Abstract
Objective
To examine the association between the nursing home (NH) concentration of Hispanics and prevalence of pressure ulcer.
Design
Secondary data analysis using data from the national repository of the 2000 Minimum Data Set (MDS) and On-Line Survey Certification and Reporting (OSCAR) data. We used a multivariate logistic model, with the Huber-White correction to account for clustering of persons within a nursing facility, to examine the association of Hispanic NH concentration with the prevalence of pressure ulcers, after adjusting for resident level characteristics.
Setting
Five states with a high population of Mexican-Americans (California, New Mexico, Arizona, Colorado, and Texas).
Participants
A total of 74,343 persons (9.26% black, 11.28% Hispanic, 79.46% non-Hispanic white) in a NH located in 1 of these 5 states during the last quarter of 2000.
Measurements
The prevalence of Stage II–IV pressure ulcers was examined in the last quarter of 2000. Stage II–IV pressure ulcers, resident demographics, and medical illness data were documented by nursing staff on the MDS.
Results
Hispanics and non-Hispanic blacks had a higher prevalence of pressure ulcers than non-Hispanic whites (7.60%, 9.71% and 12.10%, respectively). A facility’s concentration of Hispanic residents was associated with prevalent pressure ulcers after adjustment for resident characteristics.
Conclusions
Residents in nursing homes in which there is a higher concentration of Hispanic residents are more likely to have a pressure ulcer.
Keywords: Hispanics, nursing homes, disparities, pressure ulcer
The occurrence of pressure ulcers may be one indicator of poor-quality nursing home (NH) care.1,2 The development of pressure ulcers in NH residents significantly impacts quality of life and there is increased morbidity and mortality associated with the presence of a pressure ulcer.3–7
Numerous studies have demonstrated racial disparities in NH care.8 –14 Studies concerning disparities in the development of pressure ulcers have focused primarily on comparing the black and non-Hispanic white (NHW) populations. Both incident and prevalent data suggest that black NH residents are more likely than NHWs to have a pressure ulcer.15,16 The risk of pressure ulcers among black NH residents is attributable to the presence of various characteristics including immobility, dementia, diabetes, fecal incontinence and urinary incontinence,15,16 the under and late recognition of Stage I pressure ulcers,17 and the lack of resources available to poor-quality NHs in which a predominant number of black residents live.14,18 –26
Recent analysis suggests that other minority groups, such as aging Hispanics, may be increasing their use of the NH.27 Little information is known, however, about pressure ulcers among Hispanic NH residents compared with other racial and ethnic groups. Hispanics may be at increased risk for poor-quality care, as has been demonstrated in other health care settings.28 Also, it is important to understand whether homes in which Hispanics are concentrated provide poor care, as has been demonstrated with the aging black population.14,26 The primary objective of this study, therefore, is to assess whether Hispanics, like their black minority counterparts, have a higher prevalence of pressure ulcer in the homes that serve high proportions of Hispanics in comparison with homes that only serve non-Hispanic whites.
METHODS
Data Sources
We used 2 data sources for the present analysis: the national repository of the Minimum Data Set (MDS) and the Online Survey Certification and Reporting (OSCAR) data. The MDS is a federally mandated report of health status, function, and demographic characteristics on all NH residents, which was designed to improve the quality of NH care through federal and state regulation of minimum quality standards.29 Nursing home staff complete the MDS assessments upon resident admission, quarterly and yearly thereafter, and when there is a change in the resident’s health condition. We used resident assessments completed in the second quarter of 2000 for our analyses.
The OSCAR database system is a comprehensive data network of NH structural characteristics and aggregate patient characteristics and is maintained by the Centers for Medicaid and Medicare Services.29 The data are reported by the NH before and during a state survey inspection and reviewed by NH inspectors. We used OSCAR data obtained in 2000 from the nursing facilities.
