Abstract
Purpose: This study determined whether returning to the community from a recent hospitalization with unmet activities of daily living (ADL) need was associated with probability of readmission. Methods: A total of 584 respondents to the 1994, 1999, and/or 2004 National Long-Term Care Surveys (NLTCS) who were hospitalized within 90 days prior to the interview and reported ADL disability at the time of the interview were considered for analysis. Medicare claims linked to the NLTCS provided information about hospital episodes, so those enrolled in Health Maintenance Organizations or Veterans Affairs Medical Centers were not included (n = 62), resulting in a total sample size of 522. ADL disability was defined as needing human help or equipment to complete the task. Unmet ADL need was defined as receiving inadequate or no help for one or more ADL disabilities. Disability that began within 90 days of the interview was considered new disability. Results: After adjusting for demographic, health, and functioning characteristics, unmet ADL need was associated with increased risk for hospital readmission (HR: 1.37, 95% CI: 1.03–1.82). Risk of readmission was greater for those with unmet need for new disabilities than those with unmet need for disabilities that were present before the index hospitalization (HR: 1.66, 95% CI: 1.01–2.73). Implications: Many older patients are discharged from the hospital with ADL disability. Those who report unmet need for new ADL disabilities after they return home from the hospital are particularly vulnerable to readmission. Patients' functional needs after discharge should be carefully evaluated and addressed.
Key Words: Activities of daily living, Insufficient help
More than half of hospitalized Medicare beneficiaries are readmitted within a year (Jencks, Williams, & Coleman, 2009). There is increasing concern that readmissions may reflect gaps in care. The Patient Protection and Affordable Care Act, Hospital Readmissions Reduction Program addresses these concerns by stating that hospitals with high risk-adjusted readmission rates will receive reduced Medicare payments for excess readmissions for specific conditions beginning in 2013. In addition, Section 3026 of the Affordable Care Act describes the Community Care Transitions Program, which provides funds for implementation of evidence-based care transition interventions for adults who are vulnerable for readmission. It is critical to determine which patients are most vulnerable for readmission so that interventions can be efficiently targeted toward, and effectively tailored to, these patients.
Andersen’s recursive model of health care utilization posits that outcomes of health services can affect patients’ predisposing risks (e.g., prior illness status), enabling resources (e.g., access to needed care) and illness risks (e.g., illness level) for subsequent use of health services (Andersen, 1995). This model provides a framework for understanding that postdischarge health status, health needs, and access to needed health care affect vulnerability for readmission. Prior studies have considered predischarge patient characteristics that predispose, enable, and create need for readmission (Jencks et al., 2009; Ross et al., 2008). However, little is known about postdischarge patient characteristics that contribute to hospital readmission.
Many hospitalized older adults are discharged with new or worse activities of daily living (ADL) disabilities from which they do not recover in the months after discharge (Boyd et al., 2008; Sands et al., 2003). Despite the high prevalence of functional disability at discharge, many discharge planners are unaware of patients’ resources for addressing their functional disabilities when they return home from the hospital (Bowles, Naylor, & Foust, 2002). An older study reported that 11% of patients reported that their functional needs were not met after discharge (Mamon et al., 1992), but that study did not consider whether unmet functional needs were associated with readmission. Although recent studies provide evidence that unmet need for functional disabilities increases risk for future hospital admissions, those studies do not specifically assess whether patients had unmet ADL needs after they returned home from a recent hospitalization and whether unmet ADL needs after discharge were associated with readmission (Arbaje et al., 2008; Sands et al., 2006; Xu, Covinsky, Stallard, Thomas, & Sands, 2012). The purpose of this study is to build upon prior studies by assessing whether returning home from the hospital with unmet need for new or existing ADL disabilities increases vulnerability for readmission. In the context of Andersen’s recursive model, access to needed ADL care after discharge is an enabling characteristic that could affect risk for readmission. The results of this study will inform whether discharge planning and transitional care interventions should include postdischarge access to resources to meet new and existing disabilities following discharge.
Methods
Overview
Data from a national community survey and linked Medicare claims were reviewed to identify a subset of participants who were living in the community with ADL disability within three months after hospital discharge. Participants were observed forward for one year to determine postdischarge risks for readmission.
