Abstract
Background
Bulimia nervosa (BN) and borderline personality disorder (BPD) are disorders that involve emotion dysregulation, for negative emotion in particular, as well as impulsive behaviors beyond binge eating and vomiting. Given these similarities in psychopathology, it is not surprising that those with BN also present with BPD in approximately one third of cases. Improved understanding of similarities and differences in the experience of negative and positive emotion could aid in the development of treatments specifically tailored to the needs of these disorders.
Methods
In this study, we examined Ecological Momentary Assessment (EMA) data from 133 women diagnosed with BN, 25 of whom also exhibited diagnostic levels of BPD. Emotions and behaviors were assessed daily, with multiple random and event-contingent signals to complete questionnaires on portable digital devices, for a period of two weeks.
Results
Results indicated that the BPD group experienced higher negative emotional variability on bulimic event days. Both groups also demonstrated increasing negative emotion and decreasing positive emotion pre-binge eating and vomiting, with levels of negative emotion decreasing and positive emotion increasing after, for both behaviors.
Conclusions
In terms of group differences, additive effects were found for the BN comorbid with BPD group, who demonstrated greater negative emotional variability, on bulimic event days, and also had higher overall levels of negative emotion pre- and post-binge eating. Those with BN only, however, displayed increasing trajectories of positive emotion before and after binge eating and after vomiting, indicating a potential emotional dampening effect of BPD.
Keywords: borderline personality disorder, bulimia nervosa, binging, vomiting, emotion dysregulation
Bulimia nervosa (BN) is a disorder involving frequent binge eating episodes, compensatory behaviors such as vomiting and laxative use to avoid weight gain, as well as self-concept dominated by shape and weight (APA, 1994). The health consequences of this disorder can be severe and include cardiovascular problems, electrolyte disturbances, and gastrointestinal disorders (Bulik et al., 2002). Furthermore, people with BN have high rates of personality disorders (Godt, 2008). Of those co-occurring personality disorder diagnoses, borderline personality disorder (BPD) is the most common, with comoribity rates of around 30% (Cassin, & von Rason, 2005; Wonderlich & Mitchell, 1992). BPD is a chronic and severe disorder characterized by chaotic interpersonal relationships, emotional reactivity, anger control problems, identity diffusion, various forms of dysregulated behaviors, chronic feelings of emptiness, and self-injurious and suicidal behavior (APA, 2000). Given the severe and dysregulated nature of both disorders, more research is needed to understand how BN co-occurring with BPD may be different than BN alone.
Emotion Dysregulation in Bulimia Nervosa and Borderline Personality Disorder
Over the last decade research has identified that emotion dysregulation plays a major role in the propagation and maintenance of both BN and BPD symptomatology. Emotion dysregulation refers to the inability to control and modulate one’s affective state to such a degree that emotions are experienced as out of control (Shedler & Westen, 2004). Interestingly, many people with BN exhibit emotional dysregulation and impulsive behaviors (beyond binge eating and vomiting), even without a simultaneous BPD diagnosis (Crosby et al., 2009; Myers et al., 2006). Emotional variability is one form of emotion dysregulation, where an individual will experience his or her emotions as fluctuating frequently, rather than being centered around a consistent average within-person level, and may be applied to both positive and negative emotion. For example, someone with high variability in emotion may experience elevated negative emotion in the morning, be euthymic in the afternoon, and then be upset again at night. Importantly, some studies have found a strong link between BPD and emotional variability (Koenigsberg et al., 2002; Henry et al., 2001).
Often understudied, in both BN and BPD, is the dysregulation or variability of positive emotion; different responses in positive emotion may be an important factor in distinguishing these disorders. For example, studies of BN have found increases in positive emotion following binge eating and vomiting (Smyth et al., 2007) and self-injury (Muehlenkamp et al., 2009). On the other hand, some studies have failed to find evidence of positive emotional variability in BPD (Klonksy, 2008; Selby et al., 2009). One potential reason for these different findings may be related to vomiting, which in those with BN may result in momentary elevations in positive emotion due to a sense of having “undone” the negative effects of binge episodes, a feeling of control, or maintaining progress toward a weight goal. This same experience of positive emotion post-binge eating and vomiting may not be as functionally reinforcing in individuals without high-level body weight and shape concerns.
Regardless of what may be causing emotional variability in these disorders, and differences in variability of positive and negative emotion, establishing qualitative and quantitative differences between those with BN and BPD, relative to those with BN alone, may provide a richer understanding of the different roots of behavioral dysfunction. One important implication of this comorbidity is the potential for a additive effect between the two disorders, where there are more frequent and intense experiences of negative or positive emotion due to the combination of problems regulating emotions and behavior, frequent concerns with interpersonal relationships, and weight/shape related stressors seen in individuals with both diagnoses. Furthermore, when both disorders are present, the underlying biological and cognitive vulnerabilities toward dysregulated emotion may work in an additive effect.
Emotional Impact of Dysregulated Eating Behaviors
Emotion regulation models of dysregulated eating behaviors suggest that binge eating and vomiting occur following increasing levels of negative emotion, and that the behavior results in a decrease in negative emotion (Selby et al., 2008). These functions are supported by numerous cross-sectional studies on binge eating and vomiting (Agras & Telch, 1998; Lynch et al., 2000) as well as longitudinal ecological momentary assessment studies (Anestis et al., 2010; Smyth et al., 2007). Binge eating and vomiting behaviors may help reduce experience of negative emotion by narrowing attention away from upsetting thoughts and focusing on the concrete physical stimuli associated with the binge eating (Selby et al., 2008).
Consistent with this conceptualization, Smyth et al. (2007) found that negative emotion increased and positive emotion decreased in the hours prior to a binge or purge in individuals with bulimia nervosa. Conversely, they also found that following the binge, levels of negative emotion decreased and positive emotion increased in these individuals. Thus, these findings point out that the potential for emotion regulating effect of binge eating and vomiting are still at issue, and that the emotion regulation functions of dysregulated eating behaviors may be acute and frequently followed by additional emotion dysregulation. Nonetheless, more empirical exploration of emotional states surrounding dysregulated eating behaviors is needed.