Study Sample
Nursing Homes
The NH sample consisted of freestanding NHs in urban counties in California, Arizona, New Mexico, Colorado, and Texas, thereby reducing the heterogeneity of the Hispanic population to Mexican Americans. Rural counties were not included because the distribution of Hispanics in rural NHs may be different when compared with the distribution of NHs located in urban areas.30,31 Further, NHs located in rural areas may have different long-term care service use.32 Hospital-based facilities were not included in the analysis because their services focus primarily on postacute care. Nursing homes with fewer than 20 beds were excluded from the analysis because smaller facilities may have different operating practices and data obtained from these homes provide unstable estimates because of the small number of residents.
Residents
The NH residents were long-stay residents. To distinguish the long-stay population from the short-stay or post-acute NH resident, long-stay was defined as having at least 1 MDS assessment 90 days before the assessment used for the present analysis, meaning that all residents had been in the facility for at least 90 days. Residents who were younger than 65 years, who were in a coma, or who could not be matched to an OSCAR facility record were not included in the analysis.
Study Variables
The stage of pressure ulcer represents the degree of tissue involvement: stage I (nonblanchable erythema of intact skin), stage II (partial-thickness skin loss), stage III (full-thickness skin loss but not through underlying fascia or muscle), or stage IV (full-thickness skin loss with damage to muscle, bone, or supporting structures). The outcome of interest was the presence of a stage II, III, or IV pressure ulcer. Residents were considered free of a pressure ulcer if the nursing staff did not indicate the presence of an ulcer. Stage I pressure ulcers were not included in the analysis, meaning that Stage I pressure ulcers were dropped from all analyses, because nursing staff often underdiagnose stage I ulcers in black and Hispanic NH residents.33
The exposure of interest was the resident’s ethnicity and race as recorded by the nursing staff on the resident’s admission assessment. Individuals were classified as “American Indian/Alaskan Native,” “Asian/Pacific Islander,” and “black, not of Hispanic origin,” “Hispanic,” or “white, not of Hispanic origin.”29 In this study we examined the non-Hispanic black, Hispanic, and non-Hispanic white resident populations. We present the data without the other racial groups (n = 3587) because our results were unchanged from the effect estimates including the “other” racial groups.
Resident-level characteristics that we controlled for in this study included age, gender, dementia, diabetes, heart failure, immobility (bedfast), chronic obstructive pulmonary disease (COPD), hip fracture, cancer, and fecal and urinary incontinence. Urinary incontinence included those with a report of any urinary incontinence or the presence of an indwelling catheter. By contrast, a resident was considered to be free of urinary incontinence if the resident had complete control and did not have an indwelling catheter.34
The facility-level characteristics we examined included profit status, Medicaid payer status, and the concentration of Hispanics in the NH. Based on the distribution of Hispanic residents within a NH across our sample of NHs, we created quintiles representing increasing concentration of Hispanics within a facility. Quintile 1 described NHs without Hispanic residents, quintile 2 described NHs with more than 0% to fewer than 3.0 % Hispanic residents in a facility, quintile 3 described NHs with 3.0% or more to fewer than 10% Hispanic residents, quintile 4 described NHs with 10% or more to fewer than 20% Hispanic residents, and quintile 5 described NHs with 20% or more Hispanic residents.
Data Analysis
Analyses were performed using STATA, version 9.1 (STATA Corp., College Station, TX). Differences in the distribution of various categorical and continuous variables between the respective ethnic/racial groups were examined using the chi square and t test, respectively. We used logistic regression analysis to examine the association between ethnicity and race with the presence of a pressure ulcer while controlling for known confounders. We applied the Huber-White Robust Estimator to adjust the standard errors of parameter estimates for clustering of adverse events within facilities. The Hispanic pressure ulcer rate for quintile 2, quintile 3, quintile 4, and quintile 5 was examined using a post-estimation procedure to adjust for resident-level characteristics.
