Abstract
Background
Fewer patients are recorded by practices as having hypertension than are identified in systematic population surveys. However, as more patients are recorded on practice hypertension registers, mortality from coronary heart disease and stroke declines.
Aim
To determine whether the number of GPs per 1000 practice population is associated with the number of patients recorded by practices as having hypertension, and whether patients’ reports of being able to get an appointment with a GP are associated with the number of GPs and the number of patients recorded as having hypertension.
Design and setting
Cross-sectional study of available data for all general practices in England for 2008 to 2009.
Method
A model was developed to describe the hypothesised relationships between population (deprivation, ethnicity, age, poor health) and practice characteristics (list size, number of GPs per 1000 patients, management of hypertension) and the number of patients with hypertension and patient-reported ability to get an appointment fairly quickly. Two regression analyses were undertaken.
Results
Practices recorded only 13.3% of patients as having hypertension. Deprivation, age, poor health, white ethnicity, hypertension management, and the number of GPs per 1000 patients predicted the number of patients recorded with hypertension. Being able to get an appointment fairly quickly was associated with the number of patients recorded with hypertension, age, deprivation, practice list size, and the number of GPs per 1000 patients.
Conclusion
In order to improve detection of hypertension as part of a strategy to lower mortality from coronary heart disease, the capacity of practices to detect hypertension while maintaining access needs to be improved. Increasing the supply of GPs may be necessary, as well as improvements in efficiency.
Keywords: health services accessibility, hypertension, primary health care
INTRODUCTION
Untreated hypertension is an important risk factor for stroke and coronary heart disease, and the detection and management of hypertension is therefore a priority for health services in many countries. However, many people with hypertension have not been detected; for example, in the 2010 Health Survey for England, 14.7% of males and 10.3% of females were found to have untreated hypertension (hypertension defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg).1 The majority of patients with hypertension are managed in primary care, and in England in 2004, a pay for performance financial incentive scheme was introduced to reward GPs for managing chronic conditions including hypertension; the Quality and Outcomes Framework (QOF).2 This scheme requires practices to maintain a register of patients diagnosed with hypertension, and the authors have previously established that the number of people on general practice hypertension registers is associated with population mortality from coronary heart disease3 and stroke;4 greater numbers on hypertension registers are associated with lower mortality. Improved detection followed by systematic management can, therefore, be expected to reduce mortality from these two conditions.
In order to improve detection of vascular risk, a scheme was launched in 2008,5 in which general practices were incentivised to offer a health check to adults aged 40–74 years.6 However, of the 15 879 976 people eligible for a check in the year 2011 to 2012, only 2 201 836 were offered one, and 1 136 892 received one.7 If schemes to improve detection of hypertension and other vascular risk factors are to engage the majority of targeted individuals, it is necessary to understand population and service characteristics that influence detection.
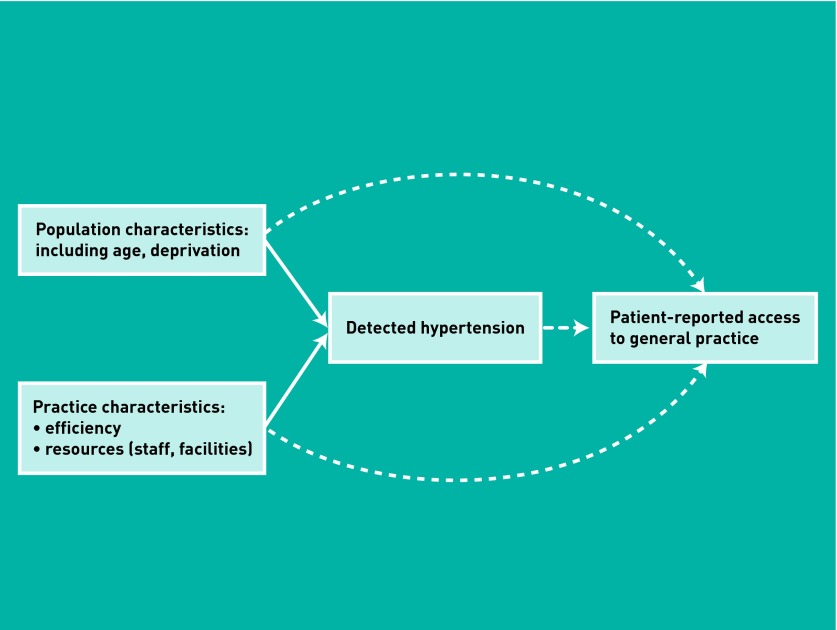
