Abstract
Objective
To estimate the effect of education and income on incident heart failure (HF) hospitalization among post-menopausal women.
Background
Investigations of socioeconomic status (SES) have focused on outcomes after HF diagnosis, not associations with incident HF. We used data from the Women’s Health Initiative Hormone Trials to examine the association between SES levels and incident HF hospitalization.
Methods
We included 26,160 healthy, post-menopausal women. Education and income were self-reported. ANOVA, Chi-square tests, and proportional hazards models were used for statistical analysis, with adjustment for demographics, co-morbid conditions, behavioral factors, and hormone and dietary modification assignments.
Results
Women with household incomes <$20,000/year had higher HF hospitalization incidence (57.3/10,000 person-years) than women with household incomes >$50,000/year (16.7/10,000 person-years; p<0.01). Women with less than a high school education had higher HF hospitalization incidence (51.2/10,000 person-years) than college graduates and above (25.5/10,000 person-years; p<0.01). In multivariable analyses, women with the lowest income levels had 56% higher risk (HR 1.56, 95% CI 1.19 to 2.04) than the highest income women; women with the least amount of education had 21% higher risk for incident HF hospitalization (HR 1.21, 95% CI 0.90 to 1.62) than the most educated women.
Conclusions
Lower income is associated with an increased incidence of HF hospitalization among healthy, post-menopausal women, whereas multivariable adjustment attenuated the association of education with incident HF.
Keywords: heart failure, socioeconomic status, women
Background
Heart failure (HF) is a growing epidemic, but little is known about the association between HF incidence and socioeconomic status (SES) in the United States. Prior investigations report that lower SES patients have increased morbidity and mortality after HF diagnosis (1), but data are sparse regarding an association between low SES and HF incidence. Less educated and lower income individuals have increased prevalence of cardiovascular disease risk factors (2), resulting in increased risk for ischemic heart disease and stroke (3,4). In European cohorts, lower SES patients also appear to have increased HF risk (5), but these studies are not representative of the United States population or its health care delivery system. The purpose of this study was to examine the association of income and education with incident HF.
Methods
We used data from the Women’s Health Initiative (WHI) Hormone Trials (6), a series of randomized-controlled trials that tested the effects of hormone therapy on a variety of health outcomes among healthy, post-menopausal women. We excluded women with baseline HF (n=198), cardiac arrest (n=81), coronary artery bypass grafting (n=509), percutaneous coronary intervention (n=180) or missing information during follow-up (n=268), yielding a cohort of 26,160 healthy post-menopausal women for this analysis.
Records were obtained and adjudicated every six months for self-reported HF hospitalizations, as well as possible HF events found during adjudication of other cardiovascular outcomes (e.g. myocardial infarction). Three cardiologists reviewed all records independently using the WHI and Framingham Heart Study (FHS) diagnostic criteria to identify HF cases(7). Ambulatory cases of HF were not included. The WHI criteria required a physician diagnosis of HF and medical treatment for HF during the index admission, with/without an imaging procedure showing impaired systolic or diastolic left ventricular function. The FHS criteria required a specific combination of major and minor criteria (7). Disagreements were resolved by consensus decision.
We identified 663 incident cases of HF: 294 met only the WHI criteria, 8 met only the FHS criteria, and 361 met both criteria. For the current analysis, we used all 663 incident HF cases a priori to maximize power and conducted sensitivity analyses on the 361 cases that met both WHI and FHS criteria. Results were similar when analyzing with WHI or FHS criteria separately.
Educational attainment was determined by self-report and collapsed into three categories from five categories collected by the WHI (Table 1). Similarly, annual household income was determined by self-report and collapsed into four categories (Table 2).
Table 1.
