Abstract
Osteoarthritis (OA) is the most frequent cause of disability in the United States, with the medial compartment of the knee being the most commonly affected.1 The initiation and progression of knee OA is influenced by many factors including kinematics. In response to loading during weight bearing, cartilage in healthy knees demonstrates spatial adaptations in morphology and mechanical properties. These adaptations allow certain regions of the cartilage to respond to loading while other regions are less well suited to accommodate loading. Alterations in normal knee kinematics shift loading from those cartilage regions adapted for loading to regions less well suited. This leads to the initiation and progression of degenerative processes consistent with knee OA. Kinematic variables associated with the development, progression and severity of knee OA are the adduction moment (Madd) and tibiofemoral rotation. Due to its strong correlation with disease progression and pain, the peak Madd during gait has been identified as a target for treatment design. Gait modification offers a non-invasive option for seeking significant reductions. Gait modification has the potential to reduce pain and slow the progression of medial compartment knee OA.
Keywords: kinematics, knee, osteoarthritis, gait
Introduction
Osteoarthritis (OA) is condition with a multifaceted etiology and afflicts both load bearing and non-weight bearing joints. The risk of developing OA substantially increases with each decade after the age of 45 years.2 Among reported upper and lower extremity sites, the most common region for OA to manifest is the medial compartment of the knee, and the knee will serve as the model for discussion in this review.1 The initiation and progression of knee OA involves mechanical, structural, genetic and environmental factors. During growth and development, the tibial and femoral cartilage adapt over time to cyclic loading during walking; 3 cartilage remodeling to loading also applies to other joints such as the hip.4 Knee cartilage thickens in the areas of greatest loading in both the anterior-to-posterior and medial-to-lateral regions.3 The tibiofemoral mechanics and loading patterns during walking, therefore, have a significant influence on the regional development of articular cartilage. Disruption of normal gait mechanics with trauma, acute injury, ligamentous laxity, weight gain and improper footwear can shift the loading patterns during weight-bearing to cartilage regions not well adapted to accept those loads. 3, 5–10 Although normal healthy cartilage responds positively to loading and increases regional thickness, diseased or injured cartilage degenerates and decreases regional thickness.3
While there are several potential biomechanical alterations that may contribute to the onset and progression of knee OA, increased internal tibiofemoral rotation and peak knee adduction moment (Madd) during load bearing may be two factors that are of particular interest. The Madd is recognized as a clinically important measure to study medial compartment knee OA,11,12 and is a surrogate for medial contact force,13 disease severity and progression, 14,15 and pain severity. 16 Normal tibiofemoral loading may be altered in knees with either anterior cruciate ligament (ACL) deficiency or OA, and may shift the weight bearing stressors to cartilage regions not previously adapted for load bearing.5 The loading of these non-adapted regions leads to cartilage fibrillation and local degenerative changes.3, 5, 17, 18 Correcting abnormalities of tibiofemoral rotation and/ or decreasing the Madd are clinically relevant for management of OA symptoms and progression.
This review will provide evidence regarding the potential roles of the separate and combined roles of tibiofemoral rotation and the Madd in the development and progression of knee OA. Emerging methods that favorably change these two parameters and thereby OA symptoms will be presented.
Setting the Stage
With normal aging, cartilage breakdown begins in joint areas with little or no contact. As destruction advances, it moves gradually into the more heavily loaded areas. At this point, biomechanical factors such as loading patterns, tibiofemoral contact time and motions about the joint generate shear and frictional stresses.4 Cartilage softens and fibrillates. Aging or injury to the knee joint increases joint laxity and permits excess or aberrant motion about the knee, a process that exacerbates progression of OA.