Data Sources
Data were from the 1994, 1999 and 2004 community interviews from the NLTCS. The interview, conducted by trained census takers, provided information about participants’ demographic characteristics, ADL functioning, ADL help, and health status at the time of the interview. Medicare claims data from 1993 through 2005 provided information about hospital episodes.
Sample
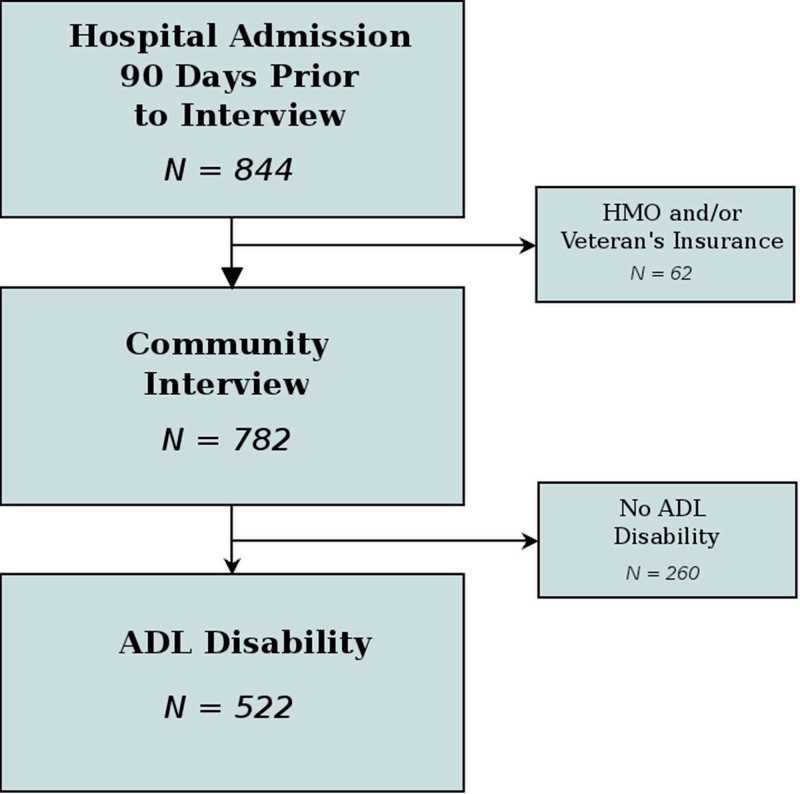
Respondents to the NLTCS community interviews were randomly selected community-living Medicare enrollees. Response rates were 95% or higher except for 2004 in which the response rate was closer to 90%. Included in this study was a subset of 844 respondents to the 1994, 1999, and 2004 community surveys that were living in the community and responded to the survey within three months after hospital discharge. Of these, 62 were excluded, because they received health care from a Health Maintenance Organization or a Veterans Affairs Medical Center, and their hospital episodes were unlikely to be recorded in the Medicare claims data. Of the remaining 782 respondents, an additional 260 were excluded, because they did not have ADL disability at the time of the interview. Only respondents with current ADL disabilities were included, because, presumably, one cannot have unmet ADL need unless one has an ADL disability. The final analytic sample size was 522 (see Figure 1). A subset of the analytic sample from this study was included in a larger study of 5,884 community-living older adults (Xu et al., 2012). That study did not focus on risks for readmission, nor did it include respondents with newly acquired ADL disability associated with a recent hospitalization.
Figure 1.
Flowchart of how sample was selected.
ADL Disability and Unmet ADL Need
For each ADL task (bathing, dressing, eating, toileting, and either getting out of bed or moving around a room), a respondent was considered to have a disability if they received help, required standby help, needed help but did not receive help, or used equipment to complete the task.
Participants were considered to have unmet ADL need if they reported that they did not receive needed help, could have used more help or had to wait to do the task, because they did not have enough help. This definition is similar to that used in previous studies of unmet need for ADL disabilities (Allen & Mor, 1997; Kennedy, 2001; LaPlante, Kaye, Kang, & Harrington, 2004).
New ADL disability was defined as disability that began less than three months prior to the interview. Existing ADL disability began more than three months prior to the community interview. Note that the index hospitalization occurred within three months of the interview.
Readmission
Date of readmission since the index discharge date was determined from the linked Medicare inpatient claims files.