In a study restricted to 146 practices in a single locality, population characteristics (higher numbers of older patients, higher numbers reporting poor health) and practice characteristics (smaller list size, lower patient turnover) were found to be associated with higher numbers of patients recorded on hypertension registers.8 Moreover, as the numbers of patients recorded with hypertension increased, the ability of patients to get an appointment at their practice declined, indicating a relationship between levels of detected disease and the capacity of practices to meet demand for care, and suggesting that to improve hypertension detection, the capacity of practices to manage large numbers of patients with chronic conditions needs to be increased.9 Two approaches may be used to increase capacity, the first being increased resourcing or supply of primary care and the second improved management of the resources available. There is evidence of inequitable distribution of GPs in England and that detection of vascular disease is associated with the supply of GPs.10 In order to explore the relationships between population characteristics, the capacity of primary care, and the detection of hypertension, a model was developed depicting how these factors may interact (Figure 1). In the model, primary care characteristics include supply or resources (staff, facilities), and the management of those resources in delivering primary care. One hypothesis derived from the model is that better management of available resources would improve the capacity of practices to detect hypertension. A second hypothesis is that increased detection of disease will be associated with reduced access to care, but that increased supply of primary care will reduce this effect. In order to provide evidence to those designing primary care services in ways that reduce population mortality, this study was undertaken to evaluate the model, using data from all general practices in England.
Figure 1.
Hypothesised model of population and primary care characteristics influencing detection of hypertension (unbroken line) and the impact of the amount of detected hypertension on access (broken line). Detection of hypertension is associated with mortality from heart disease and stroke.3,4
How this fits in
Hypertension is among the commonest of chronic conditions, but although it is a risk factor for stroke and coronary heart disease, many people with hypertension remain undiagnosed. In this cross-sectional study of all general practices in England, 2008–2009, the population and general practice characteristics influencing detection of hypertension, and also the impact of numbers of patients with hypertension on patient reports of ability to get an appointment with a GP were investigated. The findings suggest that access declines as the number of patients with hypertension increases, but greater numbers of GPs per 1000 patients was associated with detecting more patients with hypertension and with improved access. The capacity of some practices to both detect and manage chronic conditions, while also maintaining access, appears to be inadequate.
METHOD
The study was cross-sectional, and used publicly available data for the year 2008–2009. Data from the QOF provided the numbers of patients on practice hypertension registers.11 The registers include patients who have been recorded by practices as having a diagnosis of hypertension. In some cases, patients recorded as hypertensive may not, in fact, have hypertension; there may also be some patients who have been diagnosed with hypertension but have not been entered into the register. Nevertheless, the registers provide the basis for systematic recall and patient management, and practices are incentivised by the QOF to maintain them; they therefore provide a good indication of the numbers of patients under management for hypertension.
