Abstract
Purpose
To report the efficacy of intravitreal dexamethasone implant in a patient with retinitis pigmentosa and bilateral cystoid macular edema unresponsive to topical carbonic anhydrase inhibitors.
Case Report
A 36-year-old man with bilateral cystoid macular edema associated with retinitis pigmentosa that was unresponsive to topical carbonic anhydrase inhibitors underwent bilateral 0.7-mg intravitreal dexamethasone implants two weeks apart. Spectral domain optical coherence tomography revealed resolution of macular edema one week following each injection in both eyes and his visual acuity improved. However, macular edema recurred two months later in OS and three months later in OD. Second implant was considered for both eyes. No implant-related complication was experienced during the follow-up of seven months.
Conclusion
Inflammatory process seems to play a role in retinitis pigmentosa. Intravitreal dexamethasone implant may offer retina specialists a therapeutic option especially in cases unresponsive to other treatment regimens in eyes with retinitis pigmentosa-related macular edema.
Key words: Intravitreal dexamethasone implant, Retinitis pigmentosa, Macular edema
Introduction
The central vision is relatively spared up to the later stages of disease process in patients with retinitis pigmentosa (RP) [1]. However, when macular complications such as macular edema occur central vision is often dramatically impaired much earlier. In a very recent study with optical coherence tomography (OCT), Hajali et al. [2] showed that 20 of 63 patients with RP (32%) exhibited cystoid macular edema (CME) in at least one eye, whereas 11 patients (18%) even had CME in both eyes.
The pathogenesis of RP-related macular edema is still not known. Spalton et al. [3] investigated 25 patients with RP and angiographic retinal leakage. Edema was present in dominant and X-linked inherited disease and was likely to be present in recessive disease as well. The authors suggested that this might be a general inflammatory response seen in many types of tapetoretinal degeneration against actively degenerating photoreceptors and retina pigment epithelium (RPE). Küchle and associates [4] investigated blood-aqueous barrier in patients with RP with a laser cell photometer in 56 eyes of 29 patients and found that aqueous flare values were higher in patients with RP than in controls and patients with RP-related CME had even higher values with a mean of 14.66 photon counts per millisecond compared with 9.65 for patients with RP without CME. Furthermore, Heckenlively and colleagues [5] looked for the presence of antiretinal antibodies in a group of 30 consecutive patients with RP and CME, 30 consecutive patients with RP but without CME and 50 normal subjects. Twenty-seven (90%) of patients with RP and CME had antiretinal protein antibody activity compared with three (6%) of 50 normal subjects and only four (13%) of 30 control patients with RP with no CME. This study suggests that patients with RP and CME may have an underlying autoimmune process that is contributing to the macular edema formation in RP. Based on these findings, intravitreal steroids were administered in small case series with RP-related CME to modulate this autoimmune process and the inflammatory mediators [6, 7, 8, 9]. Moreover very recently, Yoshida et al. [10] retrospectively looked for the clinical evidence of sustained chronic inflammatory reaction in 371 consecutive patients with typical RP and showed that 37.3% of eyes had signs of inflammatory cells in the anterior vitreous cavity. In addition, the levels of proinflammatory cytokines and chemokines appeared to be increased in the aqueous and vitreous of RP patients.
In this case report, we describe our experience in a patient with RP and long-standing CME refractory to topical dorzolamide treatment, treated with bilateral intravitreal 0.7-mg dexamethasone implant (Ozurdex).