Covariates
Information about predisposing, enabling, and need characteristics was obtained during the community survey and from linked Medicare claims data. Predisposing risks for readmission included age, gender, race (white vs. others), living arrangement (alone or not alone), and marital status (married vs. other). A proxy respondent indicated if the respondent was unable to respond to the interview due to illness or physical or cognitive disability. Prior illness status was defined as the number of previous hospital admissions within one year prior to the interview. This information was obtained from the inpatient claims files.
Need characteristics included diagnoses, disability level, and cognitive status. Presence of arthritis, diabetes, heart disease, emphysema, and cancer were determined from self-reports provided during the community survey. Participants were classified as having cognitive impairment if they had dementia or a score on a mental status test indicating presence of cognitive impairment (Pfeiffer, 1975; Tombaugh & McIntyre, 1992). Missing cognitive status was assigned to those who did not have dementia or a mental status score. Level of ADL disability was categorized as 1–2 and 3–5 ADL disabilities.
Unmet need for either a new or an existing ADL disability was the enabling characteristic examined in this study. Participants were classified as having zero versus one or more unmet needs.
Statistical Analyses
Bivariate Cox proportional hazards models were computed to assess the association between predisposing, enabling, and need characteristics and time until the first readmission (Allison, 1995). Right censoring occurred if the participant died, was admitted to a skilled nursing facility (after the community interview, but before a subsequent hospital admission), or at the end of the study interval if not readmitted priorly. Sampling weights reflecting each participant's probability of inclusion in the sample were included in the models to obtain design consistent parameter estimates. Standard errors were computed using the Taylor series linearization approach to adjust for the complex sampling design (Cox & Oakes, 1984; Grambsch & Therneau, 1994).
A multivariable Cox proportional hazards model was used to determine the association between unmet ADL need and readmission after controlling for postdischarge subject characteristics that predispose and create need for readmission. Models were simplified using backwards variable selection. A secondary analysis was computed using a multivariable Cox model to assess the risk of unmet need for a new ADL disability compared with unmet need for an existing ADL disability.
Model diagnostics were performed using Martingale residuals to detect nonlinearity and Schoenfeld residuals to test the proportional odds assumption (Fox, 2002; Therneau & Grambsch, 2000). To assess whether the results varied across time, a main effect for assessment occasion (1994, 1999, and 2004) and an interaction between unmet need and assessment occasion were included in the final models. Analyses were performed using the SAS 9.2 survey procedures and R 2.14.1 using the survey, survival, and ggplot2 packages.
