Abstract
The triple vulnerability model (Barlow, 2000, 2002) posits that three vulnerabilities contribute to the etiology of emotional disorders: (1) general biological vulnerability (i.e., dimensions of temperament such as neuroticism and extraversion); (2) general psychological vulnerability (i.e., perceived control over life stress and emotional states); (3) disorder-specific psychological vulnerability (e.g., thought-action fusion for obsessive-compulsive disorder, OCD). Despite the prominence of this model, a comprehensive empirical evaluation has not yet been undertaken. The current study used structural equation modeling to test the triple vulnerability model in a large clinical sample (N = 700), focusing on vulnerabilities for depression, social phobia, generalized anxiety disorder (GAD), and OCD. Specifically, we examined the incremental prediction of each level of the triple vulnerability model for each disorder, with the following putative disorder-specific psychological vulnerabilities: thought-action fusion (TAF) for OCD, the dysfunctional attitudes (DAS) for depression, and intolerance of uncertainty (IoU) for GAD. In the final model that included all three levels of vulnerabilities, neuroticism had significant direct effects on all four disorder constructs, and extraversion was inversely associated with depression and social phobia. However, perceived control was significantly associated with GAD and OCD only. Of the disorder-specific psychological vulnerabilities, TAF was significantly and specifically related to OCD. In contrast, DAS and IoU were not significant predictors of depression and GAD respectively, instead contributing to other disorders. The results are discussed in regard to structural models of the emotional disorders and the various roles of general and specific vulnerability dimensions in the onset, severity, and temporal course of psychopathology.
A sizeable literature has accrued on the dimensions that act as risk factors for the anxiety and mood disorders. Although a number of vulnerability constructs has been identified, a considerable portion of this research has focused on two genetically based core dimensions of temperament: neuroticism and extraversion. Indeed, a wealth of evidence attests to the heritability of these constructs (e.g., Fanous, Gardner, Prescott, Cancro, & Kendler, 2002; Hettema, Prescott, & Kendler, 2004; Viken, Rose, Kaprio, & Koskenvuo, 1994), and their roles in accounting for the severity, overlap, and maintenance of depression and anxiety (e.g., Brown, 2007; Gershuny & Sher, 1998). However, leading conceptual models assert that dimensions of temperament (e.g., neuroticism, extraversion) do not act alone in determining the etiology, course, and complications of emotional disorders (e.g., Barlow, 2002; Carver, Johnson, & Joormann, 2008; Clark, Watson, & Mineka, 1994; Mineka, Watson, & Clark, 1998). For instance, Barlow (2000, 2002; Suárez, Bennett, Goldstein, & Barlow, 2009) formulated a triple vulnerability model of emotional disorders, which draws from and integrates the literatures of genetics, personality, cognitive and neuroscience, and emotion and learning theories. This model specifies the existence of a general biological vulnerability that consists of genetically based, stable dispositions to experience to negative emotions that corresponds to core dimensions of temperament (e.g., neuroticism). In addition, a temporally stable general psychological vulnerability emerges from early childhood experience characterized by a stressful, unpredictable environment and/or the influence of specific parenting styles (described in detail in the attachment theory literature; cf. Shear, 1991) that inhibit the development of effective coping strategies and self-efficacy. These early experiences lead to a general sense of unpredictability and uncontrollability over life events and emotions that, along with elevated sympathetic nervous system arousal, forms the core of the process of anxiety (Barlow, 2002). If the two general vulnerabilities are present, the individual is at increased risk for experiencing generalized anxiety and/or depression, in the context of triggering stressful events (Chorpita & Barlow, 1998; Suárez et al., 2009). However, a third diathesis, referred to as a disorder-specific psychological vulnerability, comes into play in the form of learning a particular focus of distress, or learning that some situations, objects, or internal states (e.g., thoughts, somatic sensations) are potentially dangerous even if objectively they are not. These learning experiences can be as straightforward as watching parents model severe fears of specific objects or situations such as small animals (e.g., as in specific phobia), or more subtle such as experiencing heightened attention from caregivers to the potential danger of unexplained somatic sensations (e.g., as in panic disorder or hypochondriasis). Thus, this third vulnerability is activated when the two general vulnerabilities, through the process of learning, become specifically associated with an object, situational context, or internal state. This process results in one or more key diagnostic features that become the principal focus or foci of distress. In the next sections, the three types of risk factors are discussed in more detail, along with extant research that bears on their relevance to the anxiety and mood disorders.
General Biological Vulnerability (Temperament)
As noted earlier, general biological vulnerability refers to genetically based dimensions of temperament such as neuroticism and extraversion that are associated with heightened levels of anxiety and related negative emotions.1 Indeed, research has shown that neuroticism and extraversion are genetically linked to the anxiety and mood disorders, accounting for about 30% to 50% of the liability for individual disorders, as well as substantial shared variance among these disorders (Bienvenu, Hettema, Neale, Prescott, & Kendler, 2007; Hettema, Neale, Myers, Prescott, & Kendler, 2006). Neuroticism is robustly associated with the mood and anxiety disorders, although to varying degrees, ranging from the strongest relationships with generalized anxiety disorder (GAD) and depression, and the weakest with specific phobia (e.g., Brown, 2007; Brown, Chorpita, & Barlow, 1998; Mineka et al., 1998; Watson, Gamez, & Simms, 2005). Whereas neuroticism is considered to be etiologically relevant to the full range of emotional disorders (i.e., both mood and anxiety disorders), the influence of extraversion is specific to depression and social phobia (e.g., Brown & Barlow, 2009; Clark et al., 1994; Mineka et al., 1998). In fact, low extraversion is most closely linked to social phobia, whereas depression has a weaker association that is primarily due to extraversion’s positive emotionality component (Brown et al., 1998; Mineka et al., 1998; Naragon-Gainey, Watson, & Markon, 2009). Although most of the empirical support for neuroticism and extraversion has emanated from cross-sectional research, longitudinal studies have also demonstrated the relevance of these constructs to the development and maintenance of depression and anxiety (e.g., Brown, 2007; Brown & Rosellini, 2011; Gershuny & Sher, 1998).
General Psychological Vulnerability
The triple vulnerability model asserts that a sense of unpredictability and uncontrollability over life events and emotional states is a psychological vulnerability to all anxiety and mood disorders. Indeed, perceived control has long been a central construct in etiological models of depression and anxiety, dating back to Rotter’s (1954) locus of control theory and Seligman’s (1975) learned helplessness theory. Despite the importance of this construct in conceptual models of emotional disorders, there is a paucity of research addressing the relationship of perceived control to the various anxiety and mood disorders. However, studies have found low levels of perceived control among smokers with panic disorder and posttraumatic stress disorder (Vujanovic, Marshall, Gibson, & Zvolensky, 2010), as well as those with elevated obsessive-compulsive symptoms/beliefs (Moulding, Kyrios, Doron, & Nedeljkovic, 2009) and GAD symptoms or worry (e.g., Chapman, Kertz, & Woodruff-Borden, 2009; Gould & Edelstein, 2010; Stapinski, Abbott, & Rapee, 2010). In addition, perceived control moderates the effect of anxiety sensitivity on agoraphobic avoidance in patients with panic disorder (White, Brown, Somers, & Barlow, 2006). In laboratory studies, participants report less anxiety in response to panic provocations when the biological challenge procedure is perceived as controllable (e.g., Sanderson, Rapee, & Barlow, 1989; Telch, Silverman, & Schmidt, 1996). Perceived control is sensitive to treatment response, increasing after treatment of GAD (Treanor, Erisman, Salters-Pedneault, Roemer, & Orsillo, 2011) and panic disorder (Meuret, Rosenfield, Seidel, Bhaskara, & Hofmann, 2010; Rapee, Craske, Brown, & Barlow, 1996). Thus, although a few studies have provided evidence for the link between perceived control and anxiety disorders, research is needed to examine if perceived control has a unique role in the onset, severity, and maintenance of the full array of anxiety and mood disorders.
Disorder-Specific Psychological Vulnerabilities
In addition to two generalized diatheses (one biological, one psychological), the triple vulnerability model posits that a specific psychological vulnerability influences the origin and expression of the anxiety and mood disorders through learning experiences that dictate a specific focus of distress; e.g., beliefs that certain thoughts, images, and impulses are dangerous as in obsessive-compulsive disorder (OCD), or beliefs that certain physical sensations are dangerous as in panic disorder. Specific psychological vulnerabilities have been proposed for most of the major anxiety and mood disorders. Although other realizations of the triple vulnerability model are possible (e.g., anxiety sensitivity in relation to panic disorder), we focus here on three specific vulnerability dimensions for the DSM-IV disorder constructs examined in the present investigation (dysfunctional attitudes in depression, thought-action fusion in OCD, intolerance of uncertainty in GAD). It is important to note that specificity is likely to be relative rather than absolute, because “specific” vulnerabilities should be significantly associated with most mood and anxiety disorders due to comorbidity and general distress (see Mineka et al., 1998). However, the magnitudes of the associations should show a pattern of relative specificity for each dimension and its corresponding disorder (particularly in multivariate analyses controlling for comorbidity). As is evident below, few studies have evaluated this issue thus far.
