Abstract
Objectives: Thoracic outlet syndrome (TOS) consists of a group of distinct disorders that are caused by compression of the brachial plexus and/or subclavian artery and vein. The aim of this study was to highlight the different modalities of diagnosing and treating vascular TOS and evaluate outcomes.
Methods: We conducted a retrospective cohort study between 1999 and 2011 using the medical records database from a teaching hospital.
Results: During the study period, 54 cases with vascular TOS were identified in 38 patients. Bilateral TOS was in 16 patients. The median age of the patients was 33 years (range 12–49), and the majority (79%) were female. Arterial TOS represented forty-nine cases (90.7%). Preoperative information derived from plain x-ray, duplex scanning and in selected cases computed tomography (CT) and/or angiography. Decompression of the TOS was performed through a supraclavicular approach in all cases with scalenectomy coupled with either cervical rib excision (70%), 1st rib excision alone (15%) and excision of both cervical and 1st ribs (15%). Adjunctive vascular reconstructive procedures were done in 11 cases (20.3%); 9 arterial cases and 2 venous cases. There was no mortality; however, postoperative complications occurred in 7 cases (13%).
Conclusion: The use of advanced radiological imaging and careful surgical planning for Vascular TOS in a high volume center resulted in good outcomes.
Keywords: thoracic outlet syndrome, subclavian artery, subclavian vein
Introduction
Thoracic outlet syndrome (TOS) refers to compression of the neurovascular structures as they course through the narrow passageway from the base of the neck into the arm via the axilla resulting in injury or irritation of neurovascular structures, which may cause group of neurological and/or vascular symptoms and signs. The most important narrow passageway in this area anatomically is the scalene triangle, which is bounded by the anterior and middle scalene muscles with the 1st rib forming the base. These muscles can be further hypertrophied after repetitive motion and create more compression. Although the narrowing of this area can be further constricted by other structures such as congenital cervical ribs, which have an incidence rate of 1%,1) fibrous bands and anomalous muscles may be a more common cause of narrowing.
The true prevalence and incidence of TOS are not known, but the reported prevalence ranges from 3 to 80 cases per 1000, and it is more commonly observed in women with a peak of onset in the 4th decade of life.2) TOS is classified into three distinct subtypes based on the involved structure: neurogenic, venous, and arterial; symptoms of each subtype are produced relative to which of the neurovascular structures is compressed in the thoracic outlet. The majority of TOS are neurogenic and vascular TOS accounts for only 5%, and only 1% are arterial.1)
Treatment of TOS can be either conservative or surgical. The goal of the surgical option is to relieve the compression over the neurovascular structures as well as reconstruct any involved vessel. Although conservative management is still recommended for neurogenic cases, surgical intervention provides good and fast results in vascular TOS, and the majority of these patients appear to benefit from surgery, mainly patients with arterial TOS. The aim of this study was to highlight the different modalities for diagnosing and treating vascular TOS and to evaluate the outcomes at King Khalid University Hospital in Riyadh, Saudi Arabia.
Methods
We conducted a retrospective cohort study using a prospectively collected vascular surgery procedures database at the division of vascular surgery, King Khalid University Hospital, Riyadh, Saudi Arabia. All consecutive patients who underwent surgical decompression for vascular thoracic outlet syndrome from January 1999 to December 2011 were included. Demographic data, clinical presentation, investigations that include radiological imaging, procedures, pathological results, complications and follow-up for all patients were collected and analyzed. Success was defined as complete relief of vascular symptoms postoperatively and reconstructing the vascular damage.
This study was approved by King Khalid University Hospital Ethics Review Board, Riyadh, Saudi Arabia as part of the clinical vascular database for vascular surgery procedures.
The numbers of specified events are expressed as percentages. Median with interquartile range was used for age and follow-up period.
Results
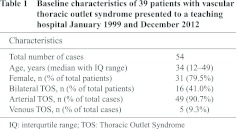
During the study period, 54 cases with vascular TOS were identified in 38 patients. Sixteen patients had bilateral TOS. The median age of the patients was 34 years (range 12–49), and the majority (79.5%) were female. Arterial TOS represented forty-nine cases (90.7%), whereas only five (9.3%) were venous TOS (Table 1).
