Abstract
Objective: To determine a treatment strategy based on the outcomes of various previous interventions for critical limb ischemia in arteriosclerosis obliterans (ASO).
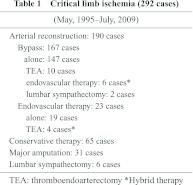
Material and Methods: We examined outcomes of 292 ASO patients who had had critical limb ischemia between May 1995 and July 2009. Patients underwent the following procedures in 167 cases: aortofemoral bypass (n = 14), femorofemoral crossover bypass (n = 29), femoropopliteal bypass (n = 104) and femorotibial bypass (n = 40). Other procedures included bypass only (n = 147), bypass combined with thromboendarterectomy (n = 10), bypass combined with endovascular therapy (n = 6), bypass combined with lumbar sympathectomy (n = 2), endovascular therapy combined with thromboendarterectomy (n = 4), endovascular therapy (n = 19), lumbar sympathectomy (n = 6), conservative therapy (n = 65), and major amputation (n = 31). We also calculated P3 risk scores and measured transcutaneous oxygen pressure (tcPO2) and skin perfusion pressure (SPP) before and after therapy.
Results: The limb salvage rate was 87% at 2 years in the arterial reconstruction group. In the low-risk group (a P 3 risk score of 3), the 1-year amputation-free survival rate was 96%. In the medium-risk group (a P 3 risk score of 4–7), the 1-year amputation-free survival rate was 88%. In the high-risk group (a P 3 risk score of 8), the 1-year amputation-free survival rate was 66%. The hospital death rate in the arterial reconstruction group was 3.2%, all of whom were patients who underwent bypass. The survival rate at 5 years was 65% and 36% in the conservative therapy only group. Ulcers healed in 140 out of 144 patients. The 4 patients with unhealed infections had tcPO2 or SPP values of more than 30 mmHg after treatment. Major amputations were performed in 4 of 5 patients who had tcPO2 or SPP values from 20 to 30 mmHg after treatment. Major amputations were performed in all 6 patients who had tcPO2 or SPP values of less than 20 mmHg after treatment.
Conclusion: In cases with tcPO2 or SPP values of more than 30 mmHg, an ulcer will probably heal, except in infected cases. We suggest that, if these values are less than 30 mmHg, complete revascularization should be performed. The P3 risk score was useful in predicting limb salvage in the current series. Hybrid therapy in bypass and endovascular therapy must be performed in cases where patients are in a generally poor condition. It is important to attempt amelioration in limb salvage and to control the operative mortality rate with sufficient perioperative control. (English Translation of Jpn J Vasc Surg 2011;20:905–911)
Keywords: critical limb ischemia, hybrid therapy, transcutaneous oxygen pressure, skin perfusion pressure
Introduction
Due to an increase in patients with diabetic mellitus including those on dialysis in recent years, critical
limb ischemia associated with arteriosclerosis obliterans (ASO) has frequently been encountered. Since critical limb ischemia, if untreated, results in necrosis, the presence or absence of emergency and the degree of improvement after treatment should be objectively evaluated. In addition, since severe complications often develop, treatment with a consideration of the general condition is necessary. We evaluated patients with critical limb ischemia, who were encountered in our department, in terms of the transcutaneous oxygen pressure (tcPO2) and skin perfusion pressure (SPP) before and after treatment, and discussed treatment strategies based on results of various treatment methods.
Subjects and Methods
The subjects consisted of 292 patients with critical limb ischemia due to ASO who were encountered in our department from May 1995, when measurement of tcPO2 was initiated, to July 2009. Arterial reconstruction was performed in 190 patients. Conservative treatment was performed in 65 patients who refused surgery, involvement in clinical trials, or a poor general condition. Major amputation was performed in 31 patients because of necrosis that was already present at the time of the first consultation in our hospital, bed-confinement with systemic infection, or marked pain at rest. Lumbar sympathectomy was performed in 6 patients with ulceration in the lower limb in whom arterial reconstruction was impossible.
As arterial reconstruction, bypass was performed in 167 patients and endovascular treatment in 29, of whom 6 patients underwent hybrid treatment consisting of endovascular treatment and bypass, and 4 underwent hybrid treatment consisting of endovascular treatment and thromboendarterectomy (common femoral artery in all patients) (Table 1). Treatment results in these patients were evaluated.
