Abstract
Background
Expectations of patients regarding their prospects for recovery have been shown to predict subsequent physical and social functioning. Evidence regarding the impact of expectations on clinical outcomes is limited.
Methods
At the inpatient service of a tertiary care hospital, we evaluated beliefs of patients undergoing coronary angiography about their prognosis as predictors of long-term survival and 1-year functional status. Baseline assessments, including a measure of expectations for recovery, were obtained during hospitalization with mortality follow-up for approximately 15 years. Patients with significant obstructive coronary artery disease were interviewed while in the hospital and enrolled in follow-up. Functional status was assessed at baseline and 1 year later with questionnaires reflecting physical capabilities. Analyses controlled for age, sex, disease severity, comorbidities, treatments, demographics, depressive symptoms, social support, and functional status. There were 1637 total deaths, 885 from cardiovascular causes, in the 2818 patients in these analyses. The outcomes were total mortality, cardiovascular mortality, and 1-year functional status.
Results
Expectations were positively associated with survival after controlling for background and clinical disease indicators. For a difference equivalent to an inter-quartile range of expectations, the hazard ratio (HR) for total mortality was 0.76 (95% confidence interval [CI], 0.71–0.82) and 0.76 (95% CI, 0.69–0.83) for cardiovascular mortality. The HRs were 0.83 (95% CI, 0.76–0.91) and 0.79 (95% CI, 0.70–0.89) with further adjustments for demographic and psychosocial covariates. Similar associations (P<.001) were observed for functional status.
Conclusion
Recovery expectations at baseline were positively associated with long-term survival and functioning in patients with coronary artery disease.
Patients differ widely in terms of their psychological reactions to major illnesses such as coronary heart disease. Their appraisals of the prospects for recovery form one aspect of these reactions. Some prior work has examined the links between recovery expectations and rehabilitation outcomes, such as self-reported well-being, functional status, and return to work, in patients with a variety of conditions.1,2 However, there has been little research to date documenting associations between patient recovery expectations and subsequent clinical events.
One would expect recovery expectations of a patient with coronary artery disease to be influenced by factors such as the severity of the illness, age, and functional status prior to the cardiac event. Furthermore, recovery expectations are likely to be related to depressive symptoms, which have a high prevalence in patients with coronary artery disease and have been shown to predict subsequent mortality as well as functional status.3,4 However, depressive symptoms are conceptually different from beliefs about recovery, even though they may be correlated or causally related. Thus, it is important for any investigation of recovery expectations to take the potentially confounding effects of illness severity, comorbidity, baseline functional status, demographic indicators, and psychosocial characteristics into account.
The present study used a cohort of patients with coronary artery disease who had a detailed baseline medical and psychosocial evaluation and extended follow-up to examine the prognostic effects of recovery expectations. The measure of recovery expectations consisted of questions relating specifically to cardiac conditions and recovery, in contrast to many other studies that use indicators of more global expectation tendencies, such as dispositional optimism.5 The measure of expectations was evaluated as a predictor of changes in functional status 1 year later and subsequent survival over a 15-year period.
METHODS
PARTICIPANTS
Patients undergoing diagnostic coronary angiography at Duke University Medical Center, Durham, North Carolina, from 1992 through 1996 who were found to have clinically significant disease (≥75% diameter stenosis of ≥1 coronary artery) were recruited for participation in the prospective Mediators of Social Support Study (MOSS), which was designed to assess the effects of social support and other psychosocial variables on patient well-being. Patients were excluded for any of the following conditions: prior angioplasty, congenital heart disease, primary valvular heart disease, substance abuse, history of impairing psychological disorder, or inability to give informed consent. The study was approved by the Duke University institutional review board, and all patients provided written informed consent. There were 3737 qualifying patients enrolled, but 368 were excluded owing to missing information on 1 or more of the basic clinical variables in the analyses. Another 551 patients were excluded because they failed to complete the measure of expectations. Therefore, the basic mortality analyses were conducted on data from 2818 patients (75% of the study population). Comparisons of those without completed expectations scores with the rest of the sample showed that patients missing these data were more likely to be male, older, and to have more severe disease. However, they did not have higher mortality rates once those clinical factors were controlled (P=.28).
There were an additional 426 patients missing from the 1-year functional status analyses because they had no data for either the baseline or 1-year assessments of that variable. Omitting the 170 patients who died before the 1-year follow-up, those patients with missing functional status data were significantly (P<.005) more likely to have congestive heart failure, diabetes mellitus, and peripheral vascular disease. They also had lower recovery expectations (P<.01). They did not differ on other baseline clinical variables.