Baseline Characteristics of Participants According to Education
| Less than High School (N=2,013) | High School ± Some College/Vocational School (N=15,985) | College Graduate ± Any Graduate Study (N=8,027) | |
|---|---|---|---|
| Sociodemographic Variables
| |||
| Age, mean years±SD | 63.7 ± 7.1 | 63.4 ± 7.1 | 63.1 ± 7.4 |
| Race/Ethnicity, n (%) | |||
| • White | 1,051 (52.2) | 13,188 (82.5) | 6,827 (85.1) |
| • Black | 347 (17.2) | 1,483 (9.3) | 713 (8.9) |
| • Hispanic | 527 (26.2) | 700 (4.4) | 193 (2.4) |
| • Asian/Pacific Islander | 29 (1.4) | 309 (1.9) | 168 (2.1) |
| • Other | 47 (2.3) | 274 (1.7) | 110 (1.4) |
| Marriage Status, n (%) | |||
| • Never | 45 (2.2) | 333 (2.1) | 604 (7.5) |
| • Divorced | 360 (17.9) | 2,694 (16.9) | 1,531 (19.1) |
| • Widowed | 470 (23.4) | 3,364 (21.0) | 1,297 (16.2) |
| • Married | 1,123 (55.8) | 9,562 (59.8) | 4,583 (57.1) |
| Insurance Type, n (%) | |||
| • No insurance | 585 (29.1) | 1,877 (11.8) | 560 (7.0) |
| • Medicare | 329 (16.3) | 1,460 (9.1) | 588 (7.3) |
| • Medicaid | 63 (3.1) | 86 (0.5) | 10 (0.1) |
| • Medicare + Medicaid | 46 (2.3) | 95 (0.6) | 22 (0.3) |
| • Private insurance | 547 (27.2) | 7,899 (49.4) | 4,543 (56.6) |
| • Private + Medicare | 396 (19.7) | 4,444 (27.8) | 2,255 (28.1) |
|
| |||
| Behavioral/Lifestyle Variables
| |||
| Smoking Status, n (%) | |||
| • Never | 1063 (52.8) | 7,856 (49.2) | 4,071 (50.7) |
| • Former Smoker | 650 (32.3) | 6,188 (38.7) | 3,222 (40.1) |
| • Current | 265 (13.2) | 1,774 (11.1) | 651 (8.1) |
| Alcohol Use, n (%) | |||
| • Non drinker | 489 (24.3) | 1,931 (12.1) | 739 (9.2) |
| • Former drinker | 615 (30.6) | 3,312 (20.7) | 1,107 (13.8) |
| • 0-7 drinks/week | 800 (39.7) | 9,002 (56.3) | 4,903 (61.1) |
| • 7+ drinks/week | 71 (3.5) | 1,605 (10.0) | 1,225 (15.3) |
| Physical Activity, n (%) | |||
| • No activity | 525 (26.1) | 3,040 (19.0) | 1,061 (13.2) |
| • Minimal activity | 894 (44.4) | 6,598 (41.3) | 2,974 (37.1) |
| • Moderate activity | 157 (7.8) | 2,144 (13.4) | 1,357 (16.9) |
| • Strenuous activity | 237 (11.8) | 2,843 (17.8) | 1,976 (24.6) |
|
| |||
| Medical Variables
| |||
| SBP≥140mmHg, DBP≥90mmHg or Treated Hypertension, n (%) | 898 (44.6) | 6,570 (41.1) | 2,705 (33.7) |
| Body Mass Index, kg/m2± SD | 30.4 ± 6.1 | 29.3 ± 6.0 | 28.2 ± 5.8 |
| Diabetes Mellitus, n (%) | 215 (10.7) | 1,013 (6.3) | 326 (4.1) |
| Myocardial Infarction During Follow-Up, n (%) | 49 (2.4) | 258 (1.6) | 83 (1.0) |
| Hormone Replacement Therapy, n (%) | |||
| • Intervention | 1,033 (51.3) | 8,104 (50.7) | 4,005 (49.9) |
| • Placebo | 980 (48.7) | 7,881 (49.3) | 4,022 (50.1) |
| Dietary Modification, n (%) | |||
| • Not randomized | 1,464 (72.7) | 11,142 (69.7) | 5,740 (71.5) |
| • Intervention | 211 (10.5) | 1,870 (11.7) | 971 (12.1) |
| • Control | 338 (16.8) | 2,973 (18.6) | 1,316 (16.4) |
SBP=systolic blood pressure; DBP=diastolic blood pressure
All p-values for the comparison of characteristics according to education group are significant at a level of p<0.01, with the exception of hormone replacement therapy (p=0.46)
Table 2.