Tibiofemoral Rotation
The knee joint is commonly thought of as a hinge joint with pure hinge-like motion. However, the anatomical structure of a femoral condyle is similar to a cam. As the femur rotates over the articular surface of the tibia, the motion involves both rotation and anterior-posterior translation. Importantly, cartilage develops with variations in regional thickness as a consequence of the loading occurring during normal gait.3, 5, 17 Thickness maps of cartilage reveal that cartilage regions are thickest at the lateral facet of the tibia and thinnest on the medial facet.19 Alterations in patterns of knee kinematics cause a shift from normal articular contact areas to articular areas that are infrequently loaded. Aberrant loading of these areas causes fibrillation of the collagen network, loss of matrix proteoglycans, increased surface friction, increased shear stress, upregulation of catabolic factors (i.e. matrix metalloproteinases, interleukins, etc) and ultimately cartilage degradation.3, 5, 17 ACL injury, ligament laxity or stiffness, decreased muscle strength, and altered muscle activation patterns can alter normal joint kinematics.3, 5, 17
During knee flexion and extension, the femur and the tibia rotate and translate relative to each other through the range of motion (ROM). During a typical walking gait cycle, the greatest weight-bearing loads occur at or near heel strike and are absorbed by the areas of thickest cartilage development on the tibia and femur.5, 19 Compared to patients with healthy knees, patients with knee OA demonstrate greater femoral internal rotation, decreased tibial posterior translation, and dysfunction with the “screw home maneuver” during extension.20 The normal rotation and translation of the tibia relative to the femur can be altered by such factors as ACL insufficiency or osteophyte formation.20 The ACL provides anteroposterior (AP) as well as rotational stability to the knee. In patients with ACL tears, 60–90% of these knees develop OA within 15 years.21 ACL injury disproportionately affects the medial compartment more than the lateral. Knees with an ACL injury are more likely to develop medial compartment OA and meniscal tears likely due to the disproportionate load distribution in this compartment compared to the lateral compartment.3, 5, 19, 21 ACL deficiency provides a framework for understanding how alterations in knee kinematics can lead to degenerative changes in knee cartilage. 3, 5, 19, 21,5, 19 In ACL deficient knees, the tibia remained internally rotated throughout the stance phase and the end of the swing phase compared to the control limb.5, 19 This offset led to loading of cartilage regions not typically loaded prior to the ACL injury. Interestingly, ACL reconstruction has been shown to restore normal AP stability, but does not consistently restore normal rotational alignment or motion.5, 19 Since knees that have undergone ACL reconstruction have a higher incidence of knee OA compared to non-injured knees, these data suggest that alterations in knee rotation influence the development and progression of knee OA.5, 19
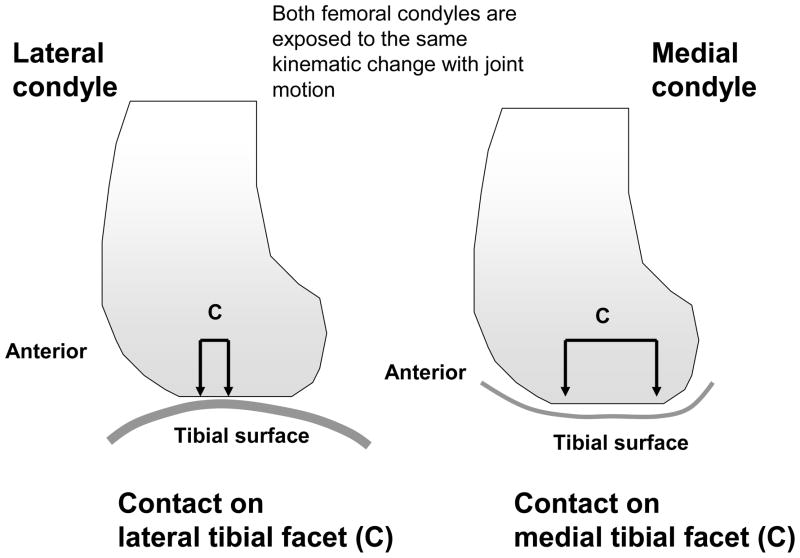
This shift in articular contact to the medial tibial facet can be problematic. While the lateral and medial femoral condyles are both shaped like cams, the two tibial surfaces with these condyles make contact are shaped differently (Figure 1). Andriacchi et al. proposed that when exposed to the same joint displacement with any kinematic change, the medial femoral condyle will experience increased contact with the concave tibial surface with lower cartilage thickness than the lateral condyle that will experience less contact with the convex tibial facet with relatively thick cartilage.19 Over time, the repeated daily loading with an increase in internal rotation will adversely wear the areas of thinnest cartilage first, causing initial cartilage breakdown. Continued exposures of the vulnerable thinner cartilage to greater internal rotation will advance cartilage wear and induce symptomatic OA. Changes in tibiofemoral rotation that contribute to OA, therefore, are complex and include the degree of internal rotation, location of rotation and amount of contact exposure on the medial compartment.