RESULTS
Resident and Facility Descriptive Statistics
A total of 74, 343 NH residents in California, New Mexico, Colorado, Arizona, and Texas (9.26% black, 11.28% Hispanic, 79.46% non-Hispanic white, respectively) comprised the study sample (Table 1). The mean age of the study sample was 83.8 years (SD ±8.1), 75.6 % of whom were women. Stage II–IV pressure ulcers were reported in 8.2% of the study sample. Non-Hispanic whites were more likely than the other groups to be older, female, and have been previously diagnosed with COPD and heart failure. Black and Hispanic residents were more likely than non-Hispanic whites to have diabetes and fecal incontinence. Non-Hispanic blacks were the most likely to have dementia, urinary incontinence, and be bedfast when compared with the other groups.
Table 1.
Baseline Characteristics of Nursing Home Residents According to Ethnic and Racial Group
| Variable | Non-Hispanic White | Hispanic | Non-Hispanic Black |
|---|---|---|---|
| Demographics | |||
| Age (mean ± SD) | 84.33 ± 7.94 | 81.95 ± 8.36 | 81.70 ± 8.56 |
| Female,* % | 78.04 | 64.92 | 71.3 |
| Comorbid States | |||
| Dementia,* % | 40.35 | 37.01 | 40.84 |
| Diabetes,* % | 17.14 | 36.31 | 32.48 |
| Heart failure,* % | 17.27 | 14.98 | 15.84 |
| Bedfast,* % | 6.76 | 7.78 | 10.87 |
| COPD,* % | 12.77 | 10.31 | 10.55 |
| Hip fracture,* % | 7.44 | 5.17 | 2.64 |
| Cancer,* % | 4.79 | 3.30 | 4.72 |
| Urinary incontinence,* % | 77.75 | 75.58 | 80.50 |
| Fecal incontinence,* % | 65.23 | 65.08 | 71.93 |
COPD, chronic obstructive pulmonary disease.
P < .001 comparing a variable across the 3 ethnic/racial groups.
Pressure Ulcer Prevalence Rates
Table 2 shows the stage II–IV pressure ulcer prevalence among non-Hispanic whites, Hispanics, and non-Hispanic blacks. We observed the highest pressure ulcer rate for non-Hispanic blacks followed by Hispanics. Non-Hispanic whites were the least likely to have any stage of pressure ulcer compared with non-Hispanic blacks or Hispanics.
Table 2.
Stage of Pressure Ulcer According to Ethnicity and Race
| Stage | Non-Hispanic White
|
Hispanic
|
Non-Hispanic Black
|
|||
|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | |
| Stage II | 9.57 | 9.22–9.91 | 12.27 | 11.23–13.32 | 15.02 | 13.67–16.38 |
| Stage III | 2.81 | 2.61–3.00 | 3.61 | 3.07–4.16 | 6.90 | 6.00–7.80 |
| Stage IV | 2.27 | 2.08–2.45 | 3.88 | 3.25–4.52 | 7.27 | 6.21–8.33 |
| Stage II–IV | 7.60 | 7.36–7.79 | 9.71 | 9.07–10.34 | 12.10 | 11.33–12.87 |
CI, confidence interval.
Figure 1 shows the pressure ulcer rate according to the quintiles of the proportion of Hispanics in the facility. We observed an increase in the pressure ulcer rate in relation to the concentration of Hispanic NH residents. The pressure ulcer rate for Quintile 1 was less than the rates observed in quintile 3, quintile 4, and quintile 5. The 95% confidence interval for quintile 1 included the lower limit of the 95% confidence interval for quintile 2. We did not observe a significant difference between quintile 3, quintile 4, and quintile 5 based on the 95% confidence intervals.
Fig. 1.
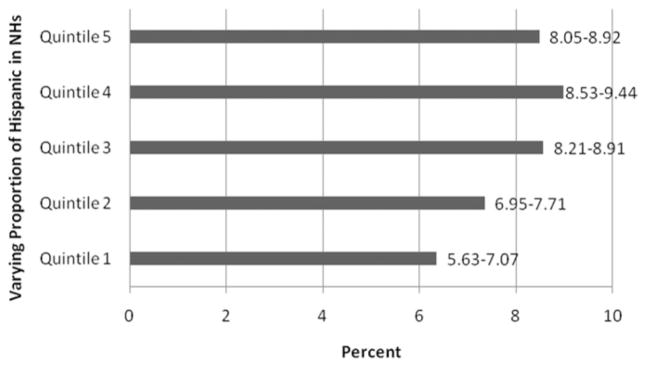
Stage II–IV pressure ulcer according to proportion of Hispanic NH residents. Quintile 1: 0% Hispanic residents, quintile 2: > 0% to < 3.0% Hispanic residents, quintile 3: ≥ 3.0 % to < 10% Hispanic residents, quintile: 4: ≥ 10% to 20% Hispanic residents, and quintile 5: ≥ 20% Hispanic residents.
