Abstract
Context
Lower cognitive ability is a risk factor for some forms of psychopathology, but much of the evidence for risk is based on individuals who required specialist care. It is unclear whether lower ability influences the risk of particular patterns of comorbidity.
Objective
To examine the relation between premorbid cognitive ability in early adulthood and the risk of major depression, generalized anxiety disorder (GAD), posttraumatic stress disorder (PTSD), alcohol and other drug abuse or dependence, and comorbid forms of these conditions in midlife.
Design
Prospective cohort study in which cognitive ability was measured on enlistment into military service at a mean age of 20.4 years and psychiatric disorder was assessed by structured diagnostic interview at a mean age of 38.3 years.
Setting
The United States.
Participants
A total of 3258 male veterans, participants in the Vietnam Experience Study.
Main Outcome Measures
Major depression, GAD, PTSD, and alcohol or other drug abuse or dependence since enlistment and currently, diagnosed according to the DSM-III.
Results
Lower cognitive ability was associated with an increased risk of depression, GAD, alcohol abuse or dependence, and PTSD and with some patterns of comorbidity. For a 1-SD decrease in cognitive ability, unadjusted odds ratios (95% confidence interval) for having these disorders currently were 1.32 (1.12–1.56) for depression, 1.43 (1.27–1.64) for GAD, 1.20 (1.08–1.35) for alcohol abuse or dependence, 1.39 (1.18–1.67) for PTSD, 2.50 (1.41–4.55) for PTSD plus GAD, 2.17 (1.47–3.22) for PTSD plus GAD plus depression, and 2.77 (1.12–6.66) for all 4 disorders. Most associations remained statistically significant after adjustment for confounders.
Conclusions
Lower cognitive ability is a risk factor for several specific psychiatric disorders, including some forms of comorbidity. Understanding the mechanisms whereby ability is linked to individual patterns of psychopathology may inform intervention.
There is increasing evidence that children and adolescents with lower scores on standard tests of intelligence may be more vulnerable to psychopathology later in life. Lower cognitive ability in childhood or adolescence has been associated with an increased risk of developing schizophrenia,1–4 severe depression or other nonaffective psychoses,3 posttraumatic stress disorder (PTSD),5,6 generalized anxiety disorder (GAD),7 and alcohol or other drug abuse.8 Although these findings suggest that cognitive ability may be a risk factor for many forms of psychiatric disorder, much of the evidence is based on individuals whose disorders were severe enough to require admission to a hospital1–4,8,9 or treatment by secondary care mental health services.10 A few recent longitudinal studies of the relation between cognitive ability and subsequent psychiatric disorder have used structured diagnostic interviews to assess psychopathology across a wider spectrum of severity. Although these studies have produced consistent findings linking cognitive ability with the risk of PTSD,5,6 results on the relation between cognitive ability and anxiety disorders were inconsistent,7,11 and the only study to examine its link with depression found no association.11
None of these studies has examined whether cognitive ability is linked with susceptibility to particular patterns of psychiatric comorbidity. The co-occurrence of 2 or more psychiatric diagnoses—sometimes involving alcohol or other drug abuse or dependence—is common12 and has major consequences in terms of increased utilization of health care services,13,14 greater functional disability,15–17 and higher levels of distress.13 Learning whether particular combinations of disorders show stronger associations with cognitive ability earlier in life may help us better understand the nature of the link between cognitive ability and psychopathology.
The Vietnam Experience Study (VES) is a longitudinal study of male US Army veterans who had their cognitive ability assessed on enlistment in early adulthood and participated in a psychological examination in middle age, when psychiatric morbidity was assessed. We used these data to examine the relation between cognitive ability in early adulthood and the risks of major depression, GAD, PTSD, and alcohol or other drug abuse or dependence since enlistment and currently, and to investigate whether cognitive ability influenced the risk of comorbidity among these conditions.
METHODS
DATA COLLECTION IN LATE ADOLESCENCE/EARLY ADULTHOOD
The VES was conducted by the Centers for Disease Control and Prevention, Atlanta, Georgia. Participants were identified retrospectively using military records, as described elsewhere.18,19 In brief, 18 313 former military personnel were drawn randomly from approximately 5 million US Army veterans who had served in Vietnam and elsewhere and whose service files were stored at the National Personnel Records Center, St Louis, Missouri. Information on place of service, rank, ethnicity, and cognitive ability were extracted from military archives. Based on rank at army discharge (mean age at discharge, 22.5 years; range, 17.9–36.8 years), monthly income based on 1964 pay scales was derived. Ethnic origin was classified as white, black, or other; the latter group consisted of Hispanic, Asian, Pacific Islander, American Indian, and Alaskan native participants.
On enlistment, participants were administered the general technical section of the Army Classification Battery as a general aptitude test.20 This battery consists of 2 subtests: verbal and arithmetic reasoning. Scores on the general technical section correlate highly with scores on standard tests of intelligence.20 We were able to validate this test by comparing scores from it with those from 2 subtests of the Wechsler Adult Intelligence Scale, a comprehensive and widely used test of cognitive ability, that were administered to participants during the psychological examination in middle age. Despite this intervening period, total general technical scores were strongly correlated with scores on the information (r =0.74; 95% confidence interval [CI], 0.73–0.76) and block design subtests (0.51; 0.49–0.55) of the Wechsler Adult Intelligence Scale. Mean age at enlistment, when cognitive ability was assessed, was 20.4 (range, 17.0–33.8) years. For ease of interpretation, we converted total scores on the general technical section to an IQ equivalent (mean, 100; SD, 15).