Dysfunctional attitudes are defined as underlying negative assumptions about the self, world, and future (Weismann & Beck, 1978). This construct was originally posited to be a specific risk factor for depression, although it is also moderately (and sometimes comparably) associated with general anxiety (e.g., Hamilton & Abramson, 1983; Hankin, Abramson, Miller, & Haeffel, 2004; Hollon, Kendall, & Lumry, 1986; Sutton et al., 2011) and social phobia (Reiter, Otto, Pollack, & Rosenbaum, 1991; Sanz & Avia, 1994; Sutton et al., 2011). However, there is evidence for specificity to depression relative to panic, agoraphobia, and specific phobia (Ohrt, Sjödin, & Thorell, 1999; Sutton et al., 2011).
Thought-action fusion (TAF)—hypothesized to be a specific risk factor to OCD—describes a tendency to believe that: (1) thinking about a disturbing event increases its likelihood of occurrence, and (2) thinking about a disturbing action is morally equivalent to carrying it out (Shafran, Thordarson, & Rachman, 1996). High TAF is consistently associated with OCD (e.g., Amir, Freshman, Ramsey, Neary, & Brigidi, 2001; Meyer & Brown, in press; Shafran et al., 1996), but is also associated with other anxiety disorders (Hazlett-Stevens, Zucker, & Craske, 2002; Rassin, Diepstraten, Merckelbach, & Muris, 2001; Rassin, Merckelback, Muris, & Schmidt, 2001) and depression (Abramowitz, Whiteside, Lynam, & Kalsy, 2003; Rassin, Merckelbach, et al., 2001; Shafran et al., 1996) (for a review, see Berle & Starcevic, 2005). However, some multivariate analyses provide support for relative specificity between OCD and TAF, in that OCD symptoms were largely responsible for the association between TAF and other symptoms (e.g., worry; Coles, Mennin, & Heimberg, 2001).
Finally, intolerance of uncertainty (IoU) has been defined as a “dispositional characteristic that results from a set of negative beliefs about uncertainty and its implications” (Dugas & Robichaud, 2007). IoU is theorized to be a specific cognitive vulnerability factor for chronic worry and GAD. A recent meta-analysis that examined the associations of IoU with GAD, OCD, and depression found that IoU was similarly and moderately related to all three disorder constructs. Other studies have indicated that IoU is related to social anxiety (e.g., Boelen & Reijntjes, 2009; Boelen, Vrinssen, & van Tulder, 2010; Carleton, Collimore, & Asmundson, 2010). However, the majority of studies on the relationship between IoU and anxiety and mood disorder constructs has been conducted in nonclinical samples. Evidence from clinical studies indicates that GAD can be distinguished from other anxiety disorder diagnoses on the basis of higher levels of IoU. Moreover, a path analytic study found that IoU had significant direct effects on symptoms of worry and depression (but not symptoms of autonomic arousal, OCD, and health anxiety), even after holding a measure of negative affectivity constant (Norton, Sexton, Walker, & Norton, 2005). These data, along with findings suggesting IoU possesses temporal stability and antecedence to worry, have been taken in support of the role of IoU as a cognitive vulnerability to GAD (e.g., Buhr & Dugas, 2002; Dugas & Ladouceur, 2000; Freeston, Rhéaume, Letarte, Dugas, & Ladouceur, 1994; cf. Koerner & Dugas, 2006).
Current Study
Despite the prominence of the triple vulnerability model as a conceptual framework for understanding the shared and unique etiological features of the emotional disorders (Barlow, 2002), a comprehensive empirical evaluation of this model has yet to be undertaken. As the preceding literature review attests, previous studies relevant to the triple vulnerability model have tended to focus on one vulnerability dimension at a time, often in the context of only one or two emotional disorders. A compelling test of the Barlow model necessitates a multivariate approach to evaluate the unique contribution of the various vulnerability dimensions to the prediction of emotional disorder psychopathology (e.g., do putative psychological vulnerabilities explain significant additional variance in the DSM-IV constructs beyond core dimensions of temperament?). Moreover, the simultaneous evaluation of multiple DSM-IV constructs is essential for ascertaining the specificity of the posited relationships between the dimensions of vulnerability and the anxiety and mood disorders (e.g., is perceived control pertinent to all emotional disorders? are disorder-specific vulnerability dimensions differentially related to the emotional disorders in the predicted fashion?).
The present study evaluated one possible application of the triple vulnerability model where the unique and specific contributions of various vulnerability dimensions to the prediction of selected DSM-IV anxiety and mood disorder constructs (unipolar depression, GAD, OCD, social phobia) were examined in a large and diagnostically diverse sample of treatment-seeking outpatients. The four DSM-IV disorder constructs were selected based on prior evidence of the substantively salient differential relationships with one another (e.g., potentially problematic phenotypic overlap between GAD and depression, and GAD and OCD) and with the various dimensions of vulnerability (e.g., differential association of extraversion with social phobia and depression; possible relevance of IoU to both GAD and OCD). Based on a series of structural equation models specified in accord with the triple vulnerability model, it was predicted that: (a) neuroticism would have significant direct effects on all DSM-IV disorders, whereas extraversion would have significant effects only on social phobia and depression (general biological vulnerability); (b) perceived control would contribute to the prediction of all disorders, holding neuroticism and extraversion constant (general psychological vulnerability); and (c) the disorder-specific psychological vulnerability dimensions would contribute significantly to the prediction of the anxiety and mood disorders, holding the general vulnerabilities constant and in a differential fashion consistent with their posited specificity (i.e., TAF, IoU, and dysfunctional attitudes would be differentially related to OCD, GAD, and depression, respectively). With regard to the third prediction, while the extant literature has not provided uniformly strong support for the specificity of the selected disorder-specific vulnerabilities, previous studies have rarely examined the differential relationships among these dimensions and emotional disorders in multivariate models (perhaps masking patterns of relative specificity). Moreover, particularly for some constructs (e.g., IoU), most studies have used nonclinical samples. Thus, predictions regarding the nature of the relationships between the disorder-specific vulnerabilities and the DSM-IV disorder constructs were guided by the originating conceptual models.
Method
Participants
The sample was 700 patients who presented to the Center for Anxiety and Related Disorders at Boston University, an outpatient clinic specializing in the assessment and treatment of anxiety and mood disorders. Women constituted the larger portion of the sample (60.6%); average age was 32.38 (SD = 11.62, range = 18 to 74). The sample was predominantly Caucasian (90.9%; African-American = 3.7%, Asian = 4.7%, Latino/Hispanic = 4.4%). Diagnoses were established with the Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994), a semi-structured interview designed to ascertain reliable diagnosis of the DSM-IV anxiety, mood, somatoform, and substance use disorders, and to screen for the presence of other conditions (e.g., psychotic disorders). The ADIS-IV-L provides dimensional assessment of the key and associated features of disorders (0–8 ratings); these features are dimensionally rated regardless of whether a formal DSM-IV diagnosis is under consideration. A previous reliability study of the ADIS-IV-L indicated good-to-excellent interrater agreement for current disorders (range of κs = .67 to .86) except dysthymia (κ = .31; Brown, Di Nardo, Lehman, & Campbell, 2001). For the dimensional ADIS-IV-L ratings used as indicators of the DSM-IV disorder factors in this study, interrater reliability estimates (intraclass correlations, ICC) are provided below, based on a subsample of 74 cases who underwent two independent administrations of the ADIS-IV-L during the course of this study. The rates of current clinical disorders occurring frequently in the sample were: social phobia (48.6%), mood disorders (i.e., major depression, dysthymic disorder, depressive disorder NOS; 35.7%), generalized anxiety disorder (33.0%), panic disorder with or without agoraphobia (25.3%), obsessive-compulsive disorder (16.0%), and specific phobia (14.6%). The majority (69.6%) of patients had more than one current disorder: 1 disorder = 30.4%, 2 disorders = 32.3%, 3 disorders = 20.0%, 4+ disorders = 17.3%.
Latent Variables and Indicators in the Measurement and Structural Models
In addition to various dimensions of the triple vulnerability model (i.e., genetic, general psychological, and disorder-specific vulnerabilities), four DSM-IV disorder constructs were examined in the measurement and structural models: Depression (DEP), Generalized Anxiety Disorder (GAD), Obsessive-Compulsive Disorder (OCD), and Social Phobia (SOC).
General biological vulnerabilities
Latent variables corresponding to the general biological vulnerabilities of Neuroticism and Extraversion were defined by subscales from the NEO-Five Factor Inventory (NFFI; Costa & McCrae, 1992) and the short form version of Eysenck Personality Questionnaire (EPQ; Eysenck & Eysenck, 1975).
General psychological vulnerability
The general psychological vulnerability dimension was assessed by the revised Anxiety Control Questionnaire (ACQ-R; Brown, White, Forsyth, & Barlow, 2004). The ACQ-R is the only extant measure of perceived (un)controllability over emotional states and situational threat, a key construct in Barlow’s (2000, 2002) triple vulnerability theory of emotional disorders. Although results of Brown et al. (2004) indicated that the latent structure of the ACQ-R is comprised of three well-defined subdomains (Emotion Control, Threat Control, Stress Control), hierarchical factor analysis supported the existence of a single higher-order dimension of Perceived Control. In fact, this higher-order dimension possessed more favorable scale reliability (ρ = .85) than the ACQ-R subdomains (range of ρs = .73 to .76). Thus, the broader dimension of Perceived Control was used as the indicator of general psychological vulnerability in the measurement and structural models (higher scores reflect greater levels of perceived emotional control).