Baseline Characteristics of Participants According to Income
| <$20,000/year (N=5,694) | $20,000/year to $34,999/year (N=7,036) | $35,000/year to $49,999/year (N=5,105) | >$50,000/year (N=6,947) | |
|---|---|---|---|---|
| Sociodemographic Variables
| ||||
| Age, mean years±SD | 64.6 ± 7.3 | 64.3 ± 7.0 | 63.1 ± 6.9 | 61.3 ± 7.0 |
| Race/Ethnicity, n (%) | ||||
| • White | 3,945 (69.3) | 5,868 (83.4) | 4,348 (85.2) | 5,972 (86.0) |
| • Black | 848 (14.9) | 655 (9.3) | 420 (8.2) | 496 (7.1) |
| • Hispanic | 676 (11.9) | 284 (4.0) | 157 (3.1) | 165 (2.4) |
| • Asian/Pacific Islander | 87 (1.5) | 102 (1.5) | 98 (1.9) | 201 (2.9) |
| • Other | 117 (2.1) | 116 (1.7) | 74 (1.5) | 101 (1.5) |
| Insurance Type, n (%) | ||||
| • No insurance | 1,466 (25.8) | 713 (10.1) | 325 (6.4) | 281 (4.0) |
| • Medicare | 869 (15.3) | 651 (9.3) | 331 (6.5) | 348 (5.0) |
| • Medicaid | 130 (2.3) | 14 (0.2) | 2 (0.04) | 2 (0.03) |
| • Medicare + Medicaid | 129 (2.3) | 11 (0.2) | 4 (0.1) | 7 (0.1) |
| • Private Insurance | 1,459 (25.6) | 3,292 (46.8) | 2,961 (58.0) | 4,837 (69.6) |
| • Private + Medicare | 1,556 (27.3) | 2,312 (32.9) | 1,454 (28.5) | 1,432 (20.6) |
| Marriage Status, n (%) | ||||
| • Never | 256 (4.5) | 287 (4.1) | 198 (3.9) | 170 (2.5) |
| • Divorced | 1,695 (29.8) | 1,418 (20.2) | 753 (14.8) | 562 (8.1) |
| • Widowed | 2,022 (35.5) | 1,617 (23.0) | 724 (14.2) | 530 (7.6) |
| • Married | 1,691 (29.7) | 3,697 (52.5) | 3,417 (66.9) | 5,673 (81.7) |
|
| ||||
| Behavioral/Lifestyle Variables
| ||||
| Smoking Status, n (%) | ||||
| • Never | 2,870 (50.4) | 3,516 (50.0) | 2,529 (49.5) | 3,407 (49.0) |
| • Former Smoker | 1,958 (34.4) | 2,713 (38.6) | 2,043 (40.0) | 2,871 (41.3) |
| • Current | 788 (13.8) | 727 (10.3) | 473 (9.3) | 613 (8.8) |
| Alcohol Use, n (%) | ||||
| • Non drinker | 997 (17.5) | 883 (12.6) | 537 (10.5) | 553 (8.0) |
| • Former drinker | 1,592 (28.0) | 1,490 (21.1) | 807 (15.8) | 860 (12.4) |
| • 0-7 drinks/per week | 2,703 (47.5) | 3,939 (56.0) | 3,106 (60.8) | 4,314 (62.1) |
| • 7+ drinks/per week | 340 (6.0) | 662 (9.4) | 611 (12.0) | 1,184 (17.0) |
| Physical Activity, n (%) | ||||
| • No Activity | 1,215 (21.3) | 1,273 (18.1) | 904 (17.7) | 989 (14.2) |
| • Minimal Activity | 2,554 (44.9) | 2,931 (41.7) | 1,994 (39.1) | 2,490 (35.9) |
| • Moderate Activity | 603 (10.6) | 987 (14.0) | 759 (14.9) | 1,150 (16.6) |