Figure 1.
A comparison of the tibiofemoral contact on the lateral and medial joint compartments (lateral view). When exposed to the same kinematic change during motion, the medial femoral condyle experiences greater contact with the medial tibial facet relative to the lateral joint compartment.
Peak Knee Adduction Moment (Madd)
The Madd describes the load distribution across the medial and lateral tibial plateaus.5 During normal ambulation in healthy knees, the medial compartment experiences 60–80% of the weight-bearing load. 21 Conceptually, the Madd can be considered the “closing force” on the medial knee compartment during gait. 22 Radiographic imaging routinely shows that joint space narrowing is present to a greater extent in the medial compartment compared to the lateral compartment. Knee malalignment that places the joint into a varus position can increase loading on the medial side of the joint. Static alignment alone does not predict incidence of OA.23 However, degeneration of the joint during progression of OA can cause an increase in varus malalignment.24 During dynamic movements medial joint loading can be estimated by measuring the Madd. The Madd is produced when the foot is in contact with the ground and the line of action of the force vector passes medial to the knee joint. An increased distance between the force vector and the knee joint will result in a higher Madd and greater loading on the medial joint. Varus alignment will cause the knee joint to move laterally relative to the position of the foot on the ground, which increases the Madd. On the contrary, shifting the position of the trunk laterally can move the line of action of the ground reaction force more medial, which can decrease the Madd moment.25 Increasing the Madd has been associated with the progression and possibly the initiation on knee OA. 3, 5, 7–9, 26 Further, the Madd during walking predicts of OA severity, progression, and clinical outcomes in patients with medial compartment knee OA. 3, 26 In patients with mild OA, medial compartment loading can distinguish between those who are symptomatic and those that are asymptomatic.16 Interestingly, in healthy persons, the medial/lateral cartilage thickness ratio is highest in those who demonstrate the highest Madd. In persons with OA, however, the cartilage is thinnest in persons with the highest Madd.4
Increasing gait speed increases the ground reaction force, and net joint forces and moments experienced at the joint level. Individuals with OA walk more slowly compared to asymptomatic controls, which presents a confounding factor when interpreting studies where subjects walked at a self-selected speed. In most studies,27, 28 with the exception of Zeni and Higginson,29 the changes in Madd are not completely explained by gait speed and seem to indicate that some fundamental gait adaptation has occurred to attempt to unload the medial compartment of the knee.
Modifying the Peak Knee Adduction Moment
Foot Wear and Assistive Devices
At least seven assisted gait modifications can reduce the peak Madd, including the use of lateral wedge insoles, 30, 31 lateral wedge insoles combined with subtalar strapping, 32 variable stiffness shoes with softer medial sides, 33 or high mobility shoes (that act similarly to natural foot flexibility),34 valgus knee braces that use three point bending, 35, 36 canes,37 and hiking poles to offset the Madd generated by the opposite knee.38 The most effective assistive gait modification methods for reducing Madd include variable stiffness shoes, lateral wedge insoles with the addition of subtalar strapping, or bilateral hiking poles. The ultimate goal of reducing the peak knee adduction moment is to reduce peak medial contact force during stance phase. For gait tests performed to date, variable stiffness shoes and valgus knee braces have produced the largest reductions in medial contact force.
Though walking with knees medialized and with hiking poles reduced the first and largest peak of medial contact force by only a small amount, these gait modification methods reduced medial contact force significantly over the rest of stance phase 39. Furthermore, elimination of excessive knee flexion during mid stance may make these two methods effective at reducing the first peak as well 39. The peak medial contact force reduction of 23% achieved by valgus knee braces should be viewed in light of the significant discomfort experienced by the subjects for this brace setting.
While these collective data do not show a causative effect of the Madd on the development of knee OA, strategies to modify the biomechanical mechanisms involved in symptomatic knee OA were obtained.
Gait Modification
While high tibial osteotomy surgery can significantly reduce the peak Madd40, gait modification may be a non-invasive alternative. The best outcome of gait modification would be to reduce the peak Madd similar to that achieved after a high tibial osteotomy surgery. A number of studies have evaluated the ability of these different gait modification methods to reduce the peak Madd. Gait modifications that can reduce the peak Madd include walking with decreased speed 41, 42 widening base the base of support at stance, 43 pointing toes outward 12, 44, 45 medializing the knees, 39, 46, 47 and increasing the magnitude of medial-lateral trunk sway.48, 49 Of these methods, walking with knees medialized and a medial-lateral trunk sway have produced Madd reductions exceeding 10% and on the order of those achieved by high tibial osteotomy surgery.