DATA COLLECTION IN MIDDLE AGE
Of 18 313 former military personnel who qualified for inclusion in the original study cohort, 446 died after discharge. The remainder (n=17 867) were considered to be alive on December 31, 1983, and eligible for follow-up through interview and examination. In all, 15 288 men (85.6% of the target population) participated in a telephone survey in 1985 through 1986. A random sample of respondents (n=6443) were invited to attend a 3-day medical and psychological examination; 4462 attended (69.3% of those invited). Participants signed a consent form on the first day. Mean age at examination was 38.3 (range, 31.1–49.0) years, and mean time since enlistment was 17.4 (range, 13–22) years. Psychological health was assessed using the Diagnostic Interview Schedule (DIS).21 The DIS is a standardized questionnaire designed to assess the prevalence of psychiatric conditions according to the DSM-III22 criteria of the American Psychiatric Association. The DIS was administered by trained psychology technicians under the supervision of clinical psychologists. Participants reported the age at which they experienced symptoms, and the age at onset was determined from this information. Participants completed a 12-item combat exposure questionnaire that inquired about the frequency with which they had experienced various combat-related events.23
We used DIS data on the prevalence of major depression, GAD, PTSD, and alcohol or other drug abuse or dependence since enlistment or in the past 12 months (current). Participants were considered to have a diagnosis of a particular condition since enlistment if they reported ever having a pattern of symptoms that met the full DSM-III criteria and onset occurred after enlistment. In total, 1126 participants reported first experiencing symptoms at an age that predated enlistment (81.0% of these had alcohol abuse or dependence). Participants were considered to have a current diagnosis if they reported a pattern of symptoms in the past 12 months that met the full criteria. To allow the study of comorbidity, the optional DSM-III exclusion rules were not used. Participants were considered to have a pure form of a disorder if they did not meet the DIS criteria for any other condition within the same period (ie, this was their sole diagnosis). Participants were considered to have a comorbid condition if they met the criteria for 2 or more of the disorders under study.
By definition, individuals cannot be at risk for PTSD unless they have a history of exposure to a traumatic event. The version of the DIS used in the VES does not permit the identification of participants who were exposed to trauma but did not develop symptoms, only of those who developed symptoms. To use a trauma-exposed comparison group in our analyses of PTSD, we therefore restricted these analyses to a subgroup who had served in Vietnam and scored 1 or more on the combat exposure questionnaire, indicating that they had experienced combat. The DIS criteria for PTSD within the past year did not require trauma exposure to have occurred within this period, only symptoms.
ANALYTICAL SAMPLE
The present analyses are based on a sample of men with complete information on cognitive ability at enlistment, DIS data, and all the covariates available from their army records (age at enlistment, ethnicity, place of service, and army income). These covariates were included as potential confounders of the relation between cognitive ability and psychiatric disorder. After we excluded men with onset of a psychiatric disorder before enlistment, the sample consisted of 3258 men. This group represents 17.8% of the target population for the telephone interview and 51.0% of those invited for examination. We compared the distribution of baseline characteristics (age, army income, place of service, ethnicity, and IQ equivalent scores) between our analytical sample and those who participated in the telephone survey but were excluded from our sample because they did not participate in the examination. Men in the excluded group had a lower IQ equivalent score than did those in the analytical sample (mean [SD] score, 100.2 [14.9] vs 101.1 [15.2]; t = 3.25; P =.001; Cohen d =0.06); they were also more likely to be in the lowest category of army income (12.8% vs 10.8%; χ2=8.90; P =.01) and less likely to be black (11.1% vs 12.7%; χ2=6.32; P=.04). There were no differences between the groups in age at enlistment. Thus, these few differences were marginal, achieving statistical significance owing to the large numbers.
STATISTICAL ANALYSIS
We used analysis of variance, correlation coefficients, and the χ2 test to examine the characteristics of the participants. We used logistic regression to examine associations between these characteristics and the risk of psychiatric morbidity and to examine how the relation between cognitive ability and the risk of morbidity changed on adjustment for potential confounding factors.
RESULTS
COGNITIVE ABILITY IN RELATION TO DEMOGRAPHIC AND ARMY SERVICE CHARACTERISTICS
Table 1 shows cognitive ability scores at enlistment in relation to characteristics in early adulthood. Cognitive ability was greater in men with a higher socioeconomic position during service (as indicated by army income), in those who were white, whose place of service did not include Vietnam, and who were older at the time of enlistment.
Table 1.
Cognitive Ability Score at Enlistment in 3258 US Male Veterans According to Demographic and Army Service Characteristics
| Characteristic | No. (%) of Participantsa | Mean (SD) Cognitive Ability Score | Correlation With Cognitive Ability Scoreb |
|---|---|---|---|
| Age at enlistment, y | 0.23c | ||
| ≤18 | 408 (12.5) | 97.4 (12.9) | |
| 19–22 | 2522 (77.4) | 101.1 (15.1) | |
| ≥23 | 328 (10.1) | 106.2 (17.6)c | |
| Army income per week, US $ | 0.30c | ||
| 83–119 | 352 (10.8) | 93.2 (13.2) | |
| 120–144 | 1621 (49.8) | 98.7 (15.3) | |
| ≥145 | 1285 (39.4) | 106.3 (14.0)c | |
| Place of service | |||
| Ever in Vietnam | 1753 (53.8) | 100.0 (14.9) | |
| Other overseas | 1505 (46.2) | 101.5 (15.6) | |
| US only | 640 (19.6) | 103.6 (15.5)d | |
| Ethnic group | |||
| White | 2634 (80.8) | 103.8 (14.4) | |
| Black | 415 (12.7) | 88.1 (12.9) | |
| Other | 209 (6.4) | 93.7 (14.3)d | |
Percentages have been rounded and may not total 100.
Correlations are calculated for continuously distributed variables only.
P <.001 for trend.
P <.001 for difference.
COGNITIVE ABILITY AND RISK OF PSYCHIATRIC DISORDERS
Table 2 shows the unadjusted odds ratios for major depression, GAD, alcohol or other drug abuse or dependence, and PTSD since enlistment or currently, according to cognitive ability. Lower cognitive ability was associated with a significantly increased risk of major depression, GAD, and PTSD since enlistment and currently. Lower cognitive ability was also associated with an increased risk of alcohol abuse or dependence but, in contrast to the other disorders, it was slightly more strongly linked with the risk of ever having the condition since enlistment than with the risk of having it currently. Risk of other drug abuse or dependence since enlistment or currently was slightly higher in men of lower cognitive ability, but these relations were not statistically significant.
Table 2.
Unadjusted ORs for Psychiatric Disorders Since Enlistment or Currently According to Cognitive Ability
| Psychiatric Disorder | No (%) of Cases | OR (95% CI)a |
|---|---|---|
| All Participants (N=3258) | ||
| Major depression | ||
| Since enlistment | 242 (7.4) | 1.15 (1.01–1.30) |
| Currently | 145 (4.5) | 1.32 (1.12–1.56) |
| GAD | ||
| Since enlistment | 473 (14.5) | 1.20 (1.09–1.32) |
| Currently | 221 (6.8) | 1.43 (1.27–1.64) |
| Alcohol abuse or dependence | ||
| Since enlistment | 1035 (31.8) | 1.25 (1.16–1.35) |
| Currently | 308 (9.5) | 1.20 (1.08–1.35) |
| Drug abuse or dependence | ||
| Since enlistment | 318 (9.8) | 1.09 (0.97–1.22) |
| Currently | 80 (2.5) | 1.11 (0.90–1.39) |
|
| ||
| Combat-Exposed Vietnam Veterans (n=1659) | ||
| PTSD | ||
| Since enlistment | 161 (9.7) | 1.32 (1.12–1.56) |
| Currently | 131 (7.9) | 1.39 (1.18–1.67) |
Abbreviations: CI, confidence interval; GAD, generalized anxiety disorder; OR, odds ratio; PTSD, posttraumatic stress disorder.