As a measure of access as reported by patients, information from the annual GP Patient Survey was used. The 2008–2009 survey was sent to samples of patients of all practices in England in January 2009, by Ipsos MORI.12 This involved 5.7 million patients aged 18 years, with 2.2 million responding. The practice sample size was calculated to produce a confidence interval of ±7% for the two questions used to calculate incentive payments to practices, whether patients who had wanted to get an appointment with a GP in the previous 6 months had been able to see a GP fairly quickly (on the same day or the next 2 days the practice was open), and whether, the last time they wanted, they were able to get an appointment more than 2 full days in advance. In the present study, the question on being able to get an appointment fairly quickly was used, since it is important that patients with urgent problems are seen quickly. The data at practice level are freely available from the Department of Health.13
In the conceptual model (Figure 1), population and primary care characteristics are hypothesised to predict levels of detected hypertension, and detected hypertension is hypothesised to predict access. The population characteristics included in the analysis were:
the proportion of patients per practice aged ≥65 years, with this information being provided on request by the NHS Information Centre;14
a measure of socioeconomic deprivation, the Index of Multiple Deprivation estimated for 2007 (IMD 2007).15 The IMD is derived from 38 indicators in seven domains (income, employment, education, health, housing, the environment, and crime), with higher scores indicating greater deprivation;
the proportion of the practice population of white ethnicity, from practice-level estimates derived from hospital admissions data over 2 years (2005–2006 to 2006–2007), provided by the Eastern Region Public Health Observatory;16 and
the proportion of the responders to the GP Patient Survey reporting their health as poor. The survey includes a question on health, worded ‘In general, would you say your health is excellent, very good, good, fair or poor?’.
Two practice characteristics were used to represent aspects of the management of practices in detecting and managing hypertension. The efficiencies of scale available to larger practices can enable them to more readily invest management staff and systems in the detection and management of chronic disease.17 As an indicator of a practice’s management of its care for individuals with hypertension, QOF points for hypertension management were used.18 In the framework, overall clinical performance in each disease domain is summarised in points calculated from the level of achievement of specific indicators, which for hypertension involved three indicators: maintenance of a register; the percentage of patients with hypertension with a blood pressure recorded in the past 9 months; and the percentage with a blood pressure ≤150/90 mmHg.19 As a measure of supply of primary care, information on the full-time equivalent number of GPs per 1000 patients was used; the data were provided on request by the NHS Information Centre.20
Analysis
The analysis sought to investigate the two hypotheses arising from the conceptual model. First, descriptive analysis of the study variables was undertaken. Secondly, a negative binomial regression was undertaken, with numbers of patients recorded on practice hypertension registers as the dependent variable, and variables for population and practice characteristics as the explanatory variables. The aim was to test the hypothesis that practices with greater capacity will have detected more individuals with hypertension. Finally, a second regression was undertaken, with the proportion of GP Patient Survey responders reporting being able to get an appointment fairly quickly as the dependent variable, and population and primary care characteristics as the explanatory variables. The hypothesis being tested here was that greater reported access is associated both with higher levels of capacity and also with lower levels of detected disease. A negative binomial regression analysis seeks to associate candidate predictor variables with an outcome. The incident rate ratio (IRR) for a particular predictor variable explains how much the expected count changes for a one-unit increase in that predictor variable, while holding all the other predictor variables constant. The different numbers of people at risk in the different practices were adjusted for by creating an offset variable for each practice, and by calculating the natural log of the practice list size and entering this into the model as a covariate, but forcing it to have a coefficient of 1.21 All analyses were carried out using SAS (version 9.3).
RESULTS
Information on the number of patients recorded on QOF hypertension registers was available for 8261 practices. For some practices, information about some of the explanatory variables was not available, and with 15 practices the data on the number of GPs per 1000 patients were implausibly high (<2) and were excluded, leaving 8052 (97.5%) practices included in the first regression model and 8079 (97.8%) in the second (Table 1). Overall, practices recorded 13.3% of their patients as having hypertension, although the Health Survey for England for 2008 reported 31.7% of adult males and 28.6% of adult females as having hypertension.22
Table 1.
