Abstract
Background
Prescription opioid use disorders are the second most common drug use disorder behind only cannabis use disorders. Despite this, very little is known about the help-seeking behavior among individuals with these disorders.
Methods
The sample included respondents of the Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) with a lifetime diagnosis of prescription drug use disorders (N= 623). Unadjusted and adjusted hazard ratios are presented for time to first treatment-seeking by sociodemographic characteristics and comorbid psychiatric disorders.
Results
The lifetime cumulative probability of treatment seeking was 42% and the median delay from prescription drug use disorder onset to first treatment was 3.83 years. Having an earlier onset of prescription opioid use disorder and a history of bipolar disorder, major depression disorder, specific phobia and cluster B personality disorders predicted shorter delays to treatment.
Conclusions
Although some comorbid psychiatric disorders increase the rate of treatment-seeking and decrease delays to first-treatment contact rates of treatment-seeking for prescription drug use disorder are low, even when compared with rates of treatment for other substance use disorders. Given the high prevalence and adverse consequences of prescription drug use disorder, there is a need to improve detection and treatment of prescription opioid use disorder.
Keywords: Treatment-seeking, prescription opioid use disorders, substance use disorders, comorbidity
1. INTRODUCTION
Although the therapeutic use of the opioids in the management of pain has long been established and opioids may even be underutilized at times (Ballantyne, 2007; Trescot et al., 2006, 2008) there also is growing concern that over the last two decades, there has been a large increase in the prevalence of prescription opioid use disorders (Blanco et al., 2007; Cicero and Inciardi, 2005; Compton and Volkow, 2006; McCabe, 2005; Rigg and Ibanez; Zacny et al., 2003). It is estimated that the 12-month prevalence of prescription opioid use disorders is 0.30% (Blanco et al., 2007), affecting over one million adults in the US (Grant et al., 2004b). Prescription opioid use disorders represent the second most common drug use disorders, behind only cannabis use disorders, 1.45% (Grant et al., 2004c), and slightly more prevalent as cocaine use disorders, 0.27% (Grant et al., 2004c).
Prescription opioid use disorders are associated with increased risk of several psychiatric and general medical disorders including cardiac arrhythmias and respiratory depression. Prescription opioid use disorders also lead to substantial impairment in daily functioning and an increased risk of premature death (Huang et al., 2006; Kuehn, 2012). In a claims-based analysis of 2 million employees and their dependents, individuals treated for opioid use disorders, including abuse and dependence, incurred 8.7 times greater mean annual direct health care costs than those who were not treated for opioid use disorders ($15,884 vs. $1,830; White et al., 2005). In 2007, total US societal costs of prescription drug use disorder were approximately $55.7 billion (Birnbaum et al., 2011). Despite the rising prevalence and extensive personal burden and societal costs, little is known about the timing and pattern of treatment-seeking for these disorders. A better understanding of the patterns and predictors of treatment-seeking for prescription opioid drug disorders is necessary to identify and address the modifiable barriers to treatment faced by this population (Rogler and Cortes, 1993).
Several studies have examined predictors of treatment-seeking of individuals with psychiatric disorders (Adamson et al., 2003; Alegria et al., 2002; Kessler et al., 2001, 1998; Mojtabai et al., 2002; Olfson et al., 1998; Wang et al., 2005). Among the common mental disorders, substance use disorders have the lowest probability of treatment contact during the first year following disorder onset and the longest delay from onset of the disorder to first treatment contact (Olfson et al., 1998; Wang et al., 2005). In a community sample of adults with substance use disorders, approximately one-half of all lifetime cases had never established treatment contact. Lower rates of treatment for substance use disorders were associated with earlier age of disorder onset, male gender and racial-ethnic minority ancestry (Kessler et al., 2001; Olfson et al., 1998; Perron et al., 2009). Because these studies aggregated all drugs into a single analytic category, the specific patterns associated with prescription opioid use disorders remain unknown. However, prior studies have suggested that the risk factors (Blanco et al., 2007; Huang et al., 2006) and course (Blanco et al., 2012; Martins et al., 2012) of prescription opioid use disorder differ from those of abuse and dependence on illicit drugs (Compton et al., 2007; Lopez-Quintero et al., 2011a, 2011b) suggesting that their pattern of treatment-seeking may also differ.
