Abstract
Objective
For evaluation of audiological service outcomes, the primary objective was to determine baseline and target profiles on the Speech, Spatial and Qualities of Hearing scale (SSQ); a secondary objective was to test a short form of the SSQ; opportunity was also taken to compare responses of samples providing consistent versus inconsistent self-assessments.
Design
2×2×2 factorial design crossed age, reported presence versus absence of hearing difficulty, and low versus high self-rated hearing ability.
Study Sample
Eight samples (total n=413), representing two age ranges; a response of “yes” or “no” to a question about having hearing difficulty, and either low or high self-rated hearing ability on six items from the SSQ.
Results
Using present and previous results, baseline SSQ profiles were determined indicating the pattern of response likely to be observed prior to clinical intervention, and both an achieved outcome and “ideal” target outcome from such intervention. The six-item SSQ yielded better test-retest results in consistent versus inconsistent samples. The inconsistent samples showed signs of different interpretations of “hearing difficulty”.
Conclusions
Baseline and both actual and ideal target outcomes can guide comparative appraisal of clinical achievements; more research is needed to determine a robust short form of the SSQ.
Introduction
The most common client group seeking audiological services offered to the general population comprises people in middle and later age. General audiological practice seeks to provide them with rehabilitation, primarily through hearing aid fitting, with the aim of reducing disabilities due to their hearing impairment. An increasingly critical element of service provision is the assessment of its beneficial outcome, and several different kinds of measures are available to appraise this. Some are physical (e.g., real-ear gain), others are psychophysical (e.g., aided hearing threshold or speech test performance). There has also been considerable research and clinical attention given to clients’ self-assessments of benefit, as reflected in measures such as the Profile of Hearing Aid Benefit (Cox et al 1991), the Client-Oriented Scale of Improvement (Dillon et al, 1997), the Glasgow Hearing Aid Benefit Profile (Gatehouse, 1999), and the International Outcomes Inventory for Hearing Aids (Cox et al. 2000).
A recent development in the self-assessment arena is the Speech, Spatial and Qualities of Hearing scale (Gatehouse & Noble, 2004), or SSQ. This is a 49-item inventory in three sections that cover various aspects of speech hearing, spatial hearing, and other qualities of hearing such as segregation of sounds, their naturalness and identification, and listening effort. Responses are scored using a 0-10 scale with higher scores representing greater ability.
Novel features of the SSQ are its coverage of dynamic and complex listening contexts in addition to more traditional themes, such as hearing speech in quiet versus noise. These new lines of assessment have emerged as significant in identifying the disabilities that drive emotional and social handicaps caused by hearing impairment (Gatehouse & Noble, 2004), and in highlighting the problems of asymmetric hearing loss and the advantages of bilateral hearing aid provision (Noble & Gatehouse 2004, 2006). Given the likely ongoing application of the SSQ in the field of hearing rehabilitation (e.g., Arndt et al., 2011; van Wieringen et al., 2011), it is valuable to determine the scale’s representation of hearing ability and disability in relevant population samples.
To achieve this goal we have drawn from results obtained in a study that was designed to allow classification of a group of middle and later aged adults into eight subsamples. These derived samples were constructed as the first step in a comprehensive project whose aim is to examine associations among a range of laboratory-based tests of cognitive and sensory functions in relation to SSQ ratings. The eight samples were deliberately stratified, and otherwise matched, according to a 2×2×2 factorial design, the factors being: 1) age group (50-64 versus 65-80 years); 2) a response of “yes” versus “no” to the question “Do you have difficulty with your hearing?”, and 3) high versus low self-assessed hearing ability on six items selected from the SSQ. The SSQ items were chosen explicitly to reflect influences of cognitive and binaural function in addition to peripheral impairment, so as to provide distinctive population samples for later laboratory investigation. Age-group was included as a factor on the basis that changes in auditory processing independent of peripheral impairment are observable with increasing age (e.g., Pichora-Fuller & Souza, 2003). The question, “Do you have difficulty with your hearing?”, was included as a factor because it has been a standard item in population surveys in the UK (e.g., Stephens et al., 1990; Davis, et al., 2007).
The primary aim of the present study was to report data from subsequent interviews using the complete SSQ so as to derive both a pre-rehabilitation profile and an “ideal outcome” profile. The former is the baseline against which rehabilitation outcome is compared, the latter is what might be aimed for as a rehabilitation target. The term “profile” refers to the pattern of responses to SSQ items grouped into ten subscales (Gatehouse & Akeroyd, 2006), as described in the Method section. These profiles were further compared to two profiles calculated from data obtained previously in clinical samples, one prior to rehabilitation management (Gatehouse & Noble, 2004) and the other six months after fitting of bilateral hearing aids (Noble & Gatehouse, 2006). The various profiles can serve to guide future judgments about the relative effectiveness of different clinical strategies. A secondary aim was to observe the test-retest reliability of the six items selected from the SSQ to determine their possible usefulness for population screening purposes.