Descriptive statistics (n = 8052)
| Outcomes | Normality (K–S test significance) | Median (IQR) | Mean (SD) |
|---|---|---|---|
| Dependent variable | |||
|
| |||
| Practice hypertension registers | <0.01 | 750 (429 to 1198) | 878 (572) |
|
| |||
| Predictors | |||
| IMD | <0.01 | 21.6 (13.4 to 32.5) | 23.8 (12.7) |
| Age (≥65 years, %) | <0.01 | 15.4 (11.6 to 18.5) | 15.1 (5.3) |
| Ethnicity (white, %) | <0.01 | 93.1 (78.1 to 97.1) | 82.0 (23.6) |
| Proportion reporting poor health | <0.01 | 5.2 (3.6 to 7.5) | 5.8 (3.0) |
| Practice list size | <0.01 | 5883 (3454 to 9118) | 6684 (4059) |
| GPs per 1000 practice population | <0.01 | 0.57 (0.46 to 0.66) | 0.57 (0.18) |
| Proportion of patients on practice hypertension registers | <0.01 | 13.2 (11.2 to 15.4) | 13.3 (3.5) |
| Total Quality and Outcomes Framework points for hypertension management | <0.01 | 83 (83 to 83) | 82.1 (4.3) |
| Proportion of patients able to get an appointment fairly quickly | <0.01 | 86 (78 to 92) | 84.1 (10.7) |
| GP Patient Survey response rate | <0.01 | 0.42 (0.34 to 0.49) | 0.41 (0.10) |
IMD = Index of Multiple Deprivation. K–S = Kolmogorov–Smirnov. IQR = interquartile range. SD = standard deviation.
The first regression supported the first hypothesis (Table 2). Of the population characteristics, higher levels of deprivation, higher numbers of patients aged ≥65 years, higher numbers reporting their health as poor, and higher numbers of patients of white ethnicity were associated with higher numbers of patients being recorded on practice hypertension registers. Of the practice characteristics, practices achieving higher QOF performance for hypertension management (management), and practices with higher numbers of full-time equivalent GPs per 1000 patients (resources) recorded higher numbers of patients on their hypertension registers. An extra GP per 1000 patients would be associated with a 6% increase in detected hypertension. In contrast, larger practices recorded proportionately fewer patients.
Table 2.
Model 1: predictors of numbers of patients on practice hypertension registers adjusted for practice size, n = 8052 in final modela
| Predictor | Beta (95% CI) | IRRb (95% CI) | Effect size | P-value |
|---|---|---|---|---|
| IMD | 0.001 (0.0004 to 0.002) | 1.001 (1.0003 to 1.002) | 0.1% | 0.001 |
| Proportion aged ≥65 years | 0.04 (0.038 to 0.041) | 1.04 (1.03 to 1.05) | 4% | <0.001 |
| Proportion of white ethnicity | 0.000007 (0.000005 to 0.00001) | 1.000007 (1.000004 to 1.00001) | 0.0007% | <0.001 |
| Proportion reporting poor health | 0.013 (0.01 to 0.02) | 1.013 (1.01 to 1.02) | 1.3% | <0.001 |
| Practice list size | −0.000008 (−0.000009 to −0.000007) | 0.999992 (0.999991 to 0.999994) | −0.0008% | <0.001 |
| GPs per 1000 practice population | 0.06 (0.03 to 0.09) | 1.06 (1.03 to 1.1) | 6% | <0.001 |
| Total Quality and Outcomes Framework points for hypertension management | 0.006 (0.004 to 0.008) | 1.006 (1.004. 1.008) | 0.6% | <0.001 |
IMD = Index of Multiple Deprivation. IRR = incident rate ratio.
Statistical model: negative binomial regression, using log of the list size as the offset.
Subtracting 1 from the IRR and then multiplying by 100 gives the percentage change in the expected count for a one-unit increase in the predictor. So for practice deprivation score, for every extra deprivation point, the expected count increases by 0.1%. IRR values less than 1.0 represent decreases and IRR values greater than 1.0 represent increases in the count.
In the second model addressing the second hypothesis (Table 3), patients reported a greater likelihood of being able to get an appointment relatively quickly in practices with a lower number of patients on a hypertension register, smaller list size, lower deprivation, and higher number of older patients, and in practices with a higher number of full-time equivalent GPs per 1000 patients. An increase of one GP per 1000 patients would increase the number of patient reports of being able to get an appointment quickly by 33%.
Table 3.