Disorder-specific vulnerabilities
The following questionnaires were used as indicators of putative disorder-specific vulnerabilities for obsessive-compulsive disorder (OCD), generalized anxiety disorder (GAD), and unipolar depression (DEP), respectively: (a) Thought-Action Fusion Scale (TAF; Shafran et al., 1996), a measure of beliefs that thinking about unwanted events is immoral or increases their likelihood of occurrence; (b) Intolerance of Uncertainty Scale (IUS; Buhr & Dugas, 2002), a measure of the excessive tendency to consider it unacceptable that a negative event may occur, however small the probability of its occurrence, and (c) Dysfunctional Attitudes Scale (DAS, Form A; Weissman & Beck, 1978), a measure of cognitions conjectured to predispose or maintain depression. Although evidence indicates the TAF is multifactorial, a broader dimension of thought-action fusion (TAF total score) was used in the present analyses based on findings from a recent psychometric investigation in a large clinical sample attesting to the existence of a broader factor that has more favorable scale reliability (ρ = .97) and concurrent validity than the TAF subdomains (Meyer & Brown, in press). Results from the most recent and largest scale psychometric investigation of the IUS (Sexton & Dugas, 2009) indicated that the latent structure of this measure is comprised of two factors (Factor 1 = 15 items, Factor 2 = 12 items). The first factor was used as the indicator of the intolerance of uncertainty construct in the current study based on findings from Sexton and Dugas (2009) that this dimension evidenced somewhat better concurrent validity than the second factor. The scale reliability estimate (Cronbach’s α) of the first factor was .92 (Sexton & Dugas, (2009). In accord with prior research (e.g., Alloy et al., 2006; Craighead, Sheets, Craighead, & Madsen, 2011; Rogers et al., 2009), the DAS total score was used as the indicator of depressogenic cognitions and maladaptive beliefs (average α across studies = .90).
Depression (DEP)
A latent variable of unipolar depression was formed using two questionnaire indicators and an ADIS-IV-L clinical rating composite: (a) Beck Depression Inventory – II (BDI-II; Beck, Steer, & Brown, 1996); (b) Depression scale of the 21-item version of the Depression Anxiety Stress Scales (DASS-D; Lovibond & Lovibond, 1995; cf. Antony, Bieling, Cox, Enns, & Swinson, 1998); and (c) the ADIS-IV dimensional ratings of the 9 symptom criteria of DSM-IV major depression (0 = “none” to 8 = “very severe”; ICC = .84). In accord with procedures from previous studies (e.g., Brown, 2007; Brown & Rosellini, 2011), the BDI-II was scored using the 10 items that load on a Cognitive/Affective factor (items 1–9, 13) that are more specific to the unipolar mood disorders.
Generalized Anxiety Disorder (GAD)
A factor of DSM-IV GAD was created in part by using two ADIS-IV-L dimensional rating measures (all 0–8 scales): excessiveness of worry in 8 areas (e.g., finances, minor matters); and a single clinical rating of patients’ difficulty controlling worry (ICCs = .68 and .62, respectively). In addition, the GAD factor was defined by the Penn State Worry Questionnaire (Meyer, Miller, Metzger, & Borkovec, 1990; cf. Brown, Antony, & Barlow, 1992), a 16-item self-report measure of chronic worry.
Social Phobia (SOC)
One questionnaire and two ADIS-IV-L clinical rating measures were used as indicators of the SOC latent variable: (a) Social Phobia scale of the Albany Panic and Phobia Questionnaire (APPQ-S; Rapee, Craske, & Barlow, 1994/1995; cf. Brown, White, & Barlow, 2005), (b) sum composite of patients’ fear of 13 social situations (e.g., initiating a conversation, participating at meetings/classes) rated by the clinician during the ADIS-IV-L (0 = “no fear” to 8 = “very severe fear”; ICC = .89); and (c) single clinical rating (0–8 scale) of interference and distress associated with patients’ social anxiety (ICC = .81).
Obsessive-Compulsive Disorder (OCD)
The OCD latent variable was represented by two clinical ratings and two questionnaires. The clinical rating indicators were: (a) a sum composite of ADIS-IV-L dimensional ratings of persistence/distress associated with 9 common obsessions (e.g., doubting, contamination; ICC = .75); and (b) a sum composite of ADIS-IV-L dimensional ratings of the frequency of 6 compulsions (e.g., washing, checking; ICC = .79). The self-report indicators were two subscales from the Obsessive-Compulsive Inventory – Revised (OCI-R; Foa et al., 2002): Obsessions and Neutralizing. These subscales were selected from the 6 possible OCI-R subscales based on their relevance to the broader construct of OCD (e.g., other OCI-R subscales, such as Hoarding, assess more specific facets of OCD).
Data Analysis
The raw data were analyzed using a latent variable software program and robust maximum-likelihood (MLR) minimization functions (Mplus 6.11, Muthén & Muthén, 1998–2011). Although negligible (average covariance coverage = .985), missing data were accommodated by MLR (cf. Allison, 2003). Goodness of fit of the models was evaluated using the root mean square error of approximation (RMSEA), and its 90% confidence interval, the Tucker-Lewis index (TLI), the comparative fit index (CFI), and the standardized root mean square residual (SRMR). Acceptable model fit was defined in part by the criteria forwarded by Hu and Bentler (1999): RMSEA values close to .06 or below (90% CI upper limit close to ≤ .06, nonsignificant CFit), CFI and TLI values close to .95 or above, and SRMR values close to .08 or below. The acceptability of the models was further evaluated by the presence/absence of salient localized areas of strains in the solutions (e.g., modification indices), and the strength and interpretability of the parameter estimates. Although widely accepted remedial strategies have not been developed, Type I error inflation is an issue in latent variable models where the statistical significance of multiple parameter estimates is evaluated (cf. Cribbie, 2007). Thus, the substantive interpretation of structural parameter estimates (e.g., regression paths) in the models relied more heavily on the magnitude (effect size, ƒ2), consistency, and specificity of the effects than on statistical significance (especially given the study’s considerable power to detect small effects as statistically significant).
Results
Measurement Model
A confirmatory factor analysis (CFA) was conducted to evaluate a measurement model comprised of latent variables corresponding to the four DSM-IV disorder constructs (DEP, GAD, SOC, OCD), Neuroticism, Extraversion, and the general psychological and disorder-specific vulnerability dimensions. Because the general psychological and disorder-specific vulnerability dimensions were defined by single indicators, measurement error in these variables was adjusted for by fixing error variances to predetermined values on the basis of the indicators’ sample variances and the scale reliability estimates reported in the Method section (cf. Brown, 2006; see Table 1 for error variances). With the exception of DEP, each DSM-IV disorder latent variable was defined by two clinical rating indicators (in addition to at least one self-report measure). Accordingly, within the GAD, OCD, and SOC latent variables, the error covariance for the clinical rating indicators was freely estimated based on the expectation of source effects (e.g., due to differential method covariance, the clinical ratings of excessive worry and difficulty controlling worry would be more strongly correlated with each other than with the Penn State Worry Questionnaire). All factor cross-loadings were fixed to zero. The global goodness of fit of this solution was satisfactory, χ2(144) = 527.29, p < .001, SRMR = .04, RMSEA = 0.06 (90% CI = .06 to .07), TLI = 0.93, CFI = .95. The completely standardized factor loading estimates from this solution are presented in Table 1 (range of λs = .51 to .99; all ps < .001).
Table 1.
Factor Loadings (Completely Standardized) for Measurement Model of DSM-IV Disorder and Triple Vulnerability Constructs (N = 700)
| Factor Loading | |
|---|---|
| Depression | |
| DASS-Depression | .86 |
| BDI | .91 |
| ADIS-IV-L Depression | .78 |
| Generalized Anxiety Disorder | |
| PSWQ | .88 |
| ADIS-IV-L excessive worry | .56 |
| ADIS-IV-L uncontrollability of worry | .55 |
| Obsessive-Compulsive Disorder | |
| OCI-R Obsessions | .79 |
| OCI-R Neutralizing | .51 |
| ADIS-IV-L obsessions | .57 |
| ADIS-IV-L compulsions | .51 |
| Social Phobia | |
| APPQ Social Phobia | .88 |
| ADIS-IV-L fear of social situations | .88 |
| ADIS-IV-L Social Phobia interference/distress | .79 |
| Neuroticism | |
| NFFI Neuroticism | .92 |
| EPQ Neuroticism | .82 |
| Extraversion | |
| NFFI Extraversion | .86 |
| EPQ Extraversion | .85 |
| Perceived Control | |
| ACQ-R | .92a |
| Thought-Action Fusion | |
| TAFS | .99a |
| Intolerance of Uncertainty | |
| IUS | .96a |
| Dysfunctional Attitudes | |
| DAS | .95a |
Note. DASS = Depression Anxiety Stress Scales, BDI = Beck Depression Inventory, ADIS-IV- L = Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version, PSWQ = Penn State Worry Questionnaire, OCI-R = Obsession-Compulsions Inventory – Revised, APPQ = Albany Panic and Phobia Questionnaire, NFFI = NEO Five-Factor Inventory, EPQ = Eysenck Personality Questionnaire, ACQ-R = Anxiety Control Questionnaire-Revised, DAS = Dysfunctional Attitudes Scale, IUS = Intolerance of Uncertainty Scale; TAFS = Thought-Action Fusion Scale. All factor loadings significant at p < .001;
Error variances of single indicators constrained to unstandardized theta values of 18.41, 124.45, 13.69, and 4.50, for the ACQ-R, DAS, IUS, and TAFS indicators, respectively.