The clinical presentation was predominantly arterial in forty-nine cases (90.7%). Arm claudication, coldness, pallor and other symptoms of chronic upper limb ischemia were the main complaints of arterial TOS patients. Five cases (9.3%) presented with critical upper limb ischemia in the form of digital gangrene and rest pain of the hand. The five venous cases presented with arm swelling and congestion consistent with venous compression. All of the venous cases were diagnosed in young athletes male. Two cases had acute onset of swelling and was diagnosed with acute deep vein thrombosis in the subclavian and axillary veins.
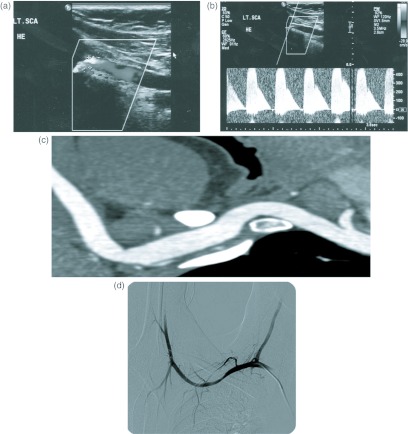
All patients had a thoracic inlet plain x-ray as a first part of the investigation protocol in our vascular center. This type of imaging study can provide useful information in the diagnosis of TOS, such as the identification of bony abnormalities including cervical ribs, prominent C7 transverse processes, anomalous first rib or other bony abnormalities. A cervical rib was detected in 46 cases (85%) as well as prominent C7 transverse processes in two cases. Anomalous first rib was detected in 8 cases (15%). Doppler ultrasound is the second line non-invasive investigation for all TOS patients in our protocol and it is considered the first diagnostic test for vascular TOS. The diagnosis of either arterial or venous TOS was confirmed in all 54 cases (100%) by stress and non-stress duplex (Fig. 1A and 1B). Duplex has been helpful as well in detecting associated vascular abnormalities such as post-stenotic subclavian artery aneurysms and arterial thrombosis. Conventional arteriography and computed tomography (CT) angiography were used as a secondary confirmatory exam and to provide more vascular complication details. During the study period, classic conventional angiography was performed in 10 (18.5%) cases with the arms in adduction and abduction, and 40 cases (74%) underwent CT angiography (Fig. 1C and 1D). Positive findings of vascular compression or occlusion were found in all cases, and post-stenotic subclavian artery aneurysm was confirmed in three patients as well as distal thrombosis in four patients. Selection of either conventional angiography or CT angiography was dependent on surgeon preference; however, since February 2006, CT angiography was used only as a second diagnostic exam aside from duplex for all TOS patients in our centre.
Fig. 1.
Different radiological modalities used to diagnose and plan the management of thoracic outlet syndrome: (A) and (B) Arterial duplex study showing the compressed left subclavian artery with hyperabduction. (C) Reconstructive computed tomography (CT) angiography showing compression of the right subclavian artery between the cervical rib and first rib. (D) Conventional arteriogram for a right subclavian artery showing stenosis of the artery with hyperabduction.
Decompression of the TOS was performed through a supraclavicular approach in all cases. Scalenectomy was performed for all 54 cases, and the pathological results showed that all excised muscles were showing hypertro phied features. Out of those 54 cases, forty six (85%) cases had undergone cervical rib removal, either alone in 38 cases (70%) or with 1st rib in 8 cases (15%), and eight cases (15%) underwent first rib resection only; these include the 2 cases with elongated C7 transverse processes that were found to be associated with ligaments from the transverse process to the first rib.
Adjunctive vascular reconstructive procedures were required in 11 cases (18.5%), nine arterial and two venous cases.