Coronary artery bypass surgery (CABG) was performed on 1277 of the participants (45.3%) at some point during the follow-up period, with 1156 (41.0%) undergoing percutaneous transluminal coronary angioplasty (PTCA). Of these, both procedures were performed on 396 (14.1% of the sample). The remaining 781 patients (27.7%) were medically treated throughout the course of the study.
BASELINE MEASURES
Recovery Expectations
The Expectations for Coping Scale (ECS)6 consists of 18 questions inquiring about the patient’s expectations regarding future lifestyle (eg, “My heart condition will have little or no effect on my ability to do work,” “I expect that my lifestyle will suffer because of my heart condition”) and future cardiac prognosis (eg, “I doubt that I will ever fully recover from my heart problems,” “I can still live a long and healthy life”). Half of the items were worded so that agreement implied positive expectations, and half were worded in the other direction. Each item was answered on a 5-point Likert scale ranging from “strongly agree” to “strongly disagree,” and the responses were summed so that higher scores meant more positive expectations. Values for missing responses were prorated from the remaining items, but the scale was set to missing if there were more than 3 unanswered questions. Of a possible range of 0 to 90, the mean (SD) score was 63 (11), with a distribution that was approximately normal. There was a single factor in the present data, and satisfactory internal consistency was documented by a Cronbach α of 0.88. The ECS has been shown to predict subjective stress during follow-up of the present sample.7
Disease Severity and Health History
Coronary disease severity was controlled in the analyses by including the number of coronary arteries with at least 75% stenosis (1–3), left ventricular ejection fraction, and a 6-level variable indicating the presence and severity of congestive heart failure. These measures were obtained during the baseline angiographic examination.
The Duke Database electronic record was the source of information about comorbidities and relevant health history.8 Binary control variables were included indicating the presence or absence of each of the following conditions: diabetes mellitus, hyperlipidemia, history of cerebrovascular disease, history of peripheral vascular disease, and history of other major illnesses. The variable corresponding to “other major illnesses” was coded as positive if any of the following disorders was recorded: leukemia, lymphoma, renal disease, tumor, chronic obstructive pulmonary disease. In addition, information was obtained from the patient during the interview regarding their smoking history, yielding a binary variable that was coded as positive if they were currently smoking.
Functional Status
The Duke Activity Status Index (DASI)9 inquires about the patient’s ability to perform 12 activities ranging in physical demands from self-care and walking around the house to strenuous work such as lifting heavy furniture. Each activity was weighted by the average amount of metabolic output implied in its performance, and the final score was a sum of the weights of the performed activities. The DASI has been validated against the criterion of peak oxygen uptake during a stress test. DASI scores, which range from 0 (worst) to 58.2 (best), and can be converted into metabolic equivalent of task (MET) units by dividing them by 3.5.10 The mean (SD) in the present sample was 18.8 (16.3).
Social Support
The Interpersonal Support Evaluation List (ISEL)11 is a 40-item inventory designed to measure the perceived availability of 4 components of social support: instrumental support, emotional support, feelings of belonging, and self-esteem. A 16-item version, with 4 items per subscale, was used in this study. It has a range of 4 to 48 with a mean (SD) score of 38.6 (7.3). This brief scale accounted for 91% of the full scale’s variance in the derivation sample12 and was shown to predict both total mortality and cardiac mortality in the present sample.13
Depressive Symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D)14 is a 20-item measure of the frequency of various depressive symptoms during the previous week that has high internal consistency and reliability. Items pertain to depressive affect, somatic complaints, feelings of well-being, and social relations. It was designed for population samples but is also widely used in clinical studies and has been validated in patients with coronary artery disease.15 Scores can range from 0 to 60, with 16 or greater considered to be indicative of potentially significant depression.14 The mean (SD) score was 14.9 (11.1) in the present sample with 41% of patients scoring 16 or higher.
Demographic Measures
In addition to age and sex, demographic variables were covaried to control for potential economic and social confounding. These included education (number of years completed), ethnicity (white vs other), and marital status (married vs not married). Reported family income was also obtained but used only in a supplementary survival model because an additional 174 patients had missing values for that variable.
Outcomes
Mortality follow-up was conducted by the Duke Clinical Research Institute. Follow-up of the patients was conducted at 6 months and 12 months after catheterization and annually thereafter. December 2008 was considered the end of follow-up for these analyses. As of that date, 1637 of the 2818 patients had died, with 885 of the deaths classified by an independent events committee as being due to cardiac causes. Procedures for the documentation of cause of death used information provided by the patient’s physician and have been described elsewhere.16
Telephone interviews were conducted with patients 1-year after their hospitalization. DASI scores were obtained for 2392 patients who also had DASI scores at baseline and data on other variables in the primary model, representing 85% of those in the mortality analyses.