Results
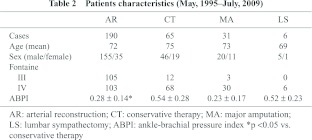
Concerning background factors, the mean age was 72 years in patients who underwent arterial reconstruction (AR group), 75 years in those who received conservative treatment (CT group), 73 years in those who underwent major amputation (MA group), and 69 years in those who underwent lumbar sympathectomy (LS group). The CT group was the oldest. The mean ankle-brachial pressure index (ABPI) was 0.28 ± 0.14 in the AR group, 0.54 ± 0.28 in the CT group, 0.23 ± 0.17 in the MA group, and 0.52 ± 0.23 in the LS group, being the highest in the CT group. The ABPI in the AR group was significantly lower than that in the CT group (Table 2).
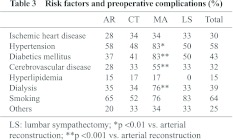
Concerning risk factors for atherosclerosis and complications in all patients, smoking was observed in 64%, hypertension in 58%, diabetes mellitus in 43%, dialysis in 39%, cerebrovascular disease in 32%, ischemic heart disease in 30%, hyperlipidemia in 15%, and others in 25%. The MA group showed significantly higher incidences of hypertension (83%), diabetes mellitus (83%), cerebrovascular disease (55%), and chronic renal failure (76%) than did the AR group (Table 3).
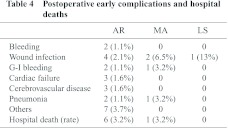
As postoperative complications, bleeding, wound infection, cerebrovascular disease, and pneumonia were observed in the AR group. The hospital death rate due to these complications was 3.2% in both the AR and MA groups (Table 4).
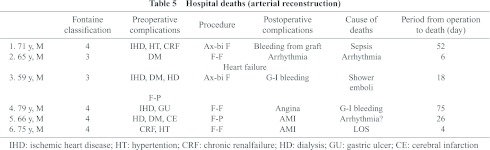
The 6 patients who died in the hospital in the AR group had diabetes mellitus or chronic renal failure complicated by dialysis or ischemic heart disease. Bypass was performed in all patients, and non-anatomical bypass was performed in the aortoiliac area. They died of sepsis, arrhythmia, or myocardial infarction (Table 5).
The primary cumulative patency rate for femoropopliteal, femorotibial, and popliteotibial bypasses was 75% at 5 years and 75% at 10 years.
The limb salvage rate was 90% at 1 year and 87% at 2 years.
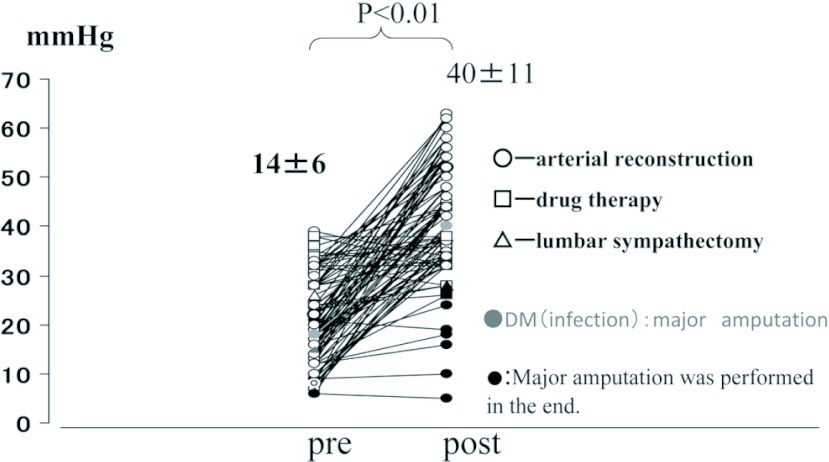
In patients with ulcer, tcPO2 values, before and about 1 month after treatment, are shown in Fig. 1. Open circles indicate the AR group, open triangles indicate drug therapy. Open triangles represent the LS group, and closed circles represent the MA group. In 6 patients with a tcPO2 ≤20 mmHg after treatment, the ulcer did not heal, and major amputation was performed. Of 5 patients with a tcPO2 of 20 mmHg–30 mmHg after treatment, 4 similarly underwent major amputation. Two patients with diabetes mellitus showing an increase to 30 mmHg after treatment underwent amputation.