Indicates per 1-SD decrease in cognitive ability, unadjusted.
Likelihood of all psychiatric disorders was increased in men with a lower income during their army service, in those who served in Vietnam, and in those who were younger at the time of enlistment. Men from nonwhite ethnic groups also tended to have a higher risk of all disorders (data not shown). We examined whether the relations between cognitive ability and the risk of psychiatric disorder were attenuated by adjustment for potential confounders. We did not adjust for age at enlistment in these analyses because, as Table 1 shows, there were large differences in cognitive ability between age groups that are likely to be caused by men with higher scores taking college deferments before entering the military. Adjustment for age could therefore result in an underestimation of the effect of cognitive ability.
Table 3 shows the adjusted odds ratios for major depression, GAD, PTSD, and alcohol abuse or dependence since enlistment or currently according to cognitive ability; the relation between cognitive ability and other drug abuse or dependence remained nonsignificant with adjustment for covariates and so was not considered further. Odds ratios for major depression, GAD, and alcohol abuse or dependence were adjusted separately and then together for ethnicity, army income, and place of service. Odds ratios for PTSD, based on a subgroup of combat-exposed Vietnam veterans, were adjusted for ethnicity and army income.
Table 3.
ORs for Psychiatric Disorders Since Enlistment or Currently According to Cognitive Ability, Adjusted Separately Then Together for Potential Confounders
| Psychiatric Disorder | Adjustments, OR (95% CI)a
|
||||
|---|---|---|---|---|---|
| Unadjusted | Ethnicity | Army Income | Place of Service | All | |
| All Participants (N=3258) | |||||
| Major depression | |||||
| Since enlistment | 1.15 (1.01–1.30) | 1.18 (1.02–1.35) | 1.12 (0.99–1.32) | 1.12 (0.99–1.29) | 1.11 (0.96–1.30) |
| Currently | 1.32 (1.12–1.56) | 1.32 (1.11–1.56) | 1.28 (1.09–1.52) | 1.30 (1.11–1.54) | 1.23 (1.03–1.47) |
| GAD | |||||
| Since enlistment | 1.20 (1.09–1.32) | 1.20 (1.09–1.33) | 1.16 (1.05–1.28) | 1.19 (1.08–1.30) | 1.16 (1.04–1.30) |
| Currently | 1.43 (1.27–1.64) | 1.44 (1.25–1.67) | 1.41 (1.23–1.64) | 1.41 (1.23–1.61) | 1.39 (1.19–1.61) |
| Alcohol abuse or dependence | |||||
| Since enlistment | 1.25 (1.16–1.35) | 1.27 (1.18–1.37) | 1.19 (1.10–1.28) | 1.23 (1.15–1.33) | 1.19 (1.10–1.30) |
| Currently | 1.20 (1.08–1.35) | 1.14 (1.01–1.28) | 1.12 (1.00–1.27) | 1.19 (1.06–1.35) | 1.04 (0.92–1.19) |
|
| |||||
| Combat-Exposed Vietnam Veterans (n=1659) | |||||
| PTSD | |||||
| Since enlistment | 1.32 (1.12–1.56) | 1.35 (1.15–1.61) | 1.28 (1.09–1.52) | … | 1.33 (1.11–1.58) |
| Currently | 1.39 (1.18–1.67) | 1.39 (1.14–1.67) | 1.33 (1.10–1.61) | … | 1.38 (1.14–1.66) |
Abbreviations: CI, confidence interval; GAD, generalized anxiety disorder; OR, odds ratio; PTSD, posttraumatic stress disorder; ellipses, not determined.
Indicates per 1-SD decrease in cognitive ability.
The relation between cognitive ability and the risk of major depression was slightly attenuated by adjustment for army income and place of service; adjustment for ethnicity had little effect (Table 3). After full adjustment, the relation between cognitive ability and the risk of depression since enlistment ceased to be statistically significant, but cognitive ability remained significantly associated with the risk of depression currently; the odds ratio for a 1-SD decrease in ability was 1.23 (95% CI, 1.03–1.47). The relation between cognitive ability and the risk of GAD was stronger than that between cognitive ability and the risk of depression. Adjustment for potential confounding factors had only slight attenuating effects, and, after full adjustment, lower cognitive ability continued to be associated with an increased risk of GAD since enlistment and currently; the odds ratios for a 1-SD decrease in ability were 1.16 (95% CI, 1.04–1.30) and 1.39 (95% CI, 1.19–1.61), respectively. The relation between cognitive ability and the risk of alcohol abuse or dependence was attenuated most strongly by adjustment for army income. After controlling for all potential confounding factors, cognitive ability ceased to be significantly associated with the risk of alcohol abuse or dependence currently but remained a significant predictor of alcohol abuse or dependence since enlistment; the odds ratio for a 1-SD decrease in cognitive ability was 1.19 (95% CI, 1.10–1.30). In the subgroup of participants exposed to combat during service in Vietnam, the strong association between lower cognitive ability and an increased risk of PTSD since enlistment or currently was only slightly weakened by adjustment for army income.