Considerations in Data Interpretation
There are several important considerations when interpreting data from gait modification research. First, when a patient’s gait pattern is changed, a decrease in peak Madd does not guarantee a decrease in peak medial contact force. For example, in a study that explored the effectiveness of walking with knees medializing or hiking poles on peak Madd39 both modifications produced little change in peak medial contact force, despite significant reductions in the peak Madd. Second, beneficial changes at the knee could induce detrimental changes at other joints 50. Such changes are most likely to occur at the ankle or the lower back, where load changes are the largest depending on the gait modification. Because ankle OA induced by lateral heel wedges has not been reported, it is unlikely that gait modifications that alter ankle loads will be detrimental. Third, different Madd calculation methods yield different interpretations of the effectiveness of a particular gait modification 51. Many studies do not provide details of how the peak Madd was calculated, making it difficult to compare results from different studies. Furthermore, several studies have suggested that the knee adduction angular impulse, which is the area under the knee adduction moment curve during stance phase, may be a better clinical target than Madd 16, 52, 53.
Applications in Physical Medicine and Rehabilitation
The concepts relating to OA and altered biomechanical parameters between two articular surfaces might be applied to joint degeneration in other joints or in medical conditions such as the following:
Knee OA Onset After Lower Extremity Amputation
Among lower extremity rehabilitating populations, those with transtibial amputations demonstrate biomechanical alterations that contribute to OA onset in the intact limb. Some prosthetic foot characteristics significantly affect the MAdd of the intact knee during gait.54 For example, prosthetic feet that generate low foot-ankle push-off appear to be associated with higher intact knee MAdd, and their use may increase the risk and burden of knee OA in this population.54
Hip OA
In hip OA, initial cartilage degeneration occurs in the fovea below the femoral head and medial/ lateral areas of the femoral head - areas with low exposure to little loading or minimal contact. Once this occurs, the contact area and motion increase frictional shear stress that facilitate OA onset.4 Also, the atypical cam shaped femoral head may alter joint motion and articular contact area with the acetabulum compared to a normal, round femoral head. Over time, the repetitive stressors with average weight-bearing activity can exacerbate frictional stress within the hip joint, causing premature cartilage breakdown and OA.
Hip OA onset might be related in part to participation in high performance competitive sport such as javelin and high jump. These sport motions induce high moments with high velocity rotation within the hip. Cross sectional data of these athletes 10 years after retirement from their sport revealed that the odds risk of developing OA was 6.1 in javelin throwers compared to controls.55
Overloaded Upper Extremity Joints and OA
In patients with spinal cord injury, the mechanical loading of upper limb joints is significantly altered compared to pre-injury. Signs and symptoms of mechanical overuse appear over time and can manifest as secondary arthritis. Maximal cartilage thickness can decrease as much as 8% at one year after the injury.56 The increased use of the shoulder joint through an arc of resistance during wheelchair propulsion and through body transfers places high forces in the shoulder on articular surfaces for which they were not designed.57 This high contact stress and distribution of the stress in patients with paraplegia were related to chronic joint pain and other impingement syndromes.
While prospective data are sparse for elbow OA, the prevalence of the condition is heaviest in heavy manual laborers, weight lifters and throwing athletes.58 All these populations share common exposure of the elbow joint to high forces during rotation.
Foot and Ankle OA
Biomechanical alterations to joint motion and force are also evident in the ankle and foot in dancers. The foot and ankle are vulnerable to repetitive microtrauma during dance. The prevalence of joint degeneration was found to be higher in a group of retired professional ballet dancers compared with controls.59 This might be explained in part by the stressors placed on the metatarsophalangeal and ankle joints compared with normal loading patterns. These joints support large forces, sometimes in excess of 20 kg/cm. Furthermore, these joints are rotated into positions in the extreme ranges of motion and this causes a valgus deformity.59 Over time, the repeated trauma with practice and performing narrows the metatarsophalangeal joint space and increases prevalence of arthritis.