In the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), approximately one quarter of respondents with prescription opioid use disorder reported having ever received drug abuse treatment at the time of the survey (Blanco et al., 2007). Previous analyses of the NESARC data or other epidemiological surveys have not examined delays to first treatment-contact, identified predictors of treatment-seeking, or estimated cumulative lifetime rates of treatment-seeking for prescription opioid drug disorder. The primary goal of this study was to identify factors associated with delays in time to first treatment seeking for lifetime prescription opioid use disorder. A greater understanding of these factors may help inform service planning and help identify modifiable barriers to treatment access. Based on prior work (Blanco et al., 2007) we hypothesized that the cumulative rates of treatment-seeking would be less than 50% and that an earlier age of disorder onset (Kessler et al., 1998; Olfson et al., 1998; Wang et al., 2004), male sex, and minority racial/ethnic ancestry (Adamson et al., 2003; Alegria et al., 2002) would predict longer delays to first-treatment contact.
2. METHOD
2.1 Sample
The target population of the 2004–2005 Wave 2 NESARC (Grant, 2007b, 2007c) was the civilian, non-institutionalized population 18 years and older, residing in households and group quarters (e.g., college quarters, group homes, boarding houses, and non-transient hotels). Blacks, Hispanics, and adults ages 18-24 years were oversampled.
Of the 43,093 respondents interviewed at Wave 1, 34,653 respondents (86.7% of eligible responders) were re-interviewed at Wave 2. Sample weights were developed to adjust for the sampling design as well as Wave 2 non-response. Once weighted, data are representative of the US population for region, age, sex, race, and ethnicity. There were no significant differences between Wave 1 and 2 respondents in terms of several baseline (Wave 1) socio-demographic measures or the presence of any lifetime substance, mood, anxiety or personality disorder (Grant, 2007b).
2.2 Assessment
Sociodemographic measures included sex, race-ethnicity (White, Black, Native American, Asian and Hispanic), nativity (US-born versus foreign born), age (as continuous variable), education (less than high school, high school, and college), and marital status (married/cohabiting, widowed/separated/divorced, and never married). The diagnostic interview was the Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-IV Version (AUDADIS-IV), Wave 2 version. This structured interview was designed for administration by experienced professional lay interviewers.
Prescription opioid use disorders included DSM-IV abuse or dependence of prescription opioids, as assessed by the AUDADIS. AUDADIS assessment of DSM-IV alcohol and drug-specific abuse and dependence have good to excellent (κ=0.70-0.91) test-retest reliability (Grant et al., 1995). Mood disorders included DSM-IV major depressive disorder (MDD), bipolar disorder, and dysthymia.
Anxiety disorders included panic disorder, social anxiety disorder (SAD), specific phobia, posttraumatic stress disorder (PTSD), and generalized anxiety disorder (GAD) (Grant et al., 2001, 2009). Test-retest reliabilities for mood and anxiety diagnoses were fair to good (κ=0.40-0.77; Chatterji et al., 1997; Grant et al., 2003, 2009, 1995; Hasin et al., 1997; Ruan et al., 2008). Wave 1 lifetime personality disorders assessments (Cottler et al., 1997; Grant et al., 2005) included avoidant, dependent, obsessive-compulsive, paranoid, schizoid, histrionic, and antisocial personality disorders and Wave 2 assessments included borderline, schizotypal, and narcissistic personality disorders with test re-test reliability of κ=0.67-0.71 (Grant et al., 2004a). Respondents were asked a series of DSM-IV personality disorder symptom questions about how they acted throughout their lives in different situations. To receive a DSM-IV diagnosis, respondents had to endorse the requisite number of DSM-IV symptoms for the particular personality disorder and at least one symptom must have caused social or occupational dysfunction. Nationally representative samples seldom assess personality disorders but recent work suggests they have been important predictors of treatment-seeking (Olfson et al., 2012).
Lifetime onset of substance use disorders and other axis I disorders were determined retrospectively by the earliest age in years at which respondents reported meeting criteria for each disorder. Respondents with a lifetime diagnosis of prescription opioid drug use disorder were also asked whether they had ever in their life seen a general medical, mental health, or human service professional for prescription opioid drug use disorders. Affirmative responses were followed by a question to assess the age at which the respondent had first contacted a professional for prescription opioid drug use disorders. These two questions were used to determine the occurrence and timing of first treatment contact.
2.3 Statistical analyses
Among respondents with lifetime prescription opioid drug use disorders (N=623), weighted cross-tabulations were used to calculate the proportion who had ever sought treatment for prescription opioid drug use disorder overall and by respondent socio-demographic and clinical characteristics (Table 1).