Tests of the differential magnitude of disorder-specific vulnerability correlations
The correlations among the dimensions from the measurement model of the DSM-IV disorder and triple vulnerability constructs are provided in Table 2. In accord with the conceptualization of disorder-specific vulnerability, it was posited that the dimensions of TAF, IoU, and DAS would be differentially related to the latent variables of OCD, GAD, and DEP, respectively. The differential magnitude of the correlations of each disorder-specific vulnerability dimension was evaluated using the Steiger z-test procedure (cf. Meng, Rosenthal, & Rubin, 1992). These results are presented in Table 3. Consistent with prediction, the TAF dimension was more strongly related to OCD (r = .48) than the other three DSM-IV disorder constructs (range of remaining rs = .18 to .28). However, the expected pattern of differential relationships was not obtained for IoU and DAS. IoU had its strongest zero-order relationship with DEP (r = .62). Although the relationship between IoU and GAD was the second largest in magnitude (r = .54), the strength of this association differed only from OCD. DAS evidenced comparable relationships with DEP, GAD, and SOC (range of rs = .50 to .55), and was more weakly associated with OCD (r = .34).
Table 2.
Correlations Among Dimensions from the Measurement Model of DSM-IV Disorder and Triple Vulnerability Constructs (N = 700)
| DEP | GAD | OCD | SOC | N | E | PC | TAF | IoU | DAS | |
|---|---|---|---|---|---|---|---|---|---|---|
| DEP | 1.00 | |||||||||
| GAD | .48 | 1.00 | ||||||||
| OCD | .41 | .49 | 1.00 | |||||||
| SOC | .49 | .29 | .17 | 1.00 | ||||||
| N | .77 | .78 | .41 | .61 | 1.00 | |||||
| E | −.44 | −.16 | .02 | −.72 | −.49 | 1.00 | ||||
| PC | −.54 | −.64 | −.43 | −.40 | −.66 | .30 | 1.00 | |||
| TAF | .24 | .28 | .48 | .18 | .25 | −.07 | −.30 | 1.00 | ||
| IoU | .62 | .54 | .36 | .47 | .66 | −.31 | −.60 | .28 | 1.00 | |
| DAS | .50 | .51 | .34 | .55 | .68 | −.34 | −.53 | .31 | .64 | 1.00 |
Note. DEP = depression, GAD = generalized anxiety disorder, OCD = obsessive-compulsive disorder, SOC = social phobia, N = neuroticism, E = extraversion, PC = perceived control, TAF = thought-action fusion, IoU = intolerance of uncertainty, DAS = dysfunctional attitudes. All correlations ≥ |.16| significant at p = .001.
Table 3.
Tests of the Differential Magnitude of Correlations Between DSM-IV Disorder Constructs and Dimensions of Disorder-Specific Vulnerability
| Disorder- Specific Vulnerability |
DSM-IV Disorder Construct
|
|||
|---|---|---|---|---|
| DEP | GAD | OCD | SOC | |
| TAF | .24b,c | .28b | .48a | .18c |
| IoU | .62a | .54b | .36c | .47b |
| DAS | .50a | .51a | .34b | .55a |
Note. DEP = depression, GAD = generalized anxiety disorder, OCD = obsessive-compulsive disorder, SOC = social phobia, TAF = thought-action fusion, IoU = intolerance of uncertainty, DAS = dysfunctional attitudes. Correlations within the same row that share a superscript letter do not differ in their relative magnitude as determined by the Steiger z-test procedure (ps < .05); e.g., although significantly different from OCD, the latent dimensions of DEP, GAD, and SOC do not differ in their strength of association with DAS.
Structural Models
A series of structural regression models was conducted to evaluate the specificity and unique contribution of the triple vulnerability dimensions in the prediction of the DSM-IV disorder constructs. The structural models were specified in a hierarchical fashion. In the first model, the DSM-IV disorder factors were regressed on the dimensions of general biological vulnerability (Neuroticism, Extraversion). The dimension of general psychological vulnerability (Perceived Control) was added as a predictor in the second model. The incremental predictive utility of each disorder-specific vulnerability was then evaluated in the last three models. In all models, the residuals of the DSM-IV endogenous variables were permitted to freely covary. The global goodness of fit and structural parameter estimates of interest (completely standardized) of the models are presented in Table 4.
Table 4.
Specificity and Strength of the Contribution of the Triple Vulnerability Dimensions in the Prediction of the DSM-IV Disorder Constructs
| DEP | GAD | OCD | SOC | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| γ* | SEγ* | γ* | SRγ* | γ* | SEγ* | γ* | SEγ* | |||
| 1. General Biological Vulnerability Dimensions | ||||||||||
| Neuroticism | .73*** | .03 | .94*** | .04 | .56*** | .05 | .34*** | .04 | ||
| Extraversion | −.08† | .04 | .30*** | .04 | .29*** | .05 | −.55*** | .04 | ||
| R2 | .60*** | .03 | .70*** | .05 | .24*** | .04 | .61*** | .03 | ||
| 2. General Psychological Vulnerability | ||||||||||
| Neuroticism | .70*** | .05 | .79*** | .06 | .35*** | .07 | .34*** | .05 | ||
| Extraversion | −.08† | .04 | .28*** | .04 | .27*** | .05 | −.55*** | .04 | ||
| Perceived Control | −.06 | .05 | −.20*** | .06 | −.28*** | .06 | −.01 | .05 | ||
| R2 | .61*** | .03 | .70*** | .05 | .28*** | .04 | .61*** | .03 | ||
| 3. Disorder-Specific Vulnerability: Thought-Action Fusion | ||||||||||
| Neuroticism | .69*** | .05 | .79*** | .06 | .33*** | .07 | .33*** | .05 | ||
| Extraversion | −.09* | .04 | .28*** | .04 | .26*** | .05 | −.55*** | .04 | ||
| Perceived Control | −.05 | .05 | −.18*** | .06 | −.18** | .07 | −.00 | .05 | ||
| Thought-Action Fusion | .05 | .03 | .05 | .03 | .36*** | .05 | .06 | .03 | ||
| R2 | .61*** | .03 | .70*** | .05 | .39*** | .04 | .61*** | .03 | ||
| 4. Disorder-Specific Vulnerability: Intolerance of Uncertainty | ||||||||||
| Neuroticism | .61*** | .05 | .79*** | .07 | .32*** | .08 | .27*** | .06 | ||
| Extraversion | −.08* | .04 | .28*** | .04 | .27*** | .05 | −.55*** | .04 | ||
| Perceived Control | −.00 | .05 | −.20*** | .06 | −.26*** | .07 | .03 | .05 | ||
| Intolerance of Uncertainty | .19*** | .04 | −.02 | .05 | .08 | .06 | .14** | .05 | ||
| R2 | .63*** | .03 | .70*** | .05 | .28*** | .04 | .62*** | .03 | ||
| 5. Disorder-Specific Vulnerability: Dysfunctional Attitudes | ||||||||||
| Neuroticism | .72*** | .06 | .81*** | .07 | .32*** | .08 | .22*** | .06 | ||
| Extraversion | −.09* | .04 | .28*** | .04 | .27*** | .05 | −.55*** | .04 | ||
| Perceived Control | −.06 | .05 | −.21*** | .06 | −.28*** | .07 | .01 | .05 | ||
| Dysfunctional Attitudes | −.05 | .04 | −.05 | .05 | .06 | .05 | .21*** | .04 | ||
| R2 | .61*** | .03 | .70*** | .05 | .28*** | .04 | .63*** | .03 | ||
Note. DEP = depression, GAD = generalized anxiety disorder, OCD = obsessive-compulsive disorder, SOC = social phobia, γ*= completely standardized path coefficient. Overall fit of models, Model 1: χ2(100) = 397.61, p < .001, SRMR = .04, RMSEA = 0.06 (90% CI = 0.06 to 0.07), TLI = 0.94, CFI = .96; Model 2: χ2(111) = 463.70, p < .001, SRMR = .04, RMSEA = 0.07 (90% CI = 0.06 to 0.07), TLI = 0.93, CFI = .95; Model 3: χ2(122) = 488.50, p < .001, SRMR = .04, RMSEA = 0.07 (90% CI = 0.06 to 0.07), TLI = 0.93, CFI = .95; Model 4: γ2(122) = 470.83, p < .001, SRMR = .04, RMSEA = 0.06 (90% CI = 0.06 to 0.07), TLI = 0.94, CFI = .95; Model 5: γ2(122) = 497.38, p < .001, SRMR = .04, RMSEA = 0.07 (90% CI = 0.06 to 0.07), TLI = 0.93, CFI = .95.
p = .052
p < .05
p < .01
p < .001
General biological vulnerability model
Consistent with prediction and prior research (e.g., Brown, 2007), each DSM-IV disorder construct was significantly predicted by Neuroticism (all ps < .001), with the strongest direct effects found for GAD and DEP (γs = .94 and .73, respectively). As expected, the direct effects of Extraversion on DEP and SOC were negatively signed (γs = -.55 and -.08, respectively) indicating that extraverted temperament was inversely associated with severity of social phobia and depression. However, whereas Extraversion was strongly associated with SOC (p < .001), the path from Extraversion to DEP approached statistical significance (p = .052). In addition, although GAD and OCD evidenced negligible zero-order relationships with Extraversion (rs = −.16 and .02, respectively; cf. Table 2), suppressor effects were obtained in the structural regression model. Specifically, holding Neuroticism constant, Extraversion had a positive direct effect on both GAD and OCD (γs = .30 and .29, respectively; ps < .001).2
General psychological vulnerability model
The second structural regression model examined whether Perceived Control uniquely contributed to the prediction of the four DSM-IV disorder constructs holding Neuroticism and Extraversion constant. As seen in Table 4, significant paths from Perceived Control were obtained for GAD and OCD (γs = −.20 and −.28, respectively; ps < .001), but not for DEP and SOC. Per the standards of Cohen (1988), Perceived Control exerted a weak effect on GAD and a small effect on OCD (f2s = .003 and .06, respectively). All paths from Neuroticism and Extraversion to the DSM-IV disorder factors that were statistically significant in the genetic vulnerability model remained significant when Perceived Control was included as an exogenous variable.