Conclusions
Knee kinematics play an important role in the development and degradation of articular cartilage. Healthy cartilage responds to loading by adapting its morphology and mechanical characteristics in the areas of greatest stress. However, once normal joint kinematics are altered, loading shifts to areas which are not well suited to accommodate the increased stress. Once the OA cycle has been initiated, the loading that once facilitated cartilage adaption, now serves to facilitate the progression of cartilage degradation.5, 19 Strategies, both surgical and non-surgical, which serve to re-establish normal joint kinematics have been shown to be effective in decreasing pain and functional impairments, and possibly slow progression. By changing pathological joint mechanics, gait modification may have disease modifying potential for medial compartment knee OA, at least in terms of slowing progression of the disease.
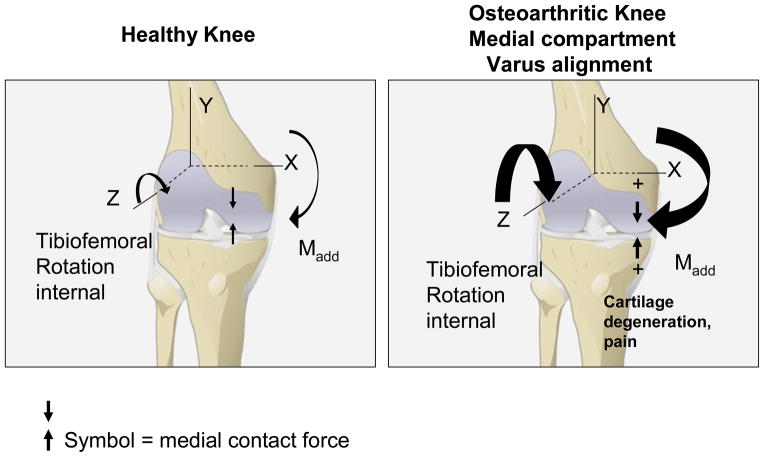
Figure 2.
Summary of the knee adduction moment (Madd) and internal tibiofemoral rotation about the knee during loading in ambulation in healthy knees and knees with medial OA (frontal view). Forces and rotation are shown relative to the X,Y,Z coordinate system. The thicker the arrows, the greater the forces or rotation. Higher Madd and internal rotation increase medial contact force; over time, the cartilage degenerates and OA develops and progresses.
Acknowledgments
Drs. Kevin and Heather Vincent were funded in part by NIH National Institute of Musculoskeletal and Skin Diseases (grants R03 AR057552-01A1, AR059786); Dr. Fregly wishes to thank the National Institutes of Health (NIH) National Center for Medical Rehabilitation Research (grant R21 HD053490) and the Hospital for Special Surgery for supporting this work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wise BL, Niu J, Yang M, et al. Patterns of compartment involvement in tibiofemoral osteoarthritis in men and women and in Caucasians and African Americans: The Multicenter Osteoarthritis Study. Arthritis Care & Research. :n/a–n/a. doi: 10.1002/acr.21606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis & Rheumatism. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andriacchi TP, Koo S, Scanlan SF. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J Bone Joint Surg Am. 2009 Feb;91( Suppl 1):95–101. doi: 10.2106/JBJS.H.01408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carter DR, Beaupre GS, Wong M, Smith RL, Andriacchi TP, Schurman DJ. The mechanobiology of articular cartilage development and degeneration. Clin Orthop Relat Res. 2004 Oct;427(Suppl):S69–77. doi: 10.1097/01.blo.0000144970.05107.7e. [DOI] [PubMed] [Google Scholar]
- 5.Andriacchi T, Mundermann A, Smith R, Alexander E, Dyrby C, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Annals of Biomedical Engineering. 2004;32(3) doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 6.Kerrigan D, Lelas J, Goggins J, Merriman G, Kaplan R, Felson D. Effectiveness of a lateral-wedge insole on knee varus torque in patients with knee osteoarthritis. Archives of Physical Medicine and Rehabilitation. 2002;83:889– 893. doi: 10.1053/apmr.2002.33225. [DOI] [PubMed] [Google Scholar]
- 7.Kerrigan DC, Johansson JL, Bryant MG, Boxer JA, Della Croce U, Riley PO. Moderate-heeled shoes and knee joint torques relevant to the development and progression of knee osteoarthritis. Arch Phys Med Rehabil. 2005 May;86(5):871–875. doi: 10.1016/j.apmr.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 8.Kerrigan DC, Karvosky ME, Lelas JL, Riley PO. Men’s shoes and knee joint torques relevant to the development and progression of knee osteoarthritis. J Rheumatol. 2003 Mar;30(3):529–533. [PubMed] [Google Scholar]
- 9.Kerrigan DC, Lelas JL, Karvosky ME. Women’s shoes and knee osteoarthritis. Lancet. 2001 Apr 7;357(9262):1097–1098. doi: 10.1016/S0140-6736(00)04312-9. [DOI] [PubMed] [Google Scholar]
