | 25,127 | 25,011 (5.3) | 116 (32.5) |
| Gender | |||
| Female | 272,825 | 272,671 (57.4) | 154 (43.1) |
| Race/Ethnicity | |||
| White | 167,713 | 167,521 (35.2) | 192 (53.8) |
| Asian/PI | 34,942 | 34,929 (7.4) | 13 (3.6) |
| Black | 65,378 | 65,302 (13.7) | 76 (21.3) |
| Hispanic | 170,921 | 170,850 (35.9) | 71 (19.9) |
| Other/Unknown | 36,875 | 36,870 (7.8) | 5 (1.4) |
| Household income1 | |||
| <=38611 | 93,488 | 93,426 (19.7) | 62 (17.4) |
| 38612-50738 | 93,679 | 93,612 (19.7) | 67 (18.8) |
| 50739-63548 | 93,534 | 93,465 (19.7) | 69 (19.3) |
| 63549-81840 | 93,648 | 93,568 (19.7) | 80 (22.4) |
| 81841+ | 93,507 | 93,429 (19.7) | 78 (21.9) |
| Unknown | 7,973 | 7,972 (1.7) | 1 (0.3) |
| Comorbidity | |||
| Myocardial infarction | 22,089 | 21,999 (4.6) | 90 (25.2) |
| Congestive heart failure | 21,952 | 21,818 (4.6) | 134 (37.5) |
| Peripheral vascular disease |
15,305 | 15,213 (3.2) | 92 (25.8) |
| Cerebrovascular disease | 28,000 | 27,885 (5.9) | 115 (32.2) |
| Dementia | 2,665 | 2,642 (0.6) | 23 (6.4) |
| Chronic pulmonary disease |
95,394 | 95,246 (20) | 148 (41.5) |
| Rheumatologic disease | 9,772 | 9,745 (2.1) | 27 (7.6) |
| Pepticulcer disease | 4,065 | 4,049 (0.9) | 16 (4.5) |
| Mild liver disease | 2,952 | 2,944 (0.6) | 8 (2.2) |
| Diabetes | 32,822 | 32,786 (6.9) | 36 (10.1) |
| Diabetes with chronic complications |
3,7489 | 37,377 (7.9) | 112 (31.4) |
| Hemiplegia or paraplegia | 4,952 | 4,925 (1.0) | 27 (7.6) |
| Renal disease | 39,126 | 38,970 (8.2) | 156 (43.7) |
| Any (primary) malignancy | 25,584 | 25,520 (5.4) | 64 (17.9) |
| Moderate or severe liver disease |
1,687 | 1,678 (0.4) | 9 (2.5) |
| Metastatic solid tumor | 8,127 | 8,068 (1.7) | 59 (16.5) |
| AIDS | 1,520 | 1,519 (0.3) | 1 (0.3) |
Presented in quintiles
Table 2.
Causes of death at 7 days after ED
| Cause of Death1 | Frequency | Percent |
|---|---|---|
| Malignancy | 69 | 19.6% |
| Coronary heart disease | 61 | 17.3% |
| Non-atherosclerotic heart disease | 40 | 11.3% |
| DM | 23 | 6.5% |
| Hypertension | 19 | 5.4% |
| Cerebrovascular Disease | 17 | 4.8% |
| COPD/Asthma | 17 | 4.8% |
| Injury, Poisoning, and Suicide | 15 | 4.3% |
| Mental disorders | 14 | 4.0% |
| CHF | 10 | 2.8% |
| Renal disease | 10 | 2.8% |
| Pneumonia and pneumonitis | 10 | 2.8% |
| PVD, Circulatory disease, and Aneurysms |
9 | 2.6% |
| GI disorders | 9 | 2.6% |
| Other infections | 8 | 2.3% |
| Autoimmune disorders | 6 | 1.7% |
| Nervous system disorders | 5 | 1.4% |
| Sepsis | 4 | 1.1% |
| Liver disease | 3 | 0.9% |
| Metabolic, endocrine, nutritional disorders |
2 | 0.6% |
| Other | 2 | 0.6% |
Four deaths had unknown cause of death
Cause of death definitions are listed in the appendix
Table 3.