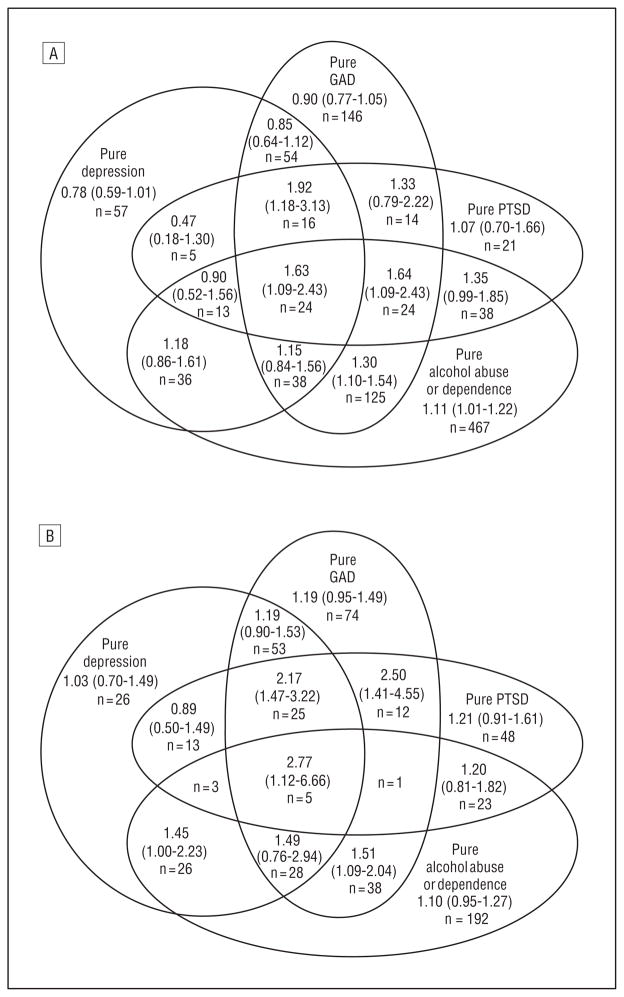
Of the 1377 men who had ever had major depression, GAD, PTSD, or alcohol abuse or dependence since enlistment, only 670 (48.7%) had a single disorder with no accompanying comorbidity. There was a similar pattern among the 543 men who had these disorders currently, of whom 296 (54.5%) had a single disorder. We examined whether the strength of the relation between cognitive ability and the risk of these disorders varied according to whether the condition was present in a pure or comorbid form (Figure and Table 4). As before, we restricted analyses of PTSD to a subgroup of combat-exposed Vietnam veterans.
Figure.
Venn diagram shows the unadjusted odds ratios and 95% confidence intervals for pure and comorbid forms of psychiatric disorder since enlistment (A) and currently (B) for a 1-SD decrease in cognitive ability. All analyses are based on our study sample (N=3258), except for pure and comorbid forms of posttraumatic stress disorder (PTSD), which are based on combat-exposed Vietnam veterans (n=1659). GAD indicates generalized anxiety disorder. We did not calculate odds ratios for forms of comorbidity with fewer than 5 cases.
Table 4.
ORs for Having a Pure or a Comorbid Form of Psychiatric Disorder Since Enlistment or Currently According to Cognitive Ability
| Psychiatric Disorder | No (%)of Cases | OR (95% CI)a
|
|
|---|---|---|---|
| Unadjusted | Adjustedb | ||
| All Participants (N=3258) | |||
| Pure alcohol abuse or dependence | |||
| Since enlistment | 467 (14.3) | 1.11 (1.01–1.22) | 1.14 (1.02–1.27) |
| Currently | 192 (5.9) | 1.10 (0.95–1.27) | 1.03 (0.88–1.20) |
| Pure GAD | |||
| Since enlistment | 146 (4.5) | 0.90 (0.77–1.05) | 0.98 (0.83–1.20) |
| Currently | 74 (2.3) | 1.19 (0.95–1.49) | 1.23 (0.97–1.59) |
| Pure depression | |||
| Since enlistment | 57 (1.7) | 0.78 (0.59–1.02) | 0.89 (0.66–1.19) |
| Currently | 26 (0.8) | 1.03 (0.70–1.49) | 1.20 (0.79–1.85) |
| Depression + GAD | |||
| Since enlistment | 49 (1.5) | 0.85 (0.64–1.12) | 0.83 (0.61–1.14) |
| Currently | 53 (1.6) | 1.19 (0.90–1.53) | 1.08 (0.81–1.45) |
| Depression + alcohol abuse or dependence | |||
| Since enlistment | 36 (1.1) | 1.18 (0.86–1.61) | 1.02 (0.72–1.45) |
| Currently | 26 (0.8) | 1.45 (1.00–2.23) | 1.32 (0.86–2.00) |
| GAD + alcohol abuse or dependence | |||
| Since enlistment | 125 (3.8) | 1.30 (1.10–1.54) | 1.14 (0.94–1.39) |
| Currently | 38 (1.2) | 1.51 (1.09–2.04) | 1.27 (0.89–1.79) |
| GAD + alcohol abuse or dependence + depression | |||
| Since enlistment | 38 (1.2) | 1.15 (0.84–1.56) | 1.02 (0.74–1.45) |
| Currently | 28 (0.9) | 1.49 (0.76–2.94) | 1.23 (0.58–2.63) |
|
| |||
| Combat-Exposed Vietnam Veterans (n=1659) | |||
| Pure PTSD | |||
| Since enlistment | 21 (1.3) | 1.07 (0.70–1.66) | 1.04 (0.65–1.66) |
| Currently | 48 (2.9) | 1.21 (0.91–1.61) | 1.39 (1.03–1.89) |
| PTSD + GAD | |||
| Since enlistment | 14 (0.8) | 1.33 (0.79–1.22) | 1.46 (0.84–2.57) |
| Currently | 12 (0.7) | 2.50 (1.41–4.55) | 2.49 (1.35–4.56) |
| PTSD + alcohol abuse or dependence | |||
| Since enlistment | 38 (2.3) | 1.35 (0.99–1.85) | 1.51 (1.08–2.10) |
| Currently | 23 (1.4) | 1.20 (0.81–1.82) | 1.07 (0.68–1.67) |
| PTSD + GAD + depression | |||
| Since enlistment | 16 (1.0) | 1.92 (1.18–3.13) | 1.50 (0.87–2.58) |
| Currently | 25 (1.5) | 2.17 (1.47–3.22) | 2.02 (1.32–3.10) |
| PTSD + GAD + alcohol abuse or dependence | |||
| Since enlistment | 24 (1.4) | 1.64 (1.09–2.43) | 1.43 (0.92–2.21) |
| Currently | 1 (0.06) | … | … |
| PTSD + depression + alcohol abuse or dependence | |||
| Since enlistment | 13 (0.01) | 0.90 (0.52–1.56) | 0.85 (0.46–1.53) |
| Currently | 3 (0.2) | … | … |
| PTSD + GAD + depression + alcohol abuse or dependence | |||
| Since enlistment | 24 (1.4) | 1.63 (1.09–2.43) | 1.65 (1.08–2.52) |
| Currently | 5 (0.3) | 2.77 (1.12–6.66) | 2.89 (1.15–7.26) |
Abbreviations: CI, confidence interval; GAD, generalized anxiety disorder; OR, odds ratio; PTSD, posttraumatic stress disorder; ellipses, not determined.
