Abstract
An emergent operation was performed on a 73-year-old woman with massive hematuria and serious shock. A computed tomography (CT) revealed that the cause of the shock was hemorrhage from an aneurysm into the ureter, with resultant massive hematuria. During surgery, we observed that the ureter was encased into the wall of the aneurysm, with exposure of the pre-positioned ureteric stent inside the aneurysmal space. Reconstruction of the ureter was performed by wrapping the tissues with the ureteric stent inside. Postoperative recovery was uneventful, and CT angiography showed complete exclusion of the right internal iliac artery with the in situ ureteric stent.
Keywords: massive hematuria, ureter, iliac artery aneurysm
Introduction
An isolated iliac artery aneurysm can cause serious problems since it grows unnoticed deep within the pelvic space and sometimes becomes large enough to rupture spontaneously or affect nearby organs, such as the bowels, the urinary system, veins, and gynecological organs via progressive compression or invasion.1) Here, we report the invasion of the ureter by an aneurysm, finally resulting in a massive hematuria.
Case
A 73-year-old woman with recent relapsing fever was admitted to our hospital for suspected pyelonephritis and sepsis. Her past history documented mixed collagen diseases, and 2 mg of oral betamethasone had been administered daily. At admission, a plain CT revealed a mass, 62 mm in diameter, inside the pelvis (Fig. 1A) compressing the right ureter to cause hydronephrosis. While her hemodynamics was improving, ureteric stenting was performed to alleviate urinary retention and infection. Enterococcus faecium was revealed to be the causative agent by urine and blood culture, and antibiotic therapy was continued. Two weeks after admission, since an enhanced CT definitively demonstrated the pelvic mass to be a huge internal iliac artery aneurysm, 68 mm in diameter, (Fig. 1B), an operation was then considered to avert rupture of her rapidly growing aneurysm. However, difficulty in controlling the urinary tract infection deferred the surgical intervention. About a month later, the sudden onset of massive hematuria and serious shock necessitated an emergent operation, because a heavy clot formation identified by CT was at this time thought to be produced by aneurysmal rupture directly into the bladder (Fig. 2). The operation was performed through a right extra-peritoneal approach. While tracing upstream along the external iliac artery with simultaneous exposure of the aneurysm, the proximal neck of the aneurysm was successfully ligated. After an aneurysmectomy, suture closure of the distal exit branch orifices was performed by an endoaneurysmal route. Inside the exposed aneurysmal space, the encased right ureter was revealed to have a broad fistulous communication with the lumen of the aneurysm. Reconstruction of the urinary route was performed by wrapping it as well as filling the space with a recto-abdominal muscle flap to prevent abscess formation or urine leakage (Fig. 3). She was doing well and was discharged 27 days after the operation. However, she required periodic replacement of the ureteric stent at an outpatient clinic thereafter.
Fig. 1.
(A) A plain CT showing an abnormal mass detected within the pelvis. (B) An enhanced CT revealing the huge mass to be an isolated internal iliac artery aneurysm. The black arrow indicates the encased right ureter.
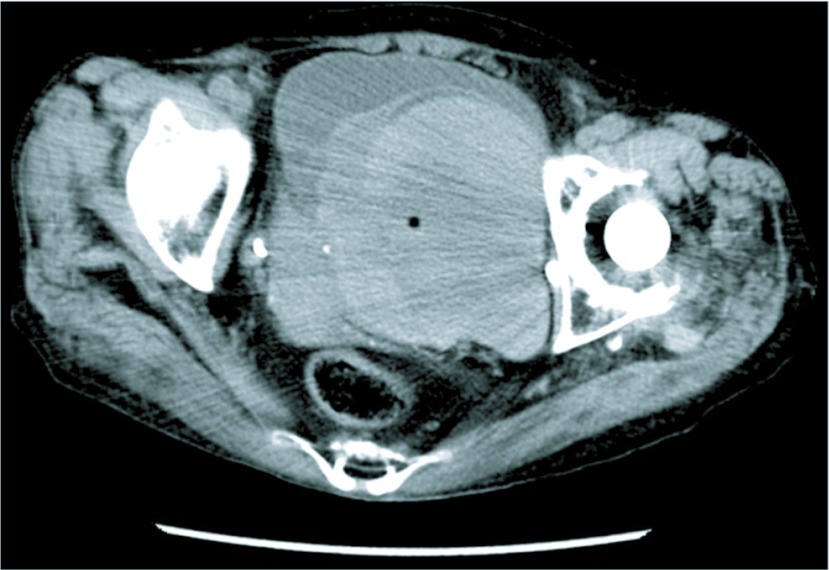
Fig. 2.
A plain CT showed a profuse amount of high density shadow suggesting a hematoma filling most of the bladder.
Fig. 3.
Schematic representation of the operative procedure.
(A) The proximal neck of the aneurysm could be ligated in this case. After incision of the aneurysm, orifices of the exit branches were sutured, and the fistula (arrow head) into the ureter was observed from inside the aneurysm.
(B) The fistula was oversewn using the nearby aneurysmal wall, and the surrounding dead space was filled with a recto-abdominal muscle flap. CIA: common iliac artery; EIA: external iliac artery; IIA: internal iliac artery; RAMF: recto-abdominal muscle flap.