Disorder-specific vulnerability models
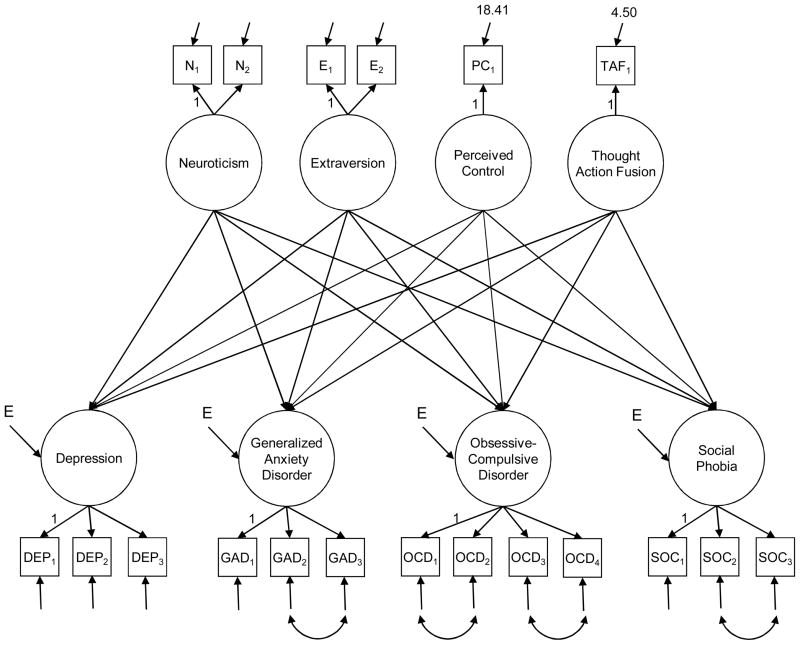
The final set of structural regression models addressed whether the putative disorder-specific vulnerabilities (TAF, IoU, DAS) contributed significantly to the prediction of the DSM-IV disorder latent variables holding the general vulnerability dimensions constant. A path diagram depicting the specification of these final structural models is presented in Figure 1, using TAF as an example (the other two structural models were specified in the same fashion, replacing TAF with a different disorder-specific vulnerability). In each of these three models, the paths from Neuroticism, Extraversion, and Perceived Control to the DSM-IV disorder factors that were statistically significant in the previous models remained significant with the inclusion of the disorder-specific vulnerability predictor. In fact, the path from Extraversion to DEP that had approached significance in the previous models (ps = .052) was statistically significant in each of the disorder-specific vulnerability models (all ps < .05), although this effect continued to be small.
Figure 1.
Structural and Measurement Model of Triple Vulnerability Model Using Thought- Action Fusion as Disorder-Specific Vulnerability. N1 = NEO Five-Factor Inventory (NFFI) Neuroticism, N2 = Eysenck Personality Questionnaire (EPQ) Neuroticism, E1 = NFFI Extraversion, E2 = EPQ Extraversion, PC1 = Anxiety Control Questionnaire-Revised Total, TAF1 = Thought-Action Fusion Total, DEP = Depression, GAD = Generalized Anxiety Disorder, OCD = Obsessive-Compulsive Disorder, SOC = Social Phobia, DEP1 = Depression from Depression Anxiety Stress Scales; DEP2 = Beck Depression Inventory, DEP3 = Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L) major depression; GAD1 = Penn State Worry Questionnaire, GAD2 = ADIS-IV-L excessive worry, GAD3 = ADIS-IV-L uncontrollability of worry, OCD1 = Obsession-Compulsions Inventory – Revised (OCI-R) Obsessions, OCD2 = OCI-R Neutralizing, OCD3 = ADIS-IV-L obsessions, OCD4 = ADIS-IV-L compulsions, SOC1 = Albany Panic and Phobia Questionnaire Social Fears, SOC2 = ADIS-IV-L fear of social situations, SOC3 = ADIS-IV-L social phobia interference/distress. Although not shown in the path diagram for presentational clarity, all covariances among exogenous variables and all covariances among endogenous variable disturbances were freely estimated.
Consistent with the conceptualization of thought-action fusion as a dimension germane to the etiology and maintenance of OCD, the TAF→ OCD path was statistically significant (p < .001) and resulted in an R2 change of .11 (f 2 = .19, a medium effect per Cohen, 1988). TAF did not contribute significantly to the prediction of any other DSM-IV disorder latent variable (Table 4). Counter to conceptualization, IoU did not explain significant unique variance in the GAD latent variable (p = .72). However, IoU exerted small, yet statistically significant, direct effects on DEP and SOC (γs = .19 and .14, respectively; f 2s = .05 and .03). Similarly, the posited direct effect of DAS on DEP was nonsignificant (p = .28). Although DAS also did not account for significant unique variance in GAD and OCD, the DAS→ SOC path was statistically significant (γ = .21, p < .001, f 2 =.06).
Discussion
The present study is the first to undertake a comprehensive evaluation of the contributions of various dimensions derived from the triple vulnerability model (Barlow, 2002) to the prediction of multiple DSM-IV anxiety and mood disorder constructs. Indeed, whereas a multitude of vulnerability dimensions has been proposed and studied in the clinical literature, rarely have such constructs been studied together to examine their unique and specific contributions to emotional disorder psychopathology. Among other limitations, studies that examine vulnerability dimensions in isolation do not address the discriminant validity of these constructs in relation to one another and to dimensions of psychopathology. For instance, the distinctiveness of some purported lower-order vulnerabilities could be questioned based on the concern that the dimensions are actually specific features of a broader diathesis (e.g., is intolerance of uncertainty merely a more elaborated facet of neuroticism?). Similar concerns may arise with regard to the distinction between dimensions of vulnerability and emotional disorders (e.g., do thought-action fusion and OCD reflect the same underlying process?; cf. the continuity/spectrum explanation for the nature of relationship between vulnerability and psychopathology; Widiger & Smith, 2008).
As researchers have previously noted (e.g., Brown, 2007), discriminant validation may be complicated in studies of clinical participants, because the associations among measures of vulnerability and psychopathology can be enhanced by general distress (i.e., mood-state distortion; cf. Clark, Vittengl, Kraft, & Jarrett, 2003; Widiger & Smith, 2008). Nevertheless, the current results indicated that the selected dimensions of vulnerability did not evidence excessive overlap with one another or with the DSM-IV disorder constructs (e.g., range of intercorrelations among vulnerability dimensions was -.07 to .68; cf. Table 2). Although these relationships were estimated adjusting for measurement error in each construct, a limitation of these analyses was that several vulnerability dimensions were represented by one indicator. A more compelling evaluation of the convergent and discriminant validity of the triple vulnerability dimensions would entail a latent variable measurement model where every construct was assessed by multiple measures from different sources (e.g., a multitrait-multimethod analysis; cf. Kollman, Brown, & Barlow, 2009). Whereas a variety of instruments have been developed to assess temperament, this is not the case for the putative lower-order vulnerabilities that are almost without exception represented in the extant literature by a single measurement scale (e.g., intolerance of uncertainty, thought-action fusion). Although most measures of lower-order vulnerability have been shown to be multifactorial, we opted to model these vulnerabilities as single indicators, using the broadest and psychometrically strongest dimension from each instrument (e.g., higher-order factors of Perceived Control and Thought-Action Fusion rather than the subdomains of these scales). However, this approach should be considered with the caveats that evidence for the latent structure of some measures is not unequivocal (e.g., DAS), and that it does not address the possibility that the vulnerability subdomains are differentially related to the DSM-IV disorder constructs (cf. Footnote 3).
In addition to discriminant validity, a key question is to what extent do the triple vulnerability dimensions contribute to the prediction of the emotional disorders. In this regard, it is important to underscore the finding that the general biological vulnerability dimensions (neuroticism, extraversion) exerted the strongest effects on the DSM-IV disorder constructs (e.g., range of R2 = .24 to .70; cf. Table 4). In accord with prediction and prior research evidence, Neuroticism had significant direct effects on each disorder construct but was most strongly associated with GAD and DEP (e.g., Brown, 2007; Watson et al., 2005). Extraversion had inverse relationships with only SOC and DEP, but was most strongly related to SOC (cf. Naragon-Gainey et al., 2009; Rosellini & Brown, 2011). Moreover the posited structural relationships between dimensions of general biological vulnerability and psychopathology remained significant (and strong) after lower-order dimensions were added to the structural models. However, in addition to these predicted relationships, two unexpected suppressor effects were obtained. Specifically, Extraversion had significant direct effects in a positive direction on GAD and OCD in the structural models (despite negligible relationships at the zero-order level; cf. Table 2). There is no precedent for this result in similar multivariate models that examined directional paths between Extraversion and GAD or OCD when controlling for neuroticism (e.g., Rosellini & Brown, 2011; van der Heiden et al., 2010). Although these suppressor effects were consistent across subsamples and indicators in the current study (see Footnote 2), further research is needed to ascertain their replicability and substantive importance.