Case Report
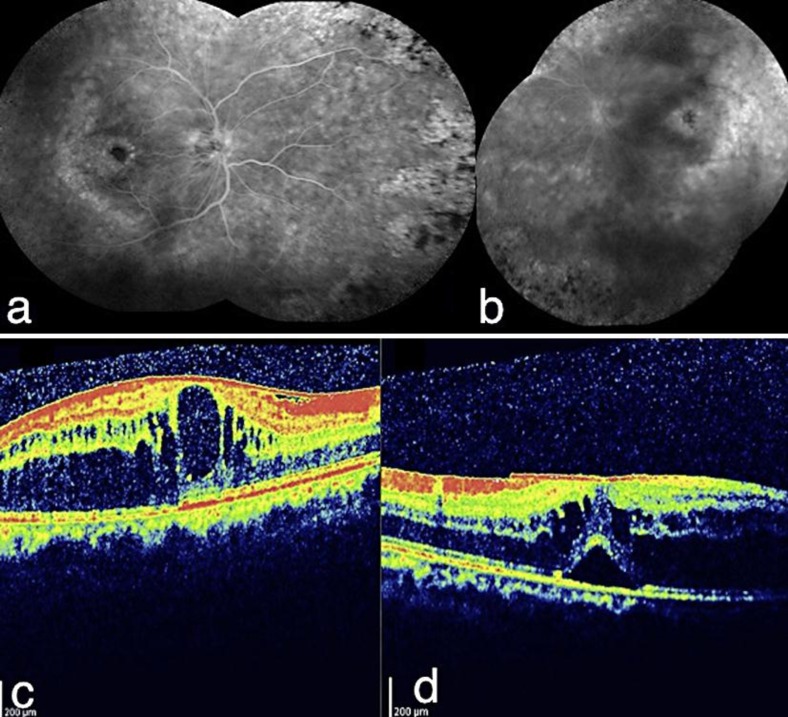
A 36-year-old man with a history of bilateral mild to moderate visual deterioration of six months’ duration with RP was referred to us for further evaluation. At the time of our examination visual acuity was 2/10 OU. Slit-lamp examination revealed bilateral mild posterior subcapsular cataract formation. Intraocular pressures were normal. On funduscopy and contact lens biomicroscopy, there were fundus changes typical for RP; bone-spicule-type intraretinal pigmentation in the mid-periphery with attenuated retinal vessels and bilateral macular edema. Fluorescein angiography and OCT exhibited CME and taut posterior hyaloid OU (fig. 1a–d). Extinguished electroretinogram recordings of all three scotopic recordings (rod, maximum, oscillatory) revealed decreased amplitudes and white-light-adapted cone response was subnormal. These findings supported the diagnosis of RP.
Fig. 1.
Fluorescein angiography, composite picture, significant petaloid-type macular edema (a right eye; b left eye), optic coherence tomography demonstrating the cystoid macular edema (c right eye; d left eye).
He was put on topical dorzolamide three times a day for almost a year without any change in visual acuity OU. As no visual improvement could be achieved with topical dorzolamide treatment, the patient was offered intravitreal dexamethasone implant (Ozurdex) for the right eye and possible injection-related complications were explained in detail.
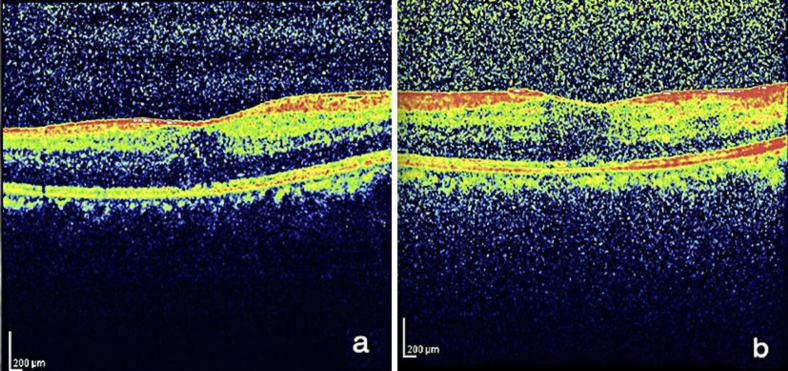
One week after the injection, his visual acuity improved 4/10 in OD and macular edema resolved (fig. 2). As the patient was exhilarated by this result, he demanded Ozurdex injection for his left eye also. Two weeks later, the left eye was also injected. Similar to the right eye, visual acuity improved to 4/10 and edema resolved in OS despite the presence of taut hyaloid.
Fig. 2.
One week after the intravitreal dexamethasone implant (a right eye; b left eye).