Table 3 shows the facility characteristics according to the concentration of Hispanic residents in an NH. NHs with greater than 85% of their residents as Medicaid payer were most likely to be those with the highest concentration of Hispanics (17.2%, 14.6%, 20.3%, 24.4%, and 36.6%, P < .001 comparing quintile 1 through quintile 5, respectively). The same pattern was seen with for-profit homes (62.3%, 76.7%, 89.3%, 93.5%, and 89.3 %, P < .001 comparing quintile 1 through quintile 5, respectively).
Table 3.
Facility Characteristics According to the Concentration of Hispanic Residents
| Facility Characteristic | Concentration of Hispanic Residents
|
||||
|---|---|---|---|---|---|
| 0% | > 0% to < 3% | ≥ 3% to < 10 % | ≥ 10% to < 20% | ≥ 20 % | |
| > 85% Medicaid payer*, % | 17.2 | 14.6 | 20.3 | 24.4 | 36.6 |
| For-profit status*, % | 62.3 | 76.7 | 89.3 | 93.5 | 89.3 |
P < .001 comparing facility characteristic across the concentration of Hispanic residents.
Multivariate Analysis
Table 4 presents the results of our multivariate analyses. The data indicate the likelihood of pressure ulcer adjusting for selected resident and facility characteristics. Non-Hispanic blacks and Hispanics were more likely to have a pressure ulcer than non-Hispanic whites in our unadjusted analyses (model 1).
Table 4.
Association Between Pressure Ulcer and Various Resident and Facility Characteristics
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
|
| |||
| Odds Ratio (95% Confidence Interval) | |||
| Ethnic/racial group | |||
| Non-Hispanic white | 1.00 | 1.00 | 1.00 |
| Hispanic | 1.31 (1.21–1.42) | 1.15 (1.05–1.25) | 1.09 (0.99–1.18) |
| Black | 1.68 (1.55–1.82) | 1.36 (1.25–1.48) | 1.34 (1.23–1.42) |
| Resident characteristics | |||
| Age > 85* | 0.98 (0.93–1.04) | 0.99 (0.94–1.05) | |
| Female† | 0.77 (0.73–0.82) | 0.78 (0.73–0.83) | |
| Dementia‡ | 1.02 (0.97–1.08) | 1.02 (0.96–1.08) | |
| Diabetes‡ | 1.63 (1.53–1.74) | 1.63 (1.53–1.73) | |
| Heart failure‡ | 1.27 (1.18–1.36) | 1.27 (1.18–1.36) | |
| Bedfast‡ | 4.48 (4.18–4.81) | 4.52 (4.22–4.86) | |
| COPD‡ | 1.07 (0.98–1.17) | 1.06 (0.97–1.15) | |
| Hip fracture‡ | 1.52 (1.38–1.68) | 1.52 (1.38–1.68) | |
| Cancer‡ | 1.31 (1.16–1.47) | 1.30 (1.16–1.47) | |
| Fecal incontinence‡ | 2.47 (2.21–2.75) | 2.45 (2.20–2.73) | |
| Urinary incontinence‡ | 1.70 (1.48–1.95) | 1.71 (1.49–1.96) | |
| Proportion Hispanic | |||
| 0% Hispanics | 1.00 | ||
| > 0% to < 3% Hispanics | 1.20 (1.04–1.38) | ||
| ≥ 3% to < 10% Hispanics | 1.36 (1.19–1.57) | ||
| ≥ 10% to < 20% Hispanics | 1.41 (1.22–1.62) | ||
| ≥ 20 % Hispanics | 1.38 (1.20–1.60) | ||
Model 1, Unadjusted effect estimates.