Discharge Diagnoses of Study Subjects
| Discharge Diagnosis | Total Cohort (N=728,312) |
Survived (N=727,955 (%)) |
Death within 7 Days (N=357) |
Chi Square |
|---|---|---|---|---|
| Other Injuries | 81,551 | 81,522 (11.2) | 29 (8.1) | 0.0654 |
| Minor Injuries | 64,119 | 64,095 (8.8) | 24 (6.7) | 0.1651 |
| Diseases of the musculoskeletal system, skin and connective tissue |
60,728 | 60,708 (8.3) | 20 (5.6) | 0.0614 |
| Other Respiratory Diseases | 21,510 | 21,491 (3.0) | 19 (5.3) | 0.0082 |
| Other Renal and GU Diseases | 35,193 | 35,174 (4.8) | 19 (5.3) | 0.6659 |
| Symptoms: Abdominal pain | 38,335 | 38,317 (5.3) | 18 (5.0) | 0.8513 |
| Symptoms: Other symptoms | 26,188 | 26,170 (3.6) | 18 (5.0) | 0.1421 |
| GI System Diseases | 53,701 | 53,683 (7.4) | 18 (5.0) | 0.0918 |
| Endocrine, nutritional, immunity and metabolic disorders |
8,093 | 8,076 (1.1) | 17 (4.8) | <0.0001 |
| Nervous System Disorders | 33,877 | 33,862 (4.7) | 15 (4.2) | 0.6865 |
| COPD | 9,692 | 9,678 (1.3) | 14 (3.9) | <0.0001 |
| Pneumonia | 4,316 | 4,303 (0.6) | 13 (3.6) | <0.0001 |
| Other residual codes | 26,269 | 26,256 (3.6) | 13 (3.6) | 0.972 |
| Urinary Tract infection | 20,079 | 20,068 (2.8) | 11 (3.1) | 0.7082 |
| Symptoms: Dizziness, vertigo and syncope | 23,603 | 23,593 (3.2) | 10 (2.8) | 0.6389 |
| Other Infectious and Parasitic Diseases | 8,928 | 8,918 (1.2) | 10 (2.8) | 0.0068 |
| DM | 6,922 | 6,912 (1.0) | 10 (2.8) | 0.0003 |
| Mental Illness | 19,593 | 19,584 (2.7) | 9 (2.5) | 0.8433 |
| Complications and Adverse events | 7,939 | 7,931 (1.1) | 8 (2.2) | 0.0362 |
| Neoplasms | 1,548 | 1,541 (0.2) | 7 (2.0) | <0.0001 |
| Circulatory Disorders | 6,645 | 6,639 (0.9) | 6 (1.7) | 0.1267 |
| Diseases of the blood | 2,305 | 2,299 (0.3) | 6 (1.7) | <0.0001 |
| Symptoms: Chest pain | 32,948 | 32,943 (4.5) | 5 (1.4) | 0.0045 |
| CHF | 1,603 | 1,598 (0.2) | 5 (1.4) | <0.0001 |
| Cerebrovascular Disease | 1,652 | 1,647 (0.2) | 5 (1.4) | <0.0001 |
| Upper respiratory infections | 25,025 | 25,021 (3.4) | 4 (1.1) | 0.0163 |
| Asthma | 8,385 | 8,381 (1.2 | 4 (1.1) | 0.9564 |
| Non-infectious Lung Disease | 955 | 951 (0.1) | 4 (1.1) | <0.0001 |
| Ischemic Heart Disease | 509 | 506 (0.1) | 3 (0.8) | <0.0001 |
| Renal Disease | 305 | 302 (0.04) | 3 (0.8) | <0.0001 |
| Major Injuries | 2,079 | 2,077 (0.3) | 2 (0.6) | 0.3304 |
| Symptoms: Headache | 22,783 | 22,781 (3.1) | 2 (0.6) | 0.0053 |
| HTN | 8,035 | 8,033 (1.1) | 2 (0.6) | 0.3259 |
| Dysrythmias | 12,120 | 12,118 (1.7) | 2 (0.6) | 0.1029 |
| Skin and Subcutaneous Infection | 16,737 | 16,736 (2.3) | 1 (0.3) | 0.0109 |
| Intestinal Infections | 1,299 | 1,299 (0.2) | 0 | 0.4244 |
| Non-atherosclerotic Heart Disease | 256 | 256 (0.04) | 0 | 0.723 |
| Pregnancy and childbirth related disorders | 24,423 | 24,423 (3.4) | 0 | 0.0004 |
Based on visit-level information
Main Results
Adjusted odds ratios for demographic variables and primary discharge diagnoses to predict 7-day ED death after discharge are presented in Table 4. This multivariate model adjusts for co-morbid conditions using a categorical Charlson comorbidity index. Increasing age and male gender are strongly predictive of early death after discharge. The top 5 primary discharge diagnoses predictive of 7-day death after discharge include non-infectious lung disease (OR 7.1, 95% CI 2.9-17.4) which includes the diagnosis of pleurisy, pneumothorax and pneumonitis, renal disease (OR 5.6, 95% CI 2.2-14.2), ischemic heart disease (OR 3.8, 95%CI 1.0-13.6), neoplasm (OR 3.7, 95%CI 1.0-13.4), and diseases of the blood with the majority being due to anemia or sickle cell disease (OR 3.6, 95%CI 1.6-8.1). Symptom based diagnoses were not associated with mortality.