Fig. 1.
TcPO2 before and after therapy in patients with ulcer.
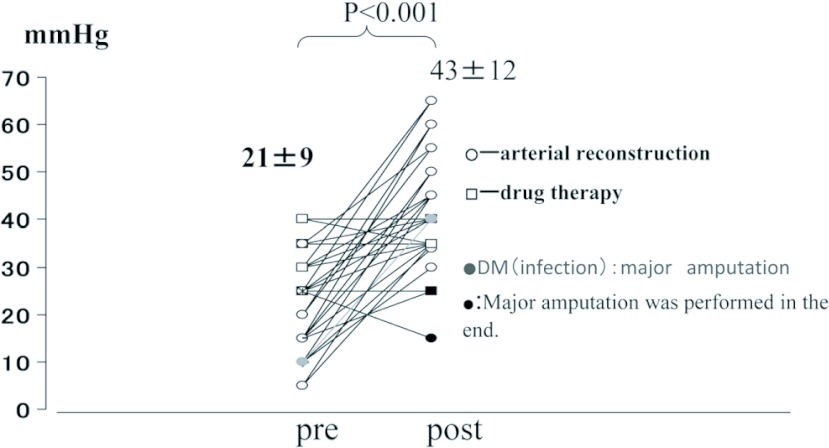
In patients with ulcer, SPP values, before and 1 month after treatment, are shown in Fig. 2. All 3 patients with an SPP ≤25 mmHg after treatment underwent major amputation while 2 patients with an SPP 30 mmHg after treatment underwent major resection, and both of them had diabetes mellitus.
Fig. 2.
SPP before and after therapy in patients with ulcer.
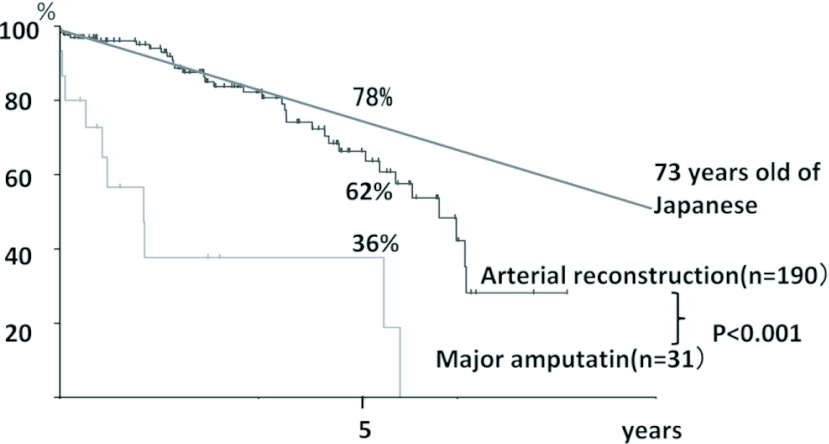
The 5-year cumulative survival rate was 62% in the AR group and 36% in the MA group, being significantly lower in the latter (Fig. 3).
Fig. 3.
Cumulative survival rates.
In the AR group, the 1-, 3-, and 5-year survival rates were 94, 80, and 67%, respectively, in non-dialysis patients and 81, 49, and 49%, respectively, in the dialysis patients, being significantly lower in the latter.
Discussion
As shown in the TASC II,1) the treatment principle for critical limb ischemia is surgical arterial reconstruction such as by bypass without endovascular treatment. However, the treatment principle should be determined by comprehensive evaluation of the general condition, limb salvage rate, predicted survival, and the site and range of the lesion.
According to the TASC II classification, indications of endovascular treatment in our department are A, B, C type iliac artery lesions, A and B type femoropopliteal lesions, and localized crural artery lesions (≤5 cm) accompanied by a poor general condition.
In our department, the limb salvage rate 1 year after arterial reconstruction including endovascular treatment was 90%. Schanzer, et al.2) developed the prevent III risk score for critical limb ischemia treated by infrainguinal bypass surgery, and showed 1-year amputation-free survival rates according to this score.
In their scoring system, 4 points were given to dialysis, 3 points to tissue loss, 2 points to age 75 years, and 1 point to coronary artery disease. The 1-year amputation-free survival rate was 86% for scores ≤3 (low risk), 74% for scores of 4–7 (medium risk), and 56% for scores 8 (high risk), which suggested the usefulness of this scoring system for the prediction of amputation-free survival. Using this prevent III risk score, the 1-year amputation-free survival rate in out department was 96% in the low-risk group, 88% in the medium-risk group, and 66% in the high-risk group. Despite higher amputation-free survival rates in our department, our results were similar to those reported by Schanzer showing the usefulness of this evaluation method.
In our department, the hospital death rate in the AR group was 3.2%, and the operative death (death within 30 days after operation) rate was 2.1%. Although direct comparison between our study and other studies is difficult due to differences in patients’ background factors, the BASIL trial3) showed an operative death rate of 3% for endovascular treatment and 5.8% for the bypass operation. Concerning ankle bypass, the operative death rate was reported to be 1.2% by Kalra, et al.4) and 0.9% by Pomposelli, et al.5) In our department, all operative deaths were observed in patients who underwent bypass under general anesthesia involving a risk. Therefore, in recent years, we have reinforced cooperation with the Department of Anesthesiology so that surgery can be performed using femoral or sciatic nerve block without general anesthesia.
The survival rate was significantly lower in dialysis patients than in non-dialysis patients. Goodney, et al.6) evaluated risk factors for deaths within 1 year after lower limb bypass surgery, and reported that the emergency operation is the most important risk factor, followed in order by dialysis dependence, age over 80 years, lack of single-segment saphenous vein, critical limb ischemia, diabetes mellitus, and congestive heart failure. The 1-year survival rate was 72% in the presence of 3 or more risk factors and 97% in the absence of risk factors, suggesting the usefulness of these risk factors for the prediction of 1-year survival. The BASIL trial,3) which compared the results of infrainguinal bypass surgery and those of endovascular treatment in patients with critical limb ischemia, showed that endovascular treatment is as effective as bypass as early stage treatment, and particularly, should be the first choice in patients with a poor general condition who are expected to survive less than 2 years, but the limb salvage rate and survival rate are lower for endovascular treatment in patients who are likely to survive 2 years or more. Therefore, predicted survival should be objectively evaluated, and less invasive methods such as endovascular treatment should be selected when the predicted survival is short. Azuma, et al.7) described that bypass should be the first choice when the patient’s general condition is favorable and there is a good autologous vein.
Therefore, recently, utilizing the characteristics of both methods, we have used hybrid treatment that can be performed at a time, reducing patient’s burden. Hybrid treatment consisting of endovascular treatment and bypass is particularly indicated, for example, when endovascular treatment of the superficial femoral artery and bypass for crural lesions are performed in the absence of long good autologous veins for lesions extending from the thigh to the crural artery. Hybrid treatment consisting of thromboendarterectomy and endovascular treatment is useful for complex lesions involving the common femoral artery since thromboendarterectomy can be performed under local anesthesia for the common femoral artery for which stents cannot be used, allowing arterial puncture on both the central and peripheral sides under direction vision.
As objective evaluation methods, we have measured tcPO2 and SPP.8) In this study, these pressures were measured before and after treatment, and ulcer healed in patients showing a tcPO2 or SPP 30 mmHg after treatment except those with infection. When either pressure is <30 mmHg, efforts to add arterial reconstruction should be made. After surgery or treatment, these pressures should be measured using devices. In patients in whom endovascular treatment or bypass is impossible, there is no alternative but to perform conservative treatment methods. Among such methods, angiogenic therapy has actively been performed in recent years.9–11) However, considering the time until its effects are obtained, this method may be also indicated in patients with a tcPO2 or SPP of 20 mmHg–30 mmHg.
In all patients who developed infection, diabetes mellitus was present, infection spread along the tendon, and resulting sepsis required major amputation. Such patients cannot be the subjects of the evaluation of blood flow such as tcPO2 or SPP. For such infection in diabetic limbs, Mitsui, et al.12) reported the usefulness of Maggot therapy. They describe that this therapy should be selected after arterial reconstruction since this therapy is not effective when blood flow is poor.