- 10.Kerrigan DC, Todd MK, Riley PO. Knee osteoarthritis and high-heeled shoes. Lancet. 1998 May 9;351(9113):1399–1401. doi: 10.1016/S0140-6736(97)11281-8. [DOI] [PubMed] [Google Scholar]
- 11.Cheng Y, Hootman J, Murphy L, Langmaid G, Helmick C. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation — United States, 2007–2009. CDC Morbidity and Mortality Weekly Report. 2010;59(39):1261–1265. [PubMed] [Google Scholar]
- 12.Andriacchi TP. Dynamics of knee malalignment. Orthopedic Clinics of North America. 1994 Jul;25(3):395–403. [PubMed] [Google Scholar]
- 13.Zhao D, Banks SA, Mitchell KH, D’Lima DD, Colwell CW, Fregly BJ. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. Journal of Orthopaedic Research. 2007;25:789–797. doi: 10.1002/jor.20379. [DOI] [PubMed] [Google Scholar]
- 14.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Annals of the Rheumatic Diseases. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma L, Hurwitz DE, Thonar EJ-MA, et al. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis & Rheumatism. 1998;41:1233–1240. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 16.Thorp LE, Sumner DR, Wimmer MA, Block JA. Relationship between pain and medial knee joint loading in mild radiographic knee osteoarthritis. Arthritis & Rheumatism. 2007 Oct 15;57(7):1254–1260. doi: 10.1002/art.22991. [DOI] [PubMed] [Google Scholar]
- 17.Andriacchi T, Mundermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Current Opinion in Rheumatology. 2006;18:514– 518. doi: 10.1097/01.bor.0000240365.16842.4e. [DOI] [PubMed] [Google Scholar]
- 18.Chaudhari AM, Briant PL, Bevill SL, Koo S, Andriacchi TP. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc. 2008 Feb;40(2):215–222. doi: 10.1249/mss.0b013e31815cbb0e. [DOI] [PubMed] [Google Scholar]
- 19.Andriacchi TP, Briant PL, Bevill SL, Koo S. Rotational changes at the knee after ACL injury cause cartilage thinning. Clin Orthop Relat Res. 2006 Jan;442:39–44. doi: 10.1097/01.blo.0000197079.26600.09. [DOI] [PubMed] [Google Scholar]
- 20.Hamai S, Moro-oka TA, Miura H, et al. Knee kinematics in medial osteoarthritis during in vivo weight-bearing activities. J Orthop Res. 2009 Dec;27(12):1555–1561. doi: 10.1002/jor.20928. [DOI] [PubMed] [Google Scholar]
- 21.Dayal N, Chang A, Dunlop D, et al. The natural history of anteroposterior laxity and its role in knee osteoarthritis progression. Arthritis Rheum. 2005 Aug;52(8):2343–2349. doi: 10.1002/art.21277. [DOI] [PubMed] [Google Scholar]
- 22.Sharma L. The role of proprioceptive deficits, ligamentous laxity, and malalignment in development and progression of knee osteoarthritis. J Rheumatol Suppl. 2004 Apr;70:87–92. [PubMed] [Google Scholar]
- 23.Hunter DJ, Niu J, Felson DT, et al. Knee alignment does not predict incident osteoarthritis: The Framingham Osteoarthritis Study. Arthritis & Rheumatism. 2007;56(4):1212–1218. doi: 10.1002/art.22508. [DOI] [PubMed] [Google Scholar]
- 24.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 25.Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005 Sep;52(9):2835–2844. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- 26.Sharma L, Song J, Dunlop D, et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. Nov;69(11):1940–1945. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mundermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: reduced walking speed. Arthritis Rheum. 2004 Apr;50(4):1172–1178. doi: 10.1002/art.20132. [DOI] [PubMed] [Google Scholar]
- 28.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. Journal of Orthopaedic Research. 2008;26(3):332–341. doi: 10.1002/jor.20496. [DOI] [PubMed] [Google Scholar]