| • Strenuous Activity | 809 (14.2) | 1,229 (17.5) | 1,027 (20.1) | 1,735 (25.0) |
|
| ||||
| Medical Variables
| ||||
| SBP≥140mmHg, DBP≥90mmHg or Treated Hypertension, n (%) | 2,585 (45.4) | 2,906 (41.3) | 1,955 (38.3) | 2,237 (32.2) |
| Body Mass Index, kg/m2±SD | 29.8 ± 6.3 | 29.3 ± 6.0 | 29.1± 6.0 | 28.2 ± 5.7 |
| Diabetes Mellitus, n (%) | 513 (9.0) | 442 (6.3) | 277 (5.4) | 233 (3.3) |
| Myocardial Infarction During Follow-Up, n (%) | 136 (2.4) | 110 (1.6) | 60 (1.2) | 59 (0.9) |
| Hormone Replacement Therapy, n (%) | ||||
| • Intervention | 2,910 (51.1) | 3,588 (51.0) | 2,553 (50.0) | 3,494 (50.3) |
| • Placebo | 2,781 (48.9) | 3,448 (49.0) | 2,553 (50.0) | 3,453 (49.7) |
| Dietary Modification, n (%) | ||||
| • Not Randomized | 4,066 (71.4) | 4,932 (70.1) | 3,533 (69.2) | 4,884 (70.3) |
| • Intervention | 632 (11.1) | 830 (11.8) | 623 (12.2) | 820 (11.8) |
| • Control | 996 (17.5) | 1,274 (18.1) | 950 (18.6) | 1,244 (17.9) |
SBP=systolic blood pressure; DBP=diastolic blood pressure
All p-values for the comparison of characteristics according to income group are significant at a level of p<0.01, with the exception of hormone replacement therapy (p=0.53) and dietary modification (p=0.03)
We used ANOVA and Chi-square tests to compare baseline characteristics according to SES. Cox proportional hazards models were used to evaluate the effect of SES on incident HF. In the multivariable regression, we adjusted for age, race/ethnicity, marriage status, hormone assignment, dietary modification assignment, level of physical activity, smoking status, alcohol consumption, body mass index, interim myocardial infarction (modeled as a time-varying covariate), systolic blood pressure, hypertension, diabetes mellitus, and health insurance. Ejection fraction was available from the index hospitalization for 78% of the women diagnosed with HF, but unavailable for those without HF; therefore it was not included in the statistical analyses. Ejection fraction measured during index hospitalization did not differ across education or income groups among women who had a first time HF hospitalization (data presented in an online supplement).