As bypass materials, when no autologous vein is available, vascular grafts are used. For grafting, adequate preparation to prevent graft infection is necessary. In particular, since patients with diabetes mellitus and those on dialysis are susceptible to infection, careful attention is necessary. Eguchi, et al.13) performed disinfection of the operative field on day 3 before operation in 378 patients undergoing cardiovascular surgery, and observed no infection in the operation area in any patient. Yamashita, et al.14) applied Isodine and gauze with Isodine gel to the planned incision site of the inguinal area, removed this gauze on the day before operation, and after careful bathing, applied this gauze again, and observed no infection at the operation area. Six years earlier, we had also applied gauze with Isodine gel after bathing on the day before the operation, and had observed only 1 patient with infection at the operation site.
Thus, critical limb ischemia is associated with various complications. Not only simple arterial reconstruction but also treatment considering the general condition is necessary.
Conclusions
When the tcPO2 or SPP is 30 mmHg after treatment, ulcer generally heals in patients without infection. When it is <30 mmHg, artery reconstruction is added.
The prevent III risk score is useful for predicting limb salvage.
In patients with a poor general condition, it is important to perform endovascular treatment or its hybrid treatment when possible, and adequate perioperative management and efforts to improve the limb amputation and operative death rates are necessary.
Disclosure Statement
The authors have no potential conflict of interest to be disclosure.
References
- Norgan I, Hiatt WR, Dormandy JA, et al. Inter-society Consensus for the Management of Peripheral Arterial Disease (TASC II). Euro J Vasc Endovasc Surg 2007; 33: S1–75 [DOI] [PubMed] [Google Scholar]
- Schanzer A, Goodney PP, Li Y, et al. Validation of the PIII CLI risk score for the prediction of amputation-free survival in patients undergoing infrainguinal autogenous vein bypass for critical limb ischemia. J Vasc Surg 2009; 50: 769–75 [DOI] [PubMed] [Google Scholar]
- Adam DJ, Beard JD, Cleveland T, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 2005; 366: 1925–34 [DOI] [PubMed] [Google Scholar]
- Kalra M, Gloviczki P, Bower TC, et al. Limb salvage after successful pedal bypass grafting is associated with improved long-term survival. J Vasc Surg 2001; 33: 6–16 [DOI] [PubMed] [Google Scholar]
- Pomposelli FB, Kansal N, Hamdan AD, et al. A decade of experience with dorsalis pedis artery bypass: analysis of outcome in more than 1000 cases. J Vasc Surg 2003; 37: 307–15 [DOI] [PubMed] [Google Scholar]
- Goodney PP, Nolan BW, Schanzer A, et al. Factors associated with death 1 year after lower extremity bypass in Northern New England. J Vasc Surg 2010; 51: 71–8 [DOI] [PubMed] [Google Scholar]
- Azuma N. Role of bypass surgery in crural arterial occlusive lesions. Nihon Geka Gakkai Zasshi 2010; 111: 97–101 [PubMed] [Google Scholar]
- Masaki H, Ishida A, Tabuchi A, et al. Evaluation of critical limb ischemia by transcutaneous oxygen pressure and skin perfusion pressure measurement. Jpn J Vasc Surg 2005; 14: 577–82 [Google Scholar]
- Makiho H, Morishita R. Progress and Prospects of Therapeutic Angiogenesis Using HGF Plasmid Gene Therapy for Peripheral Arterial Disease. J Jpn Coll Angiol 2007; 47: 187–93 [Google Scholar]
- Yukihito H. Therapeutic Angiogenesis with Autologous Bone-marrow Mononuclear Cell Implantation. J Jpn Coll Angiol 2007; 47: 195–200 [Google Scholar]
- Kawamoto A, Asahara T. Transplantation of Endothelial Progenitor Cells for Vascular Regeneration. J Jpn Col Angiol 2007; 47: 201–7 [Google Scholar]
- Mitsui H, Kawabata T, Kuroko Y, et al. Maggot debridement therapy for diabetic foot: the first in Japan. J Jpn Coll Angiol 2005; 45: 443–50 [Google Scholar]
- Eguchi S, Saito H, Kansaku R, et al. Prevention of Surgical Site Infection in Cardiovascular Surgery by a 3 Preoperative Days Skin Disinfectant Preparation. Jpn J Vasc Surg 2008; 17: 611–4 [Google Scholar]
- Yamashita H, Nagao K, Matsuda M, et al. Pasting of Povidone-Iodine Gel Gauze for Prevention of Prosthetic Graft Infection. Jpn J Vasc Surg 1999; 8: 425–30 [Google Scholar]