Abstract
This research aimed to study the effect of premarital sex on sexually transmitted infections (STIs) and high risk behaviors among women in sub-Saharan Africa. It included 1393 women randomly selected from the Moshi urban district of northern Tanzania. Participants’ demographic and socio-demographic characteristics, alcohol use, condom use, number of partners, symptoms of STIs and age at first sex and marriage were obtained. Moreover, blood and urine samples were tested for HIV-1, HSV-2, syphilis, chlamydia, gonorrhea, trichomonas and Mycoplasma genitalium infections. The average duration of premarital sex in the study participants was 1.66 years (SD of 2.61 years). Women with longer duration of premarital sex had higher odds of HIV-1, HSV-2 and other STIs. Moreover, women with longer duration of premarital sex were more likely to report multiple sexual partners. These findings highlight the importance of a lengthy period of premarital sex as a public health issue. STIs prevention programs in sub-Saharan Africa should address factors leading to a longer period of premarital sex in women
Keywords: Premarital sex, High-risk behaviors, HIV-1, HSV-2, Sexually transmitted infections
Introduction
Sub-Saharan Africa has been more devastated by HIV/AIDS than any other region in the world. An estimated 22.9 million people infected with HIV, i.e., around two thirds of the global total, live in sub-Saharan Africa (UNAIDS, 2011). Around 1.2 million deaths from AIDS occurred in sub-Saharan Africa (UNAIDS, 2011). Less than a third of people living with HIV in sub-Saharan Africa have access to antiretroviral therapy (UNAIDS, 2010). In the absence of an effective vaccine and universal access to antiretroviral therapy, recognition and comprehensive control of risk behaviors that are associated with HIV transmission remains the most promising strategy to curb and reverse the spread of the epidemic in the sub-region.
The age at first sex is an important risk factor for the acquisition of HIV. Individuals who start their sexual activity at a young age are more likely to report higher rates of STIs, drug and alcohol abuse, multiple sexual partners and to engage in unprotected sex (Dickson et al., 1998; Duncan et al., 1990; Greenberg et al., 1992; Manning et al., 2000). Several studies from sub-Saharan Africa reported a negative association between delaying sexual debut and HIV prevalence (Gregson et al., 2006; Stoneburner and Low-Beer, 2004). Age at marriage could also be another risk factor for HIV acquisition in the region. However, the relationship between age at marriage and the risk of HIV infection is not clear. Some studies suggested that late marriage is a risk factor for HIV infection (Bongaarts, 2007; Glynn et al., 2003). Bongaarts (2007) reported that late marriage after sexual initiation leads to a long period of premarital intercourse with multiple partners and facilitates the risk of acquiring HIV. However, other studies failed to report a positive association between late marriage and HIV acquisition and indicated that early marriage elevates the risk of HIV infection (Bruce and Clark, 2003; Clark, 2004). Marriage occurs at a young age for many women in sub-Saharan Africa (i.e., first sex occurs at marriage for many sub-Saharan African women). However, the young women are often married to considerably sexually experienced older men, who are likely to have had more sexual partners; thus women are at increased risk of HIV acquisition. A study in Uganda reported that the risk of HIV infection in young married women whose husbands were 10 or more years older were doubled compared to young married women whose husbands were only up to four years older (Kelly et al., 2003). Further knowledge about the association between age at first marriage and acquisition of HIV-1 might have important public health implications for the prevention of HIV and other STIs in sub-Saharan Africa.
The present study examines the association between duration of premarital sex and the risk of acquiring STIs, including HIV-1 and HSV-2, among women in sub-Saharan Africa. We hypothesized that a longer gap between first sex and marriage is associated with higher risk of STIs. To test this hypothesis, we analyzed data from a community-based survey in the Moshi urban district of Tanzania. Moshi is the capital of the Kilimanjaro region of northern Tanzania. The Kilimanjaro region, located in northern Tanzania adjacent to the Kenyan border, is one of Tanzania’s 20 regions. According to the 2002 Tanzania National Census, the population of the Moshi urban district was 144, 336 (National Bureau of Statistics (NBS), 2002). Tanzania has a population of 34.5 million people, with approximately 7% of adults infected with HIV (Tanzania Commission for AIDS (TACAIDS), National Bureau of Statistics (NBS), and ORC Macro, 2005). In the Moshi district of northern Tanzania the prevalence of HIV infection is about twice that of the national average.