In contrast to temperament (general biological vulnerability), the lower-order dimensions of vulnerability, while in many cases statistically significant, often contributed weakly to the prediction of the DSM-IV disorder constructs. For instance, although the general psychological vulnerability construct of Perceived Control was distinct from Neuroticism (r = -.66) and Extraversion (r = .30), it contributed significantly to the prediction of just two of the four disorders (GAD, OCD). However, in both instances, the size of the direct effect was small (f 2 = 0.00 and 0.06 for GAD and OCD, respectively). These findings do not provide strong support for the conceptual position that perceived control is germane to the full range of emotional disorders. Perceived Control evidenced moderate zero-order relationships with the DSM-IV disorder constructs (range of rs = -.40 to -.64), but contributed negligibly to the prediction of the disorders in the structural regression models. Thus, although Perceived Control had considerable covariance with the DSM-IV disorder constructs, findings from the structural regression models indicate that virtually all of this explanatory variance is shared with dimensions of temperament, primarily Neuroticism. Although the effects were weak, it is noteworthy that Perceived Control was uniquely predictive of GAD and OCD, disorders that are phenotypically similar with regard to a lack of control over internal states (i.e., excessive worry, obsessions). Perhaps this finding indicates that the predictive role of the Perceived Control construct is strongest for this specific aspect of emotional disorder psychopathology (i.e., control over cognitive-emotional states).3
The disorder-specific vulnerability dimensions in the current study were selected based on their prominence in literature as putative risk factors for specific emotional disorders. Despite the fact that each disorder-specific vulnerability has received considerable research attention, very few studies have examined their contribution to the prediction of psychopathology over and beyond broader, well-established diatheses (e.g., dimensions of temperament such as neuroticism). As with Perceived Control, the current results indicate that, in most instances, the disorder-specific vulnerability dimensions did not exert appreciable, unique effects on the DSM-IV disorder constructs and did not do so in a fashion that was in accord with their posited specificity (e.g., IoU contributed to the prediction of DEP and SOC, but not GAD or OCD).
The exception was TAF, which in addition to having a stronger zero-order relationship to OCD than the other DSM-IV disorder constructs at the zero-order level, had a moderate-sized (f 2 = .18) directional effect on OCD holding dimensions of temperament and perceived control constant. In addition, this structural relationship was specific to OCD (i.e., TAF did not contribute to the prediction of the other three DSM-IV constructs). Although TAF is routinely associated with OCD (e.g., Amir et al., 2001; Meyer & Brown, in press; Shafran et al., 1996), previous findings have cast doubt on the specificity of this relationship (e.g., TAF does not differentiate OCD from other anxiety and mood disorders; Rassin, Diepstraten, et al., 2001; Rassin, Merckelback, et al., 2001). However, most previous clinical studies of TAF have entailed smaller, univariate analyses conducted at the diagnostic level. It could be argued that the current multivariate analyses rendered a more compelling evaluation of the relationship between TAF and DSM-IV emotional disorder psychopathology because both the vulnerability and disorder constructs were represented dimensionally (which captured individual differences in severity that were adjusted for measurement error) and were examined in context of a broader structural model (which explicated the unique and specific contributions of TAF to DSM-IV psychopathology after controlling for dimensions of shared vulnerability). Nevertheless, more research is needed to replicate this finding and further elucidate the nature of this relationship (e.g., does TAF have a unique direct effect on the temporal course of OCD?).
Despite IoU’s original conceptualization as a specific vulnerability factor, the present findings are consistent with prior evidence that this construct is not differentially related to GAD (e.g., Gentes & Ruscio, 2011; Norton & Mehta, 2007). At the zero-order level, IoU was more strongly related to DEP than to GAD; although the relationship between IoU and GAD was the second largest in magnitude, the strength of this association differed only from OCD. Based on similar findings that IoU has moderate associations with a range of anxiety and mood disorders, it has been suggested that IoU might be better construed as a general diathesis (Gentes & Ruscio, 2011). However, this contention may be challenged by the results from the structural regression model indicating that IoU did not contribute substantially to the prediction of the DSM-IV disorder constructs after controlling for broader dimensions of vulnerability (i.e., no direct effects on GAD and OCD; weak effects on DEP and SOC, f 2s ≤ .05). Similarly, the current results did not support the conceptualization of dysfunctional attitudes as a specific risk factor for depression. DAS had comparable relationships with DEP, GAD, and SOC in the zero-order analyses, and contributed only to the prediction of SOC in the structural regression analyses. The differential (albeit weak) association with SOC might be accounted for by the fact that a large number of items on the Dysfunctional Attitudes Scale assess perfectionism and the need for social approval (cf. Cane, Olinger, Gotlib, & Kuiper, 1986; Imber et al., 1990; Oliver & Baumgart, 1985), dimensions salient to the psychopathology of social phobia (e.g., Juster et al., 1996; Rosser, Issakidis, & Peters, 2003; Shahar & Gilboa-Shechtman, 2007). Although perhaps further underscoring common features of social phobia and the unipolar mood disorders (in addition to sharing the risk factor of low extraversion, social phobia and depression are associated with similar dysfunctional thought content), the inability of DAS to distinguish DEP from other emotional disorder constructs may be due to the fact that the Dysfunctional Attitudes Scale does not sufficiently measure the third element of Beck’s cognitive triad, hopelessness about the future. Given evidence that hopelessness is relatively specific to depression (e.g., Alloy, Kelly, Mineka, & Clements, 1990; Beck, Wenzel, Riskind, Brown, & Steer, 2006; Miranda, Fontes, & Marroquín, 2008), assessment of dysfunctional attitudes with more emphasis on assumptions about the future may foster a differential relationship with the mood disorders.
The current findings provide additional support for the relevance of neuroticism and extraversion in accounting for individual differences in the severity of the emotional disorders. These results also suggest that, with the exception of TAF, the lower-order constructs of vulnerability contribute modestly to the prediction of psychopathology over broader dimensions of temperament. This pattern of results could be interpreted in support of the current movement towards transdiagnostic treatments for emotional disorders that target the broader, common features of disorders over disorder-specific elements (e.g., Barlow et al., 2011). Nevertheless, it is important to underscore that the current study tested one possible realization of the triple vulnerability model. Although the measures used to represent the general biological and psychology vulnerabilities correspond directly to the constructs named in the triple vulnerability model (Barlow, 2002), there are a variety of other measures that could be selected to represent disorder-specific vulnerabilities (e.g., sociotropy/autonomy in depression). The selection of different disorder-specific vulnerability constructs may lead to different conclusions about their incremental validity in the prediction of psychopathology. Thus, it would be informative to evaluate alternative specifications of the triple vulnerability model in future research.
In addition to the aforementioned limitations (e.g., some vulnerability dimensions represented by single indicators), these findings should be interpreted keeping in mind the study’s use of a clinical sample and a cross-sectional design. These design aspects precluded a more compelling evaluation of the various explanations for the relationships between putative dimensions of vulnerability and emotional disorder psychopathology (e.g., does TAF have a predispositional influence on OCD or simply covary with OCD symptom severity?). Moreover, it is possible that the size of the relationships between dimensions of vulnerability and psychopathology is under-stated in clinical samples; i.e., if a dimension truly operates as a diathesis, it may have its strongest effect on psychopathology as a predispositional influence. Nevertheless, research has shown that neuroticism and extraversion predict the longitudinal course of emotional disorder constructs in clinical samples (e.g., Brown, 2007; Brown & Rosellini, 2011). In addition to studies of predispositional effects (e.g., longitudinal studies of the triple vulnerability dimensions in community or at-risk samples), it would be of interest to examine whether the temporal relationships found in clinical samples for neuroticism and extraversion are evident for dimensions of lower-order vulnerability; e.g., does TAF contribute to the maintenance of OCD, over and beyond the influence of neurotic temperament?
Highlights.
A comprehensive evaluation of the Barlow triple vulnerability model of emotional disorders was undertaken in a sample of 700 outpatients
Of the various vulnerabilities, the general biological vulnerabilities (neuroticism, extraversion) were most strongly predictive of the emotional disorders
General psychological vulnerability (perceived control) contributed to the prediction of GAD and OCD, beyond dimensions of temperament
Of the various disorder-specific vulnerabilities, only thought-action fusion contributed to the prediction of disorders in accord with theory
Footnotes
Although the terminology used by Barlow (2000, 2002) in the triple vulnerability model emphasizes certain etiologies for the different vulnerability dimensions (e.g., the term “general biological vulnerability” is used in reference to neuroticism and extraversion given evidence for the strong genetic basis of these temperaments), the extant literature indicates that each vulnerability dimension would be best viewed as multiply determined by some combination of genetic diatheses and learned experiences.
Follow-up analyses were conducted to address the robustness of this unexpected finding. Specifically, the general biological vulnerability structural model was re-analyzed several times using: (a) split-halved samples (ns = 350), and (b) single indicators (NFFI, EPQ) to represent the Extraversion construct. In each instance, Extraversion continued to have a positive direct effect on GAD and OCD (range of γs = .20 to .36, all ps < .001).