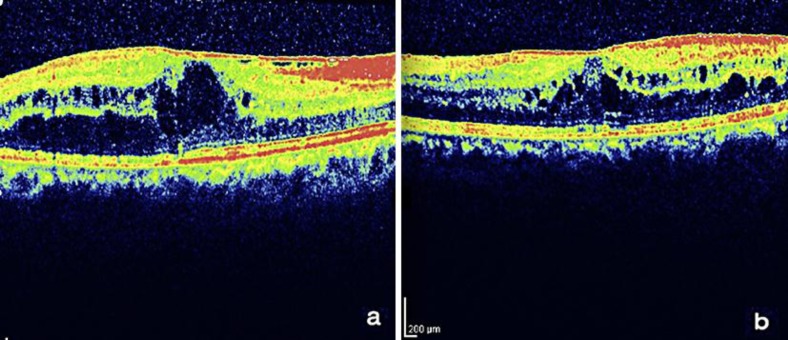
However, edema recurred two months after the injection in OS and three months after the injection in OD (fig. 3). Visual acuity returned to the pre-injection level of 2/10 bilaterally. The patient was offered second injection for both eyes but due to financial problems, he decided to wait for reimbursement of Ozurdex. No injection-related complication occurred during the follow-up of seven months.
Fig. 3.
Macular edema recurred at 3rd postinjection month in OD (a) and 2nd postinjection month in OS (b).
Discussion
Previously intravitreal triamcinolone acetonide injection was administered with some success in small case series of RP patients with CME [6, 7, 8, 9]. In a retrospective study Ozdemir et al. [8] reported the efficacy of intravitreal 4-mg triamcinolone acetonide in a group of five eyes of five patients with CME secondary to RP. The baseline median central macular thickness was 418 μm. At 1 month, the median central macular thickness had decreased to 224 μm. At 3 and 6 months, the median central macular thickness was 275 and 312 μm, respectively. In three eyes, edema recurred. Despite good anatomic outcome, no improvement in visual acuity was achieved in three of five eyes. There is only one prospective nonrandomized comparative trial about the effect of 4-mg intravitreal triamcinolone acetonide injection on CME [11]. In this study, while 20 eyes of 20 patients received the injection, 20 eyes of 20 patients who denied the injection therapy comprised the control group. The authors showed that the mean central macular thickness decreased from 459.86 to 306.75 μm at the first post-injection month but this value returned to 442 μm at the 12th month. On the other hand, there was no statistically significant difference between the two groups’ visual acuity at month 12. They concluded that intravitreal triamcinolone acetonide might be useful for some selected cases of RP patients with CME.
A sustained-release dexamethasone implant has recently been available for the treatment of macular edema secondary to retinal vein occlusion [12, 13]. It has been shown that its side effect profile is much better than intravitreal triamcinolone acetonide injection. Very recently Srour et al. [14] administered intravitreal dexamethasone implant (Ozurdex) in a group of four eyes of three patients with RP and CME. All patients completed six months of follow-up. In all eyes CME regressed noticeably. At the baseline, mean macular thickness was 443 μm. Mean macular thickness improved to 234 μm at 1 month, 332 μm at 3 months and 305 μm at 6 months. Mean visual acuity improved from 20/160 to 20/100 at 1 month, to 20/125 at 3 months and to 20/125 at 6 months. However, in two patients macular edema recurred at the third post-injection month and repeat implant administration was performed.
In our case, despite the long-standing macular edema and already present taut posterior hyaloid, both eyes initially responded well to intravitreal dexamethasone implant with anatomical and functional improvement. However, at the second and third post-injection month edema recurred bilaterally. Further preferably randomized trials may establish the place of intravitreal dexamethasone implant in the treatment armamentarium of RP-related CME.
Disclosure Statement
The authors have no proprietary or commercial interest in any materials discussed in this article.