Indicates per 1-SD decrease in cognitive ability.
For all participants, adjustments are for ethnicity, army income, and place of service; for combat-exposed Vietnam veterans, adjustments are for ethnicity and army income.
RISK OF HAVING A PURE DISORDER
Cognitive ability was not associated with the risk of having pure depression or pure GAD since enlistment or currently (Figure and Table 4). The risk of having PTSD in a pure form was raised in men with lower cognitive ability. Numbers with this condition were small and the relations were not statistically significant in unadjusted analyses, although adjustment for potential confounders strengthened the association with current disorder. Far larger numbers of men had pure alcohol abuse or dependence. As in the case of an overall diagnosis of alcohol abuse or disorder (Table 3), lower cognitive ability was associated with a significantly increased risk of having alcohol abuse or dependence in a pure form since enlistment. This relation was slightly strengthened when potentially confounding factors were added to the multivariate model. The association between cognitive ability and the risk of having this form of the disorder currently was weaker and not statistically significant.
RISK OF HAVING A COMORBID DISORDER
Numbers of cases with comorbidity involving depression, GAD, alcohol abuse or dependence, or PTSD were often very small; thus, odds ratios based on these need to be interpreted with caution. In general, men with lower cognitive ability appeared to have a higher risk of co-morbid as opposed to single disorders, particularly those involving GAD and PTSD, although only a few of these associations were statistically significant. Associations between lower cognitive ability and an increased risk of alcohol abuse or dependence in combination with GAD or depression were weakened by adjustment for potential confounding factors and ceased to be significant. Associations between lower cognitive ability and the heightened risk of some forms of comorbid PTSD tended to be little attenuated or slightly strengthened by adjustment, albeit based on very small numbers of cases. For a 1-SD decrease in cognitive ability, after adjustment, odds ratios for disorders since enlistment were 1.51 (95% CI, 1.08–2.10) for PTSD plus alcohol abuse or dependence and 1.65 (1.08–2.52) for PTSD plus alcohol abuse plus depression plus GAD. Conversely, odds ratios for current disorders were 2.49 (95% CI, 1.35–4.56) for PTSD plus GAD, 2.02 (1.32–3.10) for PTSD plus GAD plus depression, and 2.89 (1.15–7.26) for PTSD plus GAD plus alcohol abuse or dependence plus depression.
COMMENT
In this study of former US soldiers followed up in middle age, men who had lower cognitive ability in early adulthood had an increased risk of major depression, GAD, alcohol abuse or dependence, PTSD, and some comorbid forms of PTSD.
PREVIOUS STUDIES
Higher premorbid cognitive ability has been associated with a lower risk of PTSD in previous studies. In a New Zealand cohort,5 men and women who had a higher IQ at 5 years of age had a reduced risk of developing PTSD by 32 years of age. Similar findings have been reported from a small US cohort,24 in which higher IQ at 6 years of age was linked to a lower likelihood of being exposed to trauma and a reduced risk of developing PTSD by 17 years of age. Studies of military samples have also implicated cognitive ability as a risk factor for this condition. In a small prospective study of US veterans, men with a higher IQ on enlistment were less likely to develop PTSD, although interpretation of this finding is difficult because there was no adjustment for prior socioeconomic status.25 A recent co-twin control study of 2386 Vietnam-era veterans found a significant dose-response relation between a higher IQ at induction into the military and lower risk of PTSD in both between-twin and within-pair analyses.6 In our study, higher cognitive ability was associated with a reduced risk of PTSD in combat-exposed Vietnam veterans.
None of these studies of PTSD examined the potential influence of premorbid cognitive ability on the psychiatric comorbidity that frequently accompanies the condition. Our results on this need to be treated with caution because the number of cases was small, but they suggest that lower cognitive ability may be a risk factor for co-morbid forms of PTSD, perhaps in particular those involving GAD and alcohol abuse or dependence. Lower intelligence has previously been associated with hospitalization for psychiatric disorder.1–4,8,9 Our findings on comorbidity provide further indications of a link between lower cognitive ability and severity of psychiatric disorder.
Existing evidence on the relation between IQ and the subsequent risk of GAD is sparse. In a small follow-up study of members of the National Collaborative Perinatal Project when they were in the middle of their fourth decade of life,7 a 1-SD increase in IQ at 7 years of age was associated with a 50% reduction in lifetime risk of GAD. The unadjusted odds ratio for GAD with onset in adulthood was 0.81 (95% CI, 0.52–1.27) per 1-SD increase in IQ. This is similar in magnitude to the association found in the present study, in which the equivalent odds ratio for onset of GAD since enlistment was 0.83 (95% CI, 0.76–0.92) per 1-SD increase in cognitive ability. Higher childhood IQ was linked with a lower risk of anxiety disorders overall (GAD, phobias, and panic disorder) in adolescence or early adulthood in the Christchurch Health and Development Study,11 but the relation was severely attenuated and no longer significant after adjustment for potential confounding factors. The present study was based on larger numbers than either of these investigations. That factor together with the older age of our study sample may in part explain why we found a more robust association between IQ and GAD than these earlier studies. The prevalence of GAD increases substantially with age.26
Few previous studies have examined the link between cognitive ability and depression, and the findings have been inconsistent. In a study of hospital admissions during a 27-year period, the risk of severe depression was significantly higher in men with a lower IQ in late adolescence.3 Lower IQ in childhood was associated with greater depression and anxiety at 53 years of age, as measured by the General Health Questionnaire, although only in women.27 However, in a follow-up study of another cohort in which depression was assessed by structured diagnostic interview,11 there was no evidence to link IQ in childhood with the risk of depression by 25 years of age. In the present study, men with lower cognitive ability in late adolescence experienced a significantly increased risk of developing depression. We found no link between cognitive ability and depression when it co-occurred with GAD. The reasons for this are unclear. This pattern of comorbidity occurs frequently, and individuals with pure GAD or GAD plus major depression tend to show a similar risk history.28
Only 1 previous study has examined the link between IQ and drug abuse. In a longitudinal study of a Danish male cohort, those with higher cognitive ability at 12 years of age had a reduced risk of alcohol or other drug abuse, as measured by diagnosis on hospital admission or by mention on death certificates, during a 30-year follow-up.8 In the present study, we found no significant association between IQ and the risk of other drug abuse or dependence. It is likely that the relatively few cases of other drug abuse found among the men who participated in the psychological examination were at the milder end of the spectrum compared with the cases observed in the Danish cohort whose disorder was severe enough to have caused their hospitalization or death.