The factorial design of the project entailed crossing yes/no answers on the hearing difficulty question with high/low self-ratings on the six SSQ items. This results in samples of people who provide consistent responses (“no difficulty” and high SSQ ratings, or “yes, difficulty” and low SSQ ratings), because a report of “no difficulty” would be expected to be associated with higher SSQ self-ratings, and a report of “yes, difficulty” associated with lower ratings. But it also yields samples who provide inconsistent responses (“no difficulty” but low SSQ ratings, or “yes, difficulty” but high SSQ ratings). The opportunity was taken to compare the profiles of these consistent and inconsistent samples as derived from the full version of the SSQ to determine if there were differences in those profiles that might suggest a basis for inconsistent responding. Measured hearing threshold levels, the incidence of tinnitus, hearing aid use, and overall quality of life in the eight samples were also compared.
Method
Originally, a very large-scale sample was drawn at random from the electoral roll of residents of Glasgow (Scotland) and Manchester (England), distributed across a range of districts representative of the whole populations of these two cities, and who responded to a postal questionnaire. The final sample size was n=5324. The postal questionnaire was self-administered and had items covering hearing difficulties and tinnitus, dizziness, hearing aid use, hearing services provision, a generic rating of quality of life, and six items from the SSQ. The six SSQ items addressed: 1) following two speech streams simultaneously; 2) following rapidly-switching conversational turns; 3) judging distance; 4) judging movement; 5) recognizing people by their voice, and 6) clarity of voices. No direction was given about listening mode (aided or unaided) when responding to the SSQ items, as it was expected that the great majority of respondents would not use a hearing aid. The postal questionnaire is reproduced in Appendix II, with the items whose responses are analyzed in the present paper shown in boldface type. Further reports are planned on data derived from other parts of this questionnaire.
The Glasgow sample was used to generate the eight stratified samples, because subsequent interviewing was undertaken in that city (the location of MRC Institute of Hearing Research, Scottish Section). Of the 3824 people in the Glasgow sample, 1979 were aged between 50 and 80 years. The target was to get 50 people in each sample or 400 in all; in practice, 413 participated. For each of these people, a complete SSQ was obtained by home interview, using 22 experienced interviewers who were trained using a detailed set of documented guidelines compiled by the National Centre for Social Research, as briefed by IHR. Interviews were conducted between three and six months after receipt of the postal questionnaire.
The eight samples were defined by a three-factor design, each having two levels. The first factor was age: 50-64 versus 65-80 years. The second factor was subjective hearing difficulty: an answer of “yes” or “no” to the question: “Do you have difficulty with your hearing?”. The third factor was self-rated hearing ability, based on the average score on the six items from the SSQ. Anyone who scored ≤6.5 was classified as having low self-assessed ability; anyone who scored ≥6.6 was classified as having high self-assessed ability (on every SSQ item a value of 0.0 corresponds to complete lack of an ability and a score of 10.0 corresponds to perfect ability). The criterion of 6.6 was somewhat arbitrary. It was guided by calculations from previous data (Noble & Gatehouse, 2006, Table 2) that showed audiology clinic clients scored an average of 4.8 on the six-item SSQ prior to bilateral hearing aid fitting, and 6.6 six months after such fitting. This suggested that in a general population sample, average scores lower than 6.6 are likely among people who report having hearing difficulty, whereas scores exceeding 6.6 are likely among those who do not report hearing difficulty. Cases were selected to ensure matching of high and low ability samples on the six SSQ items, irrespective of an answer of “no” or “yes” to the hearing difficulty question, and to ensure substantial contrast between high and low self-rated ability.
Table 2.
Proportions of males in each of the eight samples, average ages of each sample, tinnitus incidences, and overall quality of life ratings. Samples are displayed in terms of High versus Low ssq6 ratings, and “no” versus “yes” in answer to the hearing difficulty question. The first value in each pair is for younger (50-64 years) samples, the second for older (65-80 years) samples.