Binge Eating versus Vomiting
In general, trajectories of emotion prior to and after binge eating and vomiting have been studied with relatively the same expectations, increasing negative emotion before and decreased negative emotion afterward (Smyth et al., 2007). Yet, few studies have actually looked at potential differences in the quality of emotion surrounding these behaviors separately. Binge eating and vomiting are highly related behaviors, yet they are also fundamentally distinct and as such they may arise in response to different emotional experiences or exhibit differential effects on emotion post-behavior. So the emotional context of both binge eating and vomiting individual warrants further investigation.
Current Study
Various aspects of mood and behavior have been examined in eating disordered and personality disorder samples using ecological momentary assessment (EMA; Stone & Shiffman, 1994). EMA is a relatively new and innovative way to collect data that partially circumvents the limitations inherent to self-report measures, as it reduces retrospective recall bias while also allowing for assessment in a natural setting. A number of studies implementing EMA in the areas of eating disorders and BPD have been published in the past decade (Greeno et al., 2000; Le Grange et al., 2001; Russell et al., 2007; Trull et al., 2008; Wegner et al., 2002; Wonderlich et al., 2007). Although various aspects of emotion in samples of women with BN or BPD have been examined via EMA techniques, no studies to date have used EMA to investigate the emotion-behavior relationship for those with comorbid BN and BPD. The present study contrasts emotional responding surrounding binge eating and vomiting, in a sample of women with BN and no BPD diagnosis (BN) compared to women with BN and diagnostic levels of BPD (BN+BPD). We predicted that greater levels of emotional variability would be seen in the BN + BPD group than in the BN only group. This prediction was based on a broad array of reasons to experience emotion variability in the combined BPD + BN group (due to difficulty regulating emotions and impulsive behaviors, coupled with interpersonal concerns), but also because of potential underlying biological and cognitive dispositions to emotion variability in both disorders that may have an additive effect. Thus, for the present study, we hypothesized that those with BN+BPD, in comparison to those with BN alone, would have (1) greater daily variability in levels of negative emotion and positive emotion, (2) this effect would be even larger on days when bulimic events occurred, (3) increased trajectories of negative emotion and positive emotion preceding binge/vomit behaviors, and (4) increased trajectories of negative emotion and positive emotion following binge/vomit behaviors.
Methods
Participants were 133 adult females who were recruited from the community and who met criteria for BN (assessment procedure described below). Women were either referred for the study by their physicians, eating disorder treatment providers, or self-referred via community flyers. All completed a telephone screen to confirm eligibility prior to in-person assessment (i.e., inclusion criteria: female, age > 18, meets DSM-IV criteria for BN, no changes in mental health treatment in past 6 weeks). Participants were excluded from the study if they were: 1) male1, 2) currently psychotic, 3) unable to read English at an 8th-grade reading level, 4) positive for a history of gastric bypass surgery, or 5) had initiated psychotherapy or medication within the last six weeks. No participants were excluded based on type of purging method engaged in.
Baseline Assessment
Eating Disorder Examination (EDE; Fairburn & Cooper, 1993)
The EDE interview was used to confirm BN diagnoses for all participants during the baseline assessment. It has demonstrated good internal consistency and is well validated (Cooper et al., 1989; Rizvi et al., 2000; Rosen et al., 1990). BN diagnoses were further confirmed with the SCID-I.
Revised Diagnostic Interview for Borderlines (DIB-R; Zanarini et al., 1989)
The DIB-R is a semi-structured interview assessing facets of BPD psychopathology including emotional experience, cognition, impulsiveness, and interpersonal relationships, and was used to determine BN+BPD group status. It has demonstrated adequate sensitivity and specificity in diagnosing BPD (sensitivity=.82, specificity=.80). The measure has also shown good inter-rater and test-retest reliability (kappas>.75; Zanarini et al., 2002). In research utilizing both the DIB-R and measures that assess the full spectrum of personality disorders (i.e., Structured Clinical Interview for DSM-IV Axis II Personality Disorders [SCID-II, First et al., 1997), fewer subjects diagnosed with BPD based on the DIB-R, suggesting it is a more conservative measure for BPD (Zeeck et al., 2007). In the current study, one addition was made to the typical administration of the DIB-R. For the current research, participants who scored 8 or above on the DIB-R 2-Year Total Score were given a BPD diagnosis, in accordance with guidelines published by the instrument’s authors. To further establish the validity of our procedure for assigning diagnosis of BPD, all participants also completed the Wisconsin Personality Inventory (WISPI; Klein et al., 1993).
Structured Clinical Interview for the DSM-IV Axis I (SCID-I; First et al., 1995)
This is a well-validated assessment of Axis I disorders, and was administered by a doctoral-level psychologist. Regarding comorbid, current Axis I diagnoses, 54% met criteria for a mood disorder diagnosis, 16% for substance use diagnosis, and 51% for any anxiety disorder. When compared on these major diagnostic categories, there were no significant differences in diagnostic comoribidity for either those with BN or BN/BPD. In the current study presence of an Axis I disorder besides BN was used as a covariate in analyses to control for general comorbidity effects.
EMA Signal and Event-Contingent Assessment Protocol
Positive and Negative Affect Scales (PANAS; Watson, Clark, & Tellegen, 1988)
The PANAS is a measure of state emotion consisting of both positive and negative scales. All items in this study were rated as referring to the present moment on a five-point likert scale ranging from 1(not at all) to 5 (extremely). The positive scale included the following items: happy, alert, proud, cheerful, enthusiastic, confident, concentrating, energetic, calm, strong, determined, attentive, and relaxed. Negative items were: afraid, lonely, irritable, ashamed, disgusted, nervous, dissatisfied with self, jittery, sad, distressed, and angry with self. Alphas in the current study were .91 for PA and .92 for NA.
Eating Disorder and Self-Destructive Behavior Checklist (EDSDBC; Vanderlinden & Vendereycken, 1997)
The EDSDBC is a 19-item measure designed for this study, and was used for participants to record specific eating disordered and self-destructive behaviors that occurred during the EMA assessment using a checkbox format. Eating disorder items included “I binge ate,” and “I vomited,” and “I used laxatives,” while self-destructive behavior items included “I cut myself,” “I went on a spending spree,” and “I drove dangerously or recklessly.” In the current study, only items involving binge episodes and vomiting episodes were used. Although data were collected on methods of purging in addition to vomiting (i.e. laxative use, excessive exercise), we did not examine these specific behaviors because there were not enough of these instances reported to have meaningful power for group comparisons of emotional trajectories before and after each behavior.