- 29.Zeni JAJ, Higginson JS. Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis: a result of altered walking speed? Clinical Biomechanics (Bristol, Avon) 2009;24(4):372–378. doi: 10.1016/j.clinbiomech.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kakihana W, Akai M, Nakazawa K, Takashima T, Naito K, Torii S. Effects of laterally wedged insoles on knee and subtalar joint moments. Archives of Physical Medicine and Rehabilitation. 2005;86:1465–1471. doi: 10.1016/j.apmr.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 31.Butler RJ, Marchesi S, Royer T, Davis IS. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. Journal of Orthopaedic Research. 2007;25:1121–1127. doi: 10.1002/jor.20423. [DOI] [PubMed] [Google Scholar]
- 32.Kuroyanagi Y, Nagura T, Matsumoto H, et al. The lateral wedged insole with subtalar strapping significantly reduces dynamic knee load in the medial compartment gait analysis on patients with medial knee osteoarthritis. Osteoarthritis and Cartilage. 2007 Aug;15(8):932–936. doi: 10.1016/j.joca.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 33.Erhart JC, Mundermann A, Elspas B, Giori NJ, Andriacchi TP. A variable-stiffness shoe lowers the knee adduction moment in subjects with symptoms of medial compartment knee osteoarthritis. Journal of Biomechanics. 2008 Aug 28;41(12):2720–2725. doi: 10.1016/j.jbiomech.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 34.Shakoor N, Lidtke RH, Sengupta M, Fogg LF, Block JA. Effects of specialized footwear on joint loads in osteoarthritis of the knee. Arthritis & Rheumatism. 2008 Sep 15;59(9):1214–1220. doi: 10.1002/art.24017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lindenfeld TN, Hewett TE, Andriacchi TP. Joint loading with valgus bracing in patients with varus gonarthrosis. Clinical Orthopaedics and Related Research. 1997 Nov;344:290–297. [PubMed] [Google Scholar]
- 36.Draganich L, Reider B, Rimington T, Piotrowski G, Mallik K, Nasson S. The effectiveness of self-adjustable custom and off-the-shelf bracing in the treatment of varus gonarthrosis. Journal of Bone and Joint Surgery (American) 2006 Dec;88(12):2645–2652. doi: 10.2106/JBJS.D.02787. [DOI] [PubMed] [Google Scholar]
- 37.Kemp G, Crossley KM, Wrigley TV, Metcalf BR, Hinman RS. Reducing joint loading in medial knee osteoarthritis: shoes and canes. Arthritis & Rheumatism. 2008 May 15;59(5):609–614. doi: 10.1002/art.23578. [DOI] [PubMed] [Google Scholar]
- 38.Fregly BJ, D’Lima DD, Colwell CW. Effective gait patterns for offloading the medial compartment of the knee. Journal of Orthopaedic Research. 2009;27:1016–1021. doi: 10.1002/jor.20843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walter JP, D’Lima DD, Colwell CW, Fregly BJ. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. Journal of Orthopaedic Research. 2010;28(10):1348–1354. doi: 10.1002/jor.21142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wada M, Imura S, Nagatani K, Baba H, Shimada S, Sasaki S. Relationship between gait and clinical results after high tibial osteotomy. Clinical Orthopaedics and Related Research. 1998;354:180–188. doi: 10.1097/00003086-199809000-00022. [DOI] [PubMed] [Google Scholar]
- 41.Mündermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity. Arthritis & Rheumatism. 2004;50:1172–1178. doi: 10.1002/art.20132. [DOI] [PubMed] [Google Scholar]
- 42.Robbins SM, Maly MR. The effect of gait speed on the knee adduction moment depends on waveform summary measures. Gait & Posture. 2009 Nov;30(4):543–546. doi: 10.1016/j.gaitpost.2009.08.236. [DOI] [PubMed] [Google Scholar]
- 43.Fregly BJ, Reinbolt JA, Chmielewski TL. Evaluation of a patient-specific cost function to predict the influence of foot path on the knee adduction torque during gait. Computer Methods in Biomechanics and Biomedical Engineering. 2008;11:63–71. doi: 10.1080/10255840701552036. [DOI] [PubMed] [Google Scholar]
- 44.Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. Journal of Orthopaedic Research. 2002;20:101–107. doi: 10.1016/S0736-0266(01)00081-X. [DOI] [PubMed] [Google Scholar]