Table 1.
Descriptive statistics of lifetime treatment seeking among individuals with prescription opioid use disorder, stratified by characteristics at time of assessment disordera
| N | % Seeking Treatment | SE | Odds Ratio | 95% CI | ||
|---|---|---|---|---|---|---|
| Total | 623 | 29.20 | 2.15 | |||
| Sex | ||||||
| Male | 351 | 26.24 | 2.68 | 0.67 | 0.43 | 1.04 |
| Female | 272 | 34.71 | 3.73 | 1.00 | 1.00 | 1.00 |
| Race/Ethnicity | ||||||
| White (ref) | 430 | 30.23 | 2.39 | 1.00 | 1.00 | 1.00 |
| Black | 69 | 28.45 | 6.46 | 0.92 | 0.47 | 1.79 |
| Native Americans | 29 | 27.79 | 9.02 | 0.89 | 0.36 | 2.22 |
| Asian | 9 | 15.40 | 14.49 | 0.42 | 0.05 | 3.85 |
| Hispanic | 86 | 25.17 | 7.29 | 0.78 | 0.35 | 1.73 |
| Nativity | ||||||
| US-born (ref) | 594 | 29.52 | 2.18 | 1.00 | 1.00 | 1.00 |
| Foreign-born | 29 | 21.78 | 10.10 | 0.66 | 0.20 | 2.20 |
| Educational years | ||||||
| Less than high school | 99 | 23.43 | 4.58 | 0.73 | 0.40 | 1.33 |
| High school | 182 | 31.45 | 4.16 | 1.09 | 0.65 | 1.83 |
| College (ref) | 342 | 29.66 | 3.28 | 1.00 | 1.00 | 1.00 |
| Marital Status | ||||||
| Married | 281 | 27.16 | 2.77 | 1.00 | 1.00 | 1.00 |
| Widowed/ separated/ divorced | 187 | 32.60 | 4.33 | 1.30 | 0.80 | 2.10 |
| Never Married | 155 | 30.46 | 3.99 | 1.17 | 0.77 | 1.80 |
| Mean | t-test | p | ||||
| Age at prescription opioid use disorder onset | 623 | 27.80 | 1.20 | -0.27 |
Data from NESARC Wave 2.
b. (ref)= reference group.
To assess the effects of sociodemographic and clinical characteristics on time to first prescription opioid treatment seeking, survival analysis with time-varying covariate models were performed. Retrospective follow-up time started at age of prescription opioid drug use disorder onset and terminated at age of first treatment contact. The probability of treatment-seeking was first modeled separately for each individual sociodemographic and diagnostic predictor and again in a single model that controlled for the potentially confounding effects of sex, race/ethnicity, nativity, age at prescription opioid drug use disorder onset, education years, marital status, and each of the diagnostic categories, including alcohol use disorder, drug use disorder, nicotine dependence, dysthymia, MDD, bipolar disorder, SAD, specific phobia, PTSD, GAD, and Cluster A, B and C personality disorders.
Personality disorders, divided in Cluster A, Cluster B and Cluster C, were coded as lifetime disorders with onset at age 18. Results are reported, respectively, as hazard ratios and adjusted hazard ratios with associated 95% confidence intervals (95% CI). Standard errors and 95% CI for all analyses were estimated using SUDAAN to adjust for the complex design of the NESARC (Kirana et al., 2009).
3. RESULTS
3.1 Lifetime Treatment Seeking for Non Medical Prescription Opioid Use Disorders
Among individuals with prescription opioid drug disorder (N=623), the cumulative probabilities of seeking treatment from the onset of the disorder in the first year (11.1%), first 10 years (24.5%), and ever (42.4%) are represented in Figure 1. The median delay to treatment-seeking among those who sought treatment was 3.83 years. There was no significant difference in rates of treatment-seeking between males and in females (OR: 0.67; CI=0.43-1.04), between Whites compared to Blacks (OR: 0.92; CI=0.47-1.79), Native Americans (OR: 0.80; CI=0.36-2.22), Asians (OR: 0.42; CI=0.05-3.85) or Hispanics (OR: 0.78; CI=0.35-1.73), between US-born compared to foreign-born persons (OR:0.66; CI=0.20-2.20), between adults with a high school education (OR: 1.09; CI=0.65-1.83) or less (OR: 0.73; CI=0.40-1.33) compared to those who attended some college, and between widowed or never married individuals compared to those married (Table 1).
