INTRODUCTION
The financial challenges faced by the NHS is aligned with significant social, demographic, technological, and cultural change, which collectively challenges the ability of the NHS to meet the needs of society, both now and into the future. Our ageing demography and multimorbidity will require the NHS to do far more than it currently does. Patients and society have a greater expectation for higher quality and a broader range of services from the NHS1 and healthcare technologies have the ability to extend interventions available to improve quality and quantity of life. The need to tackle inequalities in outcomes and variation in NHS provision2 is recognised as part of the transformation of the NHS.
In Boxes 1 and 2 we draw readers to consider an alternative vision of the future: one in which the role of patients and the healthcare system is radically different to the way we currently experience it. Is such a future really that far away? We believe not.
Box 1. A healthcare system of the future
24-hour care in the community
Care provided as a one-stop service
Care personalised to patients, for example, using genomic profiles
Portable and transferable medical records
Care integrated around the needs and wishes of patients
Business models aligned with care models
Box 2. Patients in the future NHS
Actively manage their own healthcare budgets
Incentives for positive health behaviours
Control over their own health records
Access clinicians by different means (for example, internet, email, telephone, face-to-face)
Provide feedback as a means of continually improving quality
Many of the innovations and ideas suggested are already in place, under pilot, or part of government strategy for health service reform in the near future. Personal health budgets are to be rolled out during the next year, GPs are expected to offer email and other forms of consultation by 2015, patient feedback is now an essential part of revalidation and the Quality and Outcomes Framework, integrated models of care delivery are emerging across the country with an evolving evidence base, patient-held records are being trialled in a number of countries across the developed world, genomic profiles are beginning to be used for tailoring of therapies for cancer, values-based healthcare and commissioning are seeking to align payment mechanisms with the desires and wishes of patients, and responsibility for the delivery of 24 hours care is likely to return to GPs in the coming years.
WITH THAT CONTEXT IN MIND THEN WHAT KIND OF GENERALIST DO WE NEED FOR SUCH A TURBULENT FUTURE?
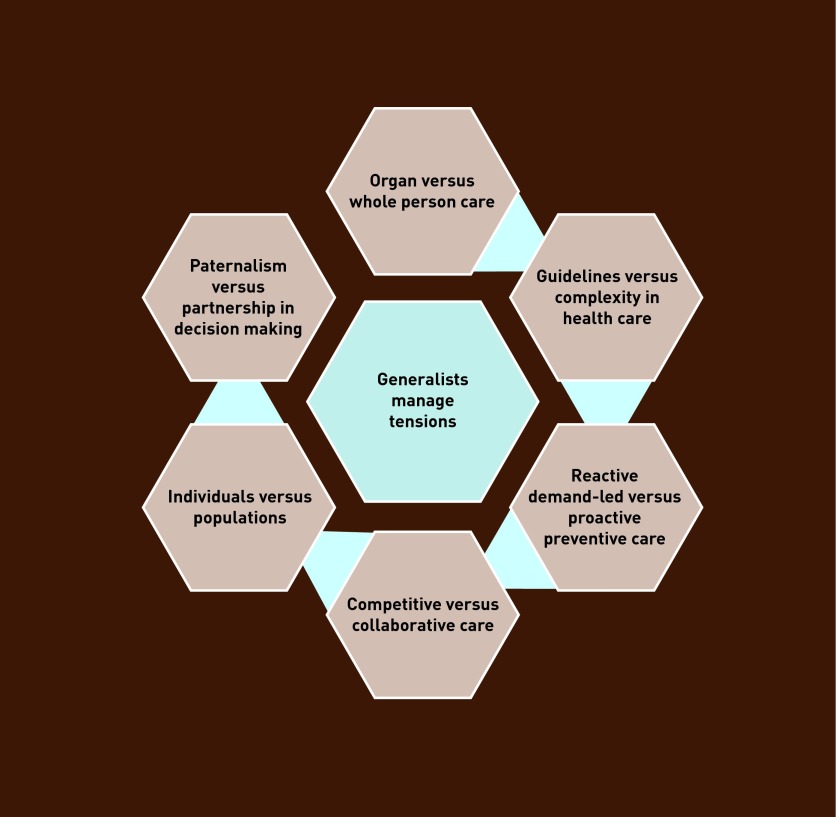
We firmly believe that high quality generalists are the answer to the challenges that face health care in the 21st century. An aspiration to provide whole person care; through the judicious use of investigations and treatments based on best evidence and practice where appropriate; in collaborative partnerships with patients and colleagues; grounded in the context of their relationships and communities is neither new nor controversial to the delivery of high quality generalist care. The unique value of community generalists in being able to tolerate uncertainty, manage tension and ambiguity, support patients in managing anxiety, and apply their well-honed professional judgement is essential for the future viability of our healthcare system (Figure 1).
Figure 1.
Generalists managing tensions.
However, we would argue that there are challenges touched on in the independent commission on generalism3 that warrant further consideration. The present coalition government, in first presenting its ideas on health reform, coined the phrase ‘no decision about me without me’. In doing so, it has set the NHS on a journey that seeks to place patients at the heart of everything it does. However, if we are to move beyond mere rhetoric it will require a profound change to what currently takes place in the consulting room and practices across the country. Patients need the resources, tools, and support to take control of their own health and illness journeys, be empowered to make decisions and take action to manage their own health care. Such a shift requires clinicians to move away from paternalistic attitudes and towards supporting patients in achieving their aims,4 forming partnerships that are a mark of collective responsibility which reach out to humanise the experience of illness for patients.