Methods
Study Participants
The data set used in this paper comes from a cross-sectional survey conducted from November 2002 to March 2003 in the Moshi urban district of Tanzania. The rationale, organization, and recruitment of the survey have been described in detail elsewhere (Larsen et al., 2007). In brief, the survey involved a two-stage sampling procedure. In the first stage of sampling, a total of 150 clusters were selected using probability proportional to the number of women aged 20–24 living in the study area. In the second stage of sampling, 18 households were randomly selected from each cluster. A total of 2,019 women aged 20–44, who were residents of the selected households, were interviewed. Information was collected on fertility, marriage, sexual practices, symptoms of STIs, socio-demographic characteristics, and husband-wife relations including domestic violence and alcohol use. Blood and urine samples were drawn to test for HIV-1, HSV-2, syphilis, chlamydia, gonorrhea, trichomonas and Mycoplasma genitalium infections. The study was approved by the Harvard School of Public Health IRB (HSC Protocol #0108ACOM), University of Maryland IRB (Protocol #05-0031), Kilimanjaro Christian Medical Center Ethics Committee, Research and Ethical Clearance of the Tanzanian National Institute for Medical Research, the Centers for Disease Control and Prevention Institutional Review Board. Written informed consent for participation in the study was obtained from participants.
Study Measures
Demographic characteristics including age (20–24, 25–29, 30–34, 35+), education (pre-secondary, secondary and above), ethnicity (Chagga, Pare, other), and religion (Muslim/other, Catholic, Protestant) were considered. Moreover, STIs infections and symptoms, alcohol abuse, condom use in the last twelve months, and number of sexual partners they had in the last three years were considered. Alcohol abuse was measured by the CAGE score (Mayfield et al., 1974). An STI symptom was defined as a positive response to at least one of the following questions: abdominal pain, abnormal genital discharge, foul smell in the genital area, excessive genital secretions, swellings in the genital area, itching in the genital area, burning pain on micturition, pain during intercourse, and genital ulcers. Blood and urine samples were tested for HIV-1, HSV-2, syphilis, chlamydia, gonorrhea, trichomonas and Mycoplasma genitalium.
Statistical Analysis
Two-sample T-tests and one way ANOVA were used to compare duration of premarital sex between groups. Regression analyses were carried out using generalized linear mixed effects regression models to examine the association between duration of premarital sex, high-risk behaviors and STIs. More specifically, two-level mixed effects logistic regression models were used to examine the association of duration of premarital sex with STIs and high risk behaviors. Random intercepts were included in the logistic regression models to model the combined effect of all unobserved cluster-specific covariates. The regression analyses allowed for the two-level nested nature of the data, with women nested within geographic clusters, and were conducted using a generalized linear mixed models procedure, i.e., PROC GLIMMIX, in SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
Sixty percent (n=1,218) of the sampled women were either married or were living with a cohabitating partner at the time of the survey. Almost 13% (n=257) of the women were widowed, divorced or separated at the time of the survey. Twenty-seven percent (n=543) reported they had never been married. Premarital sex was defined as the time from sexual initiation to age at marriage. The analysis included the participants who provided complete information on age at first sex and age at marriage. Participants who reported that they had never had sexual intercourse and participants with unknown age at first sex or marriage were excluded from the analyses.
Out of the 2,019 surveyed women, 70% (n=1,414) provided their age at first sex and marriage. Out of the 1,414 participants with complete information, twenty-one women were excluded as their reported age at first sex was greater than their age at marriage. Thus, the analysis was restricted to the 1,393 women who provided complete data on age at first sex and marriage. The average duration of premarital sex was 1.66 years (SD of 2.61 years). Table 1 display the distribution of premarital sex duration by socio-demographic characteristics, alcohol and condom use. The duration of premarital sex significantly varied among the different age groups (p<0.01). Women aged 25–34 years reported longer duration of premarital sex compared to younger (< 25 years) or older (>34 years) women. Women with secondary school education and above reported longer duration of premarital sex compared to women with no or lower than secondary school education (p<0.01). Furthermore, duration of premarital sex was significantly associated with ethnicity (p<0.01) and religion of the women (p=0.01). Women who reported condom use in the previous twelve months had longer duration of premarital sex compared to women who reported no condom use (p=0.02). However, there was no significant difference in duration of premarital sex between women who abused alcohol versus those who did not use alcohol (p=0.91).
