Abstract
Osteoblastoma is a benign neoplasm which commonly occurs in the vertebral column and long bones. The tumour grows slowly and rarely recurs after surgery. This report presents the clinicopathological and radiological findings of a case of recurrent osteoblastoma in the maxilla. A 7-year-old male patient visited our department with chief complaints of left facial swelling and pain. A panoramic radiograph showed a homogeneous radio-opaque expansile lesion in the left maxilla. The lesion was thought to be fibrous dysplasia and the patient underwent a surgical excision using the Caldwell–Luc procedure. Histopathological examination of the lesion confirmed it as benign osteoblastoma. The lesion recurred 6 months after the initial surgery. CT images revealed a large mass with multiple internal calcifications. Subsequently, the patient underwent mass excision with subtotal left maxillectomy. Follow-up CT scans at 1 year intervals showed no recurrence for 5 years.
Keywords: osteoblastoma, recurrence, X-ray computed tomography
Case report
A 7-year-old male patient visited our department with the chief complaints of left facial swelling and pain. His medical history was unremarkable. Clinical and radiographic examinations were performed. Intraoral examination revealed a firm gingivobuccal swelling extending from the left maxillary deciduous lateral incisor to the left maxillary permanent first molar. Panoramic radiographs showed a homogeneous radio-opaque expansile lesion in the left maxilla and the lesion involved the whole maxilla. The adjacent tooth germs were displaced and the innominate line in the left maxillary sinus was not detected (Figure 1). The lesion was thought to be fibrous dysplasia from the initial clinical and panoramic radiographic findings; therefore, mass excision using the Caldwell–Luc operation was performed. The surgical specimen was 3.5 cm in diameter and it was spherical, encapsulated and firm tissue. On histopathological examination, bony trabeculae surrounded by a single layer of plump osteoblasts of high cellularity were observed in the stroma. There was no atypia or mitotic activity in the osteoblasts or in the mesenchymal cells of the stroma. Most of the calcifications consisted of woven bone without obvious lamellation. Multinuclear giant cells were often identified around the osteoid. As the trabeculation progressed, the stroma changed into loose fibrovascular tissue. The lesion was finally diagnosed as benign osteoblastoma (Figure 2).
Figure 1.
Initial panoramic radiograph shows a homogenously radio-opaque expansile lesion in the left maxilla
Figure 2.
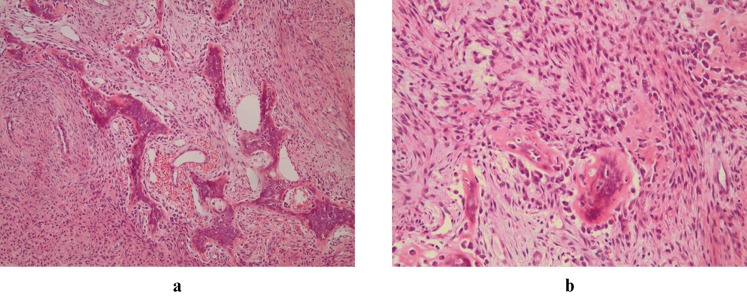
(a) Bony trabeculae are composed of woven bone, arranged in a fibrovascular stroma, and rimmed by a single layer of osteoblasts (haematoxylin and eosin stain, original magnification × 100). (b) The cytomorphology of osteoblasts are typical; they are polygonal, with moderate cytoplasm and round nuclei. There is no atypical or bizarre cell (haematoxylin and eosin stain, original magnification × 200)
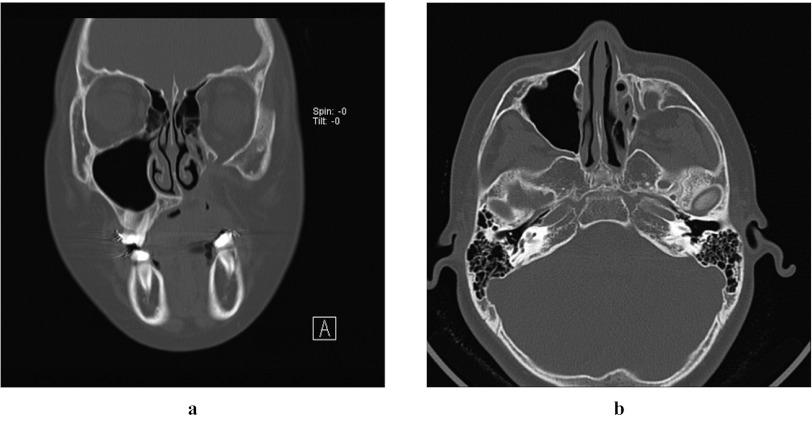
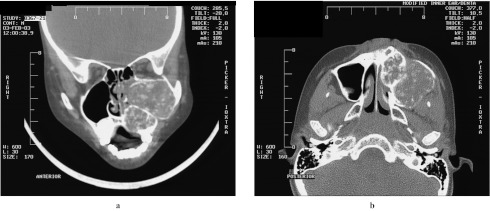
The patient revisited our department with an enlarged swelling in the same region 6 months after the operation. CT images revealed a large well-defined mass composed of two locules with multiple internal calcifications. Owing to the expansive nature of the lesion, the left orbital floor was elevated and the lateral wall of the left nasal cavity was pushed towards the medial side (Figure 3). The patient had undergone mass excision with subtotal left maxillectomy. The surgical specimens were composed of two, solid, firm soft-tissue masses 2.5 × 2.0 × 1.5 cm and 3.0 × 3.0 × 1.5 cm, respectively. Both of them were covered with a thin fibrous capsule and the sections showed marbling of yellow and grey dense soft tissue. The histopathological findings were identical to those of the previous lesion (Figure 4). Follow-up CT scans were performed at 1 year intervals; however, no recurrence was observed over a period of 5 years (Figure 5).