Table 4.
Multivariable Logistic Regression for 7-day Death after
| CDhisacrhaacrgteeristic | Estimate | OR (95% CI) |
|---|---|---|
| Male1 | 0.5161 | 1.67 (1.3-2.1)* |
| Age2 | ||
| 40-59 | 0.9151 | 2.5 (1.4-4.5)* |
| 60-79 | 1.8016 | 6.1 (3.2-11.3)* |
| 80+ | 2.3562 | 10.6 (5.4-20.6)* |
| Race/Ethnicity3 | ||
| Asian/PI | −0.7982 | 0.5 (0.3-0.8) |
| Black | 0.0563 | 1.1 (0.8-1.4) |
| Hispanic | −0.322 | 0.7 (0.5-1.0) |
| Charlson Comorbidity Index4 | ||
| 1 | 0.4086 | 1.5 (0.9-2.5) |
| 2 | 1.0001 | 2.7 (1.6-4.7)* |
| 3+ | 1.895 | 6.7 (4.2-10.5)* |
| Discharge Diagnosis5 | ||
| Non-Infectious Lung Disease | 1.9632 | 7.1 (2.9-17.4)* |
| Renal Disease | 1.7231 | 5.6 (2.2-14.2)* |
| Ischemic Heart Disease | 1.3297 | 3.8 (1.0-13.6)* |
| Neoplasms | 1.2952 | 3.7 (1.0-13.4) |
| Diseases of the blood | 1.2876 | 3.6 (1.6-8.1)* |
| Major Injuries | 1.2197 | 3.4 (1.3-8.7)* |
| Other Infectious and Parasitic Diseases: Meningitis, Infective arthritis, Bacterial, Mycoses, Viral |
1.0847 | 3.0 (1.6-5.6)* |
| Pneumonia | 1.0514 | 2.9 (1.3-6.5)* |
| Endocrine, nutritional, immunity and metabolic disorders | 0.8789 | 2.4 (1.5-3.8)* |
| Cerebrovascular Disease | 0.6155 | 1.9 (0.7-4.8) |
| COPD | 0.5359 | 1.7 (1.0-3.0) |
| CHF | 0.3365 | 1.4 (0.5-3.8) |
| Other Respiratory Diseases | 0.263 | 1.3 (0.8-2.2) |
| DM | 0.1274 | 1.1 (0.6-2.2) |
| Minor Injuries | 0.0975 | 1.1 (0.8-1.6) |
| Upper respiratory infections | 0.0676 | 1.1 (0.6-2.0) |
| Circulatory Disorders | −0.1189 | 0.9 (0.4-2.1) |
| Other Injuries | −0.2095 | 0.8 (0.6-1.2) |
| Diseases of the musculoskeletal system, skin and connective tissue |
−0.2906 | 0.8 (0.5-1.1) |
| GI System Diseases | −0.3406 | 0.7 (0.5-1.1) |
| Symptoms: Chest pain | −0.8091 | 0.5 (0.2-0.8) |
| Symptoms: Headache | −0.9548 | 0.4 (0.08-2.0) |
| Dysrythmias | −1.4303 | 0.2 (0.06-0.9)* |
| Skin and Subcutaneous Infections | −1.5599 | 0.2 (0.08-0.6)* |
This multivariate model adjusts for comorbid conditions using a categorical Charlson comorbidity index
p *lt; 0.05
Reference group: Female
Reference group: Age 18-39
Reference group: White
Reference group: 0 = No comorbidities
Reference group: Absence of any of included diagnosis group
LIMITATIONS
Our study has potential limitations. First, despite the improved internal validity of our study due to consistent event capture methods, insurance coverage and access for all members, our results may not generalize to other settings. Although demographic characteristics of this managed care population are similar to the surrounding population in Southern California, our patient population may not match those of other regions. Furthermore, health plan members may have access to rapid outpatient evaluation that may not be available to the general population, and as a consequence, the practice patterns of emergency physicians in our study EDs may differ from other health systems. In addition, a population not represented in our sample are the un- or underinsured which could potentially be at greater risk for poor outcomes following ED discharge. Second, there were relatively few decedents in each of the primary discharge diagnosis categories, which contributes to the wide-confidence interval estimates. Third, although, we attempted to exclude possible expected deaths through the exclusion of patients referred to hospice or palliative care services, we were not able to exclude patients with Do Not Resuscitate (DNR) Orders. Our findings should be regarded as a first step in identifying high-risk discharge diagnoses rather than to provide a definitive rank ordering of such conditions.