Procedures
The current research was approved by the Institutional Review Boards at the University of North Dakota and MeritCare Medical Center. During the baseline assessment, participants provided written informed consent and completed a baseline assessment to ensure eligibility. Next participants were trained in the use of a digital monitoring device (PalmPilot™ Vx). Participants then followed the assessment protocol for two days of practice, during which time they were asked to record just as they would during actual data collection.
Following the practice period, data were examined by study staff to confirm that they were input correctly (these practice data were not used in the subsequent analyses). Next, a 14-day data collection period began. During this time, participants were instructed to carry the device with them at all times, as they were prompted by random signal-continent recordings and event-continent recordings throughout the day (Wheeler & Reis, 1991). For each type of recording, participants were asked to complete ratings of their mood and behaviors. Signal-contingent recording prompted participants to complete mood ratings six times throughout the day when the portable digital device signaled them. The device signaled participants at a random following a stratified anchor blocks, and participants were to record data within 30-45 minutes of being signaled. In addition, event-contingent recording was employed as participants were asked to enter data whenever they engaged in eating disordered behaviors (e.g., binge eating, laxative use, etc.) or self-destructive behaviors (e.g., self-injury, drug abuse, etc.).
Upon completion of data collection, participants returned the device and their data were reviewed by study staff with the participant present to ensure that any potential confusion with recordings could be addressed and clarified by the participant. Participants received $100 for each week that they recorded data on the portable digital device and those participants who responded to 85% of the signal-contingent prompts within 45 minutes were given an additional $50 bonus.
Data Analytic Strategy
Patients were classified as either having BPD as a co-occurring diagnosis (BN+BPD), or no BPD diagnosis (BN-BPD), and preliminary analyses examined group differences on age, BMI, race, and marital status. Daily emotional variability was calculated separately for each participant on each separate day of EMA recording, using that person’s standard deviation from their daily average of momentary emotion ratings. In all analyses we controlled for presence of another Axis I disorder besides BN to ensure that findings were not an artifact of comorbidity in general.
A series of multilevel models were conducted in the Mixed module of SPSS 19.0.0 and used to evaluate how emotion ratings differed between the BN+BPD and BN-BPD groups. The equations for these models are displayed below, with (i) referring to the daily observation in the first set, and momentary (signal) observations in the second set. All of these observations were nested within each individual (j). In these models bulimic event days were classified as days in which (1) either binge eating and/or vomiting occurred, or neither occurred (0). Those with BN+BPD were code (1), while those with BN-BPD were coded (0) in analyses. The first set refers to the models analyzing differences in emotional variability, the second set refers to the models analyzing emotional responding before and after binge eating or vomiting.
Set 1: Daily Emotional Variability
Level 1: (PEij or NEij) = β0j + β1j(Bulimic Event Day)ij
Level 2 (individual): β0j = γ00 + γ01(Group)j + u0j
β1j = γ10 + γ11 (Group)j
Reduced Equation: (daily PEij or NEij) = γ00 + γ10(Bulimic Event Day)ij +
γ01(Group)j + γ11(Group*Bulimic Event Day)j + u0j
Set 2: Momentary Emotional Trajectory Models Pre- or Post-, Binge eating or Vomiting
Level 1: (PEij or NEij) = β0j + β1j(Time)ij + β2j(Time2)ij
Level 2 (individual): β0j + γ00 + γ01(Group)j + u0j
β1j = γ10 + γ11(Group)j
β2j = γ20 + γ21(Group)j
β3j = γ30 + γ31(Group)j
Reduced Equation: (daily PEij or NEij) = γ00 + γ10(Time)ij + γ20(Time2)ij +γ01(Group)j +
γ11(Group*Time)j + γ21(Group*Time2)j + u0j
The first set of models displays the analyses examining individual daily variability of NA or PA as the dependent variable, with levels for each day, and between each participant. Effects in the model were specified for a random intercept and fixed effects for daily experience of a bulimic event, group, and a cross-level interaction effect for bulimic event day modified by group status.
The second set of models displays momentary emotional trajectories pre- and post-either binge eating or vomiting. Separate models were run for binge eating and vomiting; and pre-event and post-event emotion ratings were included in the same model. Only days on which binge eating or vomiting occurred were included in these analyses. The dependent variables for this set of models were momentary levels of NA and PA. A continuous variable was created representing time (in hours) prior to or following a report of binge eating or vomiting, with zero representing the occurrence of the event. Mixed models included a random intercept Level 2 intercept, and fixed effects for group, time in relation to the event (i.e., linear component), time-squared (i.e., quadratic component), group-by-time, group-by-time-squared, and group-by-time-cubed. Pre- and post-event trajectories were modeled by including interactions between pre/post (0=pre-behavior; 1=post-behavior) and all time effects.
Results
Preliminary analyses
Participants had a mean age of 25.3 years (SD=7.6; range=18-55), were predominantly Caucasian (97.0%), and single/never married (76.8%). Most were well-educated, with 99.2% having completed high school and 82.0% having completed at least some college. The mean body mass index (BMI; kg/m2) for the sample was 23.9 (SD=5.2; range=17.1-47.6), which is considered to be in the normal range.
The validity of the use of the DIB-R 2 Year Total score to estimate BPD diagnoses was supported by a principal components analysis (PCA) with all items included, which supported the four-factor structure (results not shown) designed by the authors of the scale (Zanarini et al., 1989). Convergent validity of the DIB-R diagnosis with the WIPSI Borderline scale was established by examining group differences between the BN+BPD and BN-BPD groups on WISPI Borderline scale score. The groups were significantly different (t[130]= −4.06, p<.001), with the BN+BPD group (M=90.08, SD=29.59) scoring higher than the BN-BPD group (M=65.51, SD=26.72) on the WISPI Borderline scale. Using the DIB-R, a BPD diagnosis was given to 25 participants, as opposed to 33 participants given BPD diagnoses using the WISPI Borderline scale, suggesting that the DIB-R provided a valid and conservative measure of BPD diagnosis.