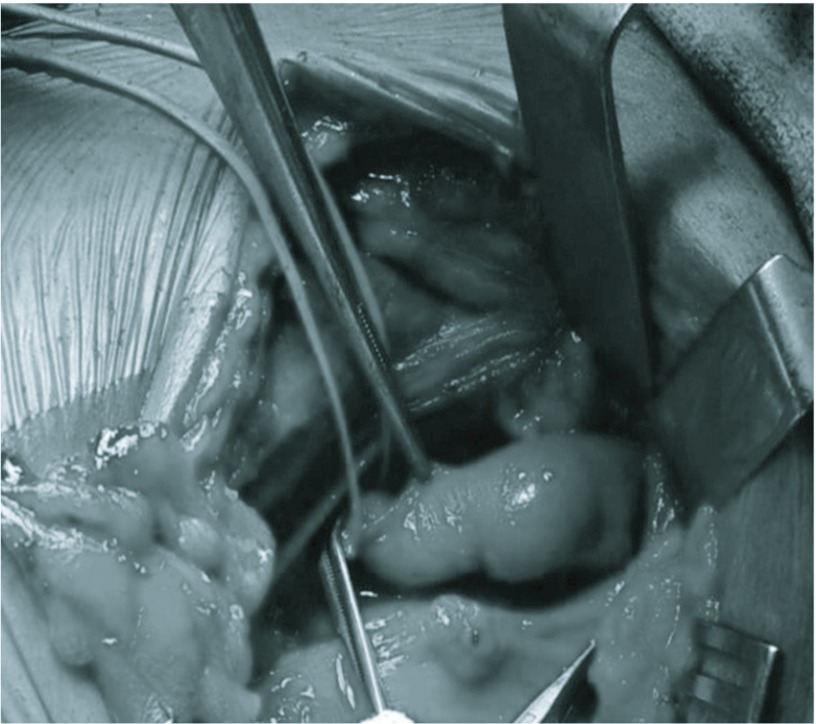
Repair of subclavian artery aneurysms (Fig. 2) were required in five cases (9.3%); resection and interposition graft was performed in 4 cases (3 cases with vein interposition graft and one case with synthetic interposition graft) and resection with end-to-end anastomosis was performed in one case. Revascularization of the upper limb was required in 4 cases (7.4%). Axillary-brachial bypass in one patient and axillary and distal thrombectomy was performed in three cases.
Fig. 2.
Intra-operative image of a supraclavicular incision after decompression of the right thoracic outlet showing the exposed right subclavian artery with an aneurysm.
Thrombolysis with stenting for subclavian vein was performed in the two cases that were presented with acute deep-vein thrombosis (DVT) prior to decompression of the thoracic outlet.
There was no postoperative mortality. Patients were followed up during the postoperative period with clinical examination and a duplex scan by vascular surgery team. The median follow-up period was 18 months (range 4–36 months). Complete relief of vascular symptoms postoperatively has been achieved in all patients immediately or gradually during follow-up, and no recurrence of the symptoms was observed.
Six patients had postoperative complications, one patient developed wound hematoma that was treated conservatively, and four patients had a transient neurological deficit in the form of hand numbness and weakness; however, all of them made a complete recovery with physiotherapy in 1 to 3 months period. Also, another patient had a thoracic duct injury which was managed conservatively for 1 month with full recovery.
Discussion
Galen and Vesalius were the first to describe the cervical rib in human dissections around 150 AD and Coot was the first to perform a decompressive operation, in which a cervical rib was removed from a young woman with improvement in the wrist pulse in 1861.3,4) The term “thoracic outlet syndrome” was first described in 1956 by Peet and his colleagues where they described a group of neurological and vascular symptoms and signs secondary to compression of neurovascular structures as they course through the narrow passageway from the base of the neck into the arm via the axilla resulting in injury or irritation of neurovascular structures.5)
Since that time, many reports have been published describing different presentations, diagnostic modalities, treatment strategies and different surgical approaches to alleviate the symptoms of TOS by relieving the compression over the neurovascular structures as well as reconstruct any involved blood vessels. Most of these published reports were produced from large referral centers as a single center experience, and most of them had a small number of cases, especially for vascular TOS. Sanders, et al. found that only 11 of 2500 TOS operations performed over a period of 40 years were for arterial TOS in their center.6) Urschel and Kourlis found that only 12% (4% arterial and 8% venous) of the 7405 TOS operations were performed over a period of 50 years.7) This might be explained by the fact that the majority of TOS are neurogenic, and vascular TOS accounts for only 5%, with arterial being only 1%.1) However, the incidence of arterial pathology, secondary to compression at the thoracic outlet, may be underestimated in the absence of ischemic events because it might be masked by symptoms of neurogenic compression as advocated by Criado, et al.8) Furthermore, this low incidence of vascular TOS compared to neurogenic TOS might be also explained by the under-utilization of non-invasive studies such as vascular duplex in most of the centers.8)
In this study, we have shown our experience in managing vascular TOS. All of the TOS cases included were symptomatic vascular (arterial in 90.7%), only with clear symptoms of either chronic or critical upper limb ischemia. Beside the clinical presentation, diagnoses were confirmed by other investigation methods. A bony abnormality was detected in 90% of plain x-rays with the majority owing to cervical ribs (85%). Doppler ultrasound (duplex) was helpful in the diagnosis for all cases. A near cut-off of blood flow during stress (arm hyperabduction) maneuver with reproduction of symptoms was the most suggestive in this non-invasive test. Duplex detected post-stenotic subclavian artery aneurysms in five cases, as well as