STATISTICAL ANALYSIS
Mortality
Analyses of the primary outcomes, all-cause and cardiac mortality, used Cox proportional hazard survival analysis techniques using SAS statistical software (version 9.1.3; SAS Inc, Cary, North Carolina). For each outcome, model 1 examined the effect of ECS scores controlling for age, sex, coronary artery disease severity indicators, medical treatments, smoking, and histories of the following comorbidities: cerebrovascular disease, peripheral vascular disease, hyperlipidemia, diabetes mellitus, and other major illnesses. Treatment was controlled with binary time-dependent variables for CABG and PTCA that were initially set to 0 and changed to 1 on the date of follow-up when they occurred. Model 2 added the DASI plus potential psychosocial and potential demographic confounders: race, education, marital status, depression, and social support. There were 2638 patients in model 2 owing to missing values for the additional covariates. A supplemental analysis was conducted that substituted household income for education in model 2. It was based on 2464 patients owing to additional missing values on the income measure. The survival time indicator was the difference between the date of enrollment and the date of death or the end of follow-up. Those who were lost or withdrew from follow-up were censored at the date of last contact. Follow-up times for surviving patients averaged 14.6 years and ranged up to 17 years. The assumption of proportional hazards was tested with an interaction between ECS and survival time in a time-dependent version of model 1.17 The test result was not significant (P>.05), indicating satisfactory fulfillment of the assumption.
Functional Status
Analyses of the functional status outcome applied general linear models to the prediction of DASI scores at the 1-year follow-up. Statistical assumptions of normality and homoscedasticity were tested by examining the equality of residual variances across the distribution of the expectations and found to be acceptable. Model 1 examined the association of ECS scores with follow-up DASI while controlling for baseline DASI scores, sex, age, disease severity indicators, treatment (CABG, PTCA) during the year, smoking, and comorbidities. Model 2 added potential psychosocial and demographic confounders. There were 2392 patients who could be included in model 1 and 2278 in model 2.
RESULTS
Patient characteristics, unadjusted death rates, and their relationships to recovery expectations are presented in Table 1. Most relationships are in the expected directions, with high positive expectations associated with less serious disease and a more positive psychosocial profile. Associations with most of the clinical indicators and risk factors are statistically significant, but they were modest in size and somewhat smaller than most of the associations with the psychosocial covariates. There were also trends for those with low expectations to be less likely to subsequently undergo CABG and PTCA. The magnitudes of these associations were independent of sex.
Table 1.
Patient Characteristics by Quartile of Expectation Scores
| Characteristic | Quartile
|
Correlation With ECSa | P Value | |||
|---|---|---|---|---|---|---|
| 1 (n = 720) | 2 (n = 657) | 3 (n = 724) | 4 (n = 717) | |||
| % Male | 67.78 | 66.82 | 68.92 | 72.38 | 0.06 | <.05 |
| Age, mean (SD), y | 62.94 (11.09) | 62.98 (10.89) | 62.68 (11.05) | 61.65 (10.79) | −0.04 | <.05 |
| Congestive heart failure, % | 34.03 | 23.29 | 20.99 | 11.58 | −0.21 | <.001 |
| 3-Vessel disease, % | 50.97 | 43.53 | 38.81 | 34.45 | −0.14 | <.001 |
| LVEF, mean (SD) | 48.15 (16.32) | 52.37 (15.59) | 53.32 (15.52) | 55.83 (13.52) | 0.19 | <.001 |
| History, % | ||||||
| Cerebrovascular disease | 17.92 | 10.35 | 11.88 | 9.34 | −0.10 | <.001 |
