Abstract
OBJECTIVES
To determine whether adoption of Medicaid case mix reimbursement is associated with greater prevalence of feeding tube use in nursing home (NH) residents.
DESIGN
Secondary analysis of longitudinal administrative data about the prevalence of feeding tube insertion and surveys of states’ adoption of case mix reimbursement.
SETTING
NHs in the United States.
PARTICIPANTS
NH residents at the time of NH inspection between 1993 and 2004.
MEASUREMENTS
Facility prevalence of feeding tubes reported at the state inspection of NHs reported in the Online Survey, Certification and Reporting database and interviews with state policy makers regarding the adoption of case mix reimbursement.
RESULTS
Between 1993 and 2004, 16 states adopted Resource Utilization Group case mix reimbursement. States varied in the prevalence of feeding tubes in their NHs. Although the use of feeding tube increased substantially over the years of the study, once temporal trends and facility fixed effects were accounted for, case mix reimbursement was not associated with greater prevalence of feeding tube use.
CONCLUSION
The adoption of Medicaid case mix reimbursement was not associated with an increase in the prevalence of feeding tube use.
Keywords: state variation, feeding tubes, financial reimbursement, nursing homes, elderly
People who have advanced dementia experience progressive functional decline, often accompanied by swallowing and eating problems, which are typically associated with recurrent aspiration pneumonia, weight loss, and death. The existing evidence suggests that the use of feeding tubes for people with advanced dementia does not improve survival, prevent aspiration pneumonia, or significantly improve other health outcomes.1,2 Nonetheless, there is striking interstate and interfacility variation3,4 in the use of feeding tubes in this population across the United States. It is now known that, in addition to patient preferences, external influences (e.g., state reimbursement policies, facility factors) are important determinants influencing decisions to insert feeding tubes.4,5
Case mix reimbursement provides incentives to increase access to nursing homes (NHs) for the most complex patients by compensating providers more for serving a disproportionate share of patients requiring more clinical resources because of their acuity. Because feeding tube use merits a higher patient acuity classification, it has been hypothesized that the introduction of such a case mix payment formula creates a financial incentive for NHs to insert feeding tubes in persons with advanced dementia, in spite of the lack of evidence that this practice is beneficial for these patients. The fact that the cost of feeding patients with dementia using feeding tubes is only half that of hand feeding further enhances this incentive.6 Thus, it was hypothesized that NHs located in states that implemented Medicaid case mix reimbursement would increase their use of feeding tubes because of the higher per diem payment rates and potential savings in staff time.
The use of Medicaid case mix reimbursement has grown substantially over time, from four states in 1981 to 19 states in 1991 and 35 by 2004. The implementation of case mix reimbursement has been associated with higher acuity of patients at the time of nursing home admission and long-term residents, suggesting better access to NHs for persons with increased disease acuity and functional burden, 7 but it has not been shown to lead to better staffing with resultant improved quality of care.8
The current study used a longitudinal multivariate model to examine whether the rate of feeding tube use increased after the implementation of case mix reimbursement. Between 1993 and 2004, 16 new states adopted case mix reimbursement. Thus, it was possible to examine the prevalence of feeding tube use at the annual NH inspection in the year before and after the implementation of case mix reimbursement. A second objective was to examine the prevalence of feeding tubes used in NHs between 1993 and 2004Fa period of national expansion in percutaneous endoscopic gastrostomy tube use in the adult population.
METHODS
To examine whether case mix reimbursement was associated with change in the rate of feeding tube use, the point prevalence of feeding tubes at the annual NH inspection document in the Online Survey Certification and Reporting (OSCAR) system was examined. This allowed changes in the point prevalence of feeding tubes in all NHs in the United States participating in Medicare and Medicaid between 1993 and 2004 to be tracked. During this time, 16 states (ME, MS, OH, SD, KS, PA, IN, NH, WA, CO, IA, ID, GA, LA, UT, and NC) implemented case mix reimbursement.
Data Sources
The Centers for Medicare and Medicaid Services (CMS) contracts with each state to conduct an onsite inspection with Medicare- and Medicaid-participating NHs in regard to whether they meet the minimum quality standards set by CMS. Inspections occur, on average, every year. Inspection results and aggregate data are collected to characterize the residents of the NH in terms of function, treatments, and services provided on the day of inspection. Organizational characteristics of the NH are also collected as part of the OSCAR database. Information on states’ Medicaid reimbursement policies was collected from a previous study9 and an ongoing survey of states’ Medicaid office staff conducted by the Center for Gerontology and Health Care Research.10
The current analysis was restricted to urban, non-hospital- based NHs located in the 48 contiguous U.S. states (excluding Alaska, Hawaii, the District of Columbia, and other U.S. territories because of the small number of NHs in these areas). Altogether, the final analytical file included 110,881 surveys from 11,002 unique facilities.