Model 2, adjusted for ethnicity/race and clinical characteristics.
Model 3, adjusted for ethnicity/race, clinical characteristics, increasing proportion of Hispanics in a nursing home, >85% Medicaid payer, for-profit status.
Reference age ≤ 85.
Reference male gender.
Reference no medical illness.
Adjustment for medical diagnosis, age, and gender attenuated the relationship between race/ethnicity and pressure ulcer (model 2). Black race and Hispanic ethnicity were associated with having a pressure ulcer. Male gender, diabetes, heart failure, immobility, COPD, hip fracture, cancer, and fecal and urinary incontinence were associated with pressure ulcer in model 2.
In the final adjusted model, black race was significantly associated with prevalent pressure ulcers (model 3). The data in model 3 also show that NHs with high proportions of Hispanic residents were associated with a higher prevalence of pressure ulcer when compared to homes with no Hispanics. Including the proportion of Hispanic NH residents in the model did not alter the effect estimates for most of the demographic and clinical variables that were independently associated with pressure ulcer in model 2. For Hispanic residents, the predicted probability of a Hispanic resident having a pressure ulcer was 3.07% (95% CI 2.70–3.44) in quintile 2, 16.39% (95% CI 15.60–17.18) in quintile 3, 24.76% (95% CI 23.84–25.68) in quintile 4, and 55.77% (95% CI 54.72–56.83) in quintile 5.
DISCUSSION
This study demonstrates 2 key findings. First, Hispanics have higher rates of pressure ulcer than their white non-Hispanic counterparts, controlling for confounding factors; and second, an older Hispanic living in an NH with more Hispanic residents, all other factors being equal is much more likely to have a pressure ulcer than an older Hispanic residing in a home with fewer Hispanics. The finding of a connection between the proportion of Hispanics in a home and this important quality measure may have implications related to reducing pressure ulcer.
After adjustment for resident characteristics, Hispanic ethnicity and black race were associated with pressure ulcer when compared with non-Hispanic whites (Table 4, model 2). Our finding that black race and Hispanic ethnicity were associated with pressure ulcer after adjustment for resident characteristics highlights the importance of developing interventions to detect stage I ulcers in these populations to reduce the risk of higher stage ulcers emerging.17
When we added the proportion of Hispanics in a home, Hispanic ethnicity was no longer associated with pressure ulcer suggesting that the ethnic difference in pressure ulcer rates is presumably attributable to the care provided by the NH. An interesting discovery is that the elevated association with pressure ulcer occurs even if there are only a few Hispanics in an NH suggesting a disparity as to where Hispanics are sent to for NH care. We did observe differences in the pressure ulcer rate for Hispanics between homes that serve Hispanics such that the pressure ulcer rate for Hispanics increased in direct relation to the NH concentration of Hispanics. The observed differences in the rate of pressure ulcers are attributable to the types of facilities Hispanics are served by, rather than the fact that these residents are Hispanic.
Based on previous methodology, we examined the effect of NH concentration of Hispanics on pressure ulcer after controlling for resident characteristics.34 In controlling for clinical characteristics we reduce the greater burden of disease among Hispanics and non-Hispanic blacks (Table 1) as an alternative explanation for the relation between pressure ulcer and concentration of Hispanics in a home.
The difference in pressure ulcer observed between homes with Hispanics and those without Hispanics may be due to the resources a nursing home has to care for all of its residents.26 The observed difference between homes with and without Hispanics, which deserves further exploration, is the extent to which a higher Medicaid payer mix and therefore reduced resources affects pressure ulcers (Table 2), and is consistent with the 2-tier system of NH care observed for non-Hispanic blacks.26
Identifying clinical factors associated with pressure ulcer is part of the recommended strategy for prevention of pressure ulcer.35 In our study, fecal and urinary incontinence, immobility, heart failure, diabetes, COPD, cancer, and hip fracture were independently associated with pressure ulcer. Consistent with previous studies, these specific medical diagnoses and measure of functional status lead to the pathological changes in blood supply to the dermal and underlying tissues that predispose residents to pressure ulcer.34 Health care providers should have a high index of suspicion for pressure ulcer in these patients. Our work further supports the need to adjust for these predictors in statistical models examining disparities in pressure ulcer.