Figure 1.
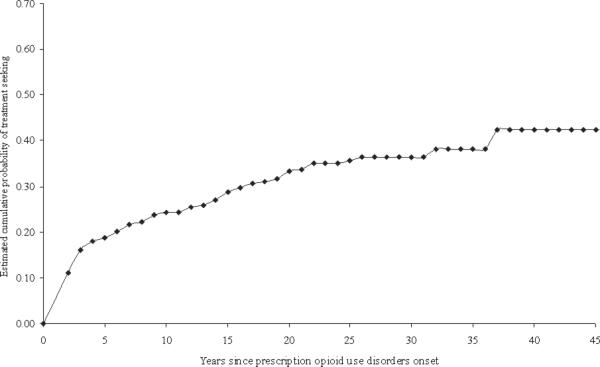
Cumulative probability of treatment-seeking among individuals with prescription opioid use disorder in the NESARC Wave 2 (n= 623).
3.2 Time to First Treatment
In the unadjusted model, males (HR: 0.58; CI=0.36-0.92) and individuals with an earlier age of onset (HR: 1.13; CI=1.09-1.17) had longer delays to treatment-seeking than females and those with a later onset, respectively, whereas having as opposed to not having an alcohol (HR: 1.97; CI=1.26-3.07) or drug use disorder (HR: 1.93; CI=1.12-3.31), nicotine dependence (HR: 1.72; CI=1.09-2.71), dysthymia (HR: 2.70; CI=1.38-5.28), MDD (HR: 2.32; CI=1.44-3.75), bipolar disorder (HR: 3.65; CI=2.07-6.42), panic disorder (HR: 3.00; CI=1.55-5.83), specific phobia (HR: 2.11; CI=1.26-3.54), GAD (HR: 3.50; CI=1.97-6.24), or a cluster A (HR: 1.81; CI=1.02-3.22) or B (HR: 2.49; CI=1.52-4.06) personality disorders increased the probability of treatment-seeking.
After adjusting for potentially confounding effects of the other covariates, significantly shorter delays in first prescription opioid drug use disorders treatment seeking were associated with being Asian (HR: 5.22; CI=1.67-16.27) , having an earlier age of onset of prescription drug use disorder (HR: 1.10; CI=1.06-1.14), and a history of comorbid MDD (HR: 2.24; CI=1.29-3.90), bipolar disorder (HR: 2.59; CI=1.44-4.67), specific phobia (HR: 1.84; CI=1.06-3.20) and Cluster B personality disorder (HR: 1.76; CI=1.04-3.00; Table 2).
Table 2.
Survival analysis of sociodemographic characteristics on the time to seeking treatment for major depressive disorder, unadjusted and adjusted analysesa,b
| Unadjusted HR | 95%CI | Adjusted HRc | 95%CI | |||
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 0.58 | 0.36 | 0.92 | 0.68 | 0.42 | 1.08 |
| Female | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Race/Ethnicity | ||||||
| White (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 0.83 | 0.43 | 1.61 | 0.70 | 0.38 | 1.30 |
| Native Americans | 0.52 | 0.18 | 1.54 | 0.81 | 0.34 | 1.91 |
| Asian | 3.08 | 0.91 | 10.45 | 5.22 | 1.67 | 16.27 |
| Hispanic | 1.33 | 0.50 | 3.52 | 0.81 | 0.35 | 1.88 |
| Nativity | ||||||
| US-born (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Foreign-born | 2.33 | 0.72 | 7.50 | 1.49 | 0.49 | 4.52 |
| Age at prescription opioid use disorder onset | 1.13 | 1.09 | 1.17 | 1.10 | 1.06 | 1.14 |
| Educational yearsd | 1.01 | 0.94 | 1.10 | 0.99 | 0.90 | 1.10 |
| Marital Statusd | ||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Widowed/ separated/ divorced | 1.54 | 0.87 | 2.74 | 0.98 | 0.54 | 1.78 |
| Never Married | 1.33 | 0.80 | 2.22 | 1.15 | 0.70 | 1.88 |
| Lifetime Comorbidityd | ||||||
| Alcohol Use Disorder | 1.97 | 1.26 | 3.07 | 1.44 | 0.97 | 2.15 |
| Drug Use Disorder | 1.93 | 1.12 | 3.31 | 1.30 | 0.83 | 2.03 |
| Nicotine Dependence | 1.72 | 1.09 | 2.71 | 1.32 | 0.84 | 2.07 |
| Dysthymia | 2.70 | 1.38 | 5.28 | 1.30 | 0.62 | 2.74 |
| Major Depressive Disorder | 2.32 | 1.44 | 3.75 | 2.24 | 1.29 | 3.90 |
| Bipolar Disorder | 3.65 | 2.07 | 6.42 | 2.59 | 1.44 | 4.67 |
| Panic disorder | 3.00 | 1.55 | 5.83 | 1.18 | 0.62 | 2.24 |
| Social Anxiety Disorder | 1.60 | 0.74 | 3.46 | 0.58 | 0.24 | 1.38 |
| Specific Phobia | 2.11 | 1.26 | 3.54 | 1.84 | 1.06 | 3.20 |
| Posttraumatic Stress Disorder | 1.75 | 0.91 | 3.37 | 0.90 | 0.44 | 1.85 |
| Generalized Anxiety Disorder | 3.50 | 1.97 | 6.24 | 1.49 | 0.73 | 3.04 |
| ClusterA | 1.81 | 1.02 | 3.22 | 1.17 | 0.67 | 2.05 |
| ClusterB | 2.49 | 1.52 | 4.06 | 1.76 | 1.04 | 3.00 |
| ClusterC | 1.26 | 0.74 | 2.16 | 0.67 | 0.38 | 1.18 |
Data from NESARC.
Significant results are in bold.