The BN+BPD group (n=25) did not differ from the BN-BPD group (n=108) on race, highest level of education, BMI, or frequency of binge eating and vomiting (in last month or lifetime peak). The groups differed on age (t[131]= −2.42, p=.022) and marital status (χ2 [5, N=133]= 11.11, p= .049), with those in the BN+BPD group being significantly older, less likely to be single, and more likely to have been divorced. Regarding comorbidity, current Axis I diagnoses, 54% met criteria for a mood disorder diagnosis, 16% for substance use diagnosis, and 51% for any anxiety disorder. When compared on these major diagnostic categories, there were no significant differences in diagnostic comorbidity for either those with BN or BN/BPD.
Regarding momentary analyses, approximately 75% of responses initiated recording within 20 minutes of being signaled, with an average response time of 11.92 minutes (SD=65.21)2. For overall number of binges reported during monitoring, those with BN+BPD (M=.61, SD=.87) did not report significantly more binge episodes than those with BN-BPD (M=.61, SD=.82; F(1, 130)=.06, p>.05.). Those in the BN+BPD group (M=.83, SD=1.03) also did not report significantly more total vomiting episodes than those with BN-BPD (M=.78, SD=.98; F(1, 130) = .98, p>.05).
Daily Emotional Variability
Negative emotion was significantly (γ=.69, p=.028) more labile on days in which bulimic events occurred (LS mean=5.22, SE=2.95) than days in which no bulimic events occurred (LS mean=3.80, SE=2.81). However, variability in negative emotion did not differ significantly by group (γ=.03, p=.89). There was a significant group-by-bulimic event day (i.e., binge, purge) interaction (γ=.88, p=.011), indicating that the variability in negative emotion on bulimic event days was higher for the BN+BPD group (See Table 1). Variability in positive emotion was not significantly different on bulimic event days than for days in which no bulimic events occurred (γ=.40, p=.21). However, there was a significant group effect on variability of emotion (γ= −.78, p<.001), with the BN-BPD group (LS mean=5.50, SE=2.98) showing more variability in PE than the BN+BPD group (LS mean=4.86, SE=2.56). There was no significant interaction effect on positive emotion for bulimic event day and group (γ=.28, p=.43). Presence of an additional Axis I diagnosis was not significant for either analysis.
Table 1.
Between-days multilevel models for bulimic events
| Parameter | γ | SE | t | p |
|---|---|---|---|---|
| Negative Emotional Variability | ||||
| Intercept | −5.24 | 0.19 | −26.96 | <.001 |
| Bulimic event day | 0.69 | 0.31 | 2.21 | .028 |
| Group | 0.03 | 0.22 | 0.14 | .890 |
| Group × Bulimic event day | 0.88 | 0.34 | 2.56 | .011 |
|
| ||||
| Positive Emotional Variability | ||||
| Intercept | −5.02 | 0.20 | −25.73 | 1.0 |
| Bulimic event day | 0.40 | 0.31 | 1.27 | .205 |
| Group | −0.78 | 0.22 | −3.56 | <.001 |
| Group × Bulimic event day | 0.28 | 0.35 | 0.80 | .425 |
Note. Bulimic event day is coded 1 for bulimic event day and 0 for no bulimic event day. Group is coded 1 for borderline personality disorder (BN+BPD) and 0 for no borderline personality disorder (BN−BPD). Analyses controlled for presence of another Axis I disorder besides BN, which is not displayed.
Emotional Trajectories Surrounding Dysregulated Eating Behaviors
Negative Emotion
Binge Eating
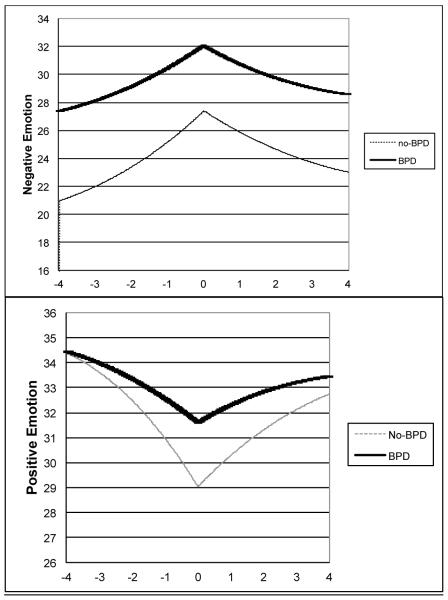
Prior to binge eating negative emotion significantly increased as a function of time (linear γ=2.44, SE=.136, p<.001; quadratic γ=.233, SE=.020, p<.001), and following the binge it significantly decreased as time progressed (linear γ= −4.13, SE=.240, p<.001; quadratic γ = −.070, SE=.028, p=.014). While the overall level of negative emotion around binge eating was higher for the BN+BPD group (group γ=4.67, SE=2.05, p=.024), the trajectory of negative emotion did not differ significantly between groups either prior to (linear difference γ=-.651, SE=.358, p=.069; quadratic difference γ= −.063, SE=.053, p=.24) or after (linear difference estimate=.861, SE=.616, p=.16; quadratic difference estimate=.070, SE=.074, p=.35) binge eating (See Table 2; Figure 1). Presence of an alternate Axis I disorder besides BN was not significant in this model, or the subsequent analyses.
Table 2.
Within-days multilevel models for binge events
| Parameter | γ | SE | t | p |
|---|---|---|---|---|
| Negative Emotion | ||||
| Antecedent | ||||
| Intercept | 27.40 | .849 | 32.26 | <.001 |
| Hours prior to event | 2.44 | .136 | 18.03 | <.001 |
| (Hours prior to event)2 | .233 | .020 | 11.66 | <.001 |
| Group | 4.67 | 2.05 | 2.28 | .024 |
| Group × Hours prior to event | −.651 | .358 | −1.82 | .069 |
| Group × (Hours prior to event)2 | −.063 | .053 | −1.18 | .238 |
| Consequent | ||||
|
| ||||
| Hours following event | −4.13 | .240 | −17.25 | <.001 |
| (Hours following event)2 | −.070 | .028 | −2.45 | .014 |
| Group × Hours following event | .861 | .616 | 1.40 | .162 |
| Group × (Hours following event)2 |
.070 | .074 | .94 | .347 |
|
| ||||
| Positive Emotion | ||||
| Antecedent | ||||
|
| ||||
| Intercept | 29.03 | .695 | 41.77 | <.001 |
| Hours prior to event | −2.16 | .137 | −15.73 | <.001 |
| (Hours prior to event)2 | −.229 | .020 | −11.28 | <.001 |
| Group | 2.57 | 1.71 | 1.51 | .133 |
| Group × Hours prior to event | 1.11 | .363 | 3.07 | .002 |
| Group × (Hours prior to event)2 | .142 | .054 | 2.63 | .008 |
| Consequent | ||||
|
| ||||
| Hours following event | 3.53 | .243 | 14.54 | <.001 |
| (Hours following event)2 | .106 | .029 | 3.67 | <.001 |
| Group × Hours following event | −1.68 | .624 | −2.70 | .007 |
| Group × (Hours following event)2 |
−.120 | .075 | −1.59 | .112 |
Note. Group is coded 1 for borderline personality disorder (BN+BPD) and 0 for no borderline personality disorder (BN−BPD). Analyses controlled for presence of another Axis I disorder besides BN, which is not displayed.