Higher IQ in childhood was also associated with a reduced risk of alcohol abuse or dependence in this Danish cohort.8 This is consistent with findings linking higher IQ with healthier behaviors in terms of smoking,29,30 diet, and exercise.31 In the present study, we found that men with higher cognitive ability were at significantly lower risk of alcohol abuse or dependence at any time after enlistment, although the relation between cognitive ability and the risk of alcoholism in the year before the mid-life examination was weaker and attenuated by adjustment, particularly for army income.
Recent findings from 2 UK national birth cohorts found a very different association between IQ and the risk of alcohol abuse from that found herein. In follow-up examinations of the 1970 British Cohort Study32 and the 1946 National Survey of Health and Development,27 performed when the participants were 30 and 53 years of age, respectively, higher IQ in childhood was associated with an increased risk of scoring positively for alcohol problems on the CAGE inventory (an acronym for cut down on drinking, annoyed by people criticizing, guilty about drinking, and eye-opener or drink first thing in the morning). The CAGE inventory has been validated against the DIS and found to be an effective screening instrument.33 The reasons for the discrepancy among these findings, the results of the present study, and those of the Danish study8 are unclear, but one explanation might be that data on the UK cohorts were collected at a time and in a society where more frequent drinking tended to be associated with higher income and greater educational attainment.34
PLAUSIBLE MECHANISMS
The mechanisms that underlie the link between cognitive ability and the risk of psychopathology are still unclear. One possible explanation is that lower cognitive ability acts as a marker of impaired neurodevelopment that itself affects the development of psychiatric disorder.3,9 The suggestion in our findings that lower cognitive ability may be more strongly linked to the risk of having comorbid rather than pure disorders could indicate that individuals with such conditions have more vulnerable brains. This vulnerability might be genetically mediated. In a study of premorbid cognitive ability and the risk of PTSD in twins,6 the variance in PTSD explained by cognitive ability was accounted for entirely by common genetic factors. There is evidence that several of the disorders studied herein share some genetic influences.35,36 Twin studies suggest that common genetic liability explains a large part of the comorbidity between major depression and PTSD37 and between major depression and GAD,38,39 although shared environmental factors largely accounted for the association between PTSD and conduct disorder,40 perhaps owing to an adverse family environment in childhood. Another explanation for the link between lower cognitive ability and psychiatric disorder might be that people with a lower IQ have a reduced perception of control over their lives. Having an internal locus of control or a stronger sense of self-efficacy decreases the risk of anxiety and depression41 and of PTSD.42 Evidence in children suggests that an internal locus of control is more common in individuals with a higher IQ.43 A further potential mechanism might be that individuals with a higher IQ are less likely to experience socioeconomic disadvantage in adult life. Socioeconomic disadvantage is linked with a high risk of experiencing depression or anxiety.44,45 Although we controlled for army income as a potential confounding factor, this might be an overadjustment because intelligence could have influenced the rank they attained and thereby their risk of psychiatric disorder. It is also possible that individuals with greater cognitive resources are better able to interpret stressful or potentially traumatic stimuli or events in a way that nullifies or reduces their effect on mental equilibrium and prevents them from developing PTSD.
STRENGTHS AND LIMITATIONS
The strengths of this study are its size and the availability of data on factors that might potentially confound the relations between cognitive ability and psychiatric disorder. The study also has some limitations. First, there has been some criticism of the psychiatric diagnoses in the VES, particularly of PTSD, because the prevalence of this disorder was markedly lower than those found in the National Vietnam Veterans Readjustment Study46,47 and in other surveys conducted at the same time.48 That some cases of psychiatric disorder in the VES participants may have been unidentified could result in an underestimation of the true strength of the relation between cognitive ability and the later risk of psychiatric disorder, particularly PTSD. Second, we examined the risk of GAD only. It is possible that our results might have been different had we examined other forms of anxiety disorders. Third, selection into military service is likely to have excluded men with severe early-onset psychopathology, so the cases of psychiatric disorder in our sample may predominantly include those with mild or moderate disease. This reduced variance may also have resulted in an underestimation of the true effect of cognitive ability on later risk. Fourth, the diagnosis of PTSD did not permit us to identify men who had experienced traumatic events but had no symptoms. To restrict our analyses of PTSD to men who had been exposed to trauma, we had to use a subgroup of combat-exposed Vietnam veterans. Some men who had a diagnosis of PTSD after non–combat-related trauma were excluded, although numbers of such cases were low (n=34 for disorder since enlistment). Fifth, retrospective self-report of first age at onset of symptoms may be subject to error, resulting in misclassification of timing of disease onset. Such reports are widely used in large-scale psychiatric surveys and have shown good reliability and validity for the short term,49 but to collect lifetime prevalence data respondents have to recall the presence and co-occurrence of symptoms, possibly many years after their first occurrence. Problems with recall can cause underestimation of lifetime prevalence.50 This may explain why cognitive ability and all risk factors tended—with the exception of alcohol abuse or dependence—to be more strongly associated with current disorder than with disorder since enlistment. Finally, although we excluded men with prior psychiatric disorder, some men’s cognitive performance may have been influenced by the presence of disease.
The results of this study suggest that lower cognitive ability is a risk factor for several forms of psychopathology, including, perhaps, some patterns of comorbidity. Distinct mechanisms may underlie some of these associations, particularly those in which the disorder has a strong behavioral component, such as alcohol abuse or dependence. Understanding the mechanisms whereby cognitive ability is linked to individual patterns of psychopathology may help inform intervention.
Acknowledgments
Funding/Support: This study was supported by core funding from the Medical Research Council (Dr Gale); the University of Edinburgh and the Medical Research Council (Dr Deary); the National Institute of Public Health, Denmark (Mr Mortensen); the National Heart, Lung, and Blood Institute and grant RO1-HL54780 from the National Institute on Aging at the National Institutes of Health (Drs Barefoot and Boyle); and UK Wellcome Trust Fellowship WBS U.1300.00.006.00012.01 (Dr Batty).
Footnotes
Author Contributions: Dr Gale performed the statistical analysis, had full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial Disclosure: None reported.