| High | Low | ||
|
|
|||
| Per cent male | no | 49, 37 | 44, 28 |
| yes | 53, 46 | 52, 57 | |
|
| |||
| Age in years | no | 57, 71 | 57, 71 |
| yes | 58, 72 | 58, 72 | |
|
| |||
| Tinnitus | no | 1.3, 1.4 | 1.6, 1.9 |
| yes | 2.1, 1.9 | 2.3, 2.1 | |
|
| |||
| QoL | no | 8.3, 8.3 | 6.5, 6.8 |
| yes | 8.3, 8.4 | 6.6, 6.5 | |
We termed the eight groups: no-difficulty/high-ability/younger, no-difficulty/high-ability/older, yes-difficulty/low-ability/younger, yes-difficulty/low-ability/older, no-difficulty/low-ability/younger, no-difficulty/low-ability/older, yes-difficulty/high-ability/younger, yes-difficulty/high-ability/older (see Table 1). For easier reference in the text these are abbreviated, with the consistent samples in lower case, as follows: no/high/y, no/high/o, yes/low/y, yes/low/o; and the inconsistent samples in upper case, thus: NO/LOW/Y, NO/LOW/O, YES/HIGH/Y, YES/HIGH/O (the age letter is dropped where we averaged across age). It is worth noting that being able to construct inconsistent samples suggests that such people are not especially rare.
Table 1.
Factors used to construct the eight stratified samples; details in Method section
| Hearing difficulty (“Do you have difficulty with your hearing?”) |
Hearin g ability (ssq6) |
Age group (50-64 vs. 65-80) |
Type | Abbreviation |
|---|---|---|---|---|
| No-difficulty | High- ability |
Younger | Consistent | no/high/y |
| No-difficulty | High- ability |
Older | Consistent | no/high/o |
| Yes -difficulty | Low- ability |
Younger | Consistent | yes/low/y |
| Yes -difficulty | Low- ability |
Older | Consistent | yes/low/o |
| No-difficulty | Low- ability |
Younger | Inconsistent | NO/LOW/Y |
| No-difficulty | Low- ability |
Older | Inconsistent | NO/LOW/O |
| Yes-difficulty | High- ability |
Younger | Inconsistent | YES/HIGH/Y |
| Yes -difficulty | High- ability |
Older | Inconsistent | YES/HIGH/O |
A subset of participants (n=141) attended the MRC Institute of Hearing Research in Glasgow for air conduction hearing threshold testing, These tests were carried out by a clinical audiologist who is a member of the Institute.
The results of the home-visit interviews were used to calculate the SSQ profiles. These are defined in terms of the ten “pragmatic” subscales devised by Gatehouse and Akeroyd (2006) rather than the scores on all 49 items. The subscales reflect the content of items that are akin to each other, in terms of meaning, within the three main subsections of the SSQ. These subscales may or may not relate to the underlying factor structure of the overall scale, a matter currently being investigated. There are four subscales in the Speech section of the SSQ addressed to hearing speech: 1) in quiet conditions; 2) in competing noise; 3) against competing speech, and 4) in the context of following two simultaneous or overlapping speech streams. There are two Spatial subscales, one on directional location, one on distance and movement discrimination, and there are four Qualities subscales: 1) clarity and naturalness of sounds; 2) identifiability of different sounds; 3) segregation of simultaneous sounds, and 4) listening effort. The items constituting these ten subscales are listed in Appendix I (note: Not every SSQ item contributes to one or other of the 10 subscales).
The average score of the six SSQ items used in the postal survey is termed (lower case) “ssq6”. The average score of the corresponding items in the home-visit SSQ interview is termed “SSQ6”.
Results
1. SSQ Profiles for the eight stratified samples
For reference purposes we report the SSQ results (including those on the ssq6) for the eight stratified samples as a table, forming Appendix III. The results from the ssq6 postal survey show both the closeness of matching in self-rated high and low ability samples, and the degree of contrast between high and low ability that was achieved across the consistent and inconsistent samples. The results on the ten subscales from the SSQ home interviews show that for the no/high and yes/low samples — i.e., the consistent ones — the pattern of those interview responses was orderly. On every subscale the scores for the no/high samples were significantly higher than for the yes/low samples, and there were no differences in scores between the older and younger groups.
The differences between the (consistent) no/high and yes/low samples’ scores ranged from 1.5 to 3.3 scale points on a 0-10 scale, aggregating across both age groups (Noble & Gatehouse, 2006, observed that a 1-scale-point difference was typically associated with a p value of ≤0.05). Among the four Speech subscales the contrast between the no/high and yes/low samples’ scores was lowest for speech in quiet (2.4 points), and greatest for multistream listening (3.3). Both of the Spatial subscales showed a contrast of 2.5 points. Three of the Qualities subscales (quality/naturalness, identifiability and segregation) had contrasts of 1.5 to 2.2 scale points; the listening effort subscale difference was 3 points.
The scores of the older (inconsistent) NO/LOW sample were all slightly (non-significantly) lower than those of the NO/LOW/Y. There were no statistically significant differences among the speech subscale scores of all four inconsistent samples. The YES/HIGH/Y and O samples showed signs of higher Spatial subscale scores than the equivalent NO/LOW samples. Finally, the YES/HIGH/O sample showed signs of higher scores on the first three of the Qualities subscales than the NO/LOW/O sample.