Model 2: predictors of percentages of patients reporting being able to get an appointment quickly at their practice, n = 8079 in final modela
| Predictor | Beta (95% CI) | IRRb (95% CI) | Effect size | P-value |
|---|---|---|---|---|
| Number of patients on practice hypertension register | −0.0002 (−0.0002 to −0.0001) | 0.9999 (0.9998 to 0.9999 ) | −0.01% | <0.001 |
| GPs per 1000 practice population | 0.28 (0.25 to 0.32) | 1.33 (1.28 to 1.38 ) | 33% | <0.001 |
| Proportion aged ≥65 years | 0.007 (0.005 to 0.009) | 1.01 (1.005 to 1.009) | 1% | <0.001 |
| IMD | −0.0007 (−0.002 to −0.0001) | 0.9994 (0.998 to 0.9999) | −0.06% | 0.013 |
| Practice list size | −0.0001 (−0.0001 to −0.0001) | 0.99987 (0.99987 to 0.99988) | −0.013% | <0.001 |
| Total Quality and Outcomes Framework points for hypertension management | −0.002 (−0.004 to −0.001) | 0.998 0.996 − 0.999 | −0.2% | <0.001 |
IMD = Index of Multiple Deprivation. IRR = incident rate ratio.
Statistical model: negative binomial regression, using log of the list size as the offset.
Subtracting 1 from the IRR and then multiplying by 100 gives the percentage change in the expected count for a one-unit increase in the predictor. So for GPs per 1000 practice population, for every extra GP per 1000, the expected percentage of patients able to get an appointment fairly quickly increases by 33%. IRR values less than 1.0 represent decreases and IRR values greater than 1.0 represent increases in the count.
DISCUSSION
Summary
The findings of the study tend to support the conceptual model. Patient population characteristics (age, deprivation, reported poor health) were found to predict the numbers of people with recorded hypertension. These were higher among practices with a greater number of people of white ethnicity. Since the prevalence of hypertension tends to be higher in non-white compared to white ethnic groups,23 the potential explanations for this finding include less successful detection of hypertension by practices with high proportions of non-white patients and lower use of screening opportunities by non-white patients themselves.
In accordance with the study model, practice characteristics also predicted the numbers of individuals recorded with hypertension, indicating that detection is a function of both the number of patients in the population with hypertension and the success of practices in identifying them. Practices with more GPs per 1000 patients, and those achieving higher points for hypertension management recorded more individuals with hypertension on their registers. However, larger practices did not record more patients; indeed, as practices increased in size, the proportion of patients on registers tended to decline.
As the numbers of people with recorded hypertension in practices increased, fewer patients reported being able to get an appointment quickly, but this was countered by better access among practices with more GPs per 1000 patients. The analyses undertaken therefore suggest that the capacity of some practices to detect hypertension is not sufficient for the populations they serve. Not only is the detection of hypertension lower, but access tends to be worse as well.
Strengths and limitations
This study included all practices in England, providing a comprehensive description of detection of hypertension in the country. However, the study was cross-sectional and has not considered trends in detection of hypertension. Moreover, the study has identified associations only, and does not offer evidence on causation. There were some limitations in the variables included; for example, information on full-time equivalent nurses and healthcare assistants in practices was not available, although these staff can play a role in detecting and managing hypertension. Variables were not included for other conditions in the population associated with hypertension, for example diabetes, stroke, or obesity, although a patient-reported measure of poor health was included. The variables were at practice level and did not account for variation at individual patient level. The measure of the management of the resources available to practices was limited to a clinical aspect of care and practice size, and did not include the cost and efficiency of services. The rates of response to the access survey were variable, and in some practices were low. However, a survey question employed in determining the sample size for each practice was used, and the reliability of the question for calculating the incentive payment to practices has been shown to be high, despite low response rates.24 Although the GP Patient Survey does not offer objective data on whether appointments are available at a practice, it does reflect whether or not practices have the capacity to meet the preferences for access of patients who have many and varied individual circumstances.25 Finally, it should be noted that recent guidelines from the National Institute for Health and Clinical Excellence recommend that the diagnosis of hypertension be made following ambulatory blood pressure monitoring and therefore the Health Survey for England may overestimate the numbers of individuals with hypertension.26
Comparison with existing literature
The study findings are similar to those reported in an analysis undertaken at local authority level,10 and confirm that deprivation is a predictor of detected disease.27 In a multilevel analysis using the Health Survey for England, a greater supply of GPs was associated with a greater number of people reporting good health.28 These findings reflect US studies demonstrating an association between the supply of primary care physicians and measures of health, including mortality.29,30
Implications for practice and research
The study shows that the supply of GPs, detection of hypertension, and patient access to GPs are linked. The findings suggest that there are insufficient GPs in England to achieve high levels of detection of hypertension while at the same time maintaining access to appointments with GPs. However, there may be ways to address this problem other than increasing the number of GPs, for example through improved management of practice appointment systems, or the employment of more practice nurses, but evaluation of such initiatives would be essential. The distribution of GPs in England is not fully matched to need, and policies thus far have not resolved this.31 Since the number of people with chronic disease is increasing, and the proportion with one or more chronic conditions varies between practices,32 action is needed to increase the capacity of practices to detect and manage chronic disease.