Finally, our analysis is based on administrative data and cannot provide explanatory causal pathways between high-risk discharge diagnoses and increased mortality. Another potential limitation inherent to the use of administrative data is the possibility of miscoding. Although a blinded data analyst reviewed 20 charts from our cohort and validated the accuracy of the coding, the possibility of miscoding remains. Similarly, there is potential for misdiagnosis that an administrative study could miss. Future work may require detailed chart review and qualitative research methods to identify such mechanisms.
DISCUSSION
Early death after emergency department discharge raises important questions about the care delivered in emergency departments. To our knowledge, our findings represent the largest cohort study of mortality following emergency department discharge in the US. Our findings reveal some novel insights into patterns and predictors of short-term mortality after an ED visit and discharge. We found a mortality rate of 50 in 100,000 visits with the most common causes of death being malignancy, coronary heart disease, and non-atherosclerotic heart disease. Using multivariable logistic regression and controlling for demographics and comorbidities, we found increasing age, male gender, and the following 5 discharge diagnosis groups to be most highly associated with mortality after discharge: non-infectious lung disease, renal disease, ischemic heart disease, neoplasm, and diseases of the blood.
Extrapolation of our event rate (0.05% or 50 in 100,000) to the 83 million adult annual ED discharges in the U.S.3 suggest that 41,500 patients experience 7-day death after ED discharge. The rate is higher than has been previously reported by Sklar et al.4, 30 per 100,000, and Kefer et al.5,13 per 100,000, possibly due to an older and more complex patient population and a more complete and comprehensive event capture method. Compared to a recent Canadian study which found a rate of 0.075%, our study rates are only slightly lower, perhaps due in part to similarities between the integrated health care system of Kaiser Permanente and the Canadian system.6 These rates are dramatically lower then rates reported in a study conducted in Iceland (0.2% or 208 in 100,000) most likely due to the difference in the health care system, the patient population, and the reliability of the national registry.7 Our study found the three most common causes of short-term death in patients discharged from the emergency department to be malignancy (19.6%), coronary heart disease (17.3%), and non-atherosclerotic heart disease (11.3%), which includes peri-, endo-, or myocarditis, cardiomyopathy, dysrythmia, pulmonary heart disease and valve disorder. These findings are similar to national statistics in which the most common cause of death in all individuals is due to diseases of the heart (26%) and malignancy (23%).19, 23 It can be expected that patients with malignancies will have a high risk for cancer-related complications and mortality. What is more concerning are patients who died of a cardiac related event and were seen in the ED days prior.