This study has several limitations. First, the cross-sectional nature of this study limits our observations to prevalent pressure ulcer. We do not have information on incident pressure ulcer (eg, NH-acquired pressure ulcer). It could be that His-panics are coming into the NH with a pressure ulcer. Future research should address incident pressure ulcer in order to examine the risk of disparities in NH-acquired pressure ulcer. Second, this study was conducted in the 5 states with the highest concentration of Mexican-Americans: California, Arizona, New Mexico, Texas, and Colorado. We do not know if the risk of pressure ulcer is different outside those states. It may be that the provision of matching ethnic background between the nurses (or nurse aides) and the Hispanic residents occurs in NHs in these 5 states. Last, our information on clinical diagnosis is limited to information collected on the MDS.
There are several strengths to the current study. Our results showed an association between black race and pressure ulcer that is consistent with previous work that found pressure ulcer prevalence related to selected resident characteristics.15,16 In addition, MDS data has undergone extensive validity and reliability testing.26,36,37 Individual assessment items in such areas as functional and cognitive status and resident diagnoses have also demonstrated reliability and validity in several large scale studies undertaken in multiple nursing facilities.38–41
Disparities in NH care clearly exist beyond black and white differences. We have demonstrated that the residents of NHs in which Hispanics reside— black, white, or Hispanic—are more likely to have a pressure ulcer. Further, Hispanics are more likely to have a pressure ulcer in NHs that house a greater share of Hispanics. Future investigations should evaluate whether our findings would hold for NH-acquired pressure ulcer.36
Acknowledgments
This research was supported by Grants HS0001122 National Institutes of Health (NIH) National Research Service Award (NRSA) Institutional Training Grant (T32) through the Agency for Healthcare Research and Quality (AHRQ), State Policies Impact on Outcomes NIA grant R01AG020557 and CMWF20050318 Commonwealth Fund.
References
- 1.Lyder CH. Pressure ulcer prevention and management. JAMA. 2003;289:223–226. doi: 10.1001/jama.289.2.223. [DOI] [PubMed] [Google Scholar]
- 2.Mor V. Defining and measuring quality outcomes in long-term care. J Am Med Dir Assoc. 2007;8:129–137. doi: 10.1016/j.jamda.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Berlowitz DR, Brandeis GH, Anderson J, et al. Effect of pressure ulcers on the survival of long-term care residents. J Gerontol A Biol Sci Med Sci. 1997;52:M106–110. doi: 10.1093/gerona/52a.2.m106. [DOI] [PubMed] [Google Scholar]
- 4.Bryan CS, Dew CE, Reynolds KL. Bacteremia associated with decubitus ulcers. Arch Intern Med. 1983;143:2093–2095. [PubMed] [Google Scholar]
- 5.Reuler JB, Cooney TG. The pressure sore:pathophysiology and principles of management. Ann Intern Med. 1981;94:661–666. doi: 10.7326/0003-4819-94-5-661. [DOI] [PubMed] [Google Scholar]
- 6.Smith DM. Pressure ulcers in the nursing home. Ann Intern Med. 1995;123:433–442. doi: 10.7326/0003-4819-123-6-199509150-00008. [DOI] [PubMed] [Google Scholar]
- 7.Sugarman B. Osteomyelitis in spinal cord injury. Arch Phys Med Rehabil. 1984;65:132–134. [PubMed] [Google Scholar]
- 8.Allsworth JE, Toppa R, Palin NC, et al. Racial and ethnic disparities in the pharmacologic management of diabetes mellitus among long-term care facility residents. Ethn Dis. 2005;15:205–212. [PubMed] [Google Scholar]
- 9.Bernabei R, Gambassi G, Lapane K, et al. Management of pain in elderly patients with cancer. SAGE Study Group. Systematic Assessment of Geriatric Drug Use via Epidemiology. JAMA. 1998;279:1877–1882. doi: 10.1001/jama.279.23.1877. [DOI] [PubMed] [Google Scholar]