Funding
MJ Bankart, Mohammed S Anwar, Nicola Walker and Richard Baker are members of the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for Leicestershire, Northamptonshire and Rutland (LNR). The views expressed in this paper do not necessarily reflect those of the NIHR or the Department of Health.
Ethical approval
The study was a service evaluation project as defined by the National Research Ethics Service, and used publicly available data, and therefore NHS research ethics approval was not required. The study was approved by the University of Leicester Ethics Committee.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.The Information Centre . Health Survey for England 2010 Trend tables. Leeds: The Information Centre; 2011. [Google Scholar]
- 2.NHS Employers . Investing in general practice The New General Medical Services contract. Leeds: NHS Employers; 2003. http://www.nhsemployers.org/SiteCollectionDocuments/gms_contract_cd_130209.pdf (accessed 12 Mar 2013). [Google Scholar]
- 3.Levene LS, Baker R, Bankart MJG, Khunti K. Association of features of primary care with coronary heart disease mortality. JAMA. 2010;304(18):2028–2034. doi: 10.1001/jama.2010.1636. [DOI] [PubMed] [Google Scholar]
- 4.Levene LS, Bankart J, Khunti K, Baker R. Association of primary care characteristics with variations in mortality rates in England: an observational study. PLOs One. 2012;7(10):e47800. doi: 10.1371/journal.pone.0047800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Department of Health . Putting prevention first Vascular checks: risk assessment and management. London: DoH; 2008. [Google Scholar]
- 6.Department of Health . Putting prevention first Vascular checks: risk assessment and management Best practice guidance. London: DoH; 2009. [Google Scholar]
- 7.Department of Health . NHS health checks. Number of eligible people that have been offered and received NHS health checks. London: DoH; 2012. May, http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/Integratedperfomancemeasuresmonitoring/DH_129481 (accessed 12 Mar 2013). [Google Scholar]
- 8.Anwar MS, Baker R, Walker N, et al. Chronic disease detection and access: does access improve detection, or does detection make access more difficult? Br J Gen Pract. 2012 doi: 10.3399/bjgp12X641456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goddard M, Gravelle H, Hole A, Marini G. Where did all the GPs go? Increasing supply and geographical equity in England and Scotland. J Health Serv Res Policy. 2010;15(1):28–35. doi: 10.1258/jhsrp.2009.009003. [DOI] [PubMed] [Google Scholar]
- 10.Soljak M, Samarasundera E, Indulkar T, et al. Variations in cardiovascular disease underdiagnosis in England: national cross-sectional spatial analysis. BMC Cardiovasc Disord. 2011;11:12. doi: 10.1186/1471-2261-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Information Centre for Health and Social Care Quality and Outcomes Framework (QOF) for April 2008 — March 2009, England. Numbers on QOF disease registers and raw prevalence rates by Practice. http://www.ic.nhs.uk/catalogue/PUB05493 (accessed 20 Mar 2013).
