Abstract
Background: The ankle-brachial pressure index (ABI) is widely used as a standard screening method for arterial occlusive lesion above the knee. However, the sensitivity of ABI is low in hemodialysis (HD) patients. Exercise stress (Ex-ABI) may reduce the false negative results.
Patients and Methods: After measuring resting ABI and toe-brachial pressure index (TBI), ankle pressure and ABI immediately after walking (Post-AP, Post-ABI) were measured using one-minute treadmill walking in 52 lower limbs of 26 HD patients. The definition of peripheral arterial occlusive disease (PAD) required an ABI value of less than 0.90, TBI value of less than 0.60, and decrease of more than 15% of the Post-ABI value and 20 mmHg of Post-AP in Ex-ABI. Computed tomographic angiography (CTA) was performed in 32 lower limbs of 16 HD patients. PAD is defined as presence of stenosis of more than 75% in the case of lesions from an iliac artery to knee on CTA.
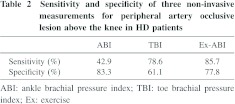
Results: The accuracy of Ex-ABI (Sensitivity, 85.7%; Specificity, 77.7%) was higher than those of ABI (Sensitivity, 42.9%; Specificity, 83.3%) or TBI (Sensitivity, 78.6%; Specificity, 61.1%).
Conclusion: Ex-ABI with one-minute treadmill walking is the most useful tool for the screening of arterial occlusive lesions above the knee in maintenance HD patients.
Keywords: peripheral arterial disease, exercise, diagnosis, screening, hemodialysis
Introduction
Patients undergoing hemodialysis (HD) are likely to develop peripheral arterial occlusive disease (PAD) due to complicated causation. PAD in HD patients is characterized by diffuse stenotic lesions below the knee. However, one-third of HD patients with lesions below the knee also have stenotic lesions above the knee1) and their presence accelerates progress to critical limb ischemia (CLI). Early detection of PAD is the most important factor for the management of CLI in HD patients and various examinations are performed for this purpose. Generally, skin perfusion pressure (SPP) is useful for the evaluation of microangiopathy below the knee or ankle.1) On the other hand, ankle-brachial pressure index (ABI) is widely used as a standard screening method for macroangiopathy above the knee. However, in HD patients, false negative results due to medial arterial calcification have been reported, which is problematic.2 3) With this background in mind, the toe-brachial pressure index (TBI), which circumvents the effects of calcification, is recommended as a screening method. However, the sensitivity of ABI for PAD can be improved by inducing ischemia of the lower limbs with an exercise (Ex-ABI),4,5) and this method may reduce the false negative results that are unclear. The purpose of this study was to compare ExABI with conventional ABI and TBI in HD patients and clarify its usefulness.
Patients and Methods
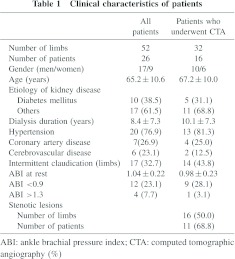
Subjects included 26 ambulatory HD patients (17 men, 9 women) with a mean age of 65.2 ± 10.6 years (range, 52 to 82 years). Patients were excluded if they had a previous history of amputation. Ten patients with diabetes mellitus and 11 patients (17 limbs) with intermittent claudication were included (Table 1). Medication was prescribed as clinically indicated in this study. This study was carefully scrutinized beforehand by an Ethics Committee in our hospital and all patients gave informed consent before their examination.
We performed 3 kinds of non-invasive measurements (ABI, TBI and Ex-ABI) in all HD patients. ABI and TBI were measured in 52 limbs that simultaneously measured unilateral brachial pressure in the arm without an arteriovenous fistula, ankle blood pressure (AP), and great toe blood pressure by using an oscillometric method (ABI-form first, Colin, Tokyo, Japan) after bed rest for 15 minute on a non-HD day. ABI and TBI were calculated as the ratio ankle and great toe systolic pressure divided by brachial systolic pressure. After measuring resting ABI and TBI, AP and ABI were measured immediately post-walking (Post-AP and Post-ABI) using the computerized treadmill system (CASE 12, Marquette Electronics, Milwaukee, WI, USA) following a protocol. Each patient’s 12-lead electrocardiogram and heart rate were monitored throughout the walking protocol for one minute (2.4 km/h, 12%). However, the walking speed was reduced to 2.0 km/h when the patient was more than 70 years old or was a low left ventricular function case.6,7) The supervising physician could stop the walking protocol based on the following criteria:
(1) the development of significant symptoms such as chest pain or dizziness;
(2) marked systolic hypotension or hypertension (more than 250/120 mmHg or a decrease in systolic blood pressure or HR in spite of increasing workload);
(3) the development of dangerous or potentially dangerous arrhythmias; and
(4) ST-segment deviations (horizontal or a downsloping depression of more than 80 ms from the J point) or elevation.