2. Comparison with prior data
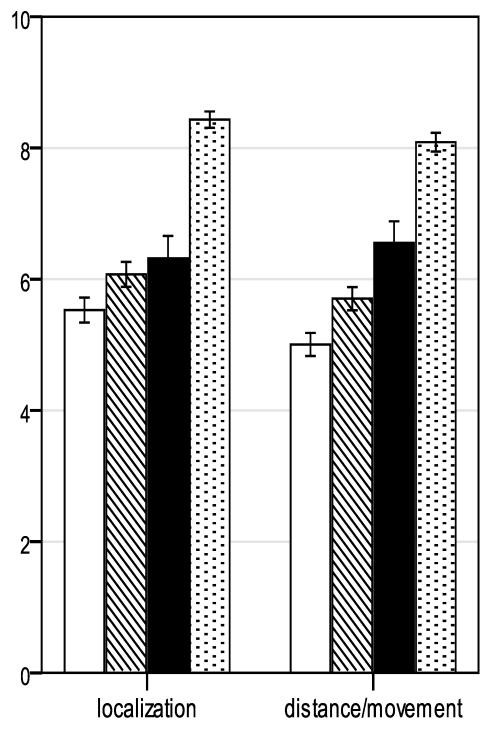
Figure 1 compares present SSQ data with SSQ profiles calculated for present purposes from prior data reported by Noble and Gatehouse (2006, p. 176). The unfilled bars are from a clinic sample in the UK National Health Service, surveyed between 2001-2002, who had not yet been assessed for rehabilitation management (n=144; average age 68.3 yr, sd 10.2). We argue that this sample’s data represent an estimate of baseline ability for a clinical population because they were provided by people referred to a general hospital audiology service for management of hearing disabilities; hence this profile is termed clinic baseline. The solid bars are from a clinic sample of bilaterally aided listeners (UK National Health Service, managed between 2002-2004; n=42; average age 66.4 yr, sd 11.5). Their scores represent residual disability following six months of consistent use of that fitting: thus this profile is labeled hearing aid outcome. The hatched and the dotted bars are, respectively, for the two consistent samples from the present data: yes/low and no/high, averaged in both cases across the two age groups (as noted above, there was no difference in scores between the younger and older groups). The yes/low group’s scores are for those people who reported difficulty with their hearing and gave a low rating of their hearing ability on the six SSQ items. Because these data are from a population sample we argue that this profile approximates the self-assessed ability of people who may benefit from audiological management. It is termed “stratified sample baseline”. There were 12 people in this sample who reported using a hearing aid “most or all of the time” (Appendix II, question 11). We have thus calculated this baseline not counting these cases, on an argument that those currently using a hearing aid should not be regarded as part of a “baseline” (thus, n=96, average age 64.5 yr, sd 8.1), though the effect of their removal was only to change the scores by about 0.1-0.2 scale points. Finally, the scores from the no/high sample represent the profile of a target that would be achieved if rehabilitation management were effective enough to return clients’ hearing to some approximation of a normal standard for the 50-80-year age group: this profile is therefore termed “ideal outcome” (n=105; average age 64.1 yr, sd 8.2).
Figure 1.
Mean SSQ pragmatic subscale scores of four profiles of respondents: clinic baseline (pre-management clinic clients, n=144; data from Noble & Gatehouse, 2006); stratified sample baseline (yes-difficulty/low-ability samples; n=96); hearing aid outcome (bilaterally fitted clinic clients, n=42; data from Noble & Gatehouse, 2006); ideal outcome (no-difficulty/high-ability samples; n=105). Error bars represent standard error (±1).
There was an average 0.9-scale-point difference in the Speech subscales between clinic baseline and the (higher) ratings for the stratified sample baseline, but the differences ranged from 0.4 (speech in speech contexts) to 1.2 (speech in quiet); there was a 0.4-scale-point difference in the Spatial subscales. There were variable differences among the Qualities subscales. The largest difference (1.3 points, in favour of the stratified sample baseline) was found in the listening effort subscale.
Several hearing domains showed appreciable benefit from fitting with bilateral hearing aids, as reflected in the difference between clinic baseline and hearing aid outcome scores. Multistream listening showed an increase of 3.1 scale points in the aided (hearing aid outcome) condition compared to the unaided (clinic baseline) condition; speech in quiet had a 2-point increase, speech in speech 1.6 points, distance and movement discrimination 1.5 points, and listening effort 1.8 points. Several domains were modestly improved by bilateral aiding (localization, 0.8 points; quality and naturalness, 0.9 points; segregation, 0.8 points); some domains can be regarded as being unaffected by hearing aid fitting (speech in noise, 0.5 points; identifiability, −0.1 points).