Figure 3.
(a) Coronal and (b) axial CT images taken 6 months after the first operation, showing large an expansile mass with two locules and multiple internal calcifications
Figure 4.
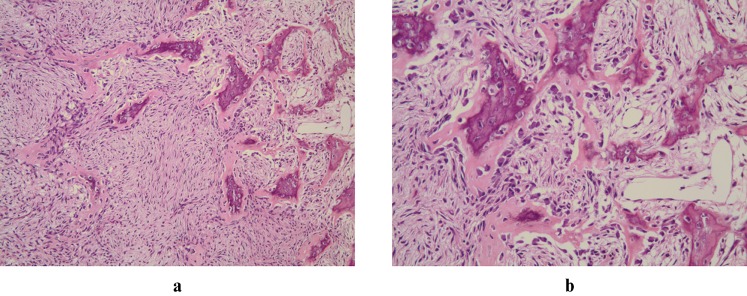
(a) The recurred lesion looks similar to the previous one except that the stroma is more fibrous (haematoxylin and eosin stain, original magnification × 100). (b) Bland osteoblasts surround bony trabeculae. No cellular pleomorphism is observed (haematoxylin and eosin stain, original magnification × 200)
Figure 5.
(a) Coronal and (b) axial CT images taken 5 years following the excision of the mass showing no signs of recurrence in left maxilla
Discussion
Osteoblastoma, which accounts for less than 1% of all tumours of bone, commonly occurs in children and young adults, with a peak incidence in the first three decades of life. The tumour has a definite predilection for males. Although osteoblastoma can involve any bone of the skeleton, the long tubular bones are the most commonly affected (26–36% of cases) followed by the spinal column (21–33% of cases). In approximately 10% of cases, this tumour has been found in the maxillofacial skeleton with a greater frequency occurring in the mandible.1,2 Jones et al3 reviewed 77 cases of osteoblastoma of the jaws, including their 24 cases. Out of these cases, 22 (28.6%) were from the maxilla. Most of these tumours (70.1%) affected the posterior region of the jaws. Osteoblastoma shows a variety of signs, symptoms and radiographic appearances. Pain, often mild and longstanding, is the most consistent symptom. Patients usually present with a localized swelling, tenderness and warmth in the region of the tumour. The tumour usually grows slowly and rarely shows aggressive behaviour. On very rare occasions, however, these tumours may demonstrate progressive growth, local recurrence and, less frequently, malignant transformation.1–6
Although the first case of benign osteobalstoma of the maxilla was reported back in 1967,7 unfortunately most of the reported cases lacked a comprehensive description of the imaging findings. Previous studies reported3,4,7–15 that generally the lesion had well-defined borders and might have a completely radiolucent appearance, or it might show radiolucencies and radio-opacities. Some lesions had large, discrete areas of organized density, and others had a mixed osseous and fibrous appearance.
Osteoblastomas of the maxilla3,16–19 may show atypical radiographic findings. Jones et al3 reported a case of osteoblastoma in the maxilla which demonstrated ground-glass opacification on plain radiographs and was difficult to differentiate from fibro-osseous lesions. The first impression of the present case was also of fibrous dysplasia, because the panoramic radiograph showed the typical features of fibrous dysplasia such as bony expansion and sinus opacification with ground glass appearance. Therefore, further examinations such as CT or bone biopsy were not performed even though the patient had pain in the region.