Our data also demonstrates that there is an exponential increase in the association of post discharge death with age, with odds of death nearly tripling at each age group (compared to the youngest patients age 18-39): age 40-59 (OR 2.5, 95%CI 1.4-4.5), age 60-79 (OR 6.1, 95%CI 3.2-11.3), and age > 80 (OR 10.6, 95%CI 5.4-20.6). The increasing risk of mortality as a function of age has been reported in previous studies and may be a function of multiple co-morbidities.6, 24-27 These findings confirm the common perception that older patients in the ED require a careful evaluation and reduced hospitalization threshold compared to younger patients; nevertheless, age-related death is expected and may suggest that certain deaths following ED evaluation may not be preventable.
We found that male gender is associated with increased mortality, consistent with previous population-based studies evaluating all-cause death.24, 28-29 The race/ethnicity found to have a lower likelihood of post-ED discharge mortality was the category of Asian or Pacific Islander, a finding that is consistent with the National Vital Statistics Reports that describe national death rates of Asian/Pacific Islanders to be lowest of all ethnicities.30
We provide insights into the associations between certain primary discharge diagnoses and mortality. We found diagnoses that seem relatively unconcerning, such as non-infectious lung disease, which includes a diagnosis of pleurisy, pneumothorax, and pneumonitis, and diseases of the blood, which on further analysis were mainly comprised of the diagnosis of anemia, to have high odds of post-ED discharge short-term mortality. This can be a result of a misdiagnosis or an underestimation of risk. Patients with non-infectious respiratory complaints may have had an underlying process caused by a pulmonary embolus or pneumonia that was not recognized. Similarly, patients with diseases of the blood, such as anemia, may have had an underlying gastrointestinal bleed that was missed.
Patients discharged with diagnoses that have a potential for poor outcomes, specifically renal disease, which includes a diagnosis of nephritis, nephrosis, renal sclerosis, acute renal failure, and chronic renal failure, and ischemic heart disease, were also associated with a high likelihood of suffering post-ED discharge mortality. This suggests that the provider recognized the presence of a concerning underlying disease but either underestimated the severity or missed the cause of the presentation. Similar to ischemic heart disease, patients with end stage renal disease have been found to have a greater disease burden, reduced life-span, and greater cardiovascular risk.31-34 Patients with renal disease and ischemic heart disease may present to the emergency departments masking important symptoms and/or with complaints that “mimic” unconcerning diagnoses. Our study suggests that individuals with a high disease burden be carefully evaluated regardless of the complaint.
These findings warrant further investigation to understand the causal pathway between diagnosis and death. Given that many of these deaths may have been unexpected, it is important to understand better which may be preventable and which may not be given the complexity of the patient population and the inevitability of death with advancing age. A qualitative chart review is currently being conducted by our team to better understand the themes associated with mortality.
An important observation from this study is that symptom-based diagnoses did not predict post-ED discharge mortality. Our data thus argue against the common perception that symptom-based discharge diagnoses such as chest pain, abdominal pain, or syncope are high risk. The study by Kefer et al.5 published in 1994 suggested a possible relationship between symptom-based diagnoses and poor outcomes, while Sklar et al.4, published in 2007 found no relationship. One possible explanation is that in recent years, physicians exercise greater caution for symptoms without a specific cause, and they may have a lower threshold for augmented testing and diagnostic admission for such patients. It may also be that providers abstain from using a symptom based diagnosis as their primary discharge diagnosis for fear of revealing uncertainty.