Discussion
Concerning the possibility of spontaneous rupture, surgical intervention for iliac artery aneurysms exceeding 30 mm in diameter has unanimously been recommended.2) However, these aneurysms are located deep within the pelvis which enables their latent growth. As a result, they sometimes become big enough to affect adjacent organs by the time they become symptomatic or are detected incidentally through imaging. In such situations, the vulnerable organs include the iliac venous channels, colon, urinary system, gynecological organs, and pelvic nerves. Occlusion, rupture, fistula formation, erosion, and infection in situ or indirectly to remote organs can all take place with a poor prognosis even if an operation is attempted.3)
Among the various complications, the urinary tract organs, especially the ureter, seem to be the most susceptible to obstruction by aneurysmal compression. Sometimes the ureter can be incorporated into the aneurysmal wall (so called encasement) frequently producing urinary tract infection and bacteremia, and micro- or macro-hematuria.4) Spontaneous iliac artery aneurysm-ureteric fistula with massive hematuria is thought to be caused by such erosive process on the tissues as has been reported in a few cases.5,6)
In our case, the isolated right internal iliac artery aneurysm was first diagnosed at a diameter of 68 mm by enhanced CT, and the patient had a complicated state of lingering infection despite the use of an indwelled ureteric catheter. However, surgical removal of the aneurysmal compression should have been performed as early as possible because of the sudden ilio-ureteric fistula formation. The cause of the fistula formation was difficult to identify; it may have been a natural outcome of the incorporated ureter in a rapidly growing aneurysm or secondary due to mechanical stimulation of the ureteric stent on the narrowed, weakened and inflamed ureter, in addition to the influence of the pulsatile movement of the aneurysmal wall.7) Whatever the cause, the bleeding resulted from the fistula, which put the patient in a state of serious shock. Prolonged control of the infection should not have been prioritized given the potential for fatal complications.
Endovascular therapy seems a promising technique for iliac aneurysms.8) However, while exclusion of the aneurysm is critical, it is also important to block back-flow from the distal branches. Another drawback of permanent stenting in this particular case is the patient’s tendency toward chronic bacteremia that risks infection during routine and emergent operations related to deployed devices.7) On the other hand, an iliac stent or balloon could be used as an effective temporary solution before emergent open surgery. However, as described in the literature,7) only the presence of a ureteric stent itself can have a local hemostatic effect, as in our case, with tolerable hemodynamics. Thus, we were able to perform the emergent operation without the need for additional endovascular techniques.
Surgical therapy has already been well-established in complex and symptomatic cases9) and should be an absolute indication in lesions with accompanying infection. The extra-peritoneal surgical approach without the use of artificial vessels seemed, in our case, accessible and less invasive. Decompression of the aneurysm was achieved by ligating its neck, plus obliterative endoaneurysmorrhaphy. With regards to the ilio-ureteric fistula, this case required additive surgical procedures. Since natural repair of the ureter was difficult, an alternative method of reconstruction was applied using plastic surgery to maintain the route of urinary flow. Aggravation of the infection was less likely at the repair site. As a result, the urinary stent became indispensable in this case.
In conclusion, huge isolated internal iliac artery aneurysms with significant compression of the adjacent organs should alert one to various catastrophic outcomes. Our specific case of irreversible ureter involvement and eventual rupture resulting in massive bleeding is therefore presented as an example of this serious condition requiring early surgical intervention.
Disclosure Statement
The authors disclose no conflict of interest.
References
- Dix FP, Titi M, Al-Khaffaf H. The isolated internal iliac artery aneurysm —A review. Eur J Vasc Endovasc Surg 2005; 30: 119–29 [DOI] [PubMed] [Google Scholar]
- McCready RA, Pairolero PC, Gilmore JC, et al. Isolated iliac artery aneurysms. Surgery 1983; 93: 688–93 [PubMed] [Google Scholar]
- Parry DJ, Kessel D, Scott DJ. Simplifying the internal iliac artery aneurysm. Ann R Coll Surg Engl 2001; 83: 302–8 [PMC free article] [PubMed] [Google Scholar]
- Krupski WC, Selzman CH, Floridia R, et al. Contemporary management of isolated iliac aneurysms. J Vasc Surg 1998; 28: 1–11; discussion 11–3 [DOI] [PubMed] [Google Scholar]
- Grime PD, Wilmshurst CC, Clyne CA. Spontaneous iliac artery aneurysm-ureteric fistula. Eur J Vasc Surg 1989; 3: 455–6 [DOI] [PubMed] [Google Scholar]
- Thiry AJ, Struyven J, Van DeCasseye M. Spontaneous rupture of right iliac arterial aneurysm into ureter. Urology 1980; 16: 101–3 [DOI] [PubMed] [Google Scholar]
- Darcy M. Uretro-arterial fistulas. Tech Vasc Interv Radiol 2009; 12: 216–21 [DOI] [PubMed] [Google Scholar]
- Boules TN, Selzer F, Stanziale SF, et al. Endovascular management of isolated iliac artery aneurysms. J Vasc Surg 2006; 44: 29–37 [DOI] [PubMed] [Google Scholar]
- Brin BJ, Busuttil RW. Isolated hypogastric artery aneurysms. Arch Surg 1982; 117: 1329–33 [DOI] [PubMed] [Google Scholar]