The recurrent lesion contained multiple internal calcifications which were clearly found on the follow-up CT scans. Similar findings were described by Guest and Juniper,19 who reported a 26-year-old male with left facial pain and marked limitation of mouth opening. The patient's panoramic radiograph showed abnormal calcification on the region of the left pterygoid plate. CT scans revealed a globular mass in the left lateral pterygoid plate with a speckled pattern of calcification within the lesion and sclerosis of the adjacent bone. Kroon and Schurmans20 reported CT findings of osteoblastomas. They described that CT was superior to plain radiography in defining the extent of the lesion, the precise origin of the tumour and the presence of mineralization, and also in demonstrating a peripheral bony shell. These observations were similar to the findings of the present case. In our case, CT was also useful in planning the surgical strategy as well as in monitoring the recurrence.
The tumour, in this case, recurred within 6 months after the initial surgery and showed rapid and extensive growth. Jackson21 reviewed 181 cases of osteoblastoma involving all the sites of the body. Among them, 18 cases (9.8%) recurred. The incidence of recurrence is even rarer in the jaws. According to Alvares Capelozza et al,22 the recurrence rate observed among 69 cases of osteoblastoma of the jaws was 7.2%, with 40% of the cases affecting the maxilla and 60% the mandible. Radiographically, the borders of the lesion were well defined in 80% of the recurrent lesions. Two lesions featured a mixed aspect (40%), two were radio-opaque (40%) and one of them was radiolucent.
According to Dorfman and Weiss,23 some osteoblastomas might show rather aggressive clinical behaviour. They termed these tumours as “aggressive osteoblastoma”. They described them as borderline tumours between osteoblastoma and osteosarcoma, usually larger than conventional osteoblastoma, and with a tendency to local invasion and recurrence. In addition, they reported that these tumours were characterized by the presence of epitheloid osteoblasts. Lypka et al24 reported a large mixed lesion in the mandible. As an expansile lesion contained larger spaces filled with sheets of epitheloid osteoblasts, it was diagnosed as aggressive osteoblastoma.
However, It has been reported that the histopathological features alone were not reliable predictors of aggressive behaviour.1,14 Even though our case exhibited aggressive growth of the recurrent lesion, there was no epitheloid osteoblast and cellular atypia in the second surgical specimen on histopathological examination. Ataoglu et al5 and Colm et al6 made similar observations in a case of recurrent osteoblastoma of the mandible.
It is important to differentiate between the aggressive osteoblastoma and the conventional osteoblastoma, as the former tumour shows a greater likelihood of recurrence. According to Gordon et al,15 the probability of recurrence for conventional osteoblastoma was 13.6%, while for aggressive osteoblastoma it was 50%. Ohkubo et al14 stated that aggressive osteoblastoma revealed the higher tendency of recurrence due to the insufficient surgical removal of the tumour mass during the initial treatment. However, Unni et al1 reported that osteoblastoma should not be designated as “aggressive” based on the local recurrence solely. Others reported that the aggressive behaviour in osteoblastoma was multifactorial.5 Tumour location and complete removal with wide safety margins are important clinical factors. In the present case, the initial misdiagnosis of the lesion prompted the surgeon to go for a rather conservative approach. Not only did the surgery not remove the tumour tissue completely but also, somehow, the procedure might have induced the proliferation of the biologically active tumour cells, which, in turn, resulted in recurrence within such a short period. In addition, it should be noted that most of the anatomical structures in the head and neck region are complicated, and these masses are often situated in the vicinity of the neuraxis; therefore, complete surgical removal of these tumours might be difficult in some cases.
In conclusion, clinicopathological and radiographic findings of a case of recurrent osteoblastoma have been presented in this report. Diagnosis of these tumours should be based on clinical, radiographic and histopathological findings. Relying solely on histopathological findings may not be adequate in anticipating recurrent osteoblastoma of the maxilla.