Statistical Analysis
The temporal trends in feeding tube use were examined by describing the distribution of the percentage of tube-fed residents per facility in each year using box plots. In addition, the point prevalence of feeding tube use in the 16 states that implemented case mix reimbursement was determined according to year relative to the timing of case mix implementation.
The main analysis used a difference-in-difference multivariate model with facility and time fixed effects to estimate the association between the introduction of case mix reimbursement and the rate of feeding tube use. This model controls for state average Medicaid payment rate, which was adjusted for inflation using the annual Consumer Price Index published by the Bureau of Labor Statistics. To account for regional differences in purchasing power of the Medicaid payment rates and the price of medical and nursing services, the county wage index (for the hospital sector), which the CMS routinely uses to adjust Medicare payment rates for hospitals and NHs, was also included in model. Additionally, the model controls for the temporal trends in feeding tube use according to yearly indicators (time fixed effect), the facility average acuity index reflecting the residents’ dependencies in activities of daily living,11 and proportion of residents in the facility receiving rehabilitation.
RESULTS
Change in Feeding Tube Use
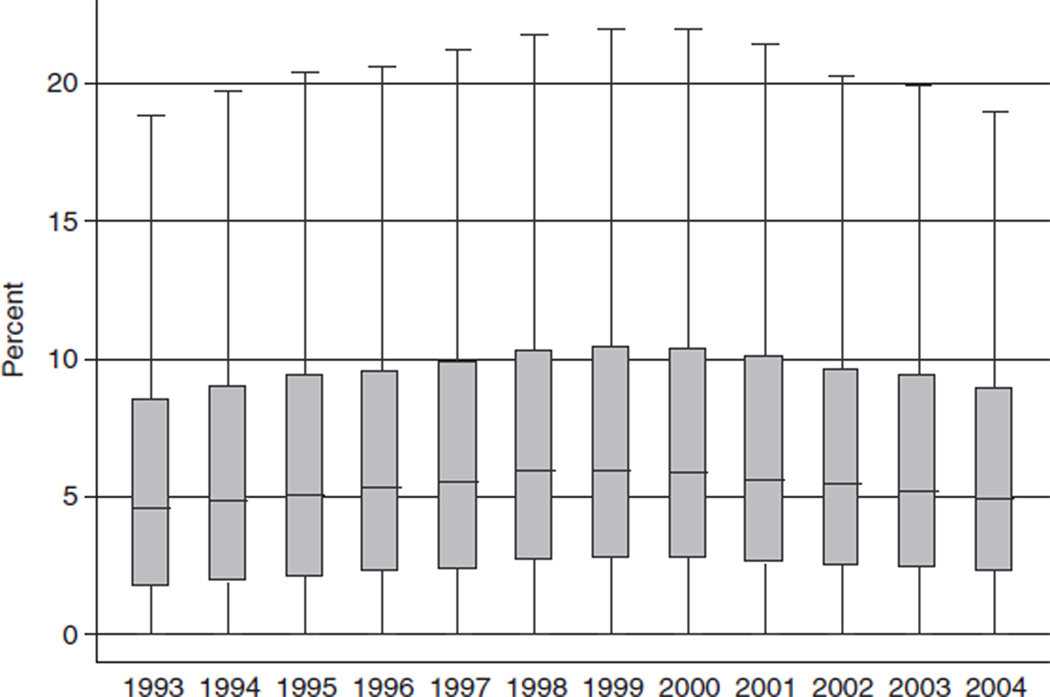
Figure 1 illustrates the temporal trends in the use of feeding tubes in 11,002 urban, freestanding NHs (74.0% for profit, average number of beds 118) between 1993 and 2004. In 1993, an average of 6.1% (median 4.6%) of NH residents were tube-fed. Since then, there has been an increase in feeding tube use, peaking in 1999 at 7.6% (median 6.0%) and declining slightly to 6.7% (median 5.0%), for an overall net increase across the entire study period (Figure 1).
Figure 1.
Annual distribution of point prevalence of feeding tube use between 1993 and 2004 for 11,002 nursing home facilities in the United States.