3. Test-retest reliability of the SSQ items
The six SSQ questions included in the initial postal questionnaire (ssq6) were repeated as part of the home interview, using the full SSQ, that occurred three-to-six months later (SSQ6). Correlating the two sets of results for these questions provides a measure of their test-retest reliability. The test-retest correlation of the ssq6:SSQ6 across all participants combined (n=413) was 0.54. The corresponding value for the combination of the two consistent samples (no/high, yes/low; n=213, both age groups combined) was 0.71; the value for the combination of the two inconsistent samples (NO/LOW, YES/HIGH; n=200) was 0.33.
4. Comparing consistent and inconsistent results
We first examined the patterns of self-ratings on the subsequent full version of the SSQ that might account for the inconsistency in the postal survey between a response of “no” or “yes” to the question “Do you have difficulty with your hearing?” and self-ratings on the ssq6. We then considered measured HTLs, tinnitus incidence, quality of life, and hearing aid use, both in connection with the consistency-inconsistency dimension and more broadly in relation to the stratification adopted in this study.
A. SSQ subscales
The results from the consistent groups demonstrated coherence and stability (Appendix III, left half of the Table). The pattern of responding in the inconsistent groups was harder to interpret. For the NO/LOW/Y sample, the data showed that on two of the Speech subscales (speech in quiet and speech in noise) and on three of the Qualities subscales (naturalness, identification and segregation) the average scores were not significantly lower than in the (consistent) no/high/y sample. But differences were evident in multiple speech stream listening, both aspects of spatial hearing, and in listening effort. Thus the inconsistency for the NO/LOW/Y sample may be accounted for if the meaning they gave to “hearing difficulty”, when answering “no” to the yes/no question about that, was “listening under relatively favourable conditions”.
No equivalent proposal can be made with regard to the NO/LOW/O group. They had uniformly (though non-significantly) lower subscale scores than the corresponding younger group. This could indicate an “age effect” of the kind reported by Gatehouse (1991, 1994) — reduced self-assessed hearing ability with increasing age reflected in the ssq6, but no self-report of difficulty reflected in answer to the “difficulty” question.
The YES/HIGH/Y and YES/HIGH/O groups did not differ from each other in their subscale scores. Their scores were not significantly different from the consistent no/high groups on either of the Spatial subscales, nor on three of the four Qualities subscales (though they did have significantly lower listening effort scores — i.e., greater effort). Both YES/HIGH groups had significantly lower ratings than the no/high groups on three Speech subscales: speech in noise, speech in speech and multistreaming. Thus, the YES/HIGH responses may be accounted for if the meaning they gave to “hearing difficulty”, when answering the general question about that, was “listening under challenging conditions”. This contrasts with the response profile of at least the NO/LOW/Y group.
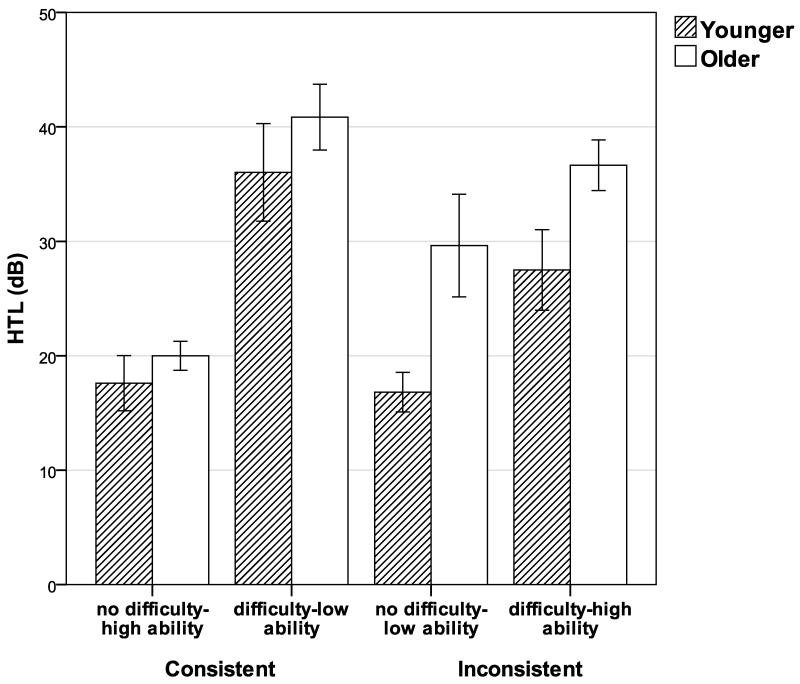
B. Hearing threshold levels
Figure 2 shows the average hearing threshold levels of the eight samples (0.5-4 kHz, both ears) and the numbers of people tested in each. The mean hearing threshold level (HTL) for the younger samples was less than for the older listeners (24 vs 31 dB), and the mean value for those who reported “no difficulty” with hearing was less than for the hearing-difficulty groups (21 vs 35 dB). The mean HTLs for groups with high ssq6 scores was 5 dB lower than those with low ssq6 scores, but there was a non-uniformity in the direction of HTL differences across age and yes/no report. The difference in mean HTL between the two consistent groups (no/high versus yes/low) was substantial (19 vs 37 dB), and in the expected direction. The mean HTLs of the inconsistent groups (NO/LOW versus YES/HIGH) were 23 versus 32 dB, suggesting yes/no hearing difficulty rather than ssq6 rating is associated with HTL in these groups. The HTL contrast between the older versus younger NO/LOW samples is congruent with the “age effect” suggested by the SSQ responses.