Room temperature was set at 25~C.
The definition of PAD required an ABI value of less than 0.90, TBI value of less than 0.60, and decrease more than 15% of the Post-ABI value8) and 20 mmHg of Post-AP9) in Ex-ABI. However, the result of Ex-ABI was judged to be test negative when the Post-AP was more than 120 mmHg.
Computed tomographic angiography (CTA) was performed in 16 patients (32 limbs) who gave informed consent on a non-HD day. To study the sensitivity and specificity of various measurements (ABI, TBI and Ex-ABI), PAD is defined as the presence of stenosis of more than 75% in the case of lesions from an iliac artery to knee on CTA (PAD-AK). CTA was performed with a 16-detector-row CT scanner (Aquilion16; Toshiba Medical, Tokyo, Japan). The scanning range was planned with a scout view and included the entire vascular tree from the abdominal aorta to ankles. A total of 100 mL of contrast media (Proscope 300, Tokyo, Japan) was administered with an automated injector (Stellant; Medrad, Pennsylvania, USA) at a flow rate of 3 mL/sec through a 16 to 22-G needle that was placed in a superficial vein or blood access.
The presence of intermittent claudication was determined by walking impairment questionnaire.10,11) Hypertension was diagnosed when a study subject had received medical treatment for hypertension. Coronary artery disease was defined as a previous history of angina pectoris or myocardial infarction. Cerebrovascular disease was defined as a previous history of clinical cerebral infarction or hemorrhage.
Data are presented as mean ±SD. A paired t-test was used for between before and after one-minute treadmill walking comparisons. Comparison of test positive rate between 3 measurements was performed using chi-square test in 3 × 2 tables. Significance was defined as P less than 0.05. All statistical analyses were performed using commercially available statistical software (StatMate III Ver.3.16, ATMS, Tokyo, Japan).
Results
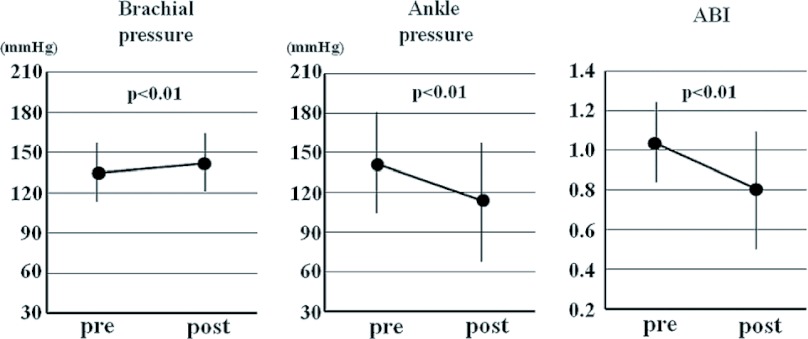
The mean ABI and TBI at rest were 1.04 ± 0.22 and 0.61 ±0.22, respectively. All HD patients were performed Ex-ABI using one-minute treadmill walking. In the Ex-ABI, though brachial pressure increased significantly (7.0± 16.0 mmHg, p <0.01), Post-AP decreased significantly (−26.6 ± 31.0 mmHg, p <0.01). As a result, Post-ABI decreased significantly (−25.3 ± 21.9%, p <0.01) (Fig. 1).
Fig. 1.
Changes of brachial, ankle pressure and ankle-brachial pressure index (ABI) between pre and post one-minute treadmill walking in HD patients.
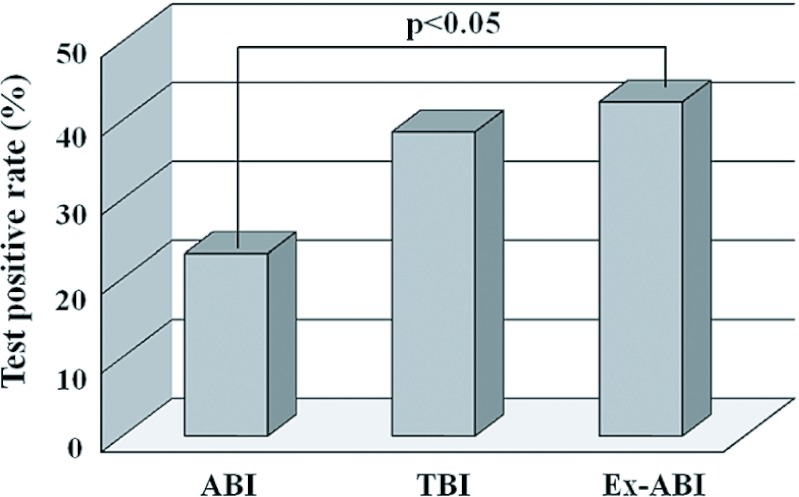
In test positive rate, though TBI (38.5%) was no significant difference compared with ABI (23.1%), ExABI (42.3%) was higher than ABI (p <0.05) (Fig. 2).