- 10.Castle NG, Mor V. Physical restraints in nursing homes: A review of the literature since the Nursing Home Reform Act of 1987. Med Care Res Rev. 1998;55:139–170. doi: 10.1177/107755879805500201. [DOI] [PubMed] [Google Scholar]
- 11.Christian JB, Lapane KL, Toppa RS. Racial disparities in receipt of secondary stroke prevention agents among US nursing home residents. Stroke. 2003;34:2693–2697. doi: 10.1161/01.STR.0000096993.90248.27. [DOI] [PubMed] [Google Scholar]
- 12.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730–1736. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- 13.Lapane KL, Fernandez HH, Friedman JH. Prevalence, clinical characteristics, and pharmacologic treatment of Parkinson’s disease in residents in long-term care facilities. SAGE Study Group. Pharmacotherapy. 1999;19:1321–1327. doi: 10.1592/phco.19.16.1321.30877. [DOI] [PubMed] [Google Scholar]
- 14.Smith D, Feng Z, Fennell M, et al. Separate and unequal: Racial segregation and disparities across US nursing homes. Health Aff. 2007;26:1448–1458. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- 15.Baumgarten M, Margolis D, van Doorn C, et al. Black/white differences in pressure ulcer incidence in nursing home residents. J Am Geriatr Soc. 2004;52:1293–1298. doi: 10.1111/j.1532-5415.2004.52358.x. [DOI] [PubMed] [Google Scholar]
- 16.Lapane KL, Jesdale W, Zierler S. Racial differences in pressure ulcer prevalence in nursing homes. J Am Geriatr Soc. 2005;53:1077–1078. doi: 10.1111/j.1532-5415.2005.53338_5.x. [DOI] [PubMed] [Google Scholar]
- 17.Lyder CH, Yu C, Stevenson D, et al. Validating the Braden Scale for the prediction of pressure ulcer risk in non-Hispanic blacks and Latino/Hispanic elders: A pilot study. Ostomy Wound Manage. 1998;44:42S–49S. discussion 50S. [PubMed] [Google Scholar]
- 18.Cherry RL. Agents of nursing home quality of care: Ombudsmen and staff ratios revisited. Gerontologist. 1991;31:302–308. doi: 10.1093/geront/31.3.302. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J, Spector W. The effect of medicaid reimbursement on quality of care in nursing homes. J Health Econ. 1996;15:23–48. doi: 10.1016/0167-6296(95)00030-5. [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine. Nursing Staffing in Hospitals and Nursing Homes: Is It Adequate? Washington, DC: National Academy Press; 1996. [Google Scholar]
- 21.Institute of Medicine. Improving the Quality of Long-Term Care. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 22.Munroe DJ. The influence of registered nurse staffing on the quality of nursing home care. Res Nurs Health. 1990;13:263–270. doi: 10.1002/nur.4770130409. [DOI] [PubMed] [Google Scholar]
- 23.Spector WD, Takada HA. Characteristics of nursing homes that affect resident outcomes. J Aging Health. 1991;3:427–454. doi: 10.1177/089826439100300401. [DOI] [PubMed] [Google Scholar]
- 24.Zinn J. The influence of nurse wage differentials on nursing home staffing and resident care decisions. Gerontologist. 1993;33:721–729. doi: 10.1093/geront/33.6.721. [DOI] [PubMed] [Google Scholar]
- 25.Howard PA, Shireman TI, Dhingra A, et al. Patterns of ACE inhibitor use in elderly Medicaid patients with heart failure. Am J Geriatr Cardiol. 2002;11:287–294. doi: 10.1111/j.1076-7460.2002.01212.x. [DOI] [PubMed] [Google Scholar]
- 26.Mor V, Zinn J, Angelelli J, et al. Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82:227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gerardo M, Feng Z, Teno JM, Mor V. Concentration of foreign-born Hispanics associated with skilled nursing facility admission rates: A county-level analysis. Gerontologist. 2008 Under review. [Google Scholar]
- 28.Kandula NR, Lauderdale DS, Baker DW. Differences in self-reported health among Asians, Latinos, and non-Hispanic whites: The role of language and nativity. Ann Epidemiol. 2007;17:191–198. doi: 10.1016/j.annepidem.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Medicaid and Medicare Services (CMS). U.S. Department of Health and Human Services. [Accessed February 12, 2007];CMS home page. Available at: http://www.cms.hhs.gov.