Figure 2.
Hearing threshold levels (HTL) averaged across 0.5, 1, 2 and 4 kHz, both ears, for eight stratified samples: Consistent — no-difficulty/high-ability/younger (n=19), no difficulty-high-ability/older (n=6), yes-difficulty/low-ability/younger (n=23), yes-difficulty/low-ability/older (n=19); Inconsistent —no-difficulty/low-ability/younger (n=15), no-difficulty/low-ability/older (n=10), yes-difficulty/high-ability/younger (n=23), yes-difficulty/high-ability/older (n=26). Error bars represent standard error (±1).
C. Tinnitus, quality of life
Table 2 provides demographic information showing that the gender distribution across the groups was broadly comparable, that the samples classed as younger were of comparable age to each other, and that those classed as older were also comparable. Tinnitus incidence was scored using a 0-3 scale (see Appendix II, question 6) where 0=no tinnitus and 3=tinnitus all or most of the time. The reported incidence of tinnitus was significantly higher in the groups answering “yes” to the hearing difficulty question than in those saying “no”, by 0.5 scale points on average, (t(410)=5.99, p<.001). Tinnitus presence may evoke a “yes” in response to the hearing difficulty question, rather than, or in addition to, hearing difficulty understood as reduced audibility of external sounds. There was a sharp contrast in overall quality of life ratings between those with low versus high ssq6 scores: 6.6 versus 8.3 on a 0-10 scale,( t(407)= −9.18, p<.001).
D. Hearing aid use
Response options about hearing aid use were “no, never”, “no, but have tried one”, “yes, some of the time”, and “yes, most or all of the time”. Aggregating across the factor of age, in the no/high samples (n=105), no one reported use of a hearing aid. In the NO/LOW samples (n=99), only one person reported using a hearing aid, most or all of the time. But in the YES/HIGH samples (n=101), 12 people reported using a hearing aid --- seven some of the time, five most or all of the time --- and in the yes/low samples (n=108), 27 people reported they used a hearing aid, 15 some of the time, 12 most or all of the time. This indicates that hearing-aid use goes with self-reported hearing difficulty rather than self-assessed hearing ability.
We compared SSQ subscale scores of those reporting hearing aid use most or all of the time with the scores of those not using an aid. In both the yes/low and YES/HIGH samples, the hearing-aid users’ scores were lower than non-users. Of those tested audiometrically, and who did not use a hearing aid (n=66), the average HTL was 30 dB (sd=13.2), whereas those tested who used a hearing aid most or all of the time (n=9) had average unaided HTL of 58 dB (sd=11.6). This substantial difference may account for the comparative lack of benefit from aiding, at least as reflected in SSQ scores.
Discussion
The basis of the present project is the Speech, Spatial and Qualities of Hearing Scale (Gatehouse & Noble, 2004). This measure has recently been independently tested as to some of its psychometric properties (Singh and Pichora-Fuller, 2010). The SSQ is itself evolving, and there is now a benefit version (SSQ-B; Jensen et al., 2009). We expect the measure will continue to have valuable application in the area of aural rehabilitation, and the present paper has taken a step to examine further its utility in this respect.
There were six items selected from the SSQ for use in a postal survey that recurred some months later as part of home interviews with the complete SSQ. The test-retest correlation in the consistent samples for these six items was 0.71, comparable with the value of 0.69 reported by Singh & Pichora-Fuller (2010) for an equivalent application of the complete SSQ, i.e., mail-out followed by interview. We can reasonably rely on the SSQ scores of the consistent samples as stable estimates of their self-rated abilities, so those results can be used to fulfill the primary objective of the present study, namely, to propose baseline and target SSQ profiles for evaluating rehabilitative outcomes.