Fig. 2.
Test positive rates on 3 non-invasive measurements (ABI, TBI and Ex-ABI) in HD patients.
Of 26 HD patients, 16 patients gave informed consent. Basic characteristics of the 16 patients who underwent CTA are listed (Table 1). Nine of 32 limbs examined showed an ABI of less than 0.9. The sensitivity of ABI set at 0.9 for detecting PAD-AK was only 42.9%, although the specificity was 83.3% (positive predictive value, 66.7%; negative predictive value, 66.5%). Eighteen of 32 limbs examined showed TBI of less than 0.6. The sensitivity of TBI set at 0.6 for detecting PAD-AK was 78.6%, and specificity was 61.1% (positive predictive value, 61.1%; negative predictive value, 78.6%). Sixteen of 32 limbs examined showed positive finding in Ex-ABI. The sensitivity of Post-ABI set at −15% and Post-AP set at −20 mmHg for detecting PAD-AK was 85.7%, and the specificity was 77.8% (positive predictive value, 75.0%; negative predictive value, 87.5%) (Table 2).
Discussion
In Japan, standard Ex-ABI testing involves walking on a treadmill inclined by 12% at a speed of 2.4 km/hr for 5 minutes.12) However, Ohta, et al.13) and Sugimoto et al.14) proposed to shorten the duration of walking from 5 to one minute. An advantage of this proposal is that Ex-ABI can be determined to detect PAD safely with a low exercise load in patients with heart disease or elderly patients with reduced exercise tolerance, while maintaining high diagnostic accuracy7) with a sensitivity of 78.8% and specificity of 93.8%.6) In this study, macroangiopathy in the lower limbs of HD patients were evaluated by Ex-ABI with one-minute treadmill walking for the first time.
In healthy individuals, the blood flow demand of lower limb skeletal muscles due to walking was met by increasing cardiac output and blood distribution to the skeletal muscles. At this time, as Post-AP increased simultaneously with brachial pressure, no change was measured in Post-ABI. However, in HD patients in this study, brachial pressure increased after walking, but Post-AP and ABI markedly decreased. These decreases in Post-AP and ABI are suggested to occur as blood in the skeletal muscles rapidly returns through veins to the right atrium by a milking action during walking, but the arterial blood supply is insufficient to balance this venous return and fails to fill the arteries. Therefore, decreases in Post-AP and ABI strongly suggest the presence of a stenotic lesion in the lumen of a lower limb artery, causing a decrease in the blood flow reserve to areas below the lesion.
Generally, ABI is widely used for the evaluation of blood flow reserve in PAD not only in HD patients, but also all patients, because of the high diagnostic accuracy with a specificity of 100% and maximum sensitivity of 95%.15) In HD patients, however, it has been reported that the sensitivity of an ABI less than 0.9 was very low at 29%, while the specificity was 100% for the detection of PAD.1,3) This is primarily due to medial arterial calcification, which causes deviations in the normal value of ABI to the right. According to our study, more abnormal findings could be induced by the Ex-ABI than ABI. Priority should be placed on high sensitivity for screening. Therefore, Ex-ABI is considered to be a better screening test than ABI for the detection of PAD-AK.
TBI is the brachial pressure divided by the great toe pressure and can be used as an index of lower limb macroangiopathy similarly to ABI. Since calcification rarely extends to toe arteries, TBI has been suggested to be a substitute for ABI in HD patients. According to our study, more abnormal findings could be observed by Ex-ABI than by TBI. This result suggests that PAD can be detected earlier using Ex-ABI, which is less affected by medial arterial calcification, than by ABI or TBI.
In HD patients, positive findings could be more readily detected using Ex-ABI than ABI or TBI. However, the percentage of false-positive results in positive results should be clarified. Although Ex-ABI after one-minute exercise has a high diagnostic accuracy in non-HD patients,6) it is unclear whether this tool can be directly applied to HD patients. We performed CTA in the subjects whenever possible, and compared the findings with the diagnostic results of the 3 measurements. As a result, the sensitivity and specificity of Ex-ABI were higher than those of ABI or TBI.