References
- 1.Unni KK, Inwards CY, Bridge JA, Kindblom LG, Wold LE. Tumors of the bones and joints: AFIP atlas of tumor pathology Series 4, Fasc 2. Silver Spring, MD: American Registry of Pathology; 2005 [Google Scholar]
- 2.Lucas DR, Unni K, Mcleod RA, O'Connor MI, Sim FH. Osteoblastoma: clinicopathologic study of 306 cases. Hum Pathol 1994; 25: 117–134 [DOI] [PubMed] [Google Scholar]
- 3.Jones AC, Prihoda TJ, Kacher JE, Odingo NA, Freedman PD. Osteoblastoma of the maxilla and mandible: a report of 24 cases, review of the literature, and discussion of its relationship to osteoid osteoma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102: 639–650 [DOI] [PubMed] [Google Scholar]
- 4.Ribera MJ. Osteoblastoma in the anterior maxilla mimicking periapical pathosis of odontogenic origin. J Endod 1996; 22: 142–146 [DOI] [PubMed] [Google Scholar]
- 5.Ataoglu O, Oygur T, Yamalik K, Yucel E. Recurrent osteoblastoma of the mandible: a case report. J Oral Maxillofac Surg 1994; 52: 86–90 [DOI] [PubMed] [Google Scholar]
- 6.Colm SJ, Abrams MB, Waldron CA. Recurrent osteoblastoma of the mandible: report of a case. J Oral Maxillofacial Surg 1988; 46: 881–885 [DOI] [PubMed] [Google Scholar]
- 7.Borello ED, Sedano HO. Giant osteoid osteoma of the maxilla. Report of a case. Oral Surg Oral Med Oral Pathol 1967; 23: 563–566 [DOI] [PubMed] [Google Scholar]
- 8.Kent JN, Castro HF, Girotti WR. Benign osteoblastoma of the maxilla. Case report and review of the literature. Oral Surg Oral Med Oral Pathol 1969; 27: 209–219 [DOI] [PubMed] [Google Scholar]
- 9.Yip WK, Lee HT. Benign osteoblastoma of the maxilla. Oral Surg Oral Med Oral Pathol 1974; 38: 259–263 [DOI] [PubMed] [Google Scholar]
- 10.Chatterji P, Purohit GN, Ramdeo Bikaner IN. Benign osteoblastoma of the maxilla (periosteal). J Laryngol Otol 1978; 92: 337–345 [DOI] [PubMed] [Google Scholar]
- 11.Monks FT, Bradley JC, Turner EP. Central osteoblastoma or cementoblastoma? A case report and 12 year review. Br J Oral Surg 1981; 19: 29–37 [DOI] [PubMed] [Google Scholar]
- 12.Miller AS, Rambo HM, Bowser MW, Gross M. Benign osteoblastoma of the jaws: report of three cases. J Oral Surg 1980; 38: 694–697 [PubMed] [Google Scholar]
- 13.van der Waal I, Greebe RB, Elias EA. Benign osteoblastoma or osteoid osteoma of the maxilla. Report of a case. Int J Oral Surg 1983; 12: 355–358 [DOI] [PubMed] [Google Scholar]
- 14.Ohkubo T, Hernandez JC, Ooya K, Krutchkoff DJ. “Aggressive” osteoblastoma of the maxilla. Oral Surg Oral Med Oral Pathol 1989; 68: 69–73 [DOI] [PubMed] [Google Scholar]
- 15.Gordon SC, MacIntosh RB, Wesley RK. A review of osteoblastoma and case report of metachronous osteoblastoma and unicystic ameloblastoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 91: 570–575 [DOI] [PubMed] [Google Scholar]
- 16.Hatakeyama S, Suzuki A. Ultrastructural study of benign osteoblastoma of the maxilla. Acta Pathol Jpn 1979; 29: 791–799 [DOI] [PubMed] [Google Scholar]
- 17.Smith RA, Hansen LS, Resnick D, Chan W. Comparison of the osteoblastoma in gnathic and extragnathic sites. Oral Surg Oral Med Oral Pathol 1982; 54: 285–298 [DOI] [PubMed] [Google Scholar]
- 18.el-Mofty S, Refai H. Benign osteoblastoma of the maxilla. J Oral Maxillofac Surg 1989; 47: 60–64 [DOI] [PubMed] [Google Scholar]
- 19.Guest PG, Juniper RP. Osteoblastoma: a case report and description of the access used to the retromaxillary area. Br J Oral Maxillofac Surg 1991; 29: 333–335 [DOI] [PubMed] [Google Scholar]
- 20.Kroon HM, Schurmans J. Osteoblastoma: clinical and radiologic findings in 98 new cases. Radiology 1990; 175: 783–790 [DOI] [PubMed] [Google Scholar]
- 21.Jackson RP. Recurrent osteoblastoma: a review. Clin Orthop Relat Res 1978; 131: 229–233 [PubMed] [Google Scholar]
- 22.Alvares Capelozza AL, Gião Dezotti MS, Casati Alvares L, Negrão Fleury R, Sant'Ana E. Osteoblastoma of the mandible: systemic review of the literature and report of a case. Dentomaxillofac Radiology 2005; 34: 1–8 [DOI] [PubMed] [Google Scholar]
- 23.Dorfman HD, Weiss SW. Borderline osteoblastic tumors: problems in the differential diagnosis of aggressive osteoblastoma and low-grade osteosarcoma. Semin Diagn Pathol 1984; 1: 215–234 [PubMed] [Google Scholar]
- 24.Lypka MA, Goos RR, Yamashita DD, Melrose R. Aggressive osteoblastoma of the mandible. Int J Oral Maxillofac Surg 2008; 37: 675–8 [DOI] [PubMed] [Google Scholar]