We labeled the consistent yes-difficulty/low-ability profile as stratified sample baseline and the consistent no-difficulty/high-ability profile as ideal outcome. We also defined two other profiles, clinic baseline and hearing aid outcome, using re-analyses of prior data. The stratified sample baseline is analogous to the profile derived from a clinical sample yet to receive rehabilitation management (clinic baseline). Both of these may be regarded as estimates of profiles for people at the beginning of the intervention journey. The stratified sample baseline is best understood as a profile in the general community of people who could well benefit from provision of hearing services, whereas the clinic baseline is probably a more realistic profile of those who actually do seek such service. We surmise that the clinic baseline may be conservative, reflecting referral practices under the UK National Health Service, and that a profile more like the stratified sample baseline might be observed in a service context such as the US Veterans Administration. The baselines we present can be used for purposes of comparison in clinical and related service settings in which the SSQ features as part of pre-management assessment.
The ideal outcome is just that: an ideal status to be attained were it possible to restore hearing function to “normal” for the age range (50-80 years) under consideration. In most clinical circumstances this ideal may never be reached. The subscale scores of the no-difficulty/high-ability samples are consistently high (Appendix III), hence it would probably be ambitious to expect similar outcomes in typical clinical settings. The ideal outcome is still a valuable profile to portray, and against which outcomes from different approaches to hearing disability management can be evaluated. For example, it may be that different fitting and communication strategies affect one versus another set of the domains addressed via the SSQ subscales. The hearing aid outcome profile is derived from SSQ scores of outpatients fitted with hearing aids bilaterally, after six months of consistent use. The conditions of clinical practice that allowed collection of these data were independent of the investigators (Noble & Gatehouse, 2006, p 173) and it is unknown if these conditions represent best attainable practice. Certainly, as shown in Figure 1, there are substantial contrasts between the hearing aid outcome and ideal outcome profiles — in particular, speech in noise, localization, and all of the Qualities subscales. Such contrasts illustrate the considerable gap between what was achieved in one particular clinical setting, and what may be construed as a goal to be aimed at. What is attainable may well also be constrained by the baseline profile, and again we emphasize that the outcomes presented here are for comparative purposes in post-management assessment.
Notwithstanding the fairly respectable test-retest correlation result for the consistent samples (0.71), the result for the complete stratified sample set was modest (0.54), being reduced by the very low level correlation observed in the inconsistent samples (0.33). It could be argued that the deliberate construction of samples exhibiting inconsistency, whilst understandable methodologically within the larger purposes of the project, heightened the risk of getting unstable results. In any event, the secondary aim of testing the stability of the ssq6 has resulted in data that do not allow a recommendation that this particular set of items can reliably substitute for the SSQ as a whole, and analysis will be continued so as to identify a more satisfactory short form.
The average values for SSQ subscale scores in Appendix III show that, in the case of the inconsistent samples, the substantial ssq6 contrasts achieved in the original stratification procedure did not carry through to the scale as a whole. This has turned out, however, to be informative. For example, the NO/LOW/Y group was not significantly different, in the domains of speech hearing in quiet and in noise, from the no/high groups. A reasonable speculation is that when responding to a general question about hearing difficulty, people in the NO/LOW/Y group answered on the basis that in favourable or merely generally noisy conditions they did not experience noticeable problems. The two items in the ssq6 addressing speech hearing were drawn from one particular subscale — multistream processing — which, it turns out, does differentiate the no/high from the NO/LOW samples. The stratification adopted has allowed the fact of different profiles of hearing ability to become apparent. Conversely, it is also worth noting that people in the YES/HIGH groups scored significantly higher on a question about tinnitus incidence, suggesting that “hearing difficulty” extends to audibility of unwanted, internally-generated noises. Because of what appears in the data to be different interpretations of “hearing difficulty” (no difficulty in favourable conditions versus difficulty but in challenging conditions), it could be worthwhile, in future study, to inquire into the attributions of respondents (Colsher & Wallace, 1989; Heider, 1958; Shaver, 1985): do they see their ability or the situation as the cause of perceptual difficulty?.
In summary, we have presented results using the SSQ that portray the likely profile of responses of people prior to rehabilitation management and following such management. Outcomes highlight the potential importance of consistent and inconsistent responding. The results will be of value to those offering hearing rehabilitation services who wish to include the SSQ in their clinical assessments.
Supplementary Material
Acknowledgments
This work was funded by the intramural program of the Medical Research Council, by the Chief Scientist Office of the Scottish Government, and by the Oticon Research Foundation; thanks to the National Centre for Social Research for self-rated data gathering, and to Patrick Howell for hearing testing. Our thanks to the reviewers of the originally submitted paper for their valuable suggestions that have improved presentation.
Footnotes
Dedication
This paper is dedicated to the memory of Stuart Gatehouse who developed the empirical project that forms the basis of the report.