Results
Table 1 reveals that the majority of participants were female (65%), white (85%), and lived with others (63%). Proxy respondents (e.g., family members) completed thirty percent of the interviews. Prevalence of diabetes (31%), cancer (15%), heart disease (60%), stroke (14%), and cognitive impairment (23%) were similar to those reported in other studies of disabled adults (Stineman et al., 2011).
Table 1.
Sample Characteristics
| N | Percent | ||
|---|---|---|---|
| Unweighted | Weighted | ||
| Sex | |||
| Male | 182 | 34.87 | 35 |
| Female | 340 | 65.13 | 65 |
| Race | |||
| White | 456 | 87.36 | 84.9 |
| Other | 66 | 12.64 | 15.1 |
| Living arrangement | |||
| Alone | 201 | 38.54 | 36.97 |
| Not alone | 320 | 61.42 | 63.03 |
| Proxy | |||
| No | 363 | 69.54 | 70.29 |
| Yes | 159 | 30.46 | 29.71 |
| Arthritis | |||
| No | 136 | 26.15 | 27.34 |
| Yes | 386 | 73.85 | 72.66 |
| Diabetes | |||
| No | 380 | 72.94 | 69.39 |
| Yes | 141 | 27.06 | 30.61 |
| Cancer | |||
| No | 438 | 84.39 | 84.82 |
| Yes | 81 | 15.61 | 15.18 |
| Heart disease | |||
| No | 214 | 41.31 | 40.28 |
| Yes | 304 | 58.69 | 59.72 |
| Stroke | |||
| No | 446 | 86.1 | 85.73 |
| Yes | 72 | 13.9 | 14.27 |
| Emphysema | |||
| No | 440 | 84.78 | 83.88 |
| Yes | 79 | 15.22 | 16.12 |
| Cognitively impaired | |||
| No | 253 | 48.47 | 48.11 |
| Yes | 119 | 22.8 | 22.57 |
| Missing | 150 | 28.74 | 29.32 |
| Number of ADL disabilities | |||
| 1–2 | 226 | 43.29 | 42.81 |
| 3–5 | 296 | 54.61 | 53.19 |
| Unmet ADL need | |||
| No | 380 | 72.8 | 70.83 |
| For existing disability | 109 | 20.8 | 21.62 |
| For new disability | 33 | 6.32 | 7.55 |
| Age | M = 78.14 SD = 7.54 | ||
| Number of previous hospital admissions | M = 1.84 SD = 1.23 | ||
Bivariate results (Table 2) show that participants most likely to be readmitted were of minority racial status (HR: 1.59, 95% CI: 1.08–2.35), and had a proxy (HR: 1.60, 95% CI: 1.19–2.25), diabetes (HR: 1.69, 95% CI: 1.27–2.25), more than one hospital admission prior to the index admission (HR: 1.51, 95% CI: 1.37–1.68), and 3–5 ADL disabilities (HR: 1.72, 95% CI: 1.31–2.27). Those who reported unmet need for ADL help were more likely to be readmitted in the year following the index hospitalization (HR: 1.66, 95% CI: 1.25– 2.20). The bivariate analyses also reveal that those with unmet need, either for a new or an existing ADL disability was associated with increased risk for readmission (HR: 2.37; 95% CI: 1.37–4.11 and HR: 1.61; 95% CI: 1.21–2.14, respectively).
Table 2.
Unadjusted Risks for Readmission
| Weighted readmission (%) | p value | Hazard ratio (95% CI) | |
|---|---|---|---|
| Gender | |||
| Female | 53.52 | — | — |
| Male | 56.04 | .34 | 1.15 (.86, 1.53) |
| Race | |||
| White | 55.96 | — | — |
| Other | 68.05 | .02 | 1.59 (1.08, 2.35) |
| Living arrangement | |||
| Alone | 51.86 | — | — |
| Not alone | 61.19 | .08 | 1.28 (.97, 1.68) |