Table 1.
Distribution of premarital sex duration by socio-demographic characteristics, high-risk behaviors and sexually transmitted infections in Moshi women, Tanzania, 2002–2003.
| N | Mean (SD) | P-value | |
|---|---|---|---|
| Study covariates | |||
| Age in years | <0.01 | ||
| 20–24 | 291 | 1.05 (1.60) | |
| 25–29 | 349 | 1.86 (2.43) | |
| 30–34 | 310 | 2.12 (3.15) | |
| 35+ | 441 | 1.58 (2.80) | |
| Ethnicity | <0.01 | ||
| Chagga | 670 | 1.91 (2.84) | |
| Pare | 179 | 1.72 (2.61) | |
| Other | 543 | 1.32 (2.26) | |
| Religion | 0.01 | ||
| Muslim/Other | 549 | 1.41 (2.42) | |
| Catholic | 498 | 1.83 (2.79) | |
| Protestant | 346 | 1.82 (2.63) | |
| Education | <0.01 | ||
| Pre-secondary | 1066 | 1.48 (2.51) | |
| Secondary and above | 327 | 2.24 (2.86) | |
| Alcohol Abuse | 0.91 | ||
| No | 642 | 1.96 (2.74) | |
| Yes | 106 | 1.99 (2.60) | |
| Condom use** | 0.02 | ||
| Never | 1086 | 1.57 (2.47) | |
| Sometimes, often, always | 236 | 2.09 (3.16) | |
| Study outcomes | |||
| HIV-1 | <0.01 | ||
| No | 884 | 1.56 (2.53) | |
| Yes | 112 | 2.71 (3.54) | |
| HSV-2 | 0.01 | ||
| No | 506 | 1.48 (2.51) | |
| Yes | 490 | 1.91 (2.85) | |
| Other STIs*** | 0.02 | ||
| No | 909 | 1.58 (2.50) | |
| Yes | 158 | 2.12 (3.34) | |
| Symptoms of STIs | 0.07 | ||
| No | 1035 | 1.58 (2.57) | |
| Yes | 358 | 1.89 (2.73) | |
| Number of partners* | <0.01 | ||
| 1 | 1205 | 1.58 (2.54) | |
| 2+ | 111 | 2.72 (3.11) |
Number of partners in the last 3 years
Condom use in the last 12 months
Syphilis, chlamydia, Mycoplasma genitalium, gonorrhea and trichomonas
Table 1 also presents the distribution of premarital sex duration by STIs and number of sexual partners. The duration of premarital sex was significantly higher for women tested positive for HIV-1 (p<0.01), HSV-2 (p=0.01), and other STIs (p=0.02). Moreover, women with multiple partners had longer duration of premarital sex compared to women with one partner (p<0.01). Although it did not reach statistical significance, women with STIs symptoms reported longer duration of premarital sex (p=0.07) compared to women with out STIs symptoms.
Figure 1 displays the odds of STIs and multiple sexual partners per 1-year increase in duration of premarital sex. The odds of HIV-1 (OR=1.13; 95% CI=1.07–1.21; p<0.01), HSV-2 (OR=1.06; 95% CI=1.01–1.11; p=0.01) and other STIs (OR=1.07; 95% CI=1.01–1.13; p=0.03) increased by 13%, 6% and 7%, respectively, for a 1-year increase in duration of premarital sex. Moreover, the odds of having multiple partners increased by 14% per 1-year increase in duration of premarital sex (OR=1.14; 95% CI=1.07–1.21; p<0.01). Though women with longer premarital sex years reported higher odds of STIs symptoms, there was no significant association between premarital sex and symptoms of STIs (OR=1.04; 95% CI=0.99–1.09; p=0.07). Multivariate models were used to assess the association between duration of premarital sex and number of partners after adjusting for the effect of age, education, religion, tribe and condom use. The multivariate models used to examine the association between duration of premarital sex and STIs adjusted for the effect of multiple partners in addition to age, education, religion, tribe and condom use. The findings from both unadjusted and adjusted models were similar and were reported in Figure 1.
Figure 1.