References
- Arndt S, Laszig R, Aschendorff A, Beck R, Schild C, Hassepass F, et al. Unilateral deafness and cochlear implantation. Audiological diagnostic evaluation and outcomes. HNO. 2011;59(5):437–446. doi: 10.1007/s00106-011-2318-8. [DOI] [PubMed] [Google Scholar]
- Colsher PL, Wallace RB. Data quality and age - health and psychobehavioral correlates of item nonresponse and inconsistent responses. Journals of Gerontology. 1989;44(2):45–52. doi: 10.1093/geronj/44.2.p45. [DOI] [PubMed] [Google Scholar]
- Cox R, Hyde M, Gatehouse S, Noble W, Dillon H, Bentler R, et al. Optimal outcome measures, research priorities, and international cooperation. Ear & Hearing. 2000;21:106S–115S. doi: 10.1097/00003446-200008001-00014. [DOI] [PubMed] [Google Scholar]
- Cox RM, Gilmore C, Alexander GC. Comparison of two questionnaires for patient-assessed hearing aid benefit. Journal of the American Academy of Audiology. 1991;2:134–145. [PubMed] [Google Scholar]
- Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I. Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models. Health Technology Assessment. 2007;11(42):1–294. doi: 10.3310/hta11420. [DOI] [PubMed] [Google Scholar]
- Dillon H, James A, Ginis J. Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. Journal of the American Academy of Audiology. 1997;8(1):27–43. [PubMed] [Google Scholar]
- Gatehouse S. The role of non-auditory factors in measured and self-reported disability. Acta Oto-laryngologica, Suppl. 1991;476:249–256. [PubMed] [Google Scholar]
- Gatehouse S. Components and determinants of hearing aid benefit. Ear and Hearing. 1994;15(1):30–49. doi: 10.1097/00003446-199402000-00005. [DOI] [PubMed] [Google Scholar]
- Gatehouse S. Glasgow Hearing Aid Benefit Profile: Derivation and validation of a client-centred outcome measure for hearing aid services. Journal of the American Academy of Audiology. 1999;10:80–103. [Google Scholar]
- Gatehouse S, Akeroyd M. Two-eared listening in dynamic situations. International Journal of Audiology. 2006;45(Supplement 1):S120–S124. doi: 10.1080/14992020600783103. [DOI] [PubMed] [Google Scholar]
- Gatehouse S, Noble W. The Speech, Spatial and Qualities of Hearing Scale (SSQ) International Journal of Audiology. 2004;43(1):85–99. doi: 10.1080/14992020400050014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heider F. The psychology of interpersonal relations. Wiley; New York: 1958. [Google Scholar]
- Jensen NS, Akeroyd MA, Noble W, Naylor G. The Speech, Spatial and Qualities of Hearing scale (SSQ) as a benefit measure; NCRAR Conference: The Ear-Brain System: Approaches to the Study and Treatment of Hearing Loss; Portland, Oregon. 2009; ( http://www.ihr.mrc.ac.uk/downloads/products/questionnaires/ssq/2009_Portland_Jensen_Akeroyd_Noble_Naylor__SSQb.pdf) [Google Scholar]
- Noble W, Gatehouse S. Interaural asymmetry of hearing loss, Speech, Spatial and Qualities of Hearing Scale (SSQ) disabilities, and handicap. International Journal of Audiology. 2004;43:100–114. doi: 10.1080/14992020400050015. [DOI] [PubMed] [Google Scholar]
- Noble W, Gatehouse S. Effects of bilateral versus unilateral hearing aid fitting on abilities measured by the speech, spatial, and qualities of hearing scale (SSQ) International Journal of Audiology. 2006;45(3):172–181. doi: 10.1080/14992020500376933. [DOI] [PubMed] [Google Scholar]
- Pichora-Fuller MK, Souza PE. Effects of aging on auditory processing of speech. International Journal of Audiology. 2003;42(2):S11–S16. [PubMed] [Google Scholar]
- Shaver KG. The attribution of blame: Causality, responsibility and blameworthiness. Springer-Verlag; New York: 1985. [Google Scholar]
- Singh G, Pichora-Fuller MK. Older adults’ performance on the Speech, Spatial, and Qualities of Hearing Scale (SSQ): Test-retest reliability and a comparison of interview and self-administration methods. International Journal of Audiology. 2010;49:733–740. doi: 10.3109/14992027.2010.491097. [DOI] [PubMed] [Google Scholar]
- Stephens SDG, Callaghan DE, Hogan S, Meredith R, Rayment A, Davis AC. Hearing disability in people aged 50-65: effectiveness and acceptability of rehabilitative intervention. British Medical Journal. 1990;300:508–511. doi: 10.1136/bmj.300.6723.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Wieringen A, De Voecht K, Bosman AJ, Wouters J. Functional benefit of the bone-anchored hearing aid with different auditory profiles: objective and subjective measures. Clinical Otolaryngology. 2011;36(2):114–120. doi: 10.1111/j.1749-4486.2011.02302.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.