- 12.Ipsos MORI . The GP Patient Survey 2008/09 Technical report. London: Ipsos MORI; 2009. http://www.gp-patient.co.uk/results/download/Y3/Y3_AnnualTechnical.pdf (accessed 12 Mar 2013). [Google Scholar]
- 13.Department of Health The GP Patient Survey Practice report Archive unweighted results. http://www.gp-patient.co.uk/results/archive_unweighted/practicereport/ (access 12 Mar 2013).
- 14.The Information Centre . Age distribution of general practice populations. Leeds: The Information Centre; 2012. [Google Scholar]
- 15.Noble M, McLennan D, Wilkinson K, et al. The English indices of deprivation 2007. London: Department for Communities and Local Government; 2007. http://webarchive.nationalarchives.gov.uk/20100410180038/http://communities.gov.uk/documents/communities/pdf/733520.pdf (accessed 20/03/13). [Google Scholar]
- 16.Association of Public Health Observatories Estimated proportion of GP practice populations by ethnic group 2005/06–2006/07. http://www.apho.org.uk/resource/item.aspx?RID=94731 (accessed 12 Mar 2013).
- 17.Mackay DF, Watt GCM. General practice size determines participation in optional activities: cross-sectional analysis of a national primary care system. Prim Care Res Dev. 2010;11:271–279. [Google Scholar]
- 18.The Information Centre . Clinical summary. Quality and Outcomes Framework (QOF) for April 2008–March 2009, England. Leeds: The Information Centre; https://catalogue.ic.nhs.uk/publications/primary-care/qof/qual-outc-fram-08-09-prac/qof-eng-08-09-prac-tabs-clin-dom-lvl-summ.xls (accessed 20 Mar 2013). [Google Scholar]
- 19.NHS Employers . Revisions to the GMS contract 2006/7. London: NHS Employers; 2006. [Google Scholar]
- 20.The Information Centre . General practitioners full time equivalent by GP practice in England 2008 and 2009. Leeds: The Information Centre; 2012. [Google Scholar]
- 21.Hilbe J. Negative binomial regression. Cambridge: Cambridge University Press; 2007. [Google Scholar]
- 22.The Information Centre Joint Health Surveys Unit . Health Survey for England 2008 Trend tables. Leeds: The Information Centre; 2008. [Google Scholar]
- 23.Hull S, Dreyer G, Badrick E, et al. The relationship of ethnicity to the prevalence and management of hypertension and associated chronic kidney disease. BMC Nephrol. 2011;12:41. doi: 10.1186/1471-2369-12-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roland M, Elliott M, Lyratzopoulos G, et al. Reliability of patient responses in pay for performance schemes: analysis of national general practitioner patient survey data in England. BMJ. 2009;339:b3851. doi: 10.1136/bmj.b3851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kontopantelis E, Roland M, Reeves D. Patient experience of access to primary care: identification of predictors in a national survey. BMC Fam Pract. 2010;11:61. doi: 10.1186/1471-2296-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Institute for Health and Clinical Excellence . Hypertension – clinical management of primary hypertension in adults. NICE clinical guideline 127. London: NICE; 2011. [Google Scholar]
- 27.Dixon A, Khachatryan A, Tian Y. Socioeconomic differences in case finding among general practices in England: analysis of secondary data. J Health Serv Res Policy. 2012;17(suppl 2):18–22. doi: 10.1258/jhsrp.2012.011112. [DOI] [PubMed] [Google Scholar]
- 28.Gravelle H, Morris S, Sutton M. Are general practitioners good for you? Endogenous supply and health. CHE Research Paper 20. York: Centre for Health Economics; 2006. [Google Scholar]
- 29.Chang C-H, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries’ health outcomes. JAMA. 2011;305(20):2096–2105. doi: 10.1001/jama.2011.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goddard M, Gravelle H, Hole A, Marini G. Where did all the GPs go? Increasing supply and geographical equity in England and Scotland. J Health Serv Res Policy. 2010;15(1):28–35. doi: 10.1258/jhsrp.2009.009003. [DOI] [PubMed] [Google Scholar]
- 32.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]