In secondary analyses, we stratified our income models at age 66 to account for possible differential income effects in employment and retirement age women. We also performed a stratified analysis between white and black women to evaluate the role of race/ethnicity. The small number of HF events in Hispanics (n=24) and Asians/Pacific Islanders (n=8) prevented meaningful analysis of risk in these subgroups. In race/ethnicity-stratified analysis, we were unable to model interim myocardial infarction as a time-varying covariate due to the small number of events among black women. Analysis was performed using SAS Version 9.2 (SAS Institute Inc., Cary, NC, USA). We found no evidence for significant interaction between education and income levels for risk of indicent HF. P-values <0.05 were considered statistically significant.
Results
Among 26,160 participants, 7.7% (n=2,013) had less than high a school education and 21.8% (n=5,694) had household incomes of less than $20,000/year. Several risk factors, including hypertension, diabetes, and interim myocardial infarction, were significantly more prevalent among lower SES women (Tables 1 and 2).
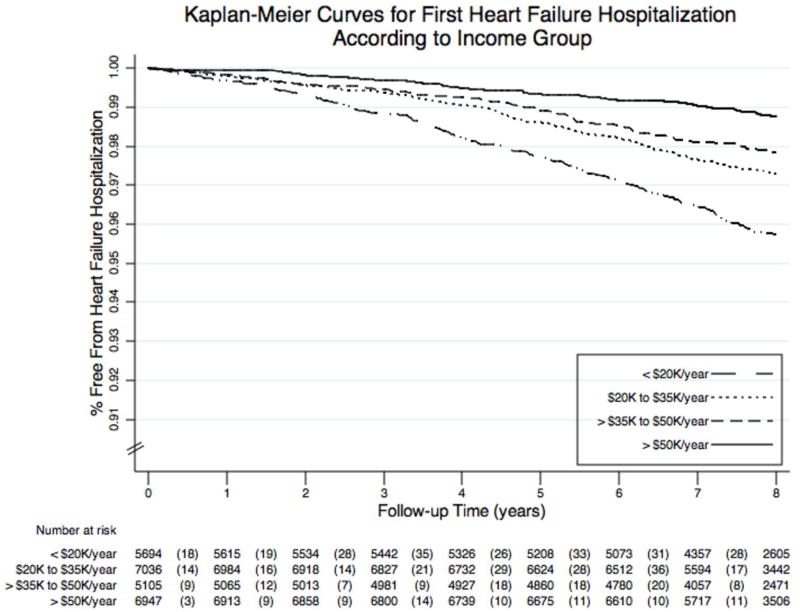
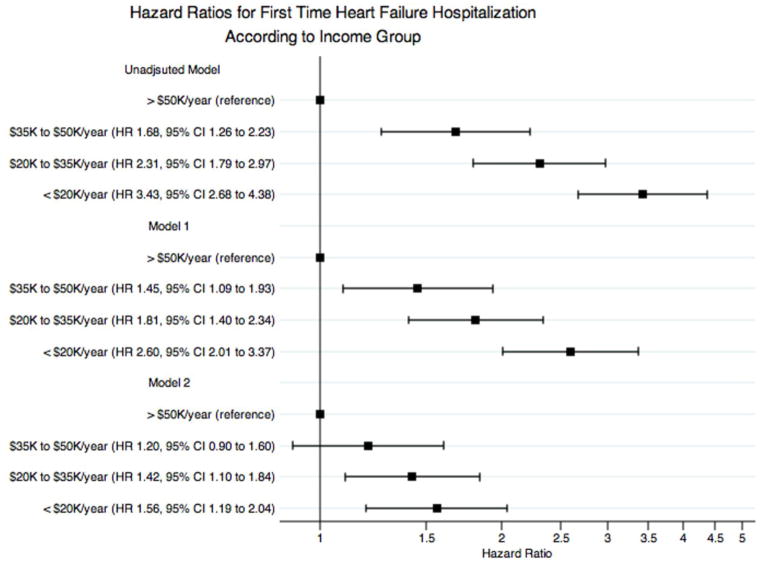
Incident HF hospitalization occurred at a higher rate among low-income women during the follow-up period; event rates decreased from 57.3 to 16.7 per 10,000 person-years between the lowest and highest income categories (p<0.01; Figure 1A). In the unadjusted model, low-income women had a HF hospitalization hazard over three times higher than high-income women (HR 3.43, 95% CI 2.68 to 4.38; Figure 2A).
Figure 1.
Figure 1A. Kaplan-Meier Curves for First Time Heart Failure Hospitalization According to Household Income
Log-rank test p < 0.0001 for comparison
< $20,000/year: 57.3/10,000 person-years (n=234)
$20,000 to $34,999/year – 38.5/10,000 person-years (n=200)
$35,000 to $49,999/year – 28.1/10,000 person-years (n=106)
> $50,000/year – 16.7/10,000 person-years (n=87)
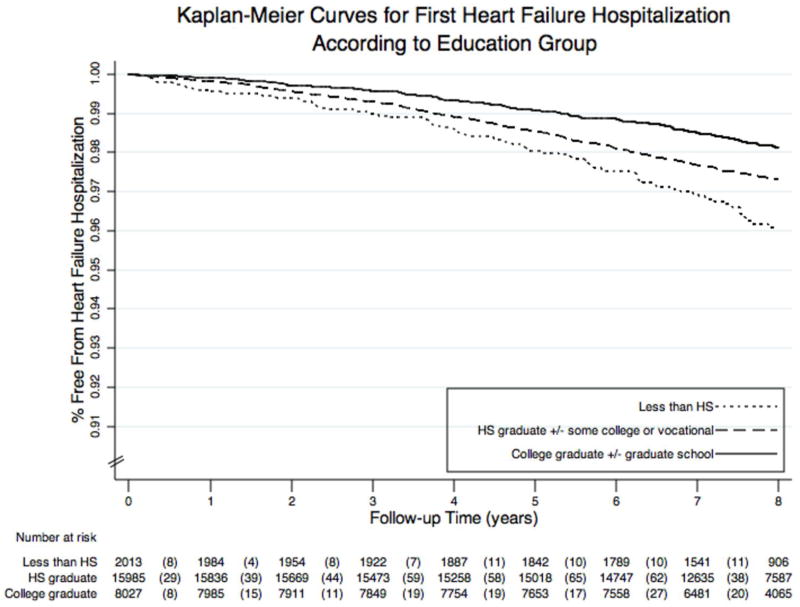
Figure 1B. Kaplan-Meier Curves for First Time Heart Failure Hospitalization According to Education Level
Log-rank test p < 0.0001 for comparison
Less than high school: 51.2/10,000 person-years (n=74)
High school graduate ± some college: 36.7/10,000 person-years (n=429)
Four-year college graduate ± any graduate school: 25.5/10,000 person-years (n=153)
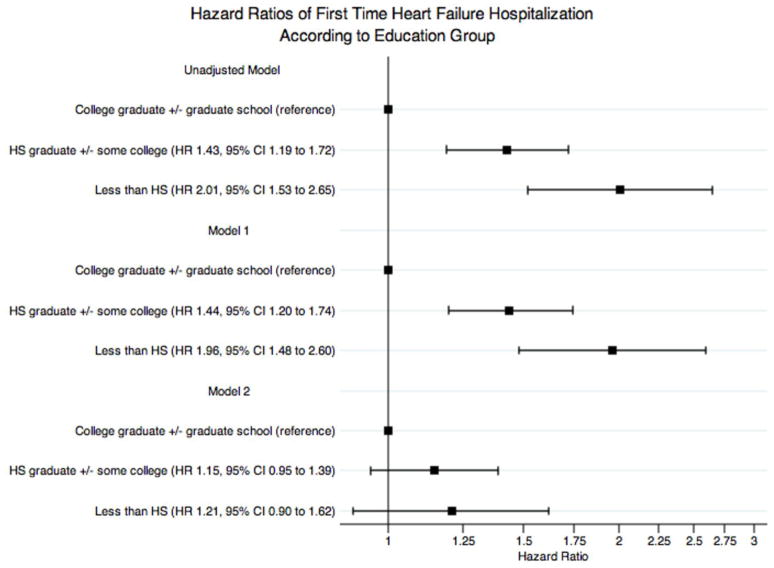
Figure 2.