| Proxy | |||
| No | 52.9 | — | — |
| Yes | 69.34 | .002 | 1.60 (1.19, 2.14) |
| Arthritis | |||
| No | 65.06 | — | — |
| Yes | 55.1 | .1 | .77 (.57, 1.05) |
| Diabetes | |||
| No | 52.4 | — | — |
| Yes | 69.7 | <.001 | 1.69 (1.27, 2.25) |
| Cancer | |||
| No | 56.4 | — | — |
| Yes | 63.38 | .83 | .96 (.68, 1.34) |
| Heart disease | |||
| No | 52.21 | — | — |
| Yes | 61.54 | .08 | 1.28 (.97, 1.68) |
| Stroke | |||
| No | 56.1 | — | — |
| Yes | 67.79 | .15 | 1.27 (.92, 1.76) |
| Emphysema | |||
| No | 56.69 | — | — |
| Yes | 63.94 | .6 | 1.10 (.77, 1.58) |
| Cognitively impaired | |||
| No | 53.79 | — | — |
| Yes | 63.62 | .06 | 1.37 (.99, 1.91) |
| Missing | 59.86 | .3 | 1.19 (.85, 1.67) |
| Number of ADL disabilities | |||
| 1–2 | 46.68 | — | — |
| 3–5 | 66.1 | <.001 | 1.72 (1.31, 2.27) |
| Unmet ADL need | |||
| No | 51.61 | — | — |
| Yes | 72.78 | <.001 | 1.66 (1.25, 2.20) |
| Unmet ADL need | |||
| No | 51.61 | — | — |
| For existing disability | 71.61 | .001 | 1.61 (1.21, 2.14) |
| For new disability | 76.13 | .002 | 2.37 (1.37, 4.11) |
| Age | .72 | 1.00 (.99, 1.02) | |
| Number of previous hospital admissions | <.001 | 1.51 (1.37, 1.68) | |
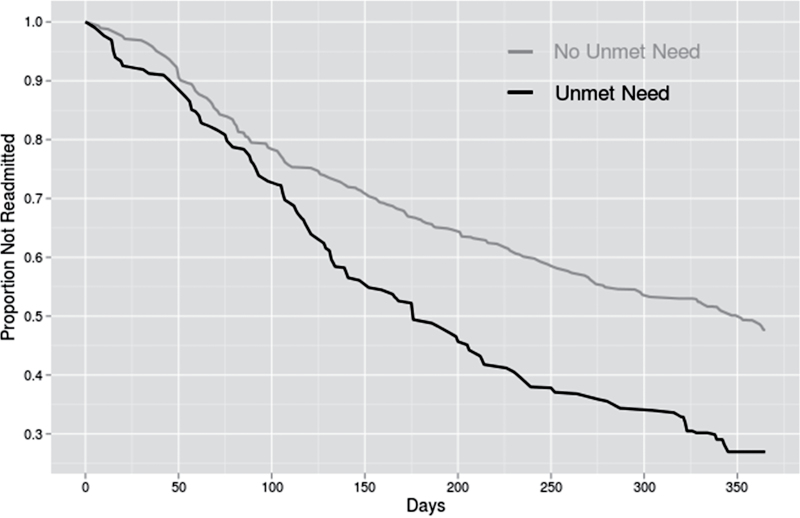
Table 3 reports adjusted risks for readmission. Higher age and having diabetes, more than one previous hospital admission, more than two ADL disabilities, and unmet need for an ADL disability were associated with an increased risk of readmission (HR: 1.37; 95% CI: 1.03, 1.82). The effects of assessment occasion and the interaction between assessment occasion and unmet need were not significant, indicating that the effect of unmet need on hospital readmission did not change significantly over time. Figure 2 illustrates the time to readmission for those with and without unmet ADL need.
Table 3.
Adjusted Risks for Readmission Including Presence versus Absence of Unmet ADL Need
| Hazard ratio (95% CI) | |
|---|---|
| Age in years | 1.02 (1.00, 1.04) |
| Diabetes | |
| No | — |
| Yes | 1.53 (1.16, 2.02) |
| Number of previous hospital admissions | 1.51 (1.37, 1.67) |
| Number of ADL disabilities | |
| 1–2 | — |
| 3–5 | 1.41 (1.05, 1.89) |
| Unmet ADL need | |
| No | — |
| Yes | 1.37 (1.03, 1.82) |
Figure 2.
Kaplan-Meier curves representing hospital readmission risk associated with unmet activities of daily living (ADL) need.
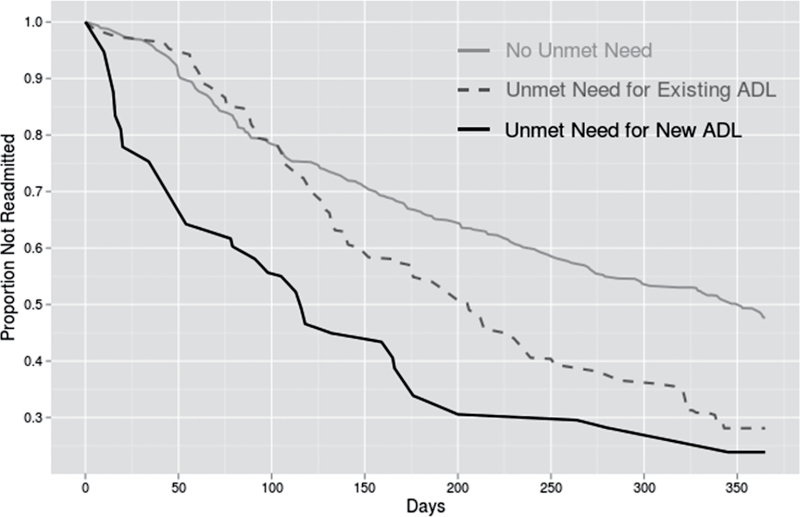
Secondary analyses showed that the hazard ratio for risk of readmission for those who reported unmet need for existing disability was 1.22 (95% CI: .90–1.65) and those who reported unmet need for new disability was 2.02 (95% CI: 1.24–3.30) compared with no unmet need (Table 4). The effect of unmet need did not change over time as demonstrated by the nonsignificant effect of assessment occasion and the nonsignificant interaction between assessment occasion and unmet need. The hazard ratio for unmet need for new disability compared with existing need for an ADL disability was 1.66 (95% CI: 1.01–2.73, see Figure 3).
Table 4.
Adjusted Risks for Readmission Including Unmet ADL Need for New and Existing Disabilities
| Hazard ratio (95% CI) | |
|---|---|
| Age in Years | 1.02 (1.00, 1.04) |
| Diabetes | |
| No | — |
| Yes | 1.53 (1.38, 1.69) |
| Number of previous hospital admissions | 1.55 (1.18, 2.04) |
| Number of ADL disabilities | |
| 1–2 | — |
| 3–5 | 1.39 (1.03, 1.88) |
| Unmet ADL need | |
| No | — |
| For existing disability | 1.22 (.90, 1.65) |
| For new disability | 2.02 (1.24, 3.30) |
Figure 3.
Kaplan-Meier curves representing hospital readmission risk for unmet need for existing and new activities of daily living (ADL) disabilities.
Discussion
One in four hospitalized Medicare patients return home with unmet need for new or existing ADL disabilities. Unmet ADL need increases risk for readmission, especially among patients who report unmet needs for recently acquired ADL disabilities. It is well documented that hospitalization is associated with the declines in ADL functioning. These declines persist after hospitalization despite the effectiveness of interventions to reduce hospital-associated functional decline (Counsell et al., 2000; Landefeld, Palmer, Kresevic, Fortinsky, & Kowal, 1995). This study provides evidence that ADL needs should be thoroughly assessed and addressed after the patients return home from a hospital episode.
To our knowledge, only two studies considered whether unmet need for functional disabilities increases risk for readmission. A study conducted in Italy demonstrated that living alone and lack of regular emotional or material support is associated with readmission. The study did not explicate whether lack of emotional support versus support for physical disabilities contributed to readmission rates (Di Iorio et al., 1998). A study of Medicare patients revealed that persons who experienced two hospitalizations within 60 days had reported unmet needs for one or more ADL or IADL disabilities prior to the first hospitalization (Arbaje et al., 2008). The authors acknowledge a limitation of that study was that it was not possible to determine whether unmet functional needs changed during the year of monitoring for readmission. In contrast, our study design provided the opportunity to demonstrate that participants who return to the community with unmet need for an ADL disability developed since the index hospitalization are more vulnerable for readmission than those who return home with unmet need for an ADL disability acquired prior to the index hospitalization.
The transition from hospital to home is problematic for many patients (Murtaugh & Litke, 2002), especially when that transition involves coping with functional disabilities for which patients feel they do not have adequate help. Formal home care services provide assistance to patients with poor functional status who are vulnerable to readmission (Bowles et al., 2002; Jencks et al., 2009), but only 4% of the patients are discharged with home care (Wier et al., 2010). Absence of home care increases the risk for hospitalization (Xu et al., 2010) and readmission (Bowles et al., 2002). Collectively, this evidence suggests that patients’ functional needs should be carefully evaluated after discharge. A recent review reveals that most postdischarge or transitional care interventions focus on medical management, but few address patients’ functional needs after discharge (Naylor, Aiken, Kurtzman, Olds, & Hirschnan, 2011).
Limitations
The findings must be considered in the context of the limitations of conducting research with existing data. First, we were not able to determine whether participants experienced a constant or periodic state of unmet ADL need. Nonetheless, results revealed that a single “snapshot” assessment of unmet need after discharge is prognostic of readmission. Second, we cannot specify the reason the individual reported unmet need. The most common reasons for reporting unmet need are that 1) the help does not occur when needed, 2) the amount of help is insufficient, and 3) the person helping with the task is not able to do what is needed (e.g., help with transferring or bathing) (LaPlante et al., 2004). Third, we cannot verify that new unmet need developed as a consequence of the illness or injury that precipitated the index hospitalization. However, it is likely that most ADL disability that began within this interval is related to the reason for the index hospitalization, because nearly half of incident ADL disability occurs in the context of hospitalization (Covinsky et al., 2000; Mehta et al., 2011). Fourth, we cannot describe the mechanism by which unmet need led to readmission. Unmet need is associated with self-reports of inadequate nutrition, skin breakdown, falls, and significantly reduced mobility in the home (LaPlante et al., 2004). However, billing records are not designed to describe causal pathways for admission. Fifth, data are not available to determine whether patients had unmet need in other aspects of self-care that are commonly included in surgical or medical discharge plans. For example, a study conducted in Japan revealed that unmet need for medication administration increases risk for hospitalization (Kuzuya et al., 2008). Despite these limitations, the results provide evidence that asking patients whether they have sufficient help at home for their self-care needs may be effective in identifying a modifiable risk for readmission.