To further address this notion, the general psychological vulnerability models were re-conducted using each of three ACQ-R subdomain factors instead of the higher-order dimension of Perceived Control (holding Neuroticism and Extraversion constant). In support of this suggestion, ACQ-R Emotional Control was more strongly predictive of GAD and OCD (γs = −.38 and −.28, respectively) than the ACQ-R subdomains of perceived control over external situations (Threat Control, Stress Control; range of γs = −.002 to −.23).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramowitz JS, Whiteside S, Lynam D, Kalsy S. Is thought–action fusion specific to obsessive-compulsive disorder? A mediating role of negative affect. Behaviour Research and Therapy. 2003;41:1069–1079. doi: 10.1016/s0005-7967(02)00243-7. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Panzarella C, Rose DT. Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2006;115:145–156. doi: 10.1037/0021-843X.115.1.145. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Kelly KA, Mineka S, Clements CM. Comorbidity in anxiety and depressive disorders: A helplessness-hopelessness perspective. In: Maser JD, Cloninger CR, editors. Comorbidity in anxiety and mood disorders. Washington, DC: American Psychiatric Press; 1990. pp. 499–543. [Google Scholar]
- Amir N, Freshman M, Ramsey B, Neary E, Brigidi B. Thought–action fusion in individuals with OCD symptoms. Behaviour Research and Therapy. 2001;39:765–776. doi: 10.1016/s0005-7967(00)00056-5. [DOI] [PubMed] [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Barlow DH. Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist. 2000;55:1247–1263. doi: 10.1037//0003-066x.55.11.1247. [DOI] [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. [Google Scholar]
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May J. The unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York: Oxford University Press; 2011. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beck AT, Wenzel A, Riskind JH, Brown G, Steer RA. Specificity of hopelessness about resolving life problems: Another test of the cognitive model of depression. Cognitive Therapy and Research. 2006;30:773–781. [Google Scholar]
- Berle D, Starcevic V. Thought-action fusion: Review of the literature and future directions. Clinical Psychology Review. 2005;25:263–284. doi: 10.1016/j.cpr.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Bienvenu OJ, Hettema JM, Neale MC, Prescott CA, Kendler KS. Low extraversion and high neuroticism as indices of genetic and environmental risk for social phobia, agoraphobia, and animal phobia. American Journal of Psychiatry. 2007;164:1714–1721. doi: 10.1176/appi.ajp.2007.06101667. [DOI] [PubMed] [Google Scholar]
- Boelen PA, Reijntjes A. Intolerance of uncertainty and social anxiety. Journal of Anxiety Disorders. 2009;23:130–135. doi: 10.1016/j.janxdis.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Boelen PA, Vrinssen I, van Tulder F. Intolerance of uncertainty in adolescents: Correlations with worry, social anxiety, and depression. Journal of Nervous and Mental Disease. 2010;198:194–200. doi: 10.1097/NMD.0b013e3181d143de. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York: Guilford Press; 2006. [Google Scholar]
- Brown TA. Temporal course and structural relationships among dimensions of temperament and DSM-IVanxiety and mood disorder constructs. Journal of Abnormal Psychology. 2007;116:313–328. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour Research and Therapy. 1992;30:33–37. doi: 10.1016/0005-7967(92)90093-v. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. A proposal for a dimensional classification system based on the shared features of the DSM-IVanxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment. 2009;21:256–271. doi: 10.1037/a0016608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IVanxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IVanxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Brown TA, Rosellini AJ. The direct and interactive effects of neuroticism and life stress on the severity and longitudinal course of depressive symptoms. Journal of Abnormal Psychology. 2011;120:844–856. doi: 10.1037/a0023035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, White KS, Barlow DH. A psychometric reanalysis of the Albany Panic and Phobia Questionnaire. Behaviour Research and Therapy. 2005;43:337–355. doi: 10.1016/j.brat.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Brown TA, White KS, Forsyth JP, Barlow DH. The structure of perceived emotional control: Psychometric properties of a revised Anxiety Control Questionnaire. Behavior Therapy. 2004;35:75–99. [Google Scholar]
- Buhr K, Dugas MJ. The Intolerance of Uncertainty Scale: Psychometric properties of the English version. Behaviour Research and Therapy. 2002;40:931–945. doi: 10.1016/s0005-7967(01)00092-4. [DOI] [PubMed] [Google Scholar]
- Cane DB, Olinger LJ, Gotlib IH, Kuiper NA. Factor structure of the dysfunctional attitude scale in a student population. Journal of Clinical Psychology. 1986;42:307–309. [Google Scholar]
- Carleton RN, Collimore KC, Asmundson GJG. ‘It’s not just the judgments—it’s that I don’t know’: Intolerance of uncertainty as a predictor of social anxiety. Journal of Anxiety Disorders. 2010;24:189–195. doi: 10.1016/j.janxdis.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, Joormann J. Serotonergic function, two-mode models of self-regulation, and vulnerability to depression: What depression has in common with impulsive aggression. Psychological Bulletin. 2008;134:912–943. doi: 10.1037/a0013740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman LK, Kertz SJ, Woodruff-Borden J. A structural equation model analysis of perceived control and psychological distress on worry among African American and European American young adults. Journal of Anxiety Disorders. 2009;23:69–76. doi: 10.1016/j.janxdis.2008.03.018. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Barlow DH. The development of anxiety: The role of control in the early environment. Psychological Bulletin. 1998;124:3–21. doi: 10.1037/0033-2909.124.1.3. [DOI] [PubMed] [Google Scholar]
- Clark LA, Vittengl J, Kraft D, Jarrett RB. Separate personality traits from states to predict depression. Journal of Personality Disorders. 2003;17:152–172. doi: 10.1521/pedi.17.2.152.23990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Coles ME, Mennin DS, Heimberg RG. Distinguishing obsessive features and worries: The role of thought-action fusion. Behaviour Research and Therapy. 2001;39:947–959. doi: 10.1016/s0005-7967(00)00072-3. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. NEO PI-R Professional Manual: Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) Odessa FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Craighead WE, Sheets ES, Craighead LW, Madsen JW. Recurrence of MDD: A prospective study of personality pathology and cognitive distortions. Personality Disorders: Theory, Research, and Treatment. 2011;2:83–97. doi: 10.1037/a0020456. [DOI] [PubMed] [Google Scholar]
- Cribbie RA. Multiplicity control in structural equation modeling. Structural Equation Modeling. 2007;14:98–112. [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) New York: Oxford University Press; 1994. [Google Scholar]
- Dugas MJ, Ladouceur R. Treatment of GAD: Targeting intolerance of uncertainty in two types of worry. Behavior Modification. 2000;24:635–657. doi: 10.1177/0145445500245002. [DOI] [PubMed] [Google Scholar]
- Dugas MJ, Robichaud M. Cognitive–behavioral treatment for generalized anxiety disorder: From science to practice. New York: Routledge; 2007. [Google Scholar]
- Eysenck HJ, Eysenck SBG. Manual of the Eysenck Personality Questionnaire (adult and junior) London: Hodder & Stoughton; 1975. [Google Scholar]
- Fanous A, Gardner CO, Prescott CA, Cancro R, Kendler KS. Neuroticism, major depression, and gender: A population-based twin study. Psychological Medicine. 2002;32:719–728. doi: 10.1017/s003329170200541x. [DOI] [PubMed] [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, Salkovskis PM. The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment. 2002;14:485–495. [PubMed] [Google Scholar]
- Freeston MH, Rhéaume J, Letarte H, Dugas MJ, Ladouceur R. Why do people worry? Personality and Individual Differences. 1994;17:791–802. [Google Scholar]
- Gentes EL, Ruscio AM. A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive-compulsive disorder. Clinical Psychology Review. 2011;31:923–933. doi: 10.1016/j.cpr.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Gershuny BS, Sher KJ. The relation between personality and anxiety: Findings from a 3-year prospective study. Journal of Abnormal Psychology. 1998;107:252–262. doi: 10.1037//0021-843x.107.2.252. [DOI] [PubMed] [Google Scholar]
- Gould CE, Edelstein BA. Worry, emotion control, and anxiety control in older and young adults. Journal of Anxiety Disorders. 2010;24:759–766. doi: 10.1016/j.janxdis.2010.05.009. [DOI] [PubMed] [Google Scholar]
- Hamilton EW, Abramson LY. Cognitive patterns and major depressive disorder: A longitudinal study in a hospital setting. Journal of Abnormal Psychology. 1983;92:173–184. doi: 10.1037//0021-843x.92.2.173. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Miller N, Haeffel GJ. Cognitive vulnerability-stress theories of depression: Examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cognitive Therapy and Research. 2004;28:309–345. [Google Scholar]