Figure 2A. Hazard Ratios for First Time Heart Failure Hospitalization According to Household Income
HR=hazard ratio
*Model 1: age, race/ethnicity, marriage status, hormone assignment, dietary modification assignment
†Model 2: Above plus level of physical activity, smoking status, alcohol consumption, body mass index, interim myocardial infarction, systolic blood pressure, treated hypertension, and diabetes mellitus, health insurance.
Figure 2B. Hazard Ratios for First Time Heart Failure Hospitalization According to Education Level
HS=high school; HR=hazard ratio
*Model 1: age, race/ethnicity, marriage status, hormone assignment, dietary modification assignment
†Model 2: ABove plus level of physical activity, smoking status, alcohol consumption, body mass index, interim myocardial infarction, systolic blood pressure, treated hypertension, and diabetes mellitus, health insurance.
In the multivariable model, women from the lowest income group had a 56% significantly higher hazard of incident HF hospitalization compared to women from the highest income group. Women with incomes $20,000 to $34,999/year had a 42% significantly higher hazard and those with $35,000 to $50,000/year had a 20% insignificantly higher hazard of incident HF hospitalization compared to the highest income women (Figure 2A).
The relationship between education and incident HF hospitalization followed a similar pattern to income – incidence increased with lower levels of education (p<0.01; Figure 1B). In the unadjusted model, women with less than a HS education had double the hazard for incident HF hospitalization compared to women with four-year college degrees and above (HR 2.01, 95% CI 1.53 to 2.65). In the multivariable model, the least educated women had a 21% higher hazard of disease (HR 1.21, 95% CI 0.90 to 1.62; Figure 2B) compared to the most educated women.
Women over age 65 years accounted for 40.0% of the cohort (n=10,463) and 63.5% (n=412) of HF events. The hazard ratios for incident HF hospitalization between the lowest and highest income women were similar for both age groups (HR 1.51, 95% CI 0.97–2.34 for employment age; HR 1.53, 95% CI 1.08–2.16 for retirement age).
First time HF hospitalization occurred in 2.5% of white women (n=536) and 3.1% of black women (n=84). The magnitudes of the effects of education and income were greater for black women, but non-significant due to small sample size (Table 3).
Table 3.
Regression Analysis of First Time Heart Failure Hospitalization Risk on Education and Income, Stratified by Race/Ethnicity
| White Women N=21,269 |
Black Women N=2,574 |
|||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| Education
| ||||
| Unadjusted Model | ||||
| • College Graduate ± Any Graduate Study (ref) | 1.00 | — | 1.00 | — |
| • High School ± Some College/Vocational School | 1.40 | 1.15 – 1.70 | 1.81 | 0.98 – 3.34 |
| • Less than High School | 1.90 | 1.33 – 2.73 | 3.62 | 1.82 – 7.18 |
| Multivariable Model* | ||||
| • College Graduate ± Any Graduate Study (ref) | 1.00 | — | 1.00 | — |
| • High School ± Some College/Vocational School | 1.10 | 0.76 – 1.60 | 2.11 | 1.02 – 4.34 |
| • Less than High School | 1.15 | 0.94 – 1.41 | 1.37 | 0.73 – 2.56 |
|
| ||||
| Income
| ||||
| Unadjusted Model | ||||
| • >$50,000/year | 1.00 | — | 1.00 | — |
| • $35,000 to $49,999/year | 1.62 | 1.20 – 2.20 | 1.87 | 0.72 – 7.29 |
| • $20,000 to $34,999/year | 2.29 | 1.76 – 3.00 | 1.63 | 0.67 – 4.00 |
| • <$20,000/year | 3.46 | 2.64 – 4.52 | 3.99 | 1.80 – 8.84 |
| Multivariable Modela | ||||
| • >$50,000/year | 1.00 | — | 1.00 | — |
| • $35,000 to $49,999/year | 1.19 | 0.88 – 1.62 | 1.48 | 0.57 – 3.86 |
| • $20,000 to $34,999/year | 1.41 | 1.07 – 1.86 | 1.15 | 0.46 – 2.85 |
| • <$20,000/year | 1.69 | 1.26 – 2.26 | 2.26 | 0.97 – 5.23 |
Multivariate model includes education or income, plus: age, marriage status, dietary modification assignment, hormone therapy assignment, activity level, smoking status, alcohol consumption, body mass index, interim myocardial infarction, systolic blood pressure, treatment for hypertension, diabetes, insurance
Discussion
Our investigation shows that incident HF hospitalization in post-menopausal women disproportionately affects women who have lower education attainment and income, regardless of race/ethnicity. Known risk factors for HF (8) were more prevalent among low SES women, consistent with prior investigations (9). However, the association of lower income with first time HF hospitalization risk persisted after adjustment for risk factors and other variables; adjustment attenuated the association with education, although the trend persisted.
Neighborhood characteristics, access to care, and health literacy may contribute to the SES disparity observed in our investigation. An investigation from the Multi-Ethnic Study of Atherosclerosis (MESA) showed that decreasing levels of education and income were associated with unfavorable neighborhood characteristics: lack of walking environment, healthy food availability, safety, and social cohesion. MESA participants in these environments were more likely to have hypertension and high body-mass indices (10,11), known risk factors for HF.
A relationship between decreased preventive care access due to cost and higher disease incidence may contribute to SES disparities. Still, lower income patients who overcome financial barriers and seek out preventive care receive lower quality of care compared to higher income patients (12). Analysis from the Community Tracking Survey, a survey of health care utilization patterns, showed that low-income patients who had access to health care services received only 52% of recommended preventive services (13). One possibility is that co-payments and deductibles prevent lower income patients from receiving care, even when insured, which may explain the stronger income effect we observed in this study.
Poor health literacy may affect low SES groups and affects preventive care on many levels. Lower SES patients report poor communication with their doctors (12) and patients with low health literacy are less likely to seek preventive care (14). Advances in medical information technology could deepen the disparity conferred by low literacy (15).
Heart failure is a costly disease, with a total estimated cost of $37.2 billion in 2009; two-thirds of the cost comes from hospitalizations (16). Heart failure costs, mortality and a growing at-risk population of elderly women are compelling reasons to design effective HF prevention programs for lower SES women (17). The Centers for Disease Control’s Well-Integrated Screening and Evaluation for Women Across the Nation project showed that tailored outreach and prevention efforts can lead to improvements in blood pressure, cholesterol and lifestyle habits among low-income, elderly women (18).
Limitations
The WHI collected information on household income, rather than total wealth. This approach could lead to a misclassification of wealthy women who report low incomes. We addressed this possibility by a stratified analysis comparing retirement age women, who may have a discrepancy between reported income and total wealth, to employment age women; low income was associated with incident HF hospitalization in both groups. Moreover, most government agencies use the income metric, rather than wealth; use of income makes our results more useful for planning agencies.
We used only hospitalizations to identify incident HF events. While this is a limitation, consideration of incident HF hospitalizations, relative to incident outpatient HF, is important due to associated disease severity and cost. Finally, the WHI includes healthy, post-menopausal women; our findings cannot be generalized to men and younger women.
Conclusions and Implications
Our analysis of the WHI HT show that post-menopausal women with lower SES are at increased risk for first time HF hospitalizations, even after adjustment for known risk factors. As the United States population ages, with women as a larger proportion of the elderly population (17), tailored prevention efforts will help us alleviate the HF health care burden and this health disparity in the future.