Adjusted HR is adjusted for sex, race, nativity, age at prescription opioid use disorder onset, education years, marital status, and comorbid disorders.
Time-varying variable. (ref)= reference group.
4. DISCUSSION
In a large and nationally representative sample of adults, we estimated that 42% of individuals with prescription opioid use disorders sought treatment for their disorder at some time in their lives. Among those who sought treatment, the median delay from disorder onset to first treatment contact was 3.83 years. Having an earlier onset of prescription opioid use disorder and a history of psychiatric comorbidity including bipolar disorder, MDD, specific phobia or a cluster B personality disorder predicted shorter treatment delays to first treatment contact for prescription opioid use disorder.
We found that the lifetime cumulative probability of treatment-seeking was 42%. Furthermore, 11% of individuals with prescription opioid use disorder sought treatment during the first year after the onset of the disorder and 24% within 10 years following the onset of the disorder. Because our study is the first one to examine the cumulative probability of treatment-seeking among individuals with prescription opioid use disorder, it is not possible to compare our estimates with those of similar studies. However, our results suggest that treatment-seeking rates are low compared to rates for other mental disorders, including to other substance use disorders. For example, Kessler et al. (2001) found that 72% of respondents with lifetime substance use disorders at some point had sought treatment for their symptoms. The NCS-R further revealed that the lifetime cumulative probabilities of treatment-seeking were lower for alcohol abuse (52.7%) dependence (57.0%) and drug abuse (69.8%) dependence (76.9%), than for mood disorders (90.8%; Wang et al., 2005). However, median delay to treatment was shorter than the median treatment delay (6.5 years) documented for substance use disorders in the National Comorbidity Survey Replication (Wang et al., 2005)
The comparatively low treatment rates among individuals with substance use disorders may be due to low perceived need of treatment (Mojtabai et al., 2002), ambivalence about the benefits of treatment (Mojtabai et al., 2002; Wang et al., 2005) and rewarding effects of the drugs themselves. The reasons for the particularly low treatment rates for prescription opioid use disorder are unknown, but may be related to prescription drugs being perceived as less dangerous than illegal drugs or to people's concern that discussing concerns about potential prescription drug misuse with their doctor may endanger future prescriptions. The shorter delay to treatment may also be related to their easier access to the health care system as compared with individuals with other substance use disorders. Regardless of the reason, the strong association between medical and non-medical prescription drug use (Fenton et al., 2010) coupled with our findings, suggests that individuals who are prescribed opioids should be periodically and systematically screened for prescription opioid use disorders. In addition, increasing rates of death from overdose of prescription opioids in the US (Bohnert et al., 2011) suggest that physicians should educate patients and their families about the dangers of toxic ingestions from recreational use of opioids, the dangers of drug interaction with alcohol and benzodiazepines, and the importance of keeping medications out of the reach of others. Fortunately, a recent multi-site randomized trial of buprenorphine treatment for prescription opioid use disorder (Weiss et al., 2010) has provided clinicians and patients with new effective ways for treating this disorder.