Community generalists are in a unique position to improve patient outcomes and tackle health inequalities5 through the development of systematic anticipatory care. Our healthcare system has championed the use of the practice list as the fundamental unit against which to make decisions about resource allocation (for example, through the Carr-Hill formula) and determinations about quality of care (as evidenced by the increasing amount of practice-specific information being made publicly available). The practice list offers the opportunity for community generalists to systematically identify population needs, design evidence-based interventions to reverse or ameliorate the ill-effects of risks and diseases, and target these interventions to those at greatest risk.
HOW CAN THE HEALTHCARE SYSTEM SUPPORT THE WORK OF COMMUNITY GENERALISTS?
Patients have better outcomes when seen by specialists for single condition management.6 By contrast, patients with multiple medical issues respond better to clinicians with a more generalist approach. Patients with multimorbid conditions requiring generalist and specialist input currently experience fragmented and chaotic healthcare. The challenge for generalists and specialists therefore, is to collaborate with each other, and offer continuity of care in new and innovative ways. Boundaries between primary and secondary care need to change and the structure of health care needs to shift to team-based patient-centric services, with generalists and specialists who coordinate their actions to move patients from transition across the traditional boundaries of secondary and primary care, as well as from illness to wellness. Continuity of care has long been a central tenet of practising generalists. Doctors and patients value it highly and it is thought to provide the basis for high quality of care.7 Other authors have questioned whether an unswerving loyalty to individual continuity is necessary and sustainable8,9 and we would suggest that individual continuity needs to be targeted to those that need it the most (for example, those with multimorbid or long-term conditions), and for others longitudinal continuity can be provided through team and informational approaches.
Tooke and Darzi1,10 highlight the fundamental role that all community generalists have as guardians of healthcare resources, collectively in their roles as members of local commissioning groups, as well as individually in their work with patients. In these austere times we would argue that a well-developed sense of responsibility towards resource utilisation and engagement with local healthcare systems is critical in ensuring the very viability of our healthcare system into the future. Perhaps more importantly, as Francis11 has suggested, community generalists need to act as advocates for their communities in the face of difficult to change attitudes towards patient-centred services.
IS THE FUTURE WORKFORCE READY AND PREPARED FOR THIS KIND OF FUTURE?
We would suggest that the Royal Colleges consider working together on developing the role of generalists and collaborative working, and embed this within their curricula and assessment strategies. There is a whole system review of postgraduate training being undertaken by the General Medical Council12 to ensure that those in training are fit for a world where patients are at the centre of everything healthcare does. For those beyond specialty training, continuing professional development, with supervision, should help individuals prepare to be fit for purpose.
Current conceptions of the community generalist need to evolve to target individual continuity more effectively; place patients at the heart of all healthcare activity (individual and team-based); challenge and overcome the parochialism of traditional boundaries within health and social care; recognise the role of leadership in managing and utilising resources; and develop systematic approaches to population health management and doctoring. In this way we can begin to talk about a healthcare system fit for the 21st century.
Provenance
Freely submitted; not externally peer reviewed.
REFERENCES
- 1.Darzi A. A high quality workforce: NHS Next Stage Review. London: Department of Health; 2008. http://webarchive.nationalarchives.gov.uk/20130107105354/ http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_085841.pdf (accessed 3 Apr 2013). [Google Scholar]
- 2.Goodwin N, Dixon A, Poole T, Raleigh V. Improving the quality of care in general practice. Report of an independent inquiry commissioned by The King’s Fund. London: King’s Fund; 2011. http://www.kingsfund.org.uk/publications/improving-quality-care-general-practice (accessed 3 Apr 2013). [Google Scholar]
- 3.The Health Foundation Inspiring Improvement . Guiding patients through complexity: modern medical generalism. London: The Health Foundation; 2011. http://www.health.org.uk/publications/generalism-report (accessed 3 Apr 2013). [Google Scholar]
- 4.The Patients Association . Primary care: Patients and GPs — partners in care? London: The Patients Association; 2012. http://patients-association.com/Portals/0/Public/Files/Research%20Publications/Patients%20and%20GP%27s%20-%20Partners%20in%20Care.pdf (accessed 3 Apr 2013). [Google Scholar]
- 5.Hutt P, Gilmour S. Tackling inequalities in general practice. London: The King’s Fund; 2010. http://www.kingsfund.org.uk/sites/files/kf/field/field_document/health-inequalities-general-practice-gp-inquiry-research-paper-mar11.pdf (accessed 3 Apr 2013). [Google Scholar]
- 6.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Millbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray DP, Evans P, Sweeney K, et al. Towards a theory of continuity of care. J R Soc Med. 2003;96(4):160–166. doi: 10.1258/jrsm.96.4.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lipman T. The future general practitioner: out of date and running out of time. Br J Gen Pract. 2000;50(458):743–746. [PMC free article] [PubMed] [Google Scholar]
- 9.Marshall M. Practice, politics, and possibilities. Br J Gen Pract. 2009;59(565):605–612. doi: 10.3399/bjgp09X420266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tooke J. Aspiring to excellence. Final report of the independent inquiry into modernising medical careers. London: MMC Inquiry; 2008. http://www.mmcinquiry.org.uk/MMC_FINAL_REPORT_REVD_4jan.pdf (accessed 3 Apr 2013). [Google Scholar]
- 11.The Mid Staffordshire NHS Foundation Trust Public Inquiry . Chaired by Robert Francis QC. London: The Mid Staffordshire NHS Foundation Trust; 2013. http://www.midstaffspublicinquiry.com/report (accessed 3 Apr 2013). [DOI] [PubMed] [Google Scholar]
- 12.General Medical Council . Shape of training review. London: GMC; 2013. http://www.shapeoftraining.co.uk (accessed 3 Apr 2013). [Google Scholar]