References
- 1.Ikeda Y, Hisatomi T, Yoshida N, Notomi S, Murakami Y, Enaida H, Ishibashi T. The clinical efficacy of a topical dorzolamide in the management of cystoid macular edema in patients with retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol. 2012;250:809–814. doi: 10.1007/s00417-011-1904-5. [DOI] [PubMed] [Google Scholar]
- 2.Hajali M, Fishman GA, Anderson RJ. The prevalence of cystoid macular oedema in retinitis pigmentosa patients determined by optical coherence tomography. Br J Ophthalmol. 2008;92:1065–1068. doi: 10.1136/bjo.2008.138560. [DOI] [PubMed] [Google Scholar]
- 3.Spalton DJ, Bird AC, Cleary PE. Retinitis pigmentosa and retinal oedema. Br J Ophthalmol. 1978;62:174–182. doi: 10.1136/bjo.62.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Küchle M, Nguyen NX, Schalnus R, Freissler K, Lüchtenberg M, Müller M. Quantification of disorders of the blood-aqueous humor barrier in retinitis pigmentosa-initial results. Klin Monbl Augenheilkd. 1994;204:211–216. doi: 10.1055/s-2008-1035519. [DOI] [PubMed] [Google Scholar]
- 5.Heckenlively JR, Jordan BL, Aptsiauri N. Association of antiretinal antibodies and cystoid macular edema in patients with retinitis pigmentosa. Am J Ophthalmol. 1999;127:565–573. doi: 10.1016/s0002-9394(98)00446-2. [DOI] [PubMed] [Google Scholar]
- 6.Wang C, Hu J, Bernstein PS, Teske MP, Payne M, Yang Z, Li C, Adams D, Baird JH, Zhang K. Intravitreal injection of triamcinolone acetonide for macular edema due to retinitis pigmentosa and other retinal diseases. Adv Exp Med Biol. 2006;572:309–314. doi: 10.1007/0-387-32442-9_43. [DOI] [PubMed] [Google Scholar]
- 7.Saraiva VS, Sallum JM, Farah ME. Treatment of cystoid macular edema related to retinitis pigmentosa with intravitreal triamcinolone acetonide. Ophthalmic Surg Lasers Imaging. 2003;34:398–400. [PubMed] [Google Scholar]
- 8.Ozdemir H, Karacorlu M, Karacorlu S. Intravitreal triamcinolone acetonide for treatment of cystoid macular oedema in patients with retinitis pigmentosa. Acta Ophthalmol Scand. 2005;83:248–251. doi: 10.1111/j.1600-0420.2005.00395.x. [DOI] [PubMed] [Google Scholar]
- 9.Kim JE. Intravitreal triamcinolone acetonide for treatment of cystoid macular edema associated with retinitis pigmentosa. Retina. 2006;26:1094–1096. doi: 10.1097/01.iae.0000254897.86389.a5. [DOI] [PubMed] [Google Scholar]
- 10.Yoshida N, Ikeda Y, Notomi S, Ishikawa K, Murakami Y, Hisatomi T, Enaida H, Ishibashi T. Clinical evidence of sustained chronic inflammatory reaction in retinitis pigmentosa. Ophthalmology. 2013;120:100–105. doi: 10.1016/j.ophtha.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 11.Scorolli L, Morara M, Meduri A, Reggiani LB, Ferreri G, Scalinci SZ, Meduri RA. Treatment of cystoid macular edema in retinitis pigmentosa with intravitreal triamcinolone. Arch Ophthalmol. 2007;125:759–764. doi: 10.1001/archopht.125.6.759. [DOI] [PubMed] [Google Scholar]
- 12.Haller J, Bandello F, Belfort R, Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jacques ML, Jiao J, Li XY, Whitcup SM, OZURDEX GENEVA Study Group Randomized sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010;117:1134–1146. doi: 10.1016/j.ophtha.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 13.Haller JA, Bandello F, Belfort R, Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jiao J, Li XY, Whitcup SM, Ozurdex GENEVA Study Group. Li J. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology. 2011;118:2453–2460. doi: 10.1016/j.ophtha.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 14.Srour M, Querques G, Leveziel N, Zerbib J, Tilleul J, Boulanger-Scemama E, Souied EH: Intravitreal dexamethasone implant (Ozurdex) for macular edema secondary to retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol 2012, E-pub ahead of print. [DOI] [PubMed]