References
- 1.David AS, Malmberg A, Brandt L, Allebeck P, Lewis G. IQ and risk for schizophrenia: a population-based cohort study. Psychol Med. 1997;27(6):1311–1323. doi: 10.1017/s0033291797005680. [DOI] [PubMed] [Google Scholar]
- 2.Gunnell D, Harrison G, Rasmussen F, Fouskakis D, Tynelius P. Associations between premorbid intellectual performance, early-life exposures and early-onset schizophrenia: cohort study. Br J Psychiatry. 2002;181:298–305. doi: 10.1192/bjp.181.4.298. [DOI] [PubMed] [Google Scholar]
- 3.Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I, Lewis G. A longitudinal study of premorbid IQ Score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch Gen Psychiatry. 2004;61(4):354–360. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]
- 4.Osler M, Lawlor DA, Nordentoft M. Cognitive function in childhood and early adulthood and hospital admission for schizophrenia and bipolar disorders in Danish men born in 1953. Schizophr Res. 2007;92(1–3):132–141. doi: 10.1016/j.schres.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Koenen KC, Moffitt TE, Poulton R, Martin J, Caspi A. Early childhood factors associated with the development of post-traumatic stress disorder: results from a longitudinal birth cohort. Psychol Med. 2007;37(2):181–192. doi: 10.1017/S0033291706009019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kremen WS, Koenen KC, Boake C, Purcell S, Eisen SA, Franz CE, Tsuang MT, Lyons MJ. Pretrauma cognitive ability and risk for posttraumatic stress disorder: a twin study. Arch Gen Psychiatry. 2007;64(3):361–368. doi: 10.1001/archpsyc.64.3.361. [DOI] [PubMed] [Google Scholar]
- 7.Martin LT, Kubzansky LD, Lewinn KZ, Lipsitt LP, Satz P, Buka SL. Childhood cognitive performance and risk of generalized anxiety disorder. Int J Epidemiol. 2007;36(4):769–775. doi: 10.1093/ije/dym063. [DOI] [PubMed] [Google Scholar]
- 8.Osler M, Nordentoft M, Andersen AM. Childhood social environment and risk of drug and alcohol abuse in a cohort of Danish men born in 1953. Am J Epidemiol. 2006;163(7):654–661. doi: 10.1093/aje/kwj084. [DOI] [PubMed] [Google Scholar]
- 9.Batty GD, Mortensen EL, Osler M. Childhood IQ in relation to later psychiatric disorder: evidence from a Danish birth cohort study. Br J Psychiatry. 2005;187:180–181. doi: 10.1192/bjp.187.2.180. [DOI] [PubMed] [Google Scholar]
- 10.Walker NP, McConville PM, Hunter D, Deary IJ, Whalley LJ. Childhood mental ability and lifetime psychiatric contact: a 66-year follow-up study of the 1932 Scottish Mental Ability Survey. Intelligence. 2002;30(3):233–245. [Google Scholar]
- 11.Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven, II: childhood intelligence and later outcomes in adolescence and young adulthood. J Child Psychol Psychiatry. 2005;46(8):850–858. doi: 10.1111/j.1469-7610.2005.01472.x. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 13.Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: data from the Australian National Survey of Mental Health and Well-being. Br J Psychiatry. 2002;181:306–314. doi: 10.1192/bjp.181.4.306. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC. Epidemiology of psychiatric comorbidity. In: Tsuang M, Tohen M, Zahner G, editors. Textbook in Psychiatric Epidemiology. New York, NY: Wiley-Liss; 1995. pp. 179–198. [Google Scholar]
- 15.Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety disorder: cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Arch Gen Psychiatry. 2007;64(6):651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- 16.Wittchen HU, Kessler RC, Pfister H, Lieb M. Why do people with anxiety disorders become depressed? a prospective-longitudinal community study. Acta Psychiatr Scand Suppl. 2000;406:14–23. [PubMed] [Google Scholar]
- 17.Bijl RV, Ravelli A. Current and residual functional disability associated with psychopathology: findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Psychol Med. 2000;30(3):657–668. doi: 10.1017/s0033291799001841. [DOI] [PubMed] [Google Scholar]
- 18.Boehmer TK, Flanders WD, McGeehin MA, Boyle C, Barrett DH. Postservice mortality in Vietnam veterans: 30-year follow-up. Arch Intern Med. 2004;164(17):1908–1916. doi: 10.1001/archinte.164.17.1908. [DOI] [PubMed] [Google Scholar]
- 19.Health status of Vietnam veterans, I: psychosocial characteristics: Centers for Disease Control Vietnam Experience Study. JAMA. 1988;259(18):2701–2707. [PubMed] [Google Scholar]
- 20.Montague EK, Williams HL, Lubin A, Gieseking CF. Army tests for assessment of intellectual deficit. U S Armed Forces Med J. 1957;8(6):883–892. [PubMed] [Google Scholar]
- 21.Robins LN, Helzer JE, Cottler LB, Works J, Goldring E, McEvoy L. The Diagnostic Interview Schedule, Version III-A: Training Manual. St Louis, MO: Veterans Administration; 1987. [Google Scholar]
- 22.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 23.Egendorf A, Kadushin C, Laufer RS. Legacies of Vietnam: Comparative Adjustment of Veterans and Their Peers. Washington, DC: Center for Policy Research Inc; 1981. Publication V101. [Google Scholar]
- 24.Breslau N, Lucia VC, Alvarado GF. Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder: a follow-up study at age 17 years. Arch Gen Psychiatry. 2006;63(11):1238–1245. doi: 10.1001/archpsyc.63.11.1238. [DOI] [PubMed] [Google Scholar]
- 25.Macklin ML, Metzger LJ, Litz BT, McNally RJ, Lasko NB, Orr SP, Pitman RK. Lower precombat intelligence is a risk factor for posttraumatic stress disorder. J Consult Clin Psychol. 1998;66(2):323–326. doi: 10.1037//0022-006x.66.2.323. [DOI] [PubMed] [Google Scholar]
- 26.Wittchen HU, Hoyer J. Generalized anxiety disorder: nature and course. J Clin Psychiatry. 2001;62(suppl 11):15–19. [PubMed] [Google Scholar]