Effect of Case Mix Reimbursement
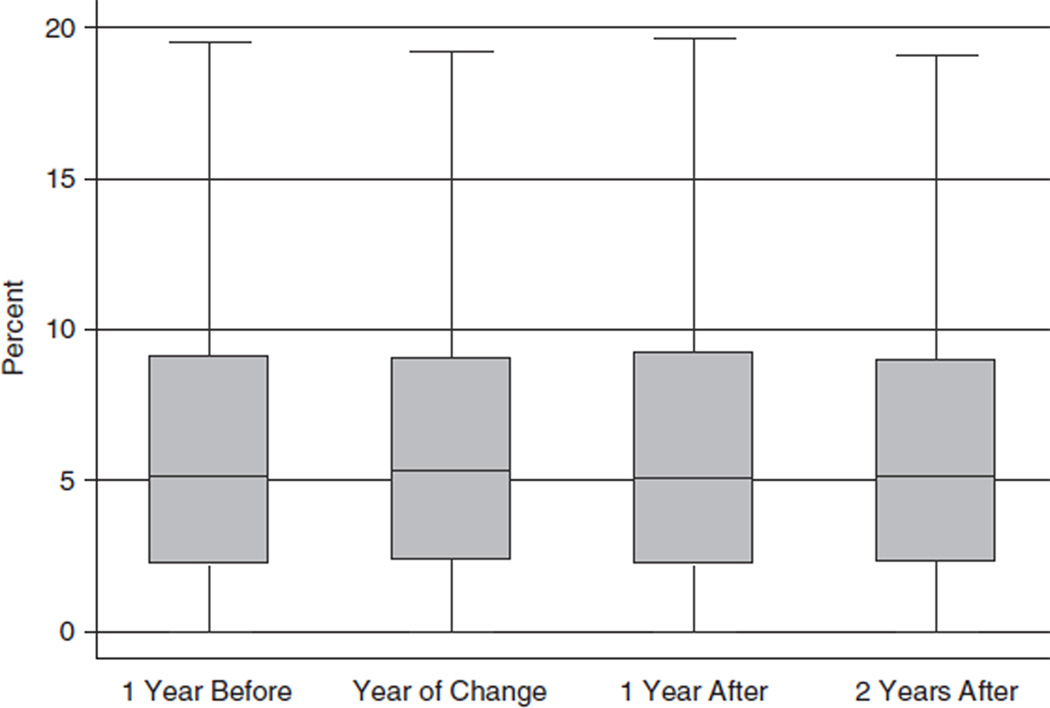
In the unadjusted analyses, the prevalence of feeding tube use in NHs located in the 16 states that adopted case mix reimbursement between 1993 and 2004 changed little from the year before the implementation of case mix reimbursement to the 2 years immediately after implementation (Figure 2). The prevalence of feeding tubes was 6.4%, on average, 1 year before case mix implementation; it increased slightly to 6.6% 2 years after case mix implementation, although after adjusting for the secular trend in overall feeding tube use across all states during this time period, facility fixed effects, and other confounders, the introduction of case mix reimbursement was associated with a slight decrease (β = −0.300, P < .01) in the average prevalence of feeding tube use (Table 1). There was increase in overall feeding tube use over time, as indicated by the strong calendar year effects. For example, the beta coefficient of 2.0 for 2000 indicates that the difference between the rates of feeding tube use in 1993 and 2000, on average, was 2.0%.
Figure 2.
Change in the prevalence of feeding tube use with the introduction of case mix reimbursement in 16 states.
Table 1.
Results of the Facility Fixed-Effects Model Examining the Effect of Case Mix Reimbursement Introduction on Feeding Tube Use (N = 110,881 Surveys from 11,002 Facilities)
| Variable | Coding | Effect on Percentage of Feeding Tubes |
|---|---|---|
| Case mix introduction | − 0.300* | |
| Medicaid rate | Consumer Price Index adjusted, centered at $112 with $10 increment | −0.055† |
| % Medicare | Centered at 10% (mean) | 0.036* |
| Activity of daily living acuity index | Centered at 10 (mean) | 0.943* |
| Percentage of residents undergoing rehabilitation | Centered at 16% (mean) | 0.006* |
| County wage index | Centered at 0.96 (mean) | − 0.202 |
| Year (1993 reference) | ||
| 1994 | 0.269* | |
| 1995 | 0.680* | |
| 1996 | 1.252* | |
| 1997 | 1.469* | |
| 1998 | 1.900* | |
| 1999 | 2.067* | |
| 2000 | 2.006* | |
| 2001 | 1.794* | |
| 2002 | 1.519* | |
| 2003 | 1.357* | |
| 2004 | 1.149* | |
| Intercept | 5.770* |
Note: The interpretation of beta coefficients is the absolute difference in the mean rate of feeding tubes per unit change in a covariate or in comparison to the reference category, and robust standard errors were applied to adjust for clustering of surveys within facility.
P<.01;
.05.
DISCUSSION
Contrary to expectations, the use of feeding tubes did not increase significantly with the introduction of state-based case mix reimbursement, despite apparent financial incentives to do so. These results indicate that the increased per diem payment for the use of feeding tubes did not result in an increase in the prevalence of feeding tubes in the 16 states that implemented case mix reimbursement between 1993 and 2004. Rather, a slight decrease in tube-feeding use was observed in these states after controlling for potential confounders, including the net increase in the prevalence of feeding tubes during this time period across facilities in all states.