Our study builds on the somewhat limited existing knowledgebase. The study conducted by Kefer et al. reported qualitative findings of 42 of 2,665 eligible medical examiner cases in Milwaukee County and found that cases with unexpected related deaths were rare, a diagnosis of aortic aneurysm should be maintained in ill patients, and that elderly patients with a fall may have a greater likelihood of death due to the injury.5 Sklar et al. conducted a qualitative review of 117 cases seen in the University of New Mexico over the course of ten years and found that the common themes associated with unexpected related deaths were abnormal vital signs, decompensation of a chronic disease, atypical presentation of a rare condition, and cognitive impairment.4 The previous studies are limited by sample size and incomplete data capture. Our database and linkage to external mortality information provide us with very complete comorbidity, diagnosis and outcomes data. We identified a higher rate of mortality (50 per 100,000) compared to Kefer et al. and Sklar et al. and found relationships between certain discharge diagnoses and mortality that to our knowledge have not been identified previously. Consistent with the findings of Sklar et al., three of the five discharge diagnoses we identified are chronic condition.
Our study identified potentially “high risk” discharge diagnoses in patients who suffer a short-term death after discharge. This finding suggests an important public health problem which requires further research to determine if death could be anticipated and if themes emerge that point to clinical scenarios, medical decisions, or health system actions that can be used to design quality improvement initiatives.
Supplementary Material
REFERENCES
- 1.Kohn L, Corrigen J, Donaldson M. In: To Err is Human: Building a Safer Health System. US Institute of Medicine CoQCiA, editor. National Academic Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- 2.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991 Feb 7;324(6):370–376. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 3.Pitts S, Niska R, Xu J, Burt C. National Hospital Ambulatory Medical Care Survey: 2006 emergency department. Natl Health Stat Report. 2008;6(7):1–38. [PubMed] [Google Scholar]
- 4.Sklar DP, Crandall CS, Loeliger E, Edmunds K, Paul I, Helitzer DL. Unanticipated death after discharge home from the emergency department. Ann Emerg Med. Jun 2007;49(6):735–745. doi: 10.1016/j.annemergmed.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 5.Kefer MP, Hargarten SW, Jentzen J. Death after discharge from the emergency department. Ann Emerg Med. Dec 1994;24(6):1102–1107. doi: 10.1016/s0196-0644(94)70239-x. [DOI] [PubMed] [Google Scholar]
- 6.Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011;342:d2983. doi: 10.1136/bmj.d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gunnarsdottir OS, Rafnsson V. Death within 8 days after discharge to home from the emergency department. European Journal of Public Health. 2008 Oct;18(5):522–526. doi: 10.1093/eurpub/ckn045. [DOI] [PubMed] [Google Scholar]
- 8.Schneider SM, Gallery ME, Schafermeyer R, Zwemer FL. Emergency department crowding: a point in time. Ann Emerg Med. 2003 Aug;42(2):167–172. doi: 10.1067/mem.2003.258. [DOI] [PubMed] [Google Scholar]
- 9.http://www.hcup-us.ahrq.gov/toolssoftware/icd_10/ccs_icd_10.jsp.
- 10.Burt CW, McCaig LF, Valverde RH. Analysis of ambulance transports and diversions among US emergency departments. Ann Emerg Med. 2006 Apr;47(4):317–326. doi: 10.1016/j.annemergmed.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Derlet R, Richards J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001 Feb;8(2):151–155. doi: 10.1111/j.1553-2712.2001.tb01280.x. [DOI] [PubMed] [Google Scholar]