| Peripheral vascular disease | 20.00 | 16.13 | 14.64 | 11.02 | −0.10 | <.001 |
| Diabetes mellitus | 36.53 | 28.92 | 24.59 | 20.22 | −0.14 | <.001 |
| Hyperlipidemia | 54.72 | 55.40 | 55.39 | 55.29 | 0.01 | <.001 |
| Smoking | 22.64 | 21.16 | 19.06 | 18.41 | −0.04 | <.05 |
| Other major disease | 17.64 | 13.70 | 10.22 | 8.09 | −0.12 | |
| Baseline DASI, mean (SD)b | 9.99 (11.42) | 16.58 (15.01) | 21.08 (16.16) | 27.54 (16.76) | 0.41 | <.001 |
| CESD, mean (SD)c | 20.93 (11.26) | 15.64 (10.84) | 13.37 (9.83) | 9.87 (9.54) | −0.38 | <.001 |
| ISEL, mean (SD)d | 35.00 (7.90) | 37.56 (7.08) | 39.56 (6.25) | 42.19 (5.60) | 0.37 | <.001 |
| Married, % | 69.03 | 72.17 | 72.61 | 79.30 | 0.09 | <.001 |
| Education, mean (SD), y | 10.24 (3.65) | 11.21 (3.91) | 11.76 (3.79) | 12.66 (3.54) | 0.24 | <.001 |
| Minority, % | 21.9 | 19.7 | 15.7 | 10.5 | −0.11 | <.001 |
| Unadjusted, % | <.001 | |||||
| Mortality | 73.1 | 60.6 | 54.6 | 44.4 | −0.22 | <.001 |
| CABG | 35.8 | 50.7 | 46.7 | 48.5 | −0.09 | <.001 |
| PTCA | 35.1 | 39.1 | 41.2 | 48.5 | −0.10 | <.001 |
Abbreviations: CABG, coronary artery bypass surgery; CESD, Center for Epidemiologic Studies Depression Scale; DASI, Duke Activity Status Index; ECS, Expectations for Coping Scale; ISEL, Interpersonal Support Evaluation List; LVEF, left ventricular ejection fraction; PTCA, percutaneous transluminal coronary angioplasty.
Based on continuous ECS variable.
Functional status.
Depressive symptoms.
Social support.
MORTALITY
Table 2 presents the results of the mortality models for both the total mortality and the cardiac mortality outcomes. Metrics for the HRs are based on 1 interquartile range for continuous predictors with binary comparisons for dichotomous predictors.
Table 2.
Adjusted Hazard Ratios (HRs) (95% Confidence Intervals) From Survival Modelsa
| Variable | Total Mortality
|
Cardiac Mortality
|
||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Age | 2.25 (2.05–2.46) | 2.10 (1.91–2.31) | 2.04 (1.81–2.30) | 1.89 (1.67–2.15) |
| Sex (1=male) | 0.87 (0.78–0.97) | 1.04 (0.91–1.18) | 0.88 (0.76–1.01) | 1.01 (0.85–1.20) |
| LVEF | 0.64 (0.59–0.69) | 0.64 (0.60–0.69) | 0.51 (0.46–0.56) | 0.51 (0.46–0.57) |
| No. of arteries with ≥75% stenosis | 1.49 (1.31–1.71) | 1.49 (1.30–1.71) | 1.88 (1.56–2.27) | 1.84 (1.52–2.24) |
| Congestive heart failure | 1.09 (1.05–1.12) | 1.08 (1.04–1.11) | 1.10 (1.05–1.15) | 1.09 (1.04–1.14) |
| Cerebrovascular disease | 1.27 (1.11–1.45) | 1.24 (1.08–1.43) | 1.35 (1.13–1.60) | 1.31 (1.08–1.57) |
| Peripheral vascular disease | 1.32 (1.16–1.49) | 1.26 (1.11–1.43) | 1.27 (1.08–1.50) | 1.24 (1.04–1.47) |
| Diabetes mellitus | 1.52 (1.36–1.68) | 1.52 (1.36–1.69) | 1.70 (1.48–1.96) | 1.72 (1.49–2.00) |
| Hyperlipidemia | 0.84 (0.76–0.93) | 0.87 (0.78–0.96) | 0.88 (0.77–1.01) | 0.90 (0.78–1.04) |
| Other diseases | 1.65 (1.44–1.88) | 1.57 (1.37–1.80) | 1.23 (1.01–1.49) | 1.16 (0.95–1.43) |
| Current smoking | 1.24 (1.08–1.41) | 1.25 (1.09–1.43) | 1.11 (0.92–1.33) | 1.11 (0.91–1.34) |
| Race (1=white) | NA | 0.90 (0.79–1.03) | NA | 1.00 (0.83–1.20) |
| Education, y | NA | 0.93 (0.88–0.98) | NA | 0.94 (0.87–1.01) |
| Marital status (1=married) | NA | 0.78 (0.69–0.89) | NA | 0.78 (0.66–0.92) |
| Functional status: DASI | NA | 0.77 (0.70–0.85) | NA | 0.80 (0.70–0.92) |
| Depressive symptoms: CESD | NA | 0.97 (0.89–1.06) | NA | 0.91 (0.81–1.02) |
| Social support: ISEL | NA | 1.04 (0.96–1.12) | NA | 1.02 (0.91–1.13) |
| Expectations: ECS | 0.76 (0.70–0.82) | 0.83 (0.76–0.91) | 0.76 (0.69–0.83) | 0.79 (0.70–0.89) |
Abbreviations: CESD, Center for Epidemiologic Studies Depression Scale; CI, confidence interval; DASI, Duke Activity Status Index; ECS, Expectations for Coping Scale; ISEL, Interpersonal Support Evaluation List; LVEF, left ventricular ejection fraction; NA, not applicable.