Figure 1.
Negative and positive emotion during the hours pre- and post-binge event by group.
Vomiting
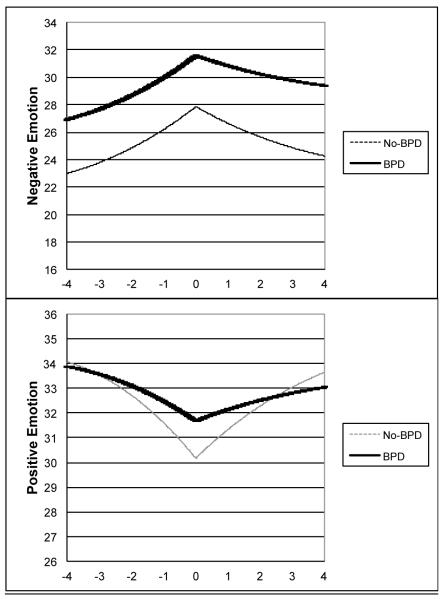
Similar to the pattern for binge eating described above, negative emotion significantly increased prior to vomiting (linear γ=1.82, SE=.127, p< .001; quadratic γ =.168, SE=.020, p<.001) and significantly decreased after vomiting (linear γ= −3.16, SE=.220, p<.001; quadratic γ= −.047, SE=.026, p=.07). The overall level of negative emotion around vomiting was higher for the BN+BPD group, but did not reach statistical significance (group γ=3.73, SE=2.08, p=.08). Also similar to above, the trajectory of negative emotion did not differ significantly between groups either prior to (linear difference estimate= −.049, SE=.334, p=.88; quadratic difference estimate=.004, SE=.051, p=.94) or after (linear difference estimate=.560, SE=.568, p=.325; quadratic difference estimate= −.048, SE=.072, p=.51) vomiting (See Table 2; Figure 1).
Positive Emotion
Binge Eating
Across groups, positive emotion significantly decreased prior to binge eating (linear γ= −2.16, SE=.137, p<.001; quadratic γ= −.229, SE=.020, p<.001) and significantly increased after binge eating (linear γ=3.53, SE=.243, p<.001; quadratic γ=.106, SE=.029, p<.001). The overall level of positive emotion around binge eating did not differ significantly between groups (group γ=2.57, SE=1.71, p=.13). However, there were distinct differences in the trajectory of positive emotion between the BN+BPD and BN-BPD groups. Prior to binge eating, the decrease in positive emotion was less pronounced for the BN+BPD group (linear difference estimate=1.11, SE=.363, p=.002; quadratic difference estimate=.142, SE=.054, p=.008); after binge eating, the linear (but not curvilinear) increase in positive emotion was less pronounced for the BN+BPD group (linear difference estimate= −1.68, SE=.624, p=.007; quadratic difference estimate= −.120, SE=.075, p=.11; See Table 3; Figure 2).
Table 3.
Within-days multilevel models for vomit events
| Parameter | γ | SE | t | p |
|---|---|---|---|---|
| Negative Emotion | ||||
| Antecedent | ||||
| Intercept | 27.86 | .822 | 33.89 | <.001 |
| Hours prior to event | 1.82 | .127 | 14.35 | <.001 |
| (Hours prior to event)2 | .168 | .020 | 8.59 | <.001 |
| Group | 3.73 | 2.08 | 1.79 | .075 |
| Group × Hours prior to event | −.049 | .334 | −.15 | .883 |
| Group × (Hours prior to event)2 | .004 | .051 | .08 | .936 |
| Consequent | ||||
|
| ||||
| Hours following event | −3.16 | .220 | −14.38 | <.001 |
| (Hours following event)2 | −.047 | .026 | −1.80 | .073 |
| Group × Hours following event | .560 | .568 | .98 | .325 |
| Group × (Hours following event)2 |
−.048 | .072 | −.66 | .508 |
|
| ||||
| Positive Emotion | ||||
| Antecedent | ||||
|
| ||||
| Intercept | 30.17 | .750 | 40.21 | <.001 |
| Hours prior to event | −1.60 | .139 | −11.53 | <.001 |
| (Hours prior to event)2 | −.173 | .021 | −8.08 | <.001 |
| Group | 1.51 | 1.92 | .79 | .434 |
| Group × Hours prior to event | .711 | .364 | 1.95 | .051 |
| Group × (Hours prior to event)2 | .080 | .056 | 1.44 | .150 |
| Consequent | ||||
|
| ||||
| Hours following event | 2.88 | .240 | 11.99 | <.001 |
| (Hours following event)2 | .057 | .029 | 1.98 | .048 |
| Group × Hours following event | −1.46 | .622 | 2.35 | .019 |
| Group × (Hours following event)2 |
−.020 | .079 | −.26 | .797 |
Note. Group is coded 1 for borderline personality disorder (BN+BPD) and 0 for no borderline personality disorder (BN–BPD). Analyses controlled for presence of another Axis I disorder besides BN, which is not displayed.
Figure 2.
Trajectories of negative and positive emotion during the hours pre- and post-vomit event by group.