- 30.Baxter J, Bryant LL, Scarbro S, et al. Patterns of rural Hispanic and non-Hispanic white health care use: The San Luis Valley Health and Aging Study. Res Aging. 2001;23:37–60. [Google Scholar]
- 31.Hamman RF, Mulgrew CL, Baxter J, et al. Methods and prevalence of ADL limitations in Hispanic and non-Hispanic white subjects in rural Colorado: The San Luis Valley Health and Aging Study. Ann Epidemiol. 1999;9:225–235. doi: 10.1016/s1047-2797(98)00036-2. [DOI] [PubMed] [Google Scholar]
- 32.Fennell ML, Campbell SE. The regulatory environment and rural hospital long-term care strategies from 1997 to 2003. J Rural Health. 2007;23:1–9. doi: 10.1111/j.1748-0361.2006.00061.x. [DOI] [PubMed] [Google Scholar]
- 33.Lyder CH, Yu C, Emerling J, et al. The Braden Scale for pressure ulcer risk: Evaluating the predictive validity in black and Latino/Hispanic elders. Appl Nurs Res. 1999;12:60– 68. doi: 10.1016/s0897-1897(99)80332-2. [DOI] [PubMed] [Google Scholar]
- 34.Berlowitz DR, Brandeis GH, Anderson J, et al. Evaluation of a risk-adjustment model for pressure development using the Minimum Data Set. J Am Geriatr Soc. 2001;49:872–876. doi: 10.1046/j.1532-5415.2001.49176.x. [DOI] [PubMed] [Google Scholar]
- 35.Thomas DR. Prevention and treatment of pressure ulcers. J Am Med Dir Assoc. 2006;1:46–59. doi: 10.1016/j.jamda.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 36.Grabowski DC, Angelelli JJ, Mor V. Medicaid payment and risk-adjusted nursing home quality measures. Health Aff (Millwood) 2004;23:243–252. doi: 10.1377/hlthaff.23.5.243. [DOI] [PubMed] [Google Scholar]
- 37.Mor V. Improving the quality of long-term care with better information. Milbank Q. 2005;85:333–364. doi: 10.1111/j.1468-0009.2005.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morris JN, Sherwood CC, Dreyer P. Inspection of care: Findings from an innovative demonstration. Health Care Financ Rev. 1989;11:57–63. [PMC free article] [PubMed] [Google Scholar]
- 39.Morris J, Nonemaker S, Murphy K, et al. A commitment to change: Revision of HCFA’s RAI. J Am Geriatr Soc. 1997;45:1011–1016. doi: 10.1111/j.1532-5415.1997.tb02974.x. [DOI] [PubMed] [Google Scholar]
- 40.Hawes C, Mor V, Phillips CD, et al. The OBRA-87 nursing home regulations and implementation of the Resident Assessment Instrument: Effects on process quality. J Am Geriatr Soc. 1997;45:977–985. doi: 10.1111/j.1532-5415.1997.tb02970.x. [DOI] [PubMed] [Google Scholar]
- 41.Gambassi G, Landi F, Peng L, et al. Validity of diagnostic and drug data in standardized nursing home resident assessments: Potential for geriatric pharmacoepidemiology. SAGE Study Group Systematic Assessment of Geriatric Drug Use via Epidemiology. Med Care. 1998;36:167–179. doi: 10.1097/00005650-199802000-00006. [DOI] [PubMed] [Google Scholar]