- 12.Pines J, Localio A, Hollander J, et al. The impact of emergency department crowding measures on time to antibiotics for. Ann Emerg Med. 2007;50(5):510–516. doi: 10.1016/j.annemergmed.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 13.McCarthy ML, Zeger SL, Ding R, et al. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann Emerg Med. 2009 Oct;54(4):492–503. doi: 10.1016/j.annemergmed.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Sun BC, Mohanty SA, Weiss R, et al. Effects of hospital closures and hospital characteristics on emergency department ambulance diversion, Los Angeles County, 1998 to 2004. Ann Emerg Med. 2006 Apr;47(4):309–316. doi: 10.1016/j.annemergmed.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Hastings SN, Whitson HE, Purser JL, Sloane RJ, Johnson KS. Emergency department discharge diagnosis and adverse health outcomes in older adults. J Am Geriatr Soc. 2009 Oct;57(10):1856–1861. doi: 10.1111/j.1532-5415.2009.02434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Travers DA, Haas SW, Waller AE, Tintinalli JE. Diagnosis clusters for emergency medicine. Acad Emerg Med. 2003 Dec;10(12):1337–1344. doi: 10.1111/j.1553-2712.2003.tb00008.x. [DOI] [PubMed] [Google Scholar]
- 18.Oster A, Bindman AB. Emergency department visits for ambulatory care sensitive conditions: insights into preventable hospitalizations. Med Care. 2003 Feb;41(2):198–207. doi: 10.1097/01.MLR.0000045021.70297.9F. [DOI] [PubMed] [Google Scholar]
- 19.Heron M, Hoyert D, Murphy S, Xu J, Kochanek K, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57(14):1–134. [PubMed] [Google Scholar]
- 20.West DW, Satariano WA, Ragland DR, Hiatt RA. Comorbidity and breast cancer survival: a comparison between black and white women. Ann Epidemiol. 1996 Sep;6(5):413–419. doi: 10.1016/s1047-2797(96)00096-8. [DOI] [PubMed] [Google Scholar]
- 21.Davies SJ, Phillips L, Naish PF, Russell GI. Quantifying comorbidity in peritoneal dialysis patients and its relationship to other predictors of survival. Nephrol Dial Transplant. 2002 Jun;17(6):1085–1092. doi: 10.1093/ndt/17.6.1085. [DOI] [PubMed] [Google Scholar]
- 22.Lesens O, Methlin C, Hansmann Y, et al. Role of comorbidity in mortality related to Staphylococcus aureus bacteremia: a prospective study using the Charlson weighted index of comorbidity. Infect Control Hosp Epidemiol. 2003 Dec;24(12):890–896. doi: 10.1086/502156. [DOI] [PubMed] [Google Scholar]
- 23.Gunnarsdottir OS, Rafnsson V. Mortality of the users of a hospital emergency department. Emergency Medicine Journal. 2006 Apr;23(4):269–273. doi: 10.1136/emj.2005.026690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fried L, Kronmal R, Newman A, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health. JAMA. 1998;279(8):585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 25.Kohn R. Cause of death in very old people. JAMA. 1982;247(20):2793–2797. [PubMed] [Google Scholar]
- 26.Campbell A, Diep C, Reinken J, McCosh L. Factors predicting mortality in a total population sample of the elderly. J Epidemiol Community Health. 1985;39(4):337–342. doi: 10.1136/jech.39.4.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Menotti A, Kromhout D, Nissinen A, et al. Short-term all-cause mortality and its determinants in elderly male populations. Prev Med. 1996;25(3):319–326. doi: 10.1006/pmed.1996.0062. [DOI] [PubMed] [Google Scholar]
- 28.Wingard D, Suarez L, Barrett-Connor E. The sex differential in mortality from all causes and ischemic heart disease. Am J Epidemiol. 1983;117(2):165–172. doi: 10.1093/oxfordjournals.aje.a113527. [DOI] [PubMed] [Google Scholar]
- 29.Janghorbani M, Hedley A, Jones R, Zhianpour M, Gilmour W. Gender differential in all-cause and cardiovascular disease mortality. Int J Epidemiol. 1993;22(6):1056–1063. doi: 10.1093/ije/22.6.1056. [DOI] [PubMed] [Google Scholar]
- 30.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009 Apr 17;57(14):1–134. [PubMed] [Google Scholar]
- 31.Goodman WG, Goldin J, Kuizon BD, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000 May 18;342(20):1478–1483. doi: 10.1056/NEJM200005183422003. [DOI] [PubMed] [Google Scholar]
- 32.Collins AJ, Foley RN, Herzog C, et al. US Renal Data System 2010 Annual Data Report. Am J Kidney Dis. 2011 Jan;57(1 Suppl 1):A8, e1–526. doi: 10.1053/j.ajkd.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 33.Foley RN, Collins AJ. End-stage renal disease in the United States: an update from the United States Renal Data System. J Am Soc Nephrol. 2007 Oct;18(10):2644–2648. doi: 10.1681/ASN.2007020220. [DOI] [PubMed] [Google Scholar]
- 34.Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int. 1999 Dec;56(6):2214–2219. doi: 10.1046/j.1523-1755.1999.00773.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.