Vomiting
Positive emotion significantly decreased prior to vomiting (linear γ= −1.60, SE=.139, p<.001; quadratic γ= −.173, SE=.021, p<.001) and significantly increased after vomiting (linear γ=2.88, SE=.240, p<.001; quadratic γ=.057, SE=.029, p=.048). The overall level of positive emotion around vomiting did not differ significantly between groups (group γ=1.51, SE=1.92, p=.43). However, again there were distinct differences in the trajectory of positive emotion between the BN+BPD and BN-BPD groups. Prior to vomiting, the decrease in positive emotion was less pronounced for the BN+BPD group, with the linear estimate approaching statistical significance (linear difference estimate=.711, SE=.364, p=.051; quadratic difference estimate=.080, SE=.056, p=.15); after vomiting, the linear (but not curvilinear) increase in positive emotion was less pronounced for the BN+BPD group (linear difference estimate= −1.46, SE=.622, p=.019; quadratic difference estimate= −.020, SE=.079, p=.80; See Table 3; Figure 2).
Other Dysregulated Behaviors
Because other potentially harmful behaviors, such as substance use and self-injury, may also be used to regulate emotion (Selby & Joiner, 2009), we examined potential group differences in other behaviors and the potential for other behaviors reported in close temporal proximity to binge or vomiting episodes. Those with BPD diagnoses had a significantly higher rate of any substance use dependence diagnosis (including alcohol) in the last month (BN+BPD=38%, BN-BPD=25%, X2=6.4, p<.05). However, no significant group differences were found for total reports of substance use during monitoring (BN+BPD M=.16, SD=.59; BN-BPD M=.15, SD=.59; F(1, 130)=.11, p>.05), but the BPD group did report more uses of alcohol (BN+BPD M=1.38, SD=1.98; BN-BPD M=1.00, SD=2.00; F(1,130)=20.20, p<.001). Despite those with BPD having more alcohol uses, number of alcohol uses was not significantly associated with either binge episodes (r=.12, p>.05), or vomit episodes (r=.04, p>.05). Furthermore, when we examined the relationship between substance dependence diagnosis and the average level of positive or negative emotion aggregated across all momentary assessments, those with substance dependence did not report significantly more negative emotion (F(1,130)=.45, p>.05) or less positive emotion (F(1,130)=.15, p>.05).
Regarding other behaviors, those with BPD reported more total instances of self-injury over monitoring (M=.11, SD=.38) than those without (M=.03, SD=.19; F(1, 130)=81.81, p<.001). Similarly, those with BPD also reported more total spending sprees (M=.51, SD=1.00) than those with out BPD (M=.36, SD=.74; F(1, 130)= 21.31, p<.001). Binge episodes were significantly correlated with simultaneous momentary reports of self-injury (r=.05, p<.001) and impulsive shopping (r=.02, p<.05). Vomiting episodes were also significantly correlated with simultaneous reports of self-injury (r=.06, p<.001) and impulsive shopping (r=.02, p<.05). Although those with BPD reported more impulsive behaviors, the momentary assessments where multiple behaviors occurred were a minority, and the correlations between these behaviors and eating behaviors were small. Furthermore, those with substance dependence did not report significantly different levels of emotion, and these other behaviors unlikely influenced the overall pattern of findings in this study.
Discussion
BN and BPD are disorders that are frequently comorbid and they share many similarities in emotion dysregulation and impulsive behavior. The purpose of this study was to establish differences in overall emotional variability and emotional responses before and after binge eating and vomiting between those with BN and comorbid BPD. Using data from an EMA study, we compared women with BN and no BPD diagnosis (BN-BPD) to those with BN and comorbid BPD (BN+BPD) on variability of negative and positive emotion, and on emotional trajectories before and after binge episodes and vomiting episodes. Contrary to our expectations, those with BPD did not exhibit overall increased emotional variability relative to those without. For both groups, negative emotional variability was also elevated on eating disorder event days, suggesting that emotional variability may have contributed to binge eating and/or vomiting. There was, however, a significant interaction where those with BPD experienced greater negative emotional variability on bulimic event days than those without BPD, supporting our second hypothesis. On the other hand, those without BPD (BN-BPD) actually exhibited significantly higher levels of positive emotion variability in general, with no differences in eating disorder event days or group interaction.
Concerning our third and fourth hypotheses, negative emotion prior to a binge was elevated for the BN+BPD group relative to the BN-BPD group, however, there were no significant group differences in increases of positive emotion as a function of time leading up to binge episodes. Following the binge episode, both groups demonstrated elevations in negative emotion as a function of time, but there were no significant group differences in magnitude of negative emotion or group interaction with time predicting higher increases in negative emotion. Regarding negative emotion surrounding vomiting, both groups demonstrated increasing negative emotion before, and decreasing negative emotion after, however there were no significant group differences or group by time interactions. In terms of positive emotion, before and after binge episodes those with BN only demonstrated steeper trajectories with positive emotion decreasing more prior to a binge and showing a larger increase after a binge than those with BPD. On the other hand, there were no differences in trajectory of positive emotion prior to a vomit episode, although both groups demonstrated decreasing positive emotion. After binge episodes there was a significantly steeper trajectory of positive emotion for those with BN only, as indicated by a significant group by time interaction.
Overall, these findings provided some support for our hypothesized additive effect between BPD and BN, and were consistent with the above findings of high emotional variability on bulimic event days in this group. The comorbid condition of BPD and BN may result in an additive higher set point of overall negative emotion, but with both groups experiencing similar variability of negative emotion. However, those with BPD may experience elevated negative emotional variability on days with binge and vomit episodes. Regarding positive emotion variability, we found that contrary to expectations those with BPD experienced less positive variability than those without, when we expected more. These findings on positive emotion indicate that the presence of a BPD diagnoses may actually dampen trajectory of positive emotion in BN, rather than amplify it, and are consistent with other findings that those with BPD may not display increase reactivity of positive emotion (Selby et al., 2009). This finding also leaves to question whether there are problems with variability of positive emotion in BN, and whether potential dysregulation of positive emotion may further contribute to symptoms in the BN group that lacks BPD comorbidity. Perhaps an important function of dysregulated eating behaviors in BN may be increasing positive emotion, in combination with reducing negative emotion, rather than in comorbid BN and BPD where such behaviors may be primarily to escape negative emotion.