- 45.Guo M, Axe MJ, Manal K. The Influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis. Gait and Posture. 2007;26:436–441. doi: 10.1016/j.gaitpost.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 46.Fregly BJ, Reinbolt JA, Rooney KL, Mitchell KH, Chmielewski TL. Design of patient-specific gait modifications for knee osteoarthritis rehabilitation. IEEE Transactions on Biomedical Engineering. 2007;54:1687–1695. doi: 10.1109/TBME.2007.891934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barrios JA, Crossley KM, Davis IS. Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment. Journal of Biomechanics. 2010 Aug 10;43(11):2208–2213. doi: 10.1016/j.jbiomech.2010.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hunt MA, Birmingham TB, Bryant D, et al. Lateral trunk lean explains variation in dynamic knee joint load in patients with medial compartment knee osteoarthritis. Osteoarthritis and Cartilage. May. 2008;16(5):591–599. doi: 10.1016/j.joca.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 49.Mündermann A, Asay JL, Mündermann L, Andriacchi TP. Implications of increased medio-lateral trunk sway for ambulatory mechanics. Journal of Biomechanics. 2008;41:165–170. doi: 10.1016/j.jbiomech.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 50.Toriyama M, Deie M, Shimada N, et al. Effects of unloading bracing on knee and hip joints for patients with medial compartment knee osteoarthritis. Clinical Biomechanics. 2011 Jun;26(5):497–503. doi: 10.1016/j.clinbiomech.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 51.Schache AG, Fregly BJ, Crossley KM, Hinman RS, Pandy MG. The effect of gait modification on the external knee adductor moment is reference frame dependent. Clinical Biomechanics. 2008;23:601–608. doi: 10.1016/j.clinbiomech.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 52.Creaby MW, Wang Y, Bennell KL, et al. Dynamic knee loading is related to cartilage defects and tibial plateau bone area in medial knee osteoarthritis. Osteoarthritis and Cartilage. 2010 Nov;18(11):1380–1385. doi: 10.1016/j.joca.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 53.Thorp LE, Sumner DR, Block JA, Moisio KC, Shott S, Wimmer MA. Knee joint loading differs in individuals with mild compared with moderate medial knee osteoarthritis. Arthritis and Rheumatism. 2006 Dec;54(12):3842–3849. doi: 10.1002/art.22247. [DOI] [PubMed] [Google Scholar]
- 54.Morgenroth DC, Segal AD, Zelik KE, et al. The effect of prosthetic foot push-off on mechanical loading associated with knee osteoarthritis in lower extremity amputees. Gait & Posture. 2011;34(4):502–507. doi: 10.1016/j.gaitpost.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schmitt H, Brocai DR, Lukoschek M. High prevalence of hip arthrosis in former elite javelin throwers and high jumpers: 41 athletes examined more than 10 years after retirement from competitive sports. Acta Orthopedics Scandinavica. 2004;75(1):34–39. doi: 10.1080/00016470410001708060. [DOI] [PubMed] [Google Scholar]
- 56.Vanwanseele B, Eckstein F, Hadwighorst H, Knecht H, Spaepen A, Stüssi E. In vivo precision of quantitative shoulder cartilage measurements, and changes after spinal cord injury. Magnetic Resonance Imaging. 2004;51(5):1026–1030. doi: 10.1002/mrm.20068. [DOI] [PubMed] [Google Scholar]
- 57.Bayley JC, Cochran TP, Sledge CB. The weight-bearing shoulder. The impingement syndrome in paraplegics. Journal of Bone and Joint Surgery (American) 1987;69(5):676–678. [PubMed] [Google Scholar]
- 58.Cheung EV, Adams R, Morrey BF. Primary osteoarthritis of the elbow: current treatment options. Journal of the American Academy of Orthopaedic Surgeons. 2008;16(2):77–87. doi: 10.5435/00124635-200802000-00005. [DOI] [PubMed] [Google Scholar]
- 59.van Dijk CN, Lim LS, Poortman A, Strübbe EH, Marti RK. Degenerative joint disease in female ballet dancers. American Journal of Sports Medicine. 1995;23(3):295–300. doi: 10.1177/036354659502300307. [DOI] [PubMed] [Google Scholar]