Conclusion
Comprehensive discharge planning and transitional care interventions can reduce readmission rates (Naylor et al., 2011; Phillips et al., 2004). The results of this study provide evidence that eligibility for transitional care should include consideration of whether a patient has sufficient ADL help after returning home from a hospitalization.
Funding
This research was funded by a grant from the National Institutes of Health (R01AG034160) to L. P. Sands.
References
- Allen S., Mor V. (1997). The prevalence and consequences of unmet need: Contrasts between older and younger adults with disability. Medical Care, 35, 1132–1148 doi:10.1097/00005650-199711000-00005 [DOI] [PubMed] [Google Scholar]
- Allison P. (1995). Survival analysis using the sas system: A practical guide. Cary, NC: SAS Institute; [Google Scholar]
- Andersen R. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36, 1–10 doi:10.1207/2137284 [PubMed] [Google Scholar]
- Arbaje A., Wolff J., Yu Q., Powe N., Anderson G., Boult C. (2008). Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Journal of the American Geriatrics Society, 48, 495–504 doi:10.1093/geront/48.4.495 [DOI] [PubMed] [Google Scholar]
- Bowles K., Naylor M., Foust J. (2002). Patient characteristics at hospital discharge and a comparison of home care referral decisions. Journal of the American Geriatrics Society, 50, 336–342 doi:10.1046/j.1532-5415.2002.50067.x [DOI] [PubMed] [Google Scholar]
- Boyd C., Landefeld C., Counsell S., Palmer R., Fortinsky R., Kresevic D, et al. (2008). Recovery of activities of daily living in older adults after hospitalization for acute medical illness. Journal of the American Geriatrics Society, 56, 2171–2179 doi:10.1111/j.1532-5415.2008.02023.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Counsell S., Holder C. M., Liebenauer L. L., Palmer R. M., Fortinsky R. M., Kresevic D, et al. (2000). Effects of a multicomponent invervention on functional outcomes and process of care in hospitalized older patients: A randomized controlled trial of acute care for elders (ACE) in a community hospital. Journal of the American Geriatrics Society, 48, 1572–1581 [DOI] [PubMed] [Google Scholar]
- Covinsky K., Palmer R., Counsell S., Pine Z., Walter L., Chren M. (2000). Retrospective reports of functional status in hospitalized elders: Evidence of validity. Journal of the American Geriatrics Society, 48, 164–169 [DOI] [PubMed] [Google Scholar]
- Cox D., Oakes D. (1984). Analysis of survival data. Boca Raton, FL: Chapman and Hall; [Google Scholar]
- Di Iorio A., Long A., Costanza M., Bandinelli S., Capasso S., Gigante M, et al. (1998). Characteristics of geriatric patients related to early and late readmissions to hospital. Aging Clinical and Experimental Research, 10, 339–346 [DOI] [PubMed] [Google Scholar]
- Fox J. (2002). Cox proportional-hazards regression for survival data: Appendix to an R and S-PLUS companion to applied regression Retrieved April 2012, from http://cran.r-project.org/doc/contrib/Fox-Companion/appendix-cox-regression.pdf
- Grambsch P., Therneau T. (1994). Proportional hazards tests and diagnostics based on weighted residuals. Biometrika, 81, 515–526 doi:10.1093/biomet/81.3.515 [Google Scholar]
- Jencks S., Williams M., Coleman E. (2009). Rehospitalizations among patients in the Medicare fee-for-service program. The New England Journal of Medicine, 360, 1418–1428AID-10.1058NEJMsa0803563[doi] [DOI] [PubMed] [Google Scholar]
- Kennedy J. (2001). Unmet and undermet need for activities of daily living and instrumental activities of daily living assistance among adults with disabilities. Medical Care, 39, 1305–1312 doi:10.1097/00005650-200112000-00006 [DOI] [PubMed] [Google Scholar]
- Kuzuya M., Hirakawa Y., Suzuki Y., Iwata M., Enoki H., Hasegawa J, et al. (2008). Association between unmet needs for medication support and all-cause hospitalization in community-dwelling disabled elderly people. Journal of the American Geriatrics Society, 56, 881–886 doi:10.1111/j.1532-5415.2008.01676.x [DOI] [PubMed] [Google Scholar]