thrombosis of axillary and other distal arteries in four other cases. Moreover, this test is non-invasive, simple and easily performed bilaterally in one sitting, making it an effective method for vascular TOS diagnosis when compared with other conventional methods,9) and in particular for symptomatic, vascular TOS.10) Conventional arteriography is an effective vascular investigation test but is a highly invasive method. It has confirmed vascular compression or occlusion in all patients who underwent this method in our series (18.5%). Arteriography can also highlight subclavian stenoses, aneurysms, mural thrombus or occlusion of the digital arteries on the side of the compressed subclavian artery and allows for dynamic views of the subclavian and axillary vessels with the arms in the abduction and adduction. This method remains a helpful tool for vascular TOS patient assessment and pre-operative planning, but its role has become limited with the presence of advanced CT angiography. The use of arteriography is less frequent in our recent series, and it is only reserved for complex cases. In our series, 74% of cases had CT angiogram. CT arterial or venous angiogram with positioning arm maneuvers becomes very useful in providing accurate information on the location and mechanism of vascular compression. Details of relationship of bony deformity or any abnormal fibrous bands with arterial compression as well as identifying all of the structures in the thoracic outlet can be easily demonstrated by CT angiography, especially three-dimensional CT imaging with the avoidance of invasive conventional arteriography testing.11,12) Rather, CT angiogram is very important method in the assessment and for per-operative planning and even in asymptomatic or questionable TOS cases; it can improve surgical success and help for selecting operative candidates.11,12) All surgical decompressions in our study included scalenectomy for all of the cases, cervical rib excision in 85%, and 1st rib removal in 30% through the supraclavicular approach, which provides good visualization of the thoracic outlet area and excellent exposure for arterial reconstruction if needed and has been shown to have excellent results in many series.13–17) Only five cases of venous TOS were treated in this series, in which 2 of them presented with acute primary DVT, which had a lower incidence than expected for a vascular TOS since venous cases are more common.1) The lower number of venous TOS cases in our series compared to arterial cases might be explained by the under-diagnosis of such cases at the referring centers. Patients with venous TOS are usually young and athletic, presenting with mild swelling in their arms. The investigation might show deep vein thrombosis where they will be started on anticoagulation therapy without further investigation for the mechanical cause secondary to thoracic outlet anomalies.18) On the other hand the relative large number of arterial cases compared to other reports might be explained by the fact that we are a large referral center for vascular diseases in the area, and also it might be related to the high estimated prevalence of cervical rib (3.4%) and elongated transverse cervical processes (23%) in Saudi Arabia.19)
The successes of surgical decompression of TOS or outcomes that have been reported in the literature vary among different series and certainly depend on the definition used for the success as well as TOS type.20) In our study, success was defined as complete relief of vascular symptoms postoperatively and reconstructing the vascular damage, which has been achieved in all patients immediately or gradually during follow-up while respecting the difference between this outcome and other postoperative complications like numbness and weakness due to transient neurological deficit.
In the evaluation of these results, certain limitations merit emphasis. The study is a retrospective in nature and the data was collected from one center. However, this study presents the first reported experience of managing vascular TOS in Saudi Arabia.
In conclusion, careful surgical planning and prediction of perioperative complications using advanced radiological imaging coupled with performance of Vascular TOS in high volume center result in good outcomes.
Disclosure Statement
Authors declare that they have no conflicting interests, and are not supported/funded by any drug companies.