Supplementary Material
Acknowledgments
Funding Disclosures:
The WHI program is funded by the NHLBI through contracts N01WH22110, 24152, 32100-2, 32105-6, 32108-9, 32111-13, 32115, 32118-32119, 32122, 42107-26, 42129-32, and 44221. Dr. Shah is supported by grants from the AHA Pharmaceutical Round Table and the Stanford NIH/NCRR CTSA grant KL2RR025743.
Dr. Klein is supported by NIH grant R21AG027471.
Dr. Phillips is supported by VA HSR&D award IIR 07-138.
Abbreviations
- FHS
Framingham Heart Study
- HF
heart failure
- HS
high school
- WHI
Women’s Health Initiative
Footnotes
Conflict Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rathore SS, Masoudi FA, Wang Y, et al. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am Heart J. 2006;152:371–8. doi: 10.1016/j.ahj.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alter DA, Chong A, Austin PC, et al. Socioeconomic status and mortality after acute myocardial infarction. Ann Intern Med. 2006;144:82–93. doi: 10.7326/0003-4819-144-2-200601170-00005. [DOI] [PubMed] [Google Scholar]
- 3.Arrich J, Mullner M, Lalouschek W, Greisenegger S, Crevenna R, Herkner H. Influence of socioeconomic status and gender on stroke treatment and diagnostics. Stroke. 2008;39:2066–72. doi: 10.1161/STROKEAHA.107.506147. [DOI] [PubMed] [Google Scholar]
- 4.Winkleby M, Sundquist K, Cubbin C. Inequities in CHD incidence and case fatality by neighborhood deprivation. Am J Prevent Med. 2007;32:97–106. doi: 10.1016/j.amepre.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christensen S, Mogelvang R, Heitmann M, Prescott E. Level of education and risk of heart failure: a prospective cohort study with echocardiography evaluation. Eur Heart J. 2011;32:450–458. doi: 10.1093/eurheartj/ehq435. [DOI] [PubMed] [Google Scholar]
- 6.Stefanick ML, Cochrane BB, Hsia J, Barad DH, Liu JH, Johnson SR. The Women’s Health Initiative postmenopausal hormone trials: overview and baseline characteristics of participants. Ann Epidemiology. 2003;13:S78–86. doi: 10.1016/s1047-2797(03)00045-0. [DOI] [PubMed] [Google Scholar]
- 7.Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62. [PubMed] [Google Scholar]
- 8.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001;161:996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 9.Winkleby MA, Kraemer HC, Ahn DK, Varady AN. Ethnic and socioeconomic differences in cardiovascular disease risk factors: findings for women from the Third National Health and Nutrition Examination Survey, 1988–1994. JAMA. 1998;280:356–62. doi: 10.1001/jama.280.4.356. [DOI] [PubMed] [Google Scholar]
- 10.Mujahid MSa, Diez Roux AVa, Morenoff JDb, et al. Neighborhood Characteristics and Hypertension. Epidemiology. 2008;19:590–598. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- 11.Mujahid MS, Diez Roux AV, Shen M, et al. Relation between neighborhood environments and obesity in the Multi-Ethnic Study of Atherosclerosis. Am J Epi. 2008;167:1349–57. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality. [Accessed 6/7/2010];National Healthcare Disparities Report, 2009. AHRQ Publication No. 10-0004. 2010 Mar; Available at http://www.ahrq.gov/qual/qrdr09.htm.
- 13.Asch SM, Kerr EA, Keesey J, et al. Who is at greatest risk for receiving poor-quality health care? N Engl J Med. 2006;354:1147–56. doi: 10.1056/NEJMsa044464. [DOI] [PubMed] [Google Scholar]
- 14.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Parker RM, Ratzan SC, Lurie N. Health literacy: a policy challenge for advancing high-quality health care. Health Affairs. 2003;22:147–53. doi: 10.1377/hlthaff.22.4.147. [DOI] [PubMed] [Google Scholar]
- 16.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 17.United States Census Bureau. [Accessed on 7/5/2010];US Interim Projections by Age, Sex, Race, and Hispanic, 2000–2050. Available at https://www.census.gov/population/www/projections/usinterimproj/
- 18.Stoddard AM, Palombo R, Troped PJ, Sorensen G, Will JC. Cardiovascular disease risk reduction: the Massachusetts WISEWOMAN project. J Womens Health. 2004;13:539–46. doi: 10.1089/1540999041281106. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.