- 27.Hatch SL, Jones PB, Kuh D, Hardy R, Wadsworth ME, Richards M. Childhood cognitive ability and adult mental health in the British 1946 birth cohort. Soc Sci Med. 2007;64(11):2285–2296. doi: 10.1016/j.socscimed.2007.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moffitt TE, Caspi A, Harrington H. Generalized anxiety disorder and depression: childhood risk factors in a birth cohort followed to age 32. Psychol Med. 2007;37(3):441–452. doi: 10.1017/S0033291706009640. [DOI] [PubMed] [Google Scholar]
- 29.Taylor MD, Hart CL, Davey Smith G, Starr JM, Hole DJ, Whalley LJ, Wilson V, Deary IJ. Childhood mental ability and smoking cessation in adulthood: prospective observational study linking the Scottish Mental Survey 1932 and the Mid-span studies. J Epidemiol Community Health. 2003;57(6):464–465. doi: 10.1136/jech.57.6.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Batty GD, Deary IJ, Schoon I, Gale CR. Mental ability across childhood and risk factors for premature mortality in adult life: the 1970 British Cohort Study. J Epidemiol Community Health. 2007;61(11):997–1003. doi: 10.1136/jech.2006.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Batty GD, Deary IJ, Schoon I, Gale CR. Childhood mental ability in relation to food intake and physical activity in adulthood: the 1970 British Cohort Study. Pediatrics. 2007;119(1):e38–e45. doi: 10.1542/peds.2006–1831. [DOI] [PubMed] [Google Scholar]
- 32.Batty GD, Deary IJ, Schoon I, Emslie C, Hunt K, Gale CR. Childhood mental ability in relation to alcohol drinking problems and consumption in adulthood: the 1970 British Cohort Study [published online January 30, 2008] Am J Public Health. doi: 10.2105/AJPH.2007.109488. [DOI] [Google Scholar]
- 33.Liskow B, Campbell J, Nickel EJ, Powell BJ. Validity of the CAGE questionnaire in screening for alcohol dependence in a walk-in (triage) clinic. J Stud Alcohol. 1995;56(3):277–281. doi: 10.15288/jsa.1995.56.277. [DOI] [PubMed] [Google Scholar]
- 34.ONS SSD. Living in Britain: Results from the 2001 General Household Survey. London, England: Stationery Office; 2002. [Google Scholar]
- 35.Chantarujikapong SI, Scherrer JF, Xian H, Eisen SA, Lyons MJ, Goldberg J, Tsuang M, True WR. A twin study of generalized anxiety disorder symptoms, panic disorder symptoms and post-traumatic stress disorder in men. Psychiatry Res. 2001;103(2–3):133–145. doi: 10.1016/s0165-1781(01)00285-2. [DOI] [PubMed] [Google Scholar]
- 36.Xian H, Chantarujikapong SI, Scherrer JF, Eisen SA, Lyons MJ, Goldberg J, Tsuang M, True WR. Genetic and environmental influences on posttraumatic stress disorder, alcohol and drug dependence in twin pairs. Drug Alcohol Depend. 2000;61(1):95–102. doi: 10.1016/s0376-8716(00)00127-7. [DOI] [PubMed] [Google Scholar]
- 37.Koenen KC, Fu QJ, Ertel K, Lyons MJ, Eisen SA, True WR, Goldberg J, Tsuang MT. Common genetic liability to major depression and posttraumatic stress disorder in men. J Affect Disord. 2008;105(1–3):109–115. doi: 10.1016/j.jad.2007.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. Am J Psychiatry. 2006;163(5):857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- 39.Middeldorp CM, Cath DC, Van DR, Boomsma DI. The co-morbidity of anxiety and depression in the perspective of genetic epidemiology: a review of twin and family studies. Psychol Med. 2005;35(5):611–624. doi: 10.1017/s003329170400412x. [DOI] [PubMed] [Google Scholar]
- 40.Fu Q, Koenen KC, Miller MW, Heath AC, Bucholz KK, Lyons MJ, Eisen SA, True WR, Goldberg J, Tsuang MT. Differential etiology of posttraumatic stress disorder with conduct disorder and major depression in male veterans. Biol Psychiatry. 2007;62(10):1088–1094. doi: 10.1016/j.biopsych.2007.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Molinari V, Khanna P. Locus of control and its relationship to anxiety and depression. J Pers Assess. 1981;45(3):314–319. doi: 10.1207/s15327752jpa4503_14. [DOI] [PubMed] [Google Scholar]
- 42.Heinrichs M, Wagner D, Schoch W, Soravia LM, Hellhammer DH, Ehlert U. Predicting posttraumatic stress symptoms from pretraumatic risk factors: a 2-year prospective follow-up study in firefighters. Am J Psychiatry. 2005;162(12):2276–2286. doi: 10.1176/appi.ajp.162.12.2276. [DOI] [PubMed] [Google Scholar]
- 43.Gale CR, Batty GD, Deary IJ. Locus of control at age 10 years and health outcomes and behaviors at age 30 years: the 1970 British Cohort Study. Psychosom Med. 2008;70(4):397–403. doi: 10.1097/PSY.0b013e31816a719e. [DOI] [PubMed] [Google Scholar]
- 44.Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157 (2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- 45.Muntaner C, Eaton WW, Miech R, O’Campo P. Socioeconomic position and major mental disorders. Epidemiol Rev. 2004;26:53–62. doi: 10.1093/epirev/mxh001. [DOI] [PubMed] [Google Scholar]
- 46.Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. Continuing controversy over the psychological risks of Vietnam for US veterans. J Trauma Stress. 2007;20(4):449–465. doi: 10.1002/jts.20296. [DOI] [PubMed] [Google Scholar]
- 47.Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for US veterans: a revisit with new data and methods. Science. 2006;313(5789):979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Snow BR, Stellman JM, Stellman SD, Sommer JF., Jr Post-traumatic stress disorder among American Legionnaires in relation to combat experience in Vietnam: associated and contributing factors. Environ Res. 1988;47(2):175–192. doi: 10.1016/s0013-9351(88)80040-9. [DOI] [PubMed] [Google Scholar]
- 49.Wittchen HU, Burke JD, Semler G, Pfister H, Von CM, Zaudig M. Recall and dating of psychiatric symptoms: test-retest reliability of time-related symptom questions in a standardized psychiatric interview. Arch Gen Psychiatry. 1989;46 (5):437–443. doi: 10.1001/archpsyc.1989.01810050051009. [DOI] [PubMed] [Google Scholar]
- 50.Andrews G, Anstey K, Brodaty H, Issakidis C, Luscombe G. Recall of depressive episode 25 years previously. Psychol Med. 1999;29(4):787–791. doi: 10.1017/s0033291799008648. [DOI] [PubMed] [Google Scholar]