This study has some limitations that need to be acknowledged. First, the OSCAR contains administrative, nonaudited data and is thus prone to potential reporting errors. Second, it was possible to examine only the aggregate prevalence of feeding tubes within NHs, rather than the prevalence specifically in NH residents with advanced dementia. Third, other ecological factors potentially occurring during the same time period may have contributed to the observed results. Despite these limitations, the study used national panel data to examine the effects of case mix reimbursement over 12 years.
It is somewhat reassuring that introduction of a reimbursement scheme that has the potential for ‘‘gaming’’ the system, because it pays differentially for patients with a feeding tube inserted, was not associated with a greater rate of feeding tube use at the time of the annual NH inspection. The prevalence of feeding tubes decreased slightly after 1998Fa time when there was debate regarding the efficacy of feeding tubes in persons with advanced dementia. Even without these additional financial incentives of case mix reimbursement, important differences remain between the amount of staff time required for the hand feeding of patients with dementia and the amount of staff time needed for the use of enteral feeding. Such difference in staff time results in important differences in the daily costs of caring for an NH resident with and without a feeding tube. Significant savings were reported in 6-month average costs for hand feedings versus enteral feedings in oneNH($4,219 for hand feeding vs $2,379 for a feeding tube).6 The current study was not able to address this issue, which remains an important area of research.
The unanswered question is the potential explanation for the striking cross-state variation in the prevalence of feeding tube use. These results suggest that differences in state policies regarding reimbursement account for little of this variation. Only the prevalence of feeding tubes could be studied with this data source. It is possible that feeding tubes are inserted in acute care hospitals, and thus the incentives of case mix reimbursement would not have played a role in the increased prevalence of feeding tube insertion over the study period. Future research is needed to better understand this variation.
ACKNOWLEDGMENTS
The authors thank Mrs. Cindy Williams for assistance in manuscript preparation.
Funding for this research was provided by the National Institute of Aging (R01AG24265).
Sponsor’s Role: The funder had no role in design, methods, recruitment, analysis, or preparation of the manuscript.
Footnotes
Conflict of Interest: There are no conflicts of interest to declare.
Author Contributions: Teno: study concept and design, data analysis, interpretation of data, and preparation of manuscript. Feng: data analysis, interpretation of data, and preparation of manuscript. Mitchell, Intrator, and Mor: study concept and design, interpretation of data, and preparation of manuscript. Kuo: interpretation of data and preparation of manuscript.
REFERENCES
- 1.Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia: A review of the evidence. JAMA. 1999;282:1365–1370. doi: 10.1001/jama.282.14.1365. [DOI] [PubMed] [Google Scholar]
- 2.Gillick MR. Rethinking the role of tube feeding in patients with advanced dementia. N Engl J Med. 2000;342:206–210. doi: 10.1056/NEJM200001203420312. [DOI] [PubMed] [Google Scholar]
- 3.Teno JM, Mor V, DeSilva D, et al. Use of feeding tubes in nursing home residents with severe cognitive impairment. JAMA. 2002;287:3211–3212. doi: 10.1001/jama.287.24.3211. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell SL, Teno JM, Roy J, et al. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. JAMA. 2003;290:73–80. doi: 10.1001/jama.290.1.73. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell SL, Kiely DK, Gillick MR. Nursing home characteristics associated with tube feeding in advanced cognitive impairment. J Am Geriatr Soc. 2003;51:75–79. [PubMed] [Google Scholar]
- 6.Mitchell SL, Buchanan JL, Littlehale S, et al. Tube-feeding versus hand-feeding nursing home residents with advanced dementia: A cost comparison. J Am Med Dir Assoc. 2003;4:27–33. doi: 10.1097/01.JAM.0000043421.46230.0E. [DOI] [PubMed] [Google Scholar]
- 7.Feng Z, Grabowski DC, Intrator O, et al. The effect of state medicaid case-mix payment on nursing home resident acuity. Health Serv Res. 2006;41:1317–1336. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis MA, Freeman JW, Kirby EC. Nursing home performance under case-mix reimbursement: Responding to heavy-care incentives and market changes. Health Serv Res. 1998;33:815–834. [PMC free article] [PubMed] [Google Scholar]
- 9.Swan JH, Harrington C, Clemena W, et al. Medicaid nursing facility reimbursement methods: 1979–1997. Med Care Res Rev. 2000;57:361–378. doi: 10.1177/107755870005700306. [DOI] [PubMed] [Google Scholar]
- 10.Grabowski DC, Feng Z, Intrator O, et al. Recent Trends in Medicaid Payment and State Nursing Home Policies. Web Page. doi: 10.1377/hlthaff.w4.363. [DOI] [PubMed] [Google Scholar]
- 11.Cowles CM. Nursing Home Statistical Yearbook. Montgomery Village, MD: Cowles Research Group; 2002. [Google Scholar]