- Hazlett-Stevens H, Zucker BG, Craske MG. The relationship of thought–action fusion to pathological worry and generalized anxiety disorder. Behaviour Research and Therapy. 2002;40:1199–1204. doi: 10.1016/s0005-7967(01)00138-3. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry. 2006;163:857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, Kendler KS. Genetic and environmental sources of covariation between generalized anxiety disorder and neuroticism. American Journal of Psychiatry. 2004;161:1581–1587. doi: 10.1176/appi.ajp.161.9.1581. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Kendall PC, Lumry A. Specificity of depressotypic cognitions in clinical depression. Journal of Abnormal Psychology. 1986;95:52–59. doi: 10.1037//0021-843x.95.1.52. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Imber SD, Pilkonis PA, Sotsky SM, Elkin I, Watkins JT, Collins JF, et al. Mode-specific effects among three treatments for depression. Journal of Consulting and Clinical Psychology. 1990;58:352–359. doi: 10.1037//0022-006x.58.3.352. [DOI] [PubMed] [Google Scholar]
- Juster HR, Heimberg RG, Frost RO, Holt CS, Mattia JI, Faccenda K. Social phobia and perfectionism. Personality and Individual Differences. 1996;21:403–410. [Google Scholar]
- Koerner N, Dugas MJ. A cognitive model of generalized anxiety disorder: The role of intolerance of uncertainty. In: Davey GCL, Wells A, editors. Worry and Its psychological disorders: Theory, assessment and treatment. Chichester, West Sussex, United Kingdom: Wiley; 2006. pp. 201–216. [Google Scholar]
- Kollman DM, Brown TA, Barlow DH. The construct validity of acceptance: A multitrait-multimethod investigation. Behavior Therapy. 2009;40:205–218. doi: 10.1016/j.beth.2008.06.002. [DOI] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33:335–342. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Meng XL, Rosenthal R, Rubin DB. Comparing correlated correlation coefficients. Psychological Bulletin. 1992;111:172–175. [Google Scholar]
- Meuret AE, Rosenfield D, Seidel A, Bhaskara L, Hofmann SG. Respiratory and cognitive mediators of treatment change in panic disorder: Evidence for intervention specificity. Journal of Clinical and Consulting Psychology. 2010;78:691–704. doi: 10.1037/a0019552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer JF, Brown TA. Psychometric properties of the Thought-Action Fusion scale in a large clinical sample. Assessment. doi: 10.1177/1073191112436670. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Miranda R, Fontes M, Marroquín B. Cognitive content-specificity in future expectations: Role of hopelessness and intolerance of uncertainty in depression and GAD symptoms. Behaviour Research and Therapy. 2008;46:1151–1159. doi: 10.1016/j.brat.2008.05.009. [DOI] [PubMed] [Google Scholar]
- Moulding R, Kyrios M, Doron G, Nedeljkovic M. Mediated and direct effects of general control beliefs on obsessive compulsive symptoms. Canadian Journal of Behavioural Science. 2009;41:84–92. [Google Scholar]
- Muthén LK, Muthén BO. Mplus 6.11 [Computer software] Los Angeles: Author; 1998–2011. [Google Scholar]
- Naragon-Gainey K, Watson D, Markon KE. Differential relations of depression and social anxiety symptoms to the facets of extraversion/positive emotionality. Journal of Abnormal Psychology. 2009;118:299–310. doi: 10.1037/a0015637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ, Mehta PD. Hierarchical model of vulnerabilities for emotional disorders. Cognitive Behaviour Therapy. 2007;36:240–254. doi: 10.1080/16506070701628065. [DOI] [PubMed] [Google Scholar]
- Norton PJ, Sexton KA, Walker JR, Norton GR. Hierarchical model of vulnerabilities for anxiety: replication and extension with a clinical sample. Cognitive Behaviour Therapy. 2005;34:49–63. doi: 10.1080/16506070410005401. [DOI] [PubMed] [Google Scholar]
- Ohrt T, Sjödin I, Thorell LH. Cognitive distortions in panic disorder and major depression: Specificity for depressed mood. Nordic Journal of Psychiatry. 1999;53:459–464. [Google Scholar]
- Oliver JM, Baumgart EP. The Dysfunctional Attitude Scale: Psychometric properties and relation to depression in an unselected adult population. Cognitive Therapy and Research. 1985;9:161–167. [Google Scholar]
- Rapee RM, Craske MG, Barlow DH. Assessment instrument for panic disorder that includes fear of sensation-producing activities: The Albany Panic and Phobia Questionnaire. Anxiety. 1994/1995;1:114–122. doi: 10.1002/anxi.3070010303. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Craske MG, Brown TA, Barlow DH. Measurement of perceived control over anxiety-related events. Behavior Therapy. 1996;27:279–293. [Google Scholar]
- Rassin E, Diepstraten P, Merckelbach H, Muris P. Thought–action fusion and thought suppression in obsessive compulsive disorder. Behaviour Research and Therapy. 2001;39:757–764. doi: 10.1016/s0005-7967(00)00051-6. [DOI] [PubMed] [Google Scholar]
- Rassin E, Merkelbach H, Muris P, Schmidt H. The Thought–Action Fusion Scale: Further evidence for its reliability and validity. Behaviour Research and Therapy. 2001;39:537–544. doi: 10.1016/s0005-7967(00)00031-0. [DOI] [PubMed] [Google Scholar]
- Reiter SR, Otto MW, Pollack MH, Rosenbaum JF. Major depression in panic disorder patients with comorbid social phobia. Journal of Affective Disorders. 1991;22:171–177. doi: 10.1016/0165-0327(91)90051-s. [DOI] [PubMed] [Google Scholar]
- Rogers GM, Park JH, Essex MJ, Klein MH, Silva SG, Hoyle RH, et al. The Dysfunctional Attitudes Scale: Psychometric properties in depressed adolescents. Journal of Clinical Child and Adolescent Psychology. 2009;38:781–789. doi: 10.1080/15374410903259007. [DOI] [PubMed] [Google Scholar]
- Rosser S, Issakidis C, Peters L. Perfectionism and social phobia: Relationship between the constructs and impact on cognitive behavior therapy. Cognitive Therapy and Research. 2003;27:143–151. [Google Scholar]
- Rotter JB. Social learning and clinical psychology. Englewood Cliffs, NJ: Prentice-Hall; 1954. [Google Scholar]
- Sanderson WC, Rapee RM, Barlow DH. The influence of perceived control on panic attacks induced via inhalation of 5.5% CO2-enriched air. Archives of General Psychiatry. 1989;46:157–162. doi: 10.1001/archpsyc.1989.01810020059010. [DOI] [PubMed] [Google Scholar]
- Sanz J, Avia MD. Cognitive specificity in social anxiety and depression: Self-statements, self-focused attention, and dysfunctional attitudes. Journal of Social and Clinical Psychology. 1994;13:105–137. [Google Scholar]
- Seligman MEP. Helplessness: On depression, development, and death. San Francisco: Freeman; 1975. [Google Scholar]
- Sexton KA, Dugas MJ. Defining distinct negative beliefs about uncertainty: Validating the factor structure of the Intolerance of Uncertainty Scale. Psychological Assessment. 2009;21:176–186. doi: 10.1037/a0015827. [DOI] [PubMed] [Google Scholar]
- Shafran R, Thordarson DS, Rachman S. Thought–action fusion in obsessive-compulsive disorder. Journal of Anxiety Disorders. 1996;10:379–391. [Google Scholar]
- Shahar G, Gilboa-Shechtman E. Depressive personality styles and social anxiety in young adults. Journal of Cognitive Psychotherapy. 2007;21:275–284. [Google Scholar]
- Shear MK. The concept of uncontrollability. Psychological Inquiry. 1991;2:88–93. [Google Scholar]
- Stapinski LA, Abbott MJ, Rapee RM. Fear and perceived uncontrollability of emotion: Evaluating the unique contribution of emotion appraisal variables to prediction of worry and generalized anxiety disorder. Behaviour Research and Therapy. 2010;48:1097–1104. doi: 10.1016/j.brat.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Suárez LM, Bennett SM, Goldstein CR, Barlow DH. Understanding anxiety disorders from a “triple vulnerability” framework. In: Antony MM, Stein MB, editors. Oxford handbook of anxiety and related disorders. New York: Oxford University Press; 2009. pp. 153–172. [Google Scholar]
- Sutton JM, Mineka S, Zinbarg RE, Craske MG, Griffith JW, Rose RD, Waters AM, Nazarian M, Mor N. The relationships of personality and cognitive styles with self-reported symptoms of depression and anxiety. Cognitive Therapy and Research. 2011;35:381–393. doi: 10.1007/s10608-010-9336-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch MJ, Silverman A, Schmidt NB. Effects of anxiety sensitivity and perceived control on emotional responding to caffiene challenge. Journal of Anxiety Disorders. 1996;10:21–35. [Google Scholar]
- Treanor M, Erisman SM, Salters-Pedneault K, Roemer L, Orsillo SM. Acceptance-based behavioral therapy for GAD: Effects on outcomes from three theoretical models. Depression and Anxiety. 2011;28:127–136. doi: 10.1002/da.20766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Heiden C, Melchior K, Muris P, Bouwmeester S, Bos AER, van der Molen HT. A hierarchical model for the relationships betwene general and specific vulnerability factors and symptom levels of generalized anxiety disorder. Journal of Anxiety Disorders. 2010;24:284–289. doi: 10.1016/j.janxdis.2009.12.005. [DOI] [PubMed] [Google Scholar]
- Viken RJ, Rose RJ, Kaprio J, Koskenvuo M. A developmental genetic analysis of adult personality: Extraversion and neuroticism from 18 to 59 years of age. Journal of Personality and Social Psychology. 1994;66:722–730. doi: 10.1037//0022-3514.66.4.722. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Marshall EC, Gibson LE, Zvolensky MJ. Cognitive-affective characteristics of smokers with and without posttraumatic stress disorder and panic psychopathology. Addictive Behaviors. 2010;35:419–425. doi: 10.1016/j.addbeh.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Gamez W, Simms LJ. Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality. 2005;39:46–66. [Google Scholar]
- Weissman AN, Beck AT. Development and validation of the Dysfunctional Attitudes Scale. Paper presented at the meeting of the Association for the Advancement of Behavior Therapy; Chicago, IL. 1978. [Google Scholar]
- White KS, Brown TA, Somers TJ, Barlow DH. Avoidance behavior in panic disorder: The moderating influence of perceived control. Behaviour Research and Therapy. 2006;44:147–157. doi: 10.1016/j.brat.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Smith GT. Personality and psychopathology. In: John OP, Robins RW, Pervin LA, editors. Handbook of personality: Theory and research. 3. New York: Guilford Press; 2008. pp. 743–769. [Google Scholar]