Given the enhanced understanding of emotional variability and emotions surrounding eating disordered behaviors in comorbid BPD and BN, there may be an opportunity to enhance current treatments for BN and BPD. For example, dialectical behavior therapy (Linehan, 1993) is a therapy traditionally used to treat BPD, but recent studies have found that it also has promising potential for the treatment of BN (Safer, Telch, & Agras, 2001). Based on the findings of the current study, DBT may also be a promising intervention to tail to those with comorbid BN and BPD, and important focuses of treatment may focus less on suicidal, self-injurious, or substance use behaviors and instead on eating behaviors such as binging and purging. Modifications might also include examining the potential triggers that elicit negative and positive emotion, to further elucidate if triggers tend to be more interpersonal/situational or weight/shape related. In addition, the specific modules of DBT might be enhanced to focus on eating specific problems, such as focusing on distress tolerance when experiencing concerns about body image. Finally, developing better emotion regulation skills and recognizing that days with worse negative emotion are associated with elevated eating disordered behaviors may help patients with both disorders develop better understanding of how their emotions may influence their behaviors.
There are some limitations to note with the current study. First, because this study did not have a BPD only comparison group, it is difficult to determine if the findings of those with BN and BPD in this sample are due to the comorbidity, or if these effects were primarily driven by BPD. Given BPD is a diagnosis driven by emotional variability, it the presence of this diagnosis alone may have accounted for the effects. This is unlikely, however, given that no main group effect was observed on negative emotional variability. Furthermore, since we controlled for presence of another Axis I disorder besides BN, it is unlikely that comorbidity in general accounted for this effect. Second, BPD diagnosis was made using a cut-off score on the DIB-R. A structured clinical interview for diagnosis of BPD would have been the preferred method for establishing diagnostic validity, although the method used in this study was fairly conservative and consistent across measures of BPD symptoms. However, we used a more conservative measure of BPD symptoms, which ameliorates this concern to some extent. Furthermore, we used BPD diagnosis in analyses for this study to help delineate differences in emotional patterns for comorbid BN and BPD, when use of a dimensional measure of BPD symptoms may have yielded somewhat different results. Another potential concern is that women who were pregnant were not excluded from participating in this study, and we did not maintain records as to whether participants were pregnant or not, so we are unable to empirically examine the impact of pregnancy on our findings. Although it is possible that some participants may have been pregnant, we expect that this would have been only a small minority of participants and would be unlikely to have influenced the result in a major way. However, pregnancy in those with BN could certainly influence the experience of binge episodes and emotional experiences. Finally, data monitoring may have introduced some level of reactivity in the participants, and thereby influenced their ratings or even overall emotional awareness.
Despite these limitations, this study is one of the first to provide an in-depth examination of pathological emotional processes in comorbid BN and BPD. Future studies should examine the potential emotion regulation effects of purging behaviors besides vomiting, and examine if those with comorbid BPD and BN exhibit similar emotional trajectories before and after these behaviors as well, and findings should be replicated in males with BN and BPD. Future studies should also examine scenarios where more than one behavior occurs in the same time frame (i.e. a binge episode along with a self-injury episode) to determine if there are differences in emotional responding relative to when a single behavior occurs. Although the overall pattern of findings in this study was unlikely influenced by simultaneous behaviors occurring along with binge and vomiting episodes, examining the emotional responding surrounding instances of multiple behaviors is an important direction for future research. Such research may enhance our understanding of the emotion regulation function of such behaviors occurring in close proximity to each other. Furthermore, those with BPD and BN should be compared to a group of those with BPD only. Doing so may provide further evidence of an additive effect or it may provide evidence that, as in positive emotion, BPD may simply mask the negative emotional responding of those with BN.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Although approximately 10% of those with BN are male (APA, 1994), males with BN were not included in the present study because they make up such a small percentage of the disorder that we would have been unable to make meaningful comparisons by sex due to low power.
Only 12 women were classified as late responders (less than 85% of their responses occurring within the 45 minute time interval), and there were no significant differences in number of late-responders for those with and without BPD (χ2(1)=1.28, p>.05). There was no significant correlation between late recordings and negative emotion (r= −.011, p>.05), however there was a significant correlation between late recordings and positive emotion (r=.09, p<.001). The correlation between a late recording and positive emotion may have been due to circumstances such as being involved in an engaging activity, and given the small magnitude of the correlation and non-significant correlation with negative emotion, these analyses suggest that lateness of responding did not influence emotional recordings in a major way. Late responders reported fewer overall binge episodes (M=.46, SD=.71) than those who were not late (M=.62, SD=.47; F(1, 130)=39.17, p<.001), and they also reported fewer vomit episodes (M=.53, SD=.70) than those where were not late (M=.81, SD=1.00; F(1, 30)=96.30, p<.001). Given that late responders reported fewer binge and vomit episodes, it is unlikely that late responding overly influenced the findings, although it is possible that they were failing to report such episodes.
Contributor Information
Edward A. Selby, Rutgers University.
Peter Doyle, The University of Chicago.
Daniel Le Grange, The University of Chicago.
References
- Agras WS, Telch CF. The effects of caloric deprivation and negative affect on binge eating in obese binge-eating disordered women. Behavior Therapy. 1998;29:491–503. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed Author; Washington, DC: 1994. [Google Scholar]
- Anestis MD, Selby EA, Crosby RD, Wonderlich SA, Engel SG, Joiner TE. A comparison of retrospective self-report versus ecological momentary assessment measures of affective lability in the examination of its relationship with bulimic symptomatology. Behaviour Research and Therapy. 2010;48:607–613. doi: 10.1016/j.brat.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Kendler KS. Medical and psychiatric morbidity in women with and without binge eating. International Journal of Eating Disorders. 2002;32:72–78. doi: 10.1002/eat.10072. [DOI] [PubMed] [Google Scholar]
- Cassin SE, von Ranson KM. Personality and eating disorders: A decade in review. Clinical Psychology Review. 2005;25:895–916. doi: 10.1016/j.cpr.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Cooper P, Fairburn C. The validity of the Eating Disorder Examination and its subscales. British Journal of Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. 1989. [DOI] [PubMed] [Google Scholar]
- Crosby RD, Wonderlich SA, Engel SG, Simonich H, Smyth J, Mitchell JE. Daily mood patterns and bulimic behaviors in the natural environment. Behaviour Research and Therapy. 2009;47:181–188. doi: 10.1016/j.brat.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12th ed Guilford Press; New York: 1993. pp. 317–331. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. The Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID/P) Biometrics Research Department, New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis II personality disorders (SCID-II) American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Godt K. Personality disorders in 545 patients with eating disorders. European Eating Disorders Review. 2008;16:94–99. doi: 10.1002/erv.844. [DOI] [PubMed] [Google Scholar]
- Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. Journal of Consulting and Clinical Psychology. 68:95–102. [PubMed] [Google Scholar]
- Henry C, Mitropoulou V, New AS, Koenigsberg HW, Silverman J, Siever LJ. Affective instability and impulsivity in borderline personality and bipolar II disorders: Similarities and differences. Journal of Psychiatric Research. 2001;35:307–312. doi: 10.1016/s0022-3956(01)00038-3. [DOI] [PubMed] [Google Scholar]
- Klein M, Benjamin L, Rosenfeld R, Treece C, Husted J, Greist J. The Wisconsin Personality Disorders Inventory: Development and psychometric characteristics. Journal of Personality Disorders. 1993;7:285–303. [Google Scholar]
- Klonsky ED. What is emptiness? Clarifying the 7th criterion for borderline personality disorder. Journal of Personality Disorders. 2008;22:418–426. doi: 10.1521/pedi.2008.22.4.418. [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW, Harvey PD, Mitropoulou V, Schmeidler J, New AS, Goodman M, et al. Characterizing affective instability in borderline personality disorder. American Journal of Psychiatry. 2002;159:784–788. doi: 10.1176/appi.ajp.159.5.784. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Gorin A, Catley D, Stone AA. Does momentary assessment detect binge eating in overweight women that is denied at interview? European Eating Disorders Review. 2001;9:309–324. [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment for borderline personality disorder. Guilford Press; New York: 1993. [Google Scholar]
- Lynch WC, Everingham A, Dubitzky J, Hartman M, Kasser T. Does binge eating play a role in the self-regulation of moods? Integrative Physiological and Behavioral Science. 2000;35:298–313. doi: 10.1007/BF02688792. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Engel SG, Crosby RD, Wonderlich SA, Simonich H, Mitchell JE. Emotional states preceding and following acts of non-suicidal self-injury in bulimia nervosa patients. Behavior Research and Therapy. 2009;47:83–87. doi: 10.1016/j.brat.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers TC, Wonderlich SA, Crosby R, Mitchell JE, Steffen KJ, Smyth J, Miltenberger Is multi-impulsive bulimia a distinct type of bulimia nervosa: Psychopathology and EMA findings. International Journal of Eating Disorders. 2006;39:655–661. doi: 10.1002/eat.20324. [DOI] [PubMed] [Google Scholar]
- Rizvi S, Peterson C, Crow S, Agras W. Test-retest reliability of the Eating Disorder Examination. International Journal of Eating Disorders. 2000;28:311–316. doi: 10.1002/1098-108x(200011)28:3<311::aid-eat8>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Rosen J, Vara L, Wendt S, Leitenberg H. Validity studies of the Eating Disorder Examination. International Journal of Eating Disorders. 1990;9:519–528. [Google Scholar]
- Russell JJ, Moskowitz DS, Zuroff DC, Sookman D, Paris J. Stability and variability of affective experience and interpersonal behavior in borderline personality disorder. Journal of Abnormal Psychology. 2007;116:578–588. doi: 10.1037/0021-843X.116.3.578. [DOI] [PubMed] [Google Scholar]
- Safer DL, Telch CF, Agras WS. Dialectical behavior therapy for bulimia nervosa. American Journal of Psychiatry. 2001;158:632–634. doi: 10.1176/appi.ajp.158.4.632. [DOI] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Bender TW, Joiner TE., Jr An exploration of the emotional cascade model in borderline personality disorder. Journal of Abnormal Psychology. 2009;118:375–387. doi: 10.1037/a0015711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Joiner TE. Understanding the relationship between emotional and behavioral dysregulation: Emotional Cascades. Behaviour Research and Therapy. 2008;46:593–611. doi: 10.1016/j.brat.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Selby EA, Joiner TE. Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Review of General Psychology. 2009;13:219–229. doi: 10.1037/a0015687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shedler J, Westen D. Refining personality disorder diagnosis: Integrating science and practice. American Journal of Psychiatry. 2004;161:1350–1365. doi: 10.1176/appi.ajp.161.8.1350. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, et al. Daily and momentary mood and stress are associated with being eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Annals of Behavioral Medicine. 1994;16:199–202. [Google Scholar]
- Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, Watson D. Affective instability: Measuring a core feature of borderline personality disorder with ecological momentary assessment. Journal of Abnormal Psychology. 2008;117:647–661. doi: 10.1037/a0012532. [DOI] [PubMed] [Google Scholar]
- Vanderlinden J, Vendereycken W. Trauma, dissociation, and impulse dyscontrol in eating disorders. Brunner Mazel; Bristol, PA: 1997. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wegner KE, Smyth JM, Crosby RD, Wittrock D, Wonderlich SA, Mitchell JE. An evaluation of the relationship between mood and binge eating in the natural environment using ecological momentary assessment. International Journal of Eating Disorders. 2002;32:352–361. doi: 10.1002/eat.10086. [DOI] [PubMed] [Google Scholar]
- Wheeler L, Reis HT. Self-recording of everyday life events: Origins, types, and uses. Journal of Personality. 1991;59:339–354. [Google Scholar]
- Wonderlich SA, Crosby R, Engel S, Mitchell JE, Smyth J, Miltenberger R. Personality-based clusters in bulimia nervosa: Differences in clinical variables and ecological momentary assessment. Journal of Personality Disorders. 2007;21:340–357. doi: 10.1521/pedi.2007.21.3.340. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Mitchell JE. Eating disorders and personality disorders. In: Yager J, Gwirtsman HE, Edelstein CK, editors. Special problems in the management of eating disorders. American Psychiatric Press; Washington, D.C.: 1992. pp. 51–86. [Google Scholar]
- Zanarini MC, Frankenburg FR, Vujanovic AA. Inter-rater and test-retest reliability of the revised diagnostic interview for borderlines. Journal of Personality Disorders. 2002;16:270–276. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The revised diagnostic interview for borderlines: Discriminating BPD from other Axis II disorders. Journal of Personality Disorders. 1989;3:10–18. [Google Scholar]
- Zeeck A, Birindelli E, Sandholz A, Joos A, Herzog T, Hartmann A. Symptom severity and treatment course of bulimic patients with and without a borderline personality disorder. European Eating Disorders Review. 2007;15:430–438. doi: 10.1002/erv.824. [DOI] [PubMed] [Google Scholar]