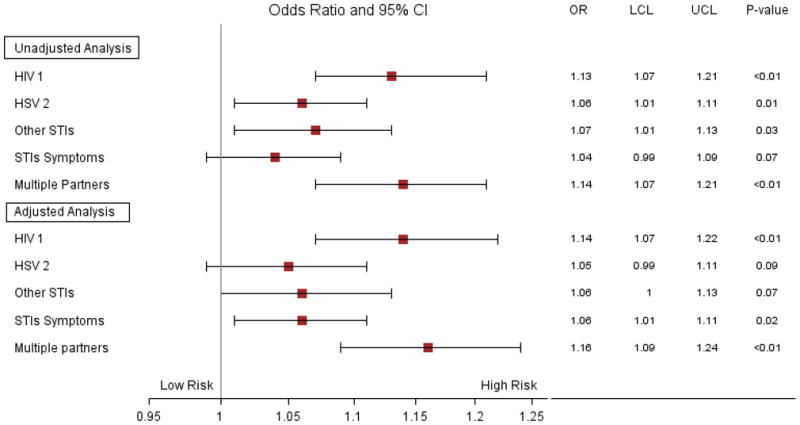
Odds of STIs and multiple sexual partners associated with 1-year increase in duration of premarital sex in Moshi women, Tanzania, 2002–2003. The adjusted analyses control for the effect of age, education, religion, tribe and condom use in the previous 12 months. Moreover, besides these variables, the adjusted analyses of STIs (HIV-1, HSV-2, other STIs, symptoms STIs) control for the effect of number of sexual partners.
Discussion
The primary focus of this study was to assess the relationship between duration of premarital sex, multiple sexual partners and the risk of acquiring STIs. Our study has revealed that time spent single after sexual debut was significantly associated with HIV and other STIs. We found higher odds of HIV-1, HSV-2 and other STIs among women with longer duration of premarital sex. Moreover, women with longer duration of premarital sex were more likely to report multiple sexual partners. These findings are consistent with previous studies from Tanzania and other sub-Saharan Africa countries (Bongaarts, 2007; Zaba et al., 2009). Bongaarts (2007) reported a positive association between late marriage after sexual initiation and HIV prevalence. In a study by Zaba et al (2009), longer duration of premarital sex was associated with higher rates of partner acquisition. Our study differs from previous studies by reporting both symptoms of STIs at the time of interview and STIs confirmed by laboratory testing in a large community based sample.
The results of our study should be interpreted in light of the following limitation. First, the data set is ten years old and changes in prevention, treatment and management of STIs should be taken into account while interpreting our findings. The accuracy of the information regarding multiple partners, age at first sex, and age at marriage may be affected by respondent and recall biases. In most sub-Saharan Africa cultures, women are not permitted to have sex outside marriage and multiple sexual partners. Thus, the self-reported data on women’s sexual behaviors could be an underestimation and may not be very reliable. Moreover, age at first sex and marriage were measured by self-report, which might have been affected by recall bias. Missing data is another limitation of the study. The analyses included only women who provided complete information on age at first sex, age at marriage, socio-demographic variables, high-risk behaviors, STIs and STIs symptoms. Analysis of the complete cases ignores the possible systematic difference between the women who provided information on these variables and those who did not. Finally, the use of recent number of partners data as a proxy for lifetime partners is subject to bias. Despite these limitations, our study has several strengths including a large sample size and a laboratory-confirmed STI diagnosis in a population based sample.
Our findings highlight the importance of long duration of premarital sex as a public health issue. These findings can be used to guide future HIV and other STIs preventive measures on late-marrying women in the region. Prevention programs should address factors leading to longer period between first sex and marriage, which may not be under the control of the woman. Further research is needed to identify the risk factors associated with longer period of premarital sex and to illuminate the association between premarital sex and STIs, which is of public health significance especially in sub-Saharan Africa where women are disproportionally affected by HIV and other STIs.
Acknowledgments
We thank the women of Moshi urban district of Tanzania for their participation and staff at the National Bureau of Statistics in Tanzania for conducting the survey. The study was supported by grants from Harvard University Center for AIDS Research (HU CFAR NIH/NAIDS P30-AI 060354).
References
- Bongaarts J. Late marriage and the HIV epidemic in sub-Saharan Africa. Popul Stud (Camb) 2007;61:73–83. doi: 10.1080/00324720601048343. [DOI] [PubMed] [Google Scholar]
- Bruce J, Clark S. Paper prepared for technical consultation on married adolescents. World Health Organization; Geneva, Switzerland: 2003. Including married adolescents in adolescent reproductive health and HIV/AIDS policy. [Google Scholar]
- Clark S. Early marriage and HIV risks in sub-Saharan Africa. Stud Fam Plann. 2004;35:149–160. doi: 10.1111/j.1728-4465.2004.00019.x. [DOI] [PubMed] [Google Scholar]
- Dickson N, Paul C, Herbison P, Silva P. First sexual intercourse: age, coercion, and later regrets reported by a birth cohort. BMJ. 1998;316:29–33. doi: 10.1136/bmj.316.7124.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan ME, Tibaux G, Pelzer A, Reimann K, Peutherer JF, Simmonds P, Young H, Jamil Y, Daroughar S. First coitus before menarche and risk of sexually transmitted disease. Lancet. 1990;335:338–340. doi: 10.1016/0140-6736(90)90617-e. [DOI] [PubMed] [Google Scholar]
- Glynn JR, Caraël M, Buvé A, Musonda RM, Kahindo M Study Group on the Heterogeneity of HIV Epidemics in African Cities . HIV risk in relation to marriage in areas with high prevalence of HIV infection. J Acquir Immune Defic Syndr. 2003;33:526–535. doi: 10.1097/00126334-200308010-00015. [DOI] [PubMed] [Google Scholar]
- Greenberg J, Magder L, Aral S. Age at first coitus. A marker for risky sexual behavior in women. Sex Transm Dis. 1992;19:331–334. [PubMed] [Google Scholar]
- Gregson S, Garnett GP, Nyamukapa CA, Hallett TB, Lewis JJ, Mason PR, Chandiwana SK, Anderson RM. HIV decline associated with behavior change in eastern Zimbabwe. Science. 2006;311:664–666. doi: 10.1126/science.1121054. [DOI] [PubMed] [Google Scholar]
- Kelly RJ, Gray RH, Sewankambo NK, Serwadda D, Wabwire-Mangen F, Lutalo T, Wawer MJ. Age differences in sexual partners and risk of HIV-1 infection in rural Uganda. J Acquir Immune Defic Syndr. 2003;32:446–451. doi: 10.1097/00126334-200304010-00016. [DOI] [PubMed] [Google Scholar]
- Larsen U, Mlay J, Aboud S, Ballard R, Sam NE, Shao JF, Kapiqa SH. Design of a community-based study of sexually transmitted infections/HIV and infertility in an urban area of northern Tanzania. Sex Transm Dis. 2007;34:20–24. doi: 10.1097/01.olq.0000218878.29220.8e. [DOI] [PubMed] [Google Scholar]
- Manning WD, Longmore MA, Giordano PC. The relationship context of contraceptive use at first intercourse. Fam Plann Perspect. 2000;32:104–110. [PubMed] [Google Scholar]
- Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistics. General report. Dar es Salaam: National Bureau of Statistics; 2002. Population and housing census 2002. [Google Scholar]
- Stoneburner RL, Low-Beer D. Population-level HIV declines and behavioral risk avoidance in Uganda. Science. 2004;304:714–718. doi: 10.1126/science.1093166. [DOI] [PubMed] [Google Scholar]
- Tanzania Commission for AIDS (TACAIDS), National Bureau of Statistics (NBS), ORC Macro. Tanzania HIV/AIDS Indicator Survey 2003–04. Calverton, Maryland, USA: TACAIDS, NBS, and ORC Macro; 2005. [Google Scholar]
- UNAIDS. Report on the global AIDS epidemic. Joint United Nations Programme on HIV/AIDS (UNAIDS) 2010; 2010. [Google Scholar]
- UNAIDS. UNAIDS world AIDS day report 2011. 2011. [Google Scholar]
- Zaba B, Isingo R, Wringe A, Marston M, Slaymaker E, Urassa M. Influence of timing of sexual debut and first marriage on sexual behaviour in later life: findings from four survey rounds in the Kisesa cohort in northern Tanzania. Sex Transm Infect. 2009;85(Suppl 1):i20–i26. doi: 10.1136/sti.2008.033704. [DOI] [PMC free article] [PubMed] [Google Scholar]