- Landefeld C. S., Palmer R. M., Kresevic D. M., Fortinsky R. H., Kowal J. (1995). A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. The New England Journal of Medicine, 332, 1338–1344 doi:10.1056/NEJM199505183322006 [DOI] [PubMed] [Google Scholar]
- LaPlante M., Kaye S., Kang T., Harrington C. (2004). Unmet need for personal assistance services: Estimating the shortfall in hours of help and adverse consequences. Journal of Gerontology: Social Sciences, 59B, S98–S108 doi:10.1093/geronb/59.2.S98 [DOI] [PubMed] [Google Scholar]
- Mamon J., Steinwach D., Fahey M., Bone L., Oktay J., Klein L. (1992). Impact of hospital discharge planning on meeting patient needs after returning home. Health Services Research, 27, 155–175 [PMC free article] [PubMed] [Google Scholar]
- Mehta K., Pierluissi E., Boscardin W., Kirby K., Walter L., Chren M, et al. (2011). A clinical index to stratify hospitalized older adults according to risk for new-onset disability. Journal of the American Geriatrics Society, 59, 1206–1216 doi:10.1111/j.1532-5415.2011.03409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murtaugh C., Litke A. (2002). Transitions through postacute and long-term care settings. Medical Care, 40, 227–236 [DOI] [PubMed] [Google Scholar]
- Naylor M., Aiken L., Kurtzman E., Olds D., Hirschman K. (2011). Health Affairs, 30, 746–754 doi:10.1377/hlthaff.2011.0041 [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. (1975). A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society, 23, 433–441 [DOI] [PubMed] [Google Scholar]
- Phillips C., Wright S., Kern D., Singa R., Shepperd S., Rubin H. (2004). Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure. Journal of the American Medical Association, 291, 1358–1367 doi:10.1001/jama.291.11.1358 [DOI] [PubMed] [Google Scholar]
- Ross J., Mulvey G., Stauffer B., Patlolla V., Bernheim S., Keenan P., Krumholz H. (2008). Statistical models and patient predictors of readmission for heart failure. A systematic review. Archives of Internal Medicine, 168, 1371–1386 doi:10.1001/archinte.168.13.1371 [DOI] [PubMed] [Google Scholar]
- Sands L., Wang Y., McCabe G., Jennings K., Eng C., Covinsky K. (2006). Rates of acute care admissions for frail elders living with met versus unmet activity of daily living needs. Journal of the American Geriatrics Society, 54, 339–344 doi:10.1111/j.15325415.2005322590.x [DOI] [PubMed] [Google Scholar]
- Sands L., Yaffe K., Covinsky K., Chren M., Counsell S., Palmer R, et al. (2003). Cognitive screening predicts magnitude of functional recovery from admission to 3 months after discharge in hospitalized elders. Journal of Gerontology: Medical Sciences, 58A, 37–45 doi:10.1093/gerona/58.1.M37 [DOI] [PubMed] [Google Scholar]
- Stineman M., Xie D., Pan Q., Kurichi J., Saliba D., Streim J. (2011). Activity of daily living staging, chronic health conditions, and perceived lack of home accessibility features for elderly people living in the community. Journal of the American Geriatrics Society, 59, 454–462 doi:10.1111/j.1532-5415.2010.03287.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Therneau T., Grambsch P. (2000). Modeling survival data: Extending the Cox model. New York, NY: Springer; [Google Scholar]
- Tombaugh T., McIntyre N. (1992). The mini-mental state examination: A comprehensive review. Journal of the American Geriatrics Society, 40, 922–935 doi:10.1037//1040-3590.8.1.48 [DOI] [PubMed] [Google Scholar]
- Wier L., Levit K., Stranges E., Ryan K., Pfuntner A., Vandivort R, et al. (2010). HCUP facts and figures: Statistics on hospital-based care in the United States, 2008 Rockville, MD: Retrieved from http://www.hcup-us.ahrq.gov/reports.jsp [Google Scholar]
- Xu H., Covinsky K., Stallard E., Thomas J., Sands L. (2012). Insufficient help for ADL disabilities and risk for all-cause hospitalization. Journal of the American Geriatrics Society, 60, 927–933 doi:10.1111/j.1532-5415.2012.03926.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Weiner M., Paul S., Thomas J., III, Craig B., Rosenman M, et al. (2010). Volume of home- and community-based Medicaid Waiver services and risk of hospital admissions. Journal of the American Geriatrics Society, 58, 109–115 doi:10.1111/j.1532-5415.2009.02614.x [DOI] [PubMed] [Google Scholar]