We also found that several comorbid psychiatric disorders, including MDD, bipolar disorder or specific phobia, increased the probability of treatment-seeking and decreased delays to first-treatment contact for prescription opioid use disorders. MDD and bipolar disorder are each associated with high rates of psychosocial disability, suicidal ideation and attempts (Judd et al., 2005), unemployment (Tse and Walsh, 2001) and increased use of mental health services (Judd et al., 2005), which may contribute to the clinical detection and treatment of a prescription opioid use disorders. The reasons that comorbid specific phobia also increases prescription opioid use disorders treatment seeking are not known, but this finding is consistent with recent results from the World Mental Health Survey suggesting that specific phobia is an important predictor of later-onset internalizing disorders and may be an early-onset marker for further psychopathology (Kessler et al., 2011). It is possible that the impairment associated with specific phobia increases the likelihood of treatment seeking for prescription opioid use disorders.
Cluster B personality disorders (narcissistic, borderline, histrionic, and antisocial) were also associated to shorter delays to treatment. The more emotional (American Psychiatric Association, 2000) and action-oriented pattern behavior (Fossati et al., 2007) associated with these personality disorders may lead to lower tolerance regarding the symptoms derived from the prescription opioid use disorders and higher perceived need for treatment. Cluster B personality disorders have also been associated with greater severity of substance use (Gibbie et al., 2011) which would also increase the objective need for treatment.
A notable finding of this study was that earlier age of onset of prescription opioid use disorder was associated with a shorter delay to treatment, in contrast with findings in other disorders (Kessler et al., 2001; Vaingankar et al., 2012; Wang et al., 2005, 2004). It is possible that this finding is due to greater contact with the health system among individuals with prescription opioid use disorders. It may also be related to lower degrees of perceived stigma associated with prescription opioid use compared to illicit drug use disorders (Subramaniam et al., 2009). Because pain is more common at older ages, young individuals using prescription opioids may also be acutely aware of the unusual pattern of behavior represented by the need to take opioid analgesic medication from a young age. They may also be more concerned than older-onset individuals about the potential for hyperalgesia that may be associated with long-term use of opioids (Angst and Clark, 2006; Chu et al., 2008).
Our findings have clinical and public health implications. From the clinical point of view, our findings highlight the need when prescribing opioids to balance the needs to alleviate pain with the increased risk of substance dependence. Systematic clinical assessments at baseline of known risk factors for prescription opioid use disorder (Huang et al., 2006; Blanco et al., 2007; Martins et al., 2011), use of evidence-based clinical practice guidelines (Manchikanti et al., 2012), periodic reassessment of other treatment options, and use of well-established measures such as the Current Opioid Misuse Measure (COMM; Chou et al., 2009; Meltzer et al., 2011) can all contribute to optimize the use of prescription opioids and minimize their associated risks.
From the public health point of view, there is a need to train clinicians in appropriate use of opioids to avoid underuse, overuse or the possibility of medication diversion. Educating patients and the general public about the short- and long-term risk and benefits of prescription opioids and the need to avoid their use by individuals to whom these medications were not prescribed may also help to decrease the rate adverse events associated with prescription opioids and save lives. The low rate of treatment-seeking documented by this study also indicates the need to facilitate treatment access for those patients. Due to complex management required for many of these patients, a better integration of primary care, mental health and substance abuse treatment seems essential for the appropriate care. Educating clinicians and patients about the medical rather moral nature of prescription opioid use disorder and the availability and efficacy of its treatment may contribute to increase treatment-seeking.
This study has several limitations. First, as in previous studies of time to treatment-seeking, information about health insurance coverage, income, and geographic location for each year of the person's life was not available, which may have led to an overestimate of the effect of some of the predictors included in the study. Second, self-report of health care-seeking may be underreported, due to the stigma associated with mental health problems and treatment (Pickles et al., 1998). Third, disorder onset and past treatment may be recalled as occurring more recently than it actually occurred (Wang et al., 2005), which may have led to an underestimate to the delay for treatment.
Only a minority of individuals with prescription opioid use disorder receives treatment. The growing prevalence of prescription opioid use disorder (Blanco et al., 2007; Howard et al., 2009), and its association with psychosocial impairment (Huang et al., 2006), overdose death (Bohnert et al., 2011), and substantial health care costs, make it desirable to improve the detection of prescription opioid use disorders to facilitate access to treatment and more integrated care.