For continuous variables the HRs reflect the effect size associated with a difference equal to the interquartile range. All estimates were controlled for the occurrence of coronary artery bypass surgery and percutaneous transluminal coronary angioplasty, which are not presented in the table because they were time-dependent covariates.
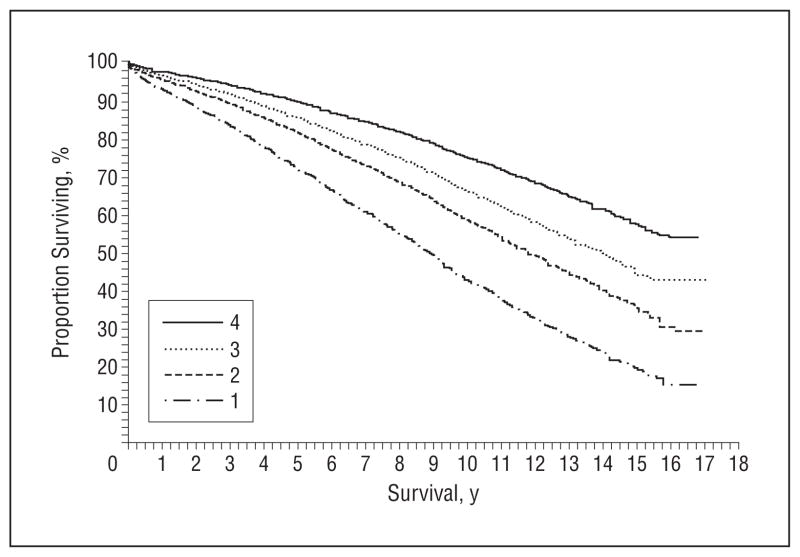
ECS scores indicating positive expectations were associated with reduced mortality risk for both outcomes despite extensive controls for clinical disease indicators (model 1) plus potentially confounding psychosocial variables (model 2). Results were essentially the same (hazard ratio [HR], 0.84; 95% confidence interval [CI],0.77–0.91 for ECS) when income was substituted for education as the covariate in the total mortality model 2. The relationship between recovery expectations quartiles and total mortality risk is further illustrated in the survival curves displayed in the Figure, which are adjusted within quartiles for the covariates in model 1. Unadjusted data show that the mortality rate of those in the highest quartile of expectations was 28.8 deaths per 100 patients during the 10 years after baseline compared with 56.9 deaths per 100 for those in the lowest quartile. The predicted rates after complete adjustments across quartiles for the covariates in model 1 yield predictions of 31.8 vs 46.2 deaths per 100, thus illustrating a substantial magnitude of this effect even after taking multiple covariates into account.
Figure.
Cox model curves of survival probability by quartiles of Expectations for Coping Scale scores adjusted within quartile for age, sex, treatment, disease severity, comorbidity, and smoking status. “4” Indicates high expectation scores, and “1” indicates low expectation scores.
FUNCTIONAL STATUS AT 1 YEAR
The mean (SD) change in functional status in the overall cohort was 2.9 points (15.7) with 53.8% showing an improvement after their hospitalization and 35.2% showing a decline. The multiple regression models showed that ECS scores were predictors (P <.001) of DASI scores at follow-up after controlling for baseline scores as well as all of the clinical and psychosocial covariates. The difference in DASI scores associated with an interquartile range difference in model 1 was 4.70, equivalent to 1.34 METS. This is above the levels considered to be clinically significant.18
COMMENT
This study of a large cohort of patients with coronary artery disease showed that a measure of patient expectations regarding the prospects for resumption of normal life was a risk factor for mortality over an extended follow-up period and a predictor of functional status recovery 1 year after hospitalization. These effects were statistically significant (P<.001) while controlling for age, sex, clinical measures of coronary disease severity, comorbidity, demographic characteristics, and indicators of psychosocial well-being.
A number of studies have examined the effects of the knowledge and attitudes of patients with cardiac disease about their disease as determinants of health behaviors and functional outcomes.19 Expectations and related beliefs have been shown to be good predictors of outcomes such as functional status and return to work,1,2 although data on the prediction of attendance at cardiac rehabilitation have been more mixed.20 The effect of ECS scores on the prediction of functional status at 1 year after hospitalization is congruent with these previous findings, and the continued presence of the relationship despite a wide array of covariates extends this evidence. However, the most novel findings in the present study are the associations between expectations and subsequent survival. There are several relevant lines of research that suggest mechanisms to potentially account for them.
Recovery expectations are linked to levels of negative affect, which has a high prevalence in patients with cardiac disease21 and has been shown to predict early mortality.4 In the present study, 41% of the patients had CESD scores of 16 or higher, a level that is indicative of substantial depression.14 There was an association between expectations and depressive symptoms (Table 1). However, statistical adjustments for depressive symptoms and other psychosocial characteristics had minimal impact on the magnitude of the expectations effect.
Another related characteristic that has been found to predict clinical events is dispositional optimism. This is conceptualized as a global personality characteristic reflecting a person’s general outlook on life.5 Measures of optimism have been shown to predict recurrent coronary events in patients undergoing surgery22 and cardiovascular deaths in a population sample.23 No direct measures of this concept were available in the present study to compare with the ECS measure, but there are reasons to believe that the recovery expectation concept has advantages in the context of the treatment of patients with existing coronary disease. Measures of more specific expectations for future activities, such as return to work, have been found to be better predictors of those outcomes than more general measures.24 It is likely that explicit characteristics, such as recovery expectations, will be more amenable to change with interventions.
An additional construct related to expectations that has been the subject of past research is self-rated health, which has been shown to predict health outcomes in both population samples25 and patients with cardiac disease.26 An earlier analysis showed that it was a predictor of mortality in a subsample of the MOSS study.27 Evaluation of current health is one aspect of recovery expectations measured by the ECS in the current study, but recovery expectations constitute a broader construct with emphasis on future, rather than current, health. It was possible to test the contributions of self-rated heath and the ECS in the present study because a 5-level rating of current heath (“In general, would you say that your health is: excellent, very good, good, fair, or poor?”) was available for 2670 of the patients. Analyses (data not shown) revealed that ECS scores remained as a statistically significant (P<.01) predictor of survival even after controls for self-rated health were instituted. The ECS HR for total mortality was 0.86 (95% CI, 0.80–0.93) controlling for age, sex, disease severity, comorbidities, smoking, and self-rated health. For cardiac mortality the HR was 0.85 (95% CI, 0.76–0.94).
There are at least 2 plausible mechanisms that might help explain the observed effects of expectations. One involves the effectiveness of strategies that patients use to cope with the recovery process, the mechanism that is often used to explain the association between optimistic predispositions and good health.28 Optimists have been found to be more likely to address the demands of a problem rather than withdrawing or focusing on its emotional consequences.5,28 This coping predisposition may generalize to those patients with high recovery expectations, making their coping more effective in reducing risk factor levels and improving levels of life satisfaction.
A second hypothesis is based on the likelihood that those with pessimistic expectations will experience more tension and negative emotions during the recovery period, resulting in heightened stress reactions, autonomic dysregulation and other physiological responses that increase the risk of cardiac events.29 This tendency has been observed in the sample of the present study.7
There are a number of limitations to this study that should be kept in mind when interpreting its findings. Foremost is the possibility that both expectations and survival are associated with some unmeasured confounders, such as unmeasured risk factors or differential treatment by physicians and staff, that may affect expectations. In addition, a recent study of patients with heart failure reported no association between patients’ estimates of their longevity and actual survival. The apparent discrepancy with the findings of the current study could be due to a number of factors. The predictor in the previous study was 1 item on expected life span in contrast to the more comprehensive content of the ECS measure. There are also some differences in patient selection criteria and a substantial difference in sample sizes. However, results of the previous study30 suggest that there are limits on the phenomena we observed, constituting an important issue for future work.
Selection bias is another potential limitation of these data. Patients were not included in the study if they did not qualify, did not agree to participate, or had missing data on critical variables. Those patients undoubtedly differed from those who were included, and it is not certain that the findings will generalize to them. This is especially true for the follow-up functional status outcome, which was not obtained on the most severely ill patients who had an early death. Of course, this bias could also create an underestimate of the expectations effect through restriction of range in the predictors.
Recovery expectations are parts of a wider array of health beliefs that affect a person’s decisions about risk factors and health care.31 A promising aspect of research on this topic suggests that these beliefs are subject to modification through brief clinical interventions. Initial clinical trials involving individualized counseling sessions designed to improve the patient’s pattern of illness beliefs have been conducted with patients with cardiac disease during their hospitalization and were successful in improving rates of return to work, with some evidence of positive effects on anginal pain and exercise habits.31,32 The present study suggests that additional trials should be undertaken to see if these benefits extend to mortality rates and other clinical outcomes. If so, it could be an efficient and valuable addition to cardiac care.
In conclusion, patients with coronary artery disease who had more favorable expectations about their likelihood of recovery and return to a normal lifestyle had better long-term survival as well as better functional status after their hospitalization. The effects were independent of numerous potential clinical, demographic, and psychosocial confounders. These findings argue for expanded efforts to understand the influence of recovery expectations and the potential benefits of attempts to modify them. The potential feasibility of altering specific aspects of patient beliefs provides a promising avenue for intervention if the importance of expectations is confirmed.
Acknowledgments
Funding/Support: This study was funded by grants RO1-HL45702 and PO1-HL36587 from the National Heart, Lung, and Blood Institute and by grant RO1-HL54780 from the National Heart, Lung, and Blood Institute with cofunding by the National Institute on Aging.
Footnotes
Financial Disclosure: Dr Williams has a patent pending (No. 7 311 522) on the use of 5HTTLPR L allele as a marker of increased CVD risk due to stress. He is a founder and major stockholder in Williams LifeSkills Inc.
Previous Presentation: A preliminary version of this study was presented at the 66th Meeting of the American Psychosomatic Society; March 14, 2008; Baltimore, Maryland.
Author Contributions: Dr Barefoot had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Barefoot. Acquisition of data: Barefoot, Clapp-Channing, and Siegler. Analysis and interpretation of data: Barefoot, Brummett, Williams, Siegler, Helms, Boyle, and Mark. Drafting of the manuscript: Barefoot. Critical revision of the manuscript for important intellectual content: Barefoot, Brummett, Williams, Siegler, Helms, Boyle, Clapp-Channing, and Mark. Statistical analysis: Barefoot, Brummett, Helms, and Boyle. Obtained funding: Barefoot, Williams, and Mark. Administrative, technical, and material support: Siegler. Study supervision: Clapp-Channing and Mark.
References
- 1.Petrie KJ, Weinman J, Sharpe N, Buckley J. Role of patients’ view of their illness in predicting return to work and functioning after myocardial infarction: longitudinal study. BMJ. 1996;312(7040):1191–1194. doi: 10.1136/bmj.312.7040.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you’ll do? a systematic review of the evidence for a relation between patients’ recovery expectations and health outcomes. CMAJ. 2001;165(2):174–179. [PMC free article] [PubMed] [Google Scholar]
- 3.Blumenthal JA, Lett HS, Babyak MA, et al. NORG Investigators. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003;362(9384):604–609. doi: 10.1016/S0140-6736(03)14190-6. [DOI] [PubMed] [Google Scholar]
- 4.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 5.Scheier MF, Carver CS. Effects of optimism on psychological and physical well-being: theoretical overview and empirical update. Cognit Ther Res. 1992;16 (2):201–228. [Google Scholar]
- 6.Axelrad K. Locus of control and causal attributions as they relate to expectations for coping with a heart attack. Diss Abstr Int. 1982;42(12):4924. [Google Scholar]
- 7.Brummett BH, Babyak MA, Mark DB, Clapp-Channing NE, Siegler IC, Barefoot JC. Prospective study of perceived stress in cardiac patients. Ann Behav Med. 2004;27(1):22–30. doi: 10.1207/s15324796abm2701_4. [DOI] [PubMed] [Google Scholar]
- 8.Fortin DF, Califf RM, Pryor DB, Mark DB. The way of the future redux. Am J Cardiol. 1995;76(16):1177–1182. doi: 10.1016/s0002-9149(99)80331-2. [DOI] [PubMed] [Google Scholar]
- 9.Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 10.Wessel TR, Arant CB, Olson MB, et al. Relationship of physical fitness vs body mass index with coronary artery disease and cardiovascular events in women. JAMA. 2004;292(10):1179–1187. doi: 10.1001/jama.292.10.1179. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research and Application. The Hague, the Netherlands: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- 12.Brummett BH, Babyak MA, Barefoot JC, et al. Social support and hostility as predictors of depressive symptoms in cardiac patients one month after hospitalization: a prospective study. Psychosom Med. 1998;60(6):707–713. doi: 10.1097/00006842-199811000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Brummett BH, Mark DB, Siegler IC, et al. Perceived social support as a predictor of mortality in coronary patients: effects of smoking, sedentary behavior, and depressive symptoms. Psychosom Med. 2005;67(1):40–45. doi: 10.1097/01.psy.0000149257.74854.b7. [DOI] [PubMed] [Google Scholar]
- 14.Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 15.McManus D, Pipkin SS, Whooley MA. Screening for depression in patients with coronary heart disease (data from the Heart and Soul Study) Am J Cardiol. 2005;96(8):1076–1081. doi: 10.1016/j.amjcard.2005.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PJ, Lee KL, Harrell FE, Jr, Behar VS, Rosati RA. Outcome in medically treated coronary artery disease: ischemic events: nonfatal infarction and death. Circulation. 1980;62(4):718–726. doi: 10.1161/01.cir.62.4.718. [DOI] [PubMed] [Google Scholar]
- 17.Collett D. Modeling Survival Data in Medical Research. 2. New York, NY: Chapman & Hall; 2003. [Google Scholar]
- 18.Hlatky MA, Rogers WJ, Johnstone I, et al. Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. N Engl J Med. 1997;336(2):92–99. doi: 10.1056/NEJM199701093360203. [DOI] [PubMed] [Google Scholar]
- 19.Petrie KJ, Weinman JA. Illness representations and recovery from myocardial infarction. In: Petrie KJ, Weinman JA, editors. Perceptions of Health and Illness: Current Research and Applications. Amsterdam, the Netherlands: Harwood Academic Publishers; 1997. pp. 441–462. [Google Scholar]
- 20.French DP, Cooper A, Weinman J. Illness perceptions predict attendance at cardiac rehabilitation following acute myocardial infarction: a systematic review with meta-analysis. J Psychosom Res. 2006;61(6):757–767. doi: 10.1016/j.jpsychores.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 21.Schleifer SJ, Macari-Hinson MM, Coyle DA, et al. The nature and course of depression following myocardial infarction. Arch Intern Med. 1989;149(8):1785–1789. [PubMed] [Google Scholar]
- 22.Scheier MF, Matthews KA, Owens JF, et al. Optimism and rehospitalization after coronary artery bypass graft surgery. Arch Intern Med. 1999;159(8):829–835. doi: 10.1001/archinte.159.8.829. [DOI] [PubMed] [Google Scholar]
- 23.Giltay EJ, Kamphuis MH, Kalmijn S, Zitman FG, Kromhout D. Dispositional optimism and the risk of cardiovascular death: the Zutphen Elderly Study. Arch Intern Med. 2006;166(4):431–436. doi: 10.1001/archinte.166.4.431. [DOI] [PubMed] [Google Scholar]
- 24.Maeland JG, Havik OE. Psychological predictors for return to work after a myocardial infarction. J Psychosom Res. 1987;31(4):471–481. doi: 10.1016/0022-3999(87)90005-5. [DOI] [PubMed] [Google Scholar]
- 25.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 26.Gerber Y, Benyamini Y, Goldbourt U, Drory Y Israel Study Group on First Acute Myocardial Infarction. Prognostic importance and long-term determinants of self-rated health after initial acute myocardial infarction. Med Care. 2009;47(3):342–349. doi: 10.1097/MLR.0b013e3181894270. [DOI] [PubMed] [Google Scholar]
- 27.Bosworth HB, Siegler IC, Brummett BH, et al. The association between self-rated health and mortality in a well-characterized sample of coronary artery disease patients. Med Care. 1999;37(12):1226–1236. doi: 10.1097/00005650-199912000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Nes LS, Segerstrom SC. Dispositional optimism and coping: a meta-analytic review. Pers Soc Psychol Rev. 2006;10(3):235–251. doi: 10.1207/s15327957pspr1003_3. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 30.Allen LA, Yager JE, Funk MJ, et al. Discordance between patient-predicted and model-predicted life expectancy among ambulatory patients with heart failure. JAMA. 2008;299(21):2533–2542. doi: 10.1001/jama.299.21.2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ. Further development of an illness perception intervention for myocardial infarction patients: a randomized controlled trial. J Psychosom Res. 2009;67(1):17–23. doi: 10.1016/j.jpsychores.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Petrie KJ, Cameron LD, Ellis CJ, Buick D, Weinman J. Changing illness perceptions after myocardial infarction: an early intervention randomized controlled trial. Psychosom Med. 2002;64(4):580–586. doi: 10.1097/00006842-200207000-00007. [DOI] [PubMed] [Google Scholar]