References
- Fugate MW, Rotellini-Coltvet L, Freischlag JA. Current management of thoracic outlet syndrome. Curr Treat Options Cardiovasc Med 2009; 11: 176–83 [DOI] [PubMed] [Google Scholar]
- Huang JH, Zager EL. Thoracic outlet syndrome. Neurosurgery 2004; 55: 897–902; discussion 902–3 [DOI] [PubMed] [Google Scholar]
- Atasoy E. History of thoracic outlet syndrome. Hand Clin 2004; 20: 15–6, v [DOI] [PubMed] [Google Scholar]
- Urschel HC. The history of surgery for thoracic outlet syndrome. Chest Surg Clin N Am 2000; 10: 183–8, x–xi [PubMed] [Google Scholar]
- Peet RM, Henriksen JD, Anderson Tp, et al. Thoracic-outlet syndrome: evaluation of a therapeutic exercise program. Proc Staff Meet Mayo Clin 1956; 31: 281–7 [PubMed] [Google Scholar]
- Sanders RJ, Hammond SL, Rao NM. Diagnosis of thoracic outlet syndrome. J Vasc Surg 2007; 46: 601–4 [DOI] [PubMed] [Google Scholar]
- Urschel HC, Kourlis H. Thoracic outlet syndrome: a 50-year experience at Baylor University Medical Center. Proc (Bayl Univ Med Cent) 2007; 20: 125–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Criado E, Berguer R, Greenfield L. The spectrum of arterial compression at the thoracic outlet. J Vasc Surg 2010; 52: 406–11 [DOI] [PubMed] [Google Scholar]
- Wadhwani R, Chaubal N, Sukthankar R, et al. Color Doppler and duplex sonography in 5 patients with thoracic outlet syndrome. J Ultrasound Med 2001; 20: 795–801 [DOI] [PubMed] [Google Scholar]
- Hachulla E, Camilléri G, Fournier C, et al. [Clinical, flowmetric and radiologic study of the thoracic outlet in 95 healthy subjects: physiologic limitations and practical impact]. Rev Med Interne 1990; 11: 19–24 [DOI] [PubMed] [Google Scholar]
- Hasanadka R, Towne JB, Seabrook GR, et al. Computed tomography angiography to evaluate thoracic outlet neurovascular compression. Vasc Endovascular Surg 2007; 41: 316–21 [DOI] [PubMed] [Google Scholar]
- Remy-Jardin M, Remy J, Masson P, et al. Helical CT angiography of thoracic outlet syndrome: functional anatomy. AJR Am J Roentgenol 2000; 174: 1667–74 [DOI] [PubMed] [Google Scholar]
- Sanders RJ, Pearce WH. The treatment of thoracic outlet syndrome: a comparison of different operations. J Vasc Surg 1989; 10: 626–34 [DOI] [PubMed] [Google Scholar]
- McCarthy MJ, Varty K, London NJ, et al. Experience of supraclavicular exploration and decompression for treatment of thoracic outlet syndrome. Ann Vasc Surg 1999; 13: 268–74 [DOI] [PubMed] [Google Scholar]
- Maxey TS, Reece TB, Ellman PI, et al. Safety and efficacy of the supraclavicular approach to thoracic outlet decompression. Ann Thorac Surg 2003; 76: 396–9; discussion 399–400 [DOI] [PubMed] [Google Scholar]
- Glynn RW, Tawfick W, Elsafty Z, et al. Supraclavicular scalenectomy for thoracic outlet syndrome—functional outcomes assessed using the DASH scoring system. Vasc Endovascular Surg 2012; 46: 157–62 [DOI] [PubMed] [Google Scholar]
- Reilly LM, Stoney RJ. Supraclavicular approach for thoracic outlet decompression. J Vasc Surg 1988; 8: 329–34 [PubMed] [Google Scholar]
- Thompson JF, Winterborn RJ, Bays S, et al. Venous thoracic outlet compression and the Paget-Schroetter syndrome: a review and recommendations for management. Cardiovasc Intervent Radiol 2011; 34: 903–10 [DOI] [PubMed] [Google Scholar]
- Bokhari RF, Al-Sayyad MJ, Baeesa SS. Prevalence of cervical ribs and elongated transverse processes in Saudi Arabia. Saudi Med J 2012; 33: 66–9 [PubMed] [Google Scholar]
- Bhattacharya V, Hansrani M, Wyatt MG, et al. Outcome following surgery for thoracic outlet syndrome. Eur J Vasc Endovasc Surg 2003; 26: 170–5 [DOI] [PubMed] [Google Scholar]