Acknowledgments
Role of funding sources
Funding/Support: This study is supported by NIH grants DA019606, DA023200, DA023973, MH076051, CA133050 and MH082773 (Dr. Blanco), and the New York State Psychiatric Institute (Dr. Blanco).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Blanco C designed the study and wrote the first draft of the manuscrip, Iza M managed the literature searches and Wang S conducted the statistical analyses. All authors contributed to and have approved the final manuscript.
Conflict of Interest
No conflict declared.
References
- Adamson J, Ben-Shlomo Y, Chaturvedi N, Donovan J. Ethnicity, socioeconomic position and gender--do they affect reported health-care seeking behaviour? Soc. Sci. Med. 2003;57:895–904. doi: 10.1016/s0277-9536(02)00458-6. [DOI] [PubMed] [Google Scholar]
- Alegria M, Canino G, Rios R, Vera M, Calderon J, Rusch D, Ortega AN. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatr. Serv. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Text Revision. Washington, DC: 2000. [Google Scholar]
- Angst MS, Clark JD. Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology. 2006;104:570–587. doi: 10.1097/00000542-200603000-00025. [DOI] [PubMed] [Google Scholar]
- Ballantyne JC. Opioid analgesia: perspectives on right use and utility. Pain Physician. 2007;10:479–491. [PubMed] [Google Scholar]
- Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12:657–667. doi: 10.1111/j.1526-4637.2011.01075.x. [DOI] [PubMed] [Google Scholar]
- Blanco C, Alderson D, Ogburn E, Grant BF, Nunes EV, Hatzenbuehler ML, Hasin DS. Changes in the prevalence of non-medical prescription drug use and drug use disorders in the United States: 1991-1992 and 2001-2002. Drug Alcohol Depend. 2007;90:252–260. doi: 10.1016/j.drugalcdep.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Blanco C, Secades-Villa R, Garcia-Rodriguez O, Labrador-Mendez M, Wang S, Schwartz RP. Probability and predictors of remission from life-time prescription drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Psychiatr. Res. 2012 doi: 10.1016/j.jpsychires.2012.08.019. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305:1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule--Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47:171–185. doi: 10.1016/s0376-8716(97)00088-4. [DOI] [PubMed] [Google Scholar]
- Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, Donovan MI, Fishbain DA, Foley KM, Fudin J, Gilson AM, Kelter A, Mauskop A, O'Connor PG, Passik SD, Pasternak GW, Portenoy RK, Rich BA, Roberts RG, Todd KH, Miaskowski C. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J. Pain. 2009;10:113–130. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu LF, Angst MS, Clark D. Opioid-induced hyperalgesia in humans: molecular mechanisms and clinical considerations. Clin. J. Pain. 2008;24:479–496. doi: 10.1097/AJP.0b013e31816b2f43. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Inciardi JA. Diversion and abuse of methadone prescribed for pain management. JAMA. 2005;293:297–298. doi: 10.1001/jama.293.3.297. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch. Gen. Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend. 2006;81:103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Grant BF, Blaine J, Mavreas V, Pull C, Hasin D, Compton WM, Rubio-Stipec M, Mager D. Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend. 1997;47:195–205. doi: 10.1016/s0376-8716(97)00090-2. [DOI] [PubMed] [Google Scholar]
- Fenton MC, Keyes KM, Martins SS, Hasin DS. The role of a prescription in anxiety medication use, abuse, and dependence. Am. J. Psychiatry. 2010;167:1247–1253. doi: 10.1176/appi.ajp.2010.09081132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossati A, Barratt ES, Borroni S, Villa D, Grazioli F, Maffei C. Impulsivity, aggressiveness, and DSM-IV personality disorders. Psychiatry Res. 2007;149:157–167. doi: 10.1016/j.psychres.2006.03.011. [DOI] [PubMed] [Google Scholar]
- Gibbie TM, Hides LM, Cotton SM, Lubman DI, Aitken C, Hellard M. The relationship between personality disorders and mental health, substance use severity and quality of life among injecting drug users. Med. J. Aust. 2011;195:S16–21. doi: 10.5694/j.1326-5377.2011.tb03260.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol. Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2007a. [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Prevalence, correlates, and disability of personality disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J. Clin. Psychiatry. 2004a;65:948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan KK, Stinson FS. Source and Accuracy Statement for the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. National Institute on Alcohol Abuse and Alcoholism; Bethesda: 2005a. [Google Scholar]
