Abstract
Objective:
To assess changes in mandibular third molar angulation during orthodontic treatment in subjects having either first or second premolars or neither removed.
Materials and Methods:
In a retrospective study approved by the institutional review board, right and left mandibular third molar angulations were compared to the vertical axis of adjacent second molars before and at the end of orthodontic treatment. The sample included 25 subjects with first premolars removed, 25 subjects with second premolars removed, and 24 subjects with no premolars removed. A decrease in angulation over time of at least 5°, so that the third molar became more vertical, was considered clinically favorable. Data were assessed by a linear mixed effect model and a proportional odds model with significance set at P < .05.
Results:
Prior to treatment, the average mandibular third molar angulation did not differ significantly among the three study groups (P = .97). The average change during treatment was not significantly affected by group (P = .59), but a higher proportion of mandibular third molars were more vertical by at least 5° in the second premolar extraction group compared to the other two groups at the completion of treatment.
Conclusion:
Although creating space for third molars to erupt and function has intuitive appeal, clinicians should not assume that third molars will move upright to a vertical position even if premolar removal is performed as part of an orthodontic treatment plan.
Keywords: Premolar, Third molar
INTRODUCTION
Adolescent patients and their parents often question why premolars and third molars should be removed as part of an orthodontic plan. Most understand that premolar removal creates space so teeth can be aligned. However, the question regarding third molars arises toward the end of orthodontic treatment, “Why do I have to lose more permanent teeth?” A greater chance of having space to retain useful third molars was offered as an additional reason for premolar extraction when more frequent removal of premolars was proposed in the mid-20th century.1 Are third molars more likely to be in a position to erupt to the occlusal plane when premolars are removed?
Third molars are the last teeth to erupt to the occlusal plane, often after jaw growth is complete.2 As a consequence, incomplete eruption of a third molar occurs chiefly because insufficient space exists in the jaw. Investigators have studied eruption patterns of mandibular third molars, but predicting the required space before jaw growth is complete has not been successful.3 And even when the space was judged to be inadequate, mandibular third molars erupted half the time.4 Nance et al.5 suggested that if unerupted third molars were more vertical, eruption to the occlusal plane was more likely than if the third molars were inclined more mesially. This supports the thought that if additional space is created in the jaw by removal of premolars, third molars may be more likely to move upright to a vertical position as a prelude to eruption.
This study was designed to assess changes in mandibular third molar angulation as compared to the long axis of second molars from beginning to end of orthodontic treatment in subjects having first or second premolars removed or no premolars removed.
MATERIALS AND METHODS
For this retrospective study approved by the institutional review board, a sample of 25 subjects with first premolars removed, 25 subjects with second premolars removed, and 24 subjects with no premolars removed was obtained from records in a university orthodontic clinic with treatment by orthodontic residents. Patients who had third molars removed before completion of orthodontic treatment, with an orthognathic surgery plan, or treatment for a craniofacial defect were excluded. A review of records began in 2011 and all subjects with completed records before and after treatment were included, working backward until the desired number of subjects in each category was obtained. Sufficient electronic records with digital panoramic radiographs were available for subjects in the first premolar and no premolar removal groups. Since second premolar removal is less frequent in orthodontic treatment, both electronic and hard copies of records were utilized, spanning the years 1996 to 2011.
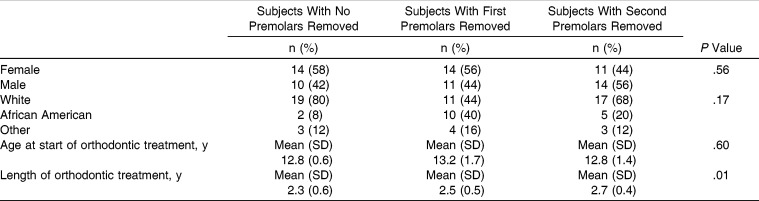
The three study groups did not differ significantly in average age (P = .60) (Table 1). Overall, the subjects were approximately 13 years old on average at the start of treatment, were predominately white (64%), and almost equally divided by gender (53% female). The proportion of African Americans was slightly higher in the first premolar removal group, but the racial distribution was not statistically different among the groups (P = .17).
Table 1.
Characteristics of Subjects/Patients (N = 74) at Enrollment Grouped by Those With No Mandibular Premolars Removed (n = 24), Mandibular First Premolars Removed (n = 25), or Second Premolars Removed (n = 25) as Part of Orthodontic Treatment
For each subject, the vertical axis of the mandibular second and third molars was established from the panoramic radiographs, and changes in the orientation of the third molars relative to the second molars during treatment was calculated for each side (Figure 1). A decrease of 5° or more was considered clinically favorable, and an increase of 5° or more was considered clinically detrimental.
Figure 1.
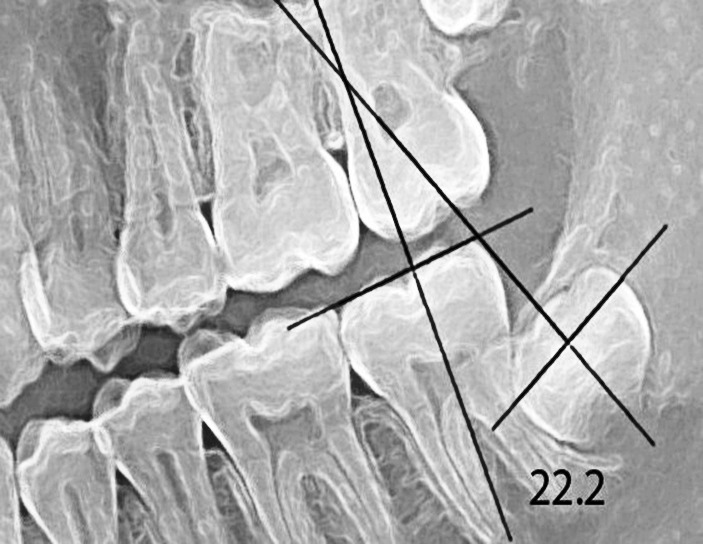
The angulation of the developing third molar was compared to the long axis of the adjacent second molar on panoramic radiographs at the beginning and at the end of orthodontic treatment.
The demographic characteristics and treatment length of the three study groups were compared using chi-square test for nominal variables and one-way analysis of variance for continuous variables. The changes in angulation as well as the categorization of the change as clinically favorable or unfavorable were assessed using a linear mixed effect model and a proportional odds model with one between-subject factor, extraction group, and one within-subject factor, side. Significance was set at P < .05.
RESULTS
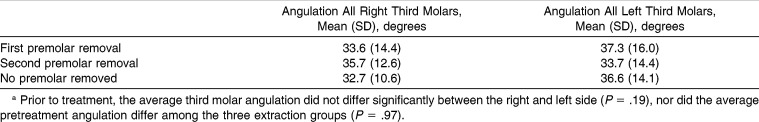
Prior to treatment, the average mandibular third molar angulation did not differ significantly between the right and left sides (P = .19), nor did the average pretreatment angulation differ among the three study groups (P = .97) (Table 2). Average treatment time was significantly different among the three groups (P = .01): treatment in the second premolar group took 4 months longer, on average, than in the nonextraction group, and took 2 months longer in the first premolar group (Table 1).
Table 2.
The Angulation of Mandibular Third Molars to the Long Axis of Adjacent Second Molars at the Initiation of Orthodontic Treatment Compared by Anatomic Side and First or Second Premolar Removal or No Premolar Removeda
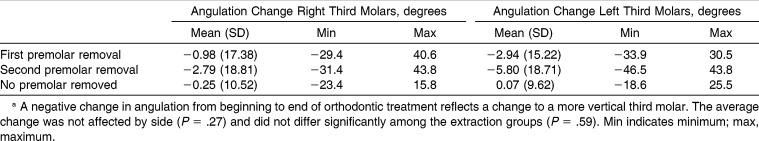
The average change in third molar inclination during treatment was not affected by side (P = .27) and did not differ significantly among the study groups (P = .59), likely because of the extremely large variability observed (Table 3). A higher proportion of mandibular third molars, both right and left, were more vertical by at least 5° in the second premolar removal group compared to the other two groups at the completion of treatment. But again, neither side (P = .27) nor extraction group (P = .34) was a statistically significant explanatory factor for a clinically favorable change in angulation (Figure 2).
Table 3.
Changes in the Angulation of Mandibular Third Molars Compared to the Long Axis of Adjacent Second Molars During Orthodontic Treatment Compared by First or Second Premolar Removal or No Premolar Removeda
Figure 2.
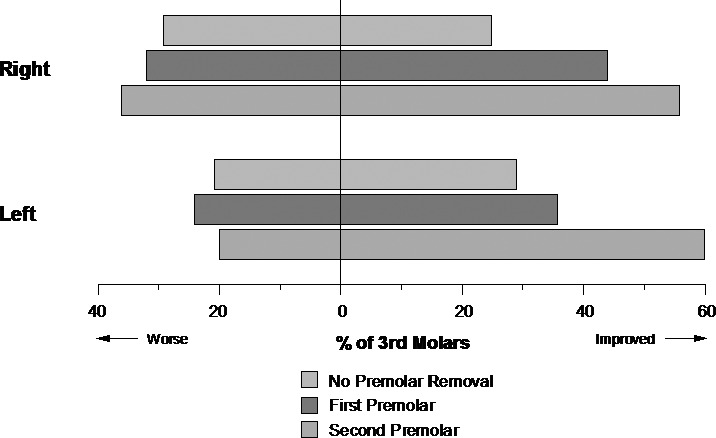
Changes in mandibular third molar angulation from beginning to end of orthodontic treatment: no premolars removed (n = 24), first premolars removed (n = 25), and second premolars removed (n = 25). Improved indicates third molars were more vertical at the end of treatment as compared to the beginning of treatment.
DISCUSSION
It seems reasonable that orthodontic treatment leading to mesial movement of mandibular second molars would provide space for eruption of the third molars, and it has been shown that removal of mandibular first molars does improve the chance of third molar eruption.6 First molar removal, however, rarely is an option in orthodontic treatment, while second or first premolar removal is an option and mesial movement of the molars is expected in orthodontic closure of premolar extraction spaces.
The data from this study indicate that although second premolar removal increases the number of patients with upright third molars that are more likely to erupt, clinicians are not able to reliably advise patients to retain or remove third molars at the end of orthodontic treatment based on premolar removal or not. The changes in third molar angulation over the time course of orthodontic treatment in the three groups were not statistically significant because of the wide range of angulations and changes within each group. Approximately a quarter of third molars from each of the three groups showed an unfavorable change in angulation, so that they were more horizontal at treatment completion than pretreatment. The wide variability in outcomes over time for third molars in each of the three groups of subjects studied is reflected in the standard deviations for the average changes in third molar angulation (Table 3).
The decision to remove either first or second premolars as part of orthodontic treatment is based on the need to create space at specific locations in the dental arch. Most orthodontists would consider space to accommodate third molars as a secondary consideration or not applicable to successful orthodontic outcomes. If mandibular anterior teeth are proclined, removal of first premolars to allow incisor retraction is a reasonable option. The greater number of African American subjects in the first premolar group likely reflects the fact that proclined incisors are found frequently in this ethnic group. In contrast, second premolar removal indicates that mesial movement of the molars, not incisor retraction, is desired, usually in treatment of Class II problems. The additional space might allow a developing third molar to move into a more vertical position. Unfortunately, this outcome for third molars after orthodontic treatment with second premolar removal is not uniform and cannot reliably be predicted.
Clinicians should consider risk indicators other than the likelihood of eruption to the occlusal plane when making recommendations on third molar management. In the Nance et al.5 study of 237 young adults with asymptomatic third molars followed for an average of 2 years, vertical or distoangular third molars were more likely to erupt to the occlusal plane as compared to third molars angled at least 25° to the long axis of the adjacent second molar. However, half of the mandibular third molars in the Nance et al.5 subjects had clinical indicators suggesting periodontal inflammatory disease after eruption, at least one probing depth 4 mm or greater (PD4+).
For 194 subjects with asymptomatic third molars followed for an average of 6 years, if one PD4+ was detected around a third molar or on the distal of the adjacent second molar at enrollment, odds were twelvefold that at least four PD4+ were detected at follow-up, P < .01.7 For the subjects affected at enrollment, odds were fivefold greater that at least one PD4+ would be detected on teeth more anterior in the mouth at follow-up with no teeth more anterior involved prior, P < .01.
A recent review of available third molar data from clinical studies and studies conducted for other purposes suggested that having a visible third molar may be a risk indicator by itself for an anaerobic environment conducive to periodontal inflammatory disease.8 Deeper mean periodontal probing depths around first and second molar regions were detected more often in individuals with visible third molars, and third molar mean probing depths were greater than mean probing depths on other teeth more anterior in the mouth.
Third molars at the occlusal plane may be affected by caries with or without periodontal inflammatory disease. In a comprehensive analysis of caries incidence and increment over time, Divaris et al.9 suggested that occlusal caries is not unique to third molars. If caries was detected in a first or second molar, chances were high, 80% greater, that a third molar would be affected subsequently. Conversely, Fisher et al.10 reported that few third molars, 2% or less, had caries experience detected at enrollment or at follow-up an average of 7 years later if no caries experience was detected on molars more anterior.
The data we report have limitations. The ethnic distribution of the subjects was not representative of the general population. African Americans were overrepresented as compared to whites. Few Asians or Latinos were studied, limiting the generalizability of the findings across all ethnic groups. Also, all subjects received orthodontic treatment. It is possible, though we consider it unlikely, that those who do not receive orthodontic treatment would exhibit results different from the subjects of this study. Further study might add to the outcomes we report. A prospective clinical study that included premolar removal and measurement of the deliberate anterior movement of lower molar teeth in the jaw might lead to different results.
How should clinicians interpret and use the data we report to advise patients about third molar management? The removal of premolars as part of an orthodontic treatment plan should not influence the decision to retain or remove third molars. Other risk indicators should be considered, particularly third molar caries or periodontal inflammatory disease affecting third molars.
CONCLUSION
Although creating space for third molars to erupt and function has intuitive appeal, clinicians should not assume that third molars will move upright to a vertical position even if premolar removal is performed as part of an orthodontic treatment plan.
REFERENCES
- 1.Begg PR, Kesling PC. Begg Orthodontic Theory and Technique. Philadelphia, Pa: Saunders; 1977. [Google Scholar]
- 2.Rantanen AV. The age of eruption of the third molar teeth. A clinical study based on Finnish university students. Acta Odontol Scand. 1967;25(48 suppl):1–86. [Google Scholar]
- 3.Forsberg CM. Tooth size, spacing and crowding in relation to eruption or impaction of third molars. Am J Orthod. 1988;94:57–62. doi: 10.1016/0889-5406(88)90451-9. [DOI] [PubMed] [Google Scholar]
- 4.Forsberg CM, Vingren B, Wesslen U. Mandibular third molar eruption in relation to available space as assessed on lateral cephalograms. Swed Dent J. 1989;13:23–31. [PubMed] [Google Scholar]
- 5.Nance PE, White RP, Jr, Offenbacher S, Phillips C, Blakey GH, Haug RH. Change in third molar angulation and position in young adults and follow-up periodontal pathology. J Oral Maxillofac Surg. 2006;64:424–428. doi: 10.1016/j.joms.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Ay S, Agar U, Bicakci A, Kosger HH. Changes in mandibular third molar angle and position after unilateral mandibular first molar extraction. Am J Orthod Dentofacial Orthop. 2006;129:36–41. doi: 10.1016/j.ajodo.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 7.White RP, Jr, Phillips C, Hull DJ, Offenbacher S, Blakey GH, Haug RH. Risk markers for progression of periodontal pathology in the third molar and non-third molar regions in young adults. J Oral Maxillofac Surg. 2008;66:749–754. doi: 10.1016/j.joms.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 8.White RP, Fisher EL, Phillips C, Tucker M, Moss KL, Offenbacher S. Visible third molars as risk indicators for increased periodontal probing depth. J Oral Maxillofac Surg. 2011;69:92–103. doi: 10.1016/j.joms.2010.07.076. [DOI] [PubMed] [Google Scholar]
- 9.Divaris K, Fisher EL, Shugars DA, White RP., Jr Risk factors for third molar occlusal caries: a longitudinal clinical investigation. J Oral Maxillofac Surg. 2012;70:1771–1780. doi: 10.1016/j.joms.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 10.Fisher E, Garaas R, Blakey G, Offenbacher S, Shugars D, Phillips C, White R. Changes over time in the prevalence of caries experience or periodontal pathology on third molars in young adults. J Oral Maxillofac Surg. 2012;70:1016–1022. doi: 10.1016/j.joms.2011.10.016. [DOI] [PubMed] [Google Scholar]