SPP is the most useful for evaluating below the knee or ankle microangiopathy.1) For the evaluation of above the knee stenotic lesions, ABI is considered to be useful, but its sensitivity has been reported to be low in HD patients.2,3) In this study, Ex-ABI in HD patients overcame this problem of ABI on screening for above the knee stenotic lesions by increasing the positive result rate and reducing the false-positive rate.
Study Limitations
With CTA, it is difficult to visualize lumens with blood flow within severe calcification lesions. In addition, the possibility that patients with multi-vessel occlusive lesions below the knee affected the diagnostic accuracy of each measurement cannot be excluded.
Conclusion
Ex-ABI with one-minute treadmill walking is most useful tool for a screening of arterial occlusive lesion above the knee in maintenance HD patients.
Acknowledgment
The authors thank Mrs Yukiyo Ishiwata, Tomoko Okada and Miss Takako Sakamoto, Ayaka Inai for technical support.
Diclosure Statement
The authors declare that they have no competing interests.
References
- Okamoto K, Oka M, Maesato K, et al. Peripheral arterial occlusive disease is more prevalent in patients with hemodialysis: comparison with the findings of multidetector-row computed tomography. Am J Kidney Dis 2006; 48: 269–76 [DOI] [PubMed] [Google Scholar]
- Leskinen Y, Salenius JP, Lehtimäki T, et al. The prevalence of peripheral arterial disease and medial arterial calcification in patients with chronic renal failure: requirements for diagnostics. Am J Kidney Dis 2002; 40: 472–9 [DOI] [PubMed] [Google Scholar]
- Okamoto K, Oka M, Maesato K, et al. Non-invasive diagnostic modality for peripheral arterial occlusive disease in hemodialysis patients. J Jpn Coll Angiol 2006; 46: 829–35 [Google Scholar]
- Fabry R, Dubost JJ, Pochon P, et al. Comparison of standard one-minute treadmill exercise and strandness test (absolute walking distance) in relation to site of lesion, walking distance, and diastolic blood flow velocity (Doppler curves). Angiology 1990; 41: 869–76 [DOI] [PubMed] [Google Scholar]
- Laing SP, Greenhalgh RM. Standard exercise test to assess peripheral arterial disease. Br Med J 1980; 280: 13–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuyuki K, Kohno K, Ebine K, et al. Accuracy of one minute walking on treadmill exercise test using automatic measurements of ankle-brachial pressure index. J Jpn Coll Angiol 2012; 52: 175–9 [Google Scholar]
- Watanabe S, Tsuyuki K, Sakamoto T, et al. Safty of exercise-ankle brachial pressure index in patients with cardiovascular disease: Comparison of standard method and one minute method. Rehab sports 2011; 30: 2–5 (in Japanese) [Google Scholar]
- TASC II Working Group: Intermittent claudication Inter-society consensus for the management of peripheral arterial disease (TASC II), Tokyo, Medical tribune, 2009; 37–49 (JCA printed in Japan) [Google Scholar]
- Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg 1997; 26: 517–38 [DOI] [PubMed] [Google Scholar]
- Regensteiner JG, Steiner JF, Panzer RJ, et al. Evaluation of walking impairment by questionnaire in patients with peripheral arterial disease. J Vasc Med Biol 1990; 2: 142–52 [Google Scholar]
- Hiatt WR, Hirsch AT, Regensteiner JG, et al. Clinical trials for claudication. Assessment of exercise performance, functional status, and clinical end points. Vascular Clinical Trialists. Circulation 1995; 92: 614–21 [DOI] [PubMed] [Google Scholar]
- Fujioka K, Esato K, Nakajima N, et al. An objective assessment for claudications on drug using treadmill test and near-infrared spectroscopy. J Jpn Coll Angiol 2000; 40: 851–7 [Google Scholar]
- Ohota T, Sugimoto I, Hida K, et al. The prediction of the effects of exercise training in patients with intermittent claudication. Jpn J Vasc Surg 1998; 7: 455–60 [Google Scholar]
- Sugimoto I, Ohota T, Katoh R, et al. Quantitative evaluation of claudicatory limbs: Recovery process in the ankle pressure index following walking tolerance test. J Jpn Coll Angiol 1992; 32: 729–35 [Google Scholar]
- Bernstein EF, Fronek A. Current status of noninvasive tests in the diagnosis of peripheral arterial disease. Surg Clin Noth Am 1982; 62: 473–87 [DOI] [PubMed] [Google Scholar]