- Grant BF, Kaplan K, Stinson FS. Source and Accuracy Statement: The Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. National Institute on Alcohol Abuse and Alcoholism; Bethesda: 2007b. [Google Scholar]
- Grant BF, Moore T, Shepard J, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) National Institute on Alcohol Abuse and Alcoholism; Bethesda: 2007c. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2004c;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ. Co-occurrence of DSM-IV personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Compr. Psychiatry. 2005;46:1–5. doi: 10.1016/j.comppsych.2004.07.019. [DOI] [PubMed] [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Howard MM, Weiler RM, Haddox JD. Development and reliability of items measuring the nonmedical use of prescription drugs for the Youth Risk Behavior Survey: results from an initial pilot test. J. School Health. 2009;79:554–560. doi: 10.1111/j.1746-1561.2009.00448.x. [DOI] [PubMed] [Google Scholar]
- Huang B, Dawson DA, Stinson FS, Hasin DS, Ruan WJ, Saha TD, Smith SM, Goldstein RB, Grant BF. Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: Results of the National Epidemiologic Survey on Alcohol and Related Conditions. J. Clin. Psychiatry. 2006;67:1062–1073. doi: 10.4088/jcp.v67n0708. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, Endicott J, Leon AC, Solomon DA, Coryell W, Maser JD, Keller MB. Psychosocial disability in the course of bipolar I and II disorders: a prospective, comparative, longitudinal study. Arch. Gen. Psychiatry. 2005;62:1322–1330. doi: 10.1001/archpsyc.62.12.1322. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Berglund PA, Caraveo-Anduaga JJ, DeWit DJ, Greenfield SF, Kolody B, Olfson M, Vega WA. Patterns and predictors of treatment seeking after onset of a substance use disorder. Arch. Gen. Psychiatry. 2001;58:1065–1071. doi: 10.1001/archpsyc.58.11.1065. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Olfson M, Berglund PA. Patterns and predictors of treatment contact after first onset of psychiatric disorders. Am. J. Psychiatry. 1998;155:62–69. doi: 10.1176/ajp.155.1.62. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Stein DJ, Zaslavsky AM, Aguilar-Gaxiola S, Alonso J, Andrade L, Benjet C, de Girolamo G, de Graaf R, Demyttenaere K, Fayyad J, Haro JM, Hu C, Karam A, Lee S, Lepine JP, Matchsinger H, Mihaescu-Pintia C, Posada-Villa J, Sagar R, Ustun TB. Development of lifetime comorbidity in the World Health Organization World Mental Health Surveys. Arch. Gen. Psychiatry. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirana PS, Rosen R, Hatzichristou D. Subjective well-being as a determinant of individuals’ responses to symptoms: a biopsychosocial perspective. Int. J. Clin. Pract. 2009;63:1435–1445. doi: 10.1111/j.1742-1241.2009.02183.x. [DOI] [PubMed] [Google Scholar]
- Kuehn BM. Scientists, officials eye tools aimed at combating abuse of painkillers. JAMA. 2012;307:19–21. doi: 10.1001/jama.2011.1900. [DOI] [PubMed] [Google Scholar]
- Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, Blanco C. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011a;106:657–669. doi: 10.1111/j.1360-0443.2010.03194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Quintero C, Perez de los Cobos J, Hasin DS, Okuda M, Wang S, Grant BF, Blanco C. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug Alcohol Depend. 2011b;115:120–130. doi: 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, Brown KR, Bruel BM, Bryce DA, Burks PA, Burton AW, Calodney AK, Caraway DL, Cash KA, Christo PJ, Damron KS, Datta S, Deer TR, Diwan S, Eriator I, Falco FJ, Fellows B, Geffert S, Gharibo CG, Glaser SE, Grider JS, Hameed H, Hameed M, Hansen H, Harned ME, Hayek SM, Helm S, 2nd, Hirsch JA, Janata JW, Kaye AD, Kaye AM, Kloth DS, Koyyalagunta D, Lee M, Malla Y, Manchikanti KN, McManus CD, Pampati V, Parr AT, Pasupuleti R, Patel VB, Sehgal N, Silverman SM, Singh V, Smith HS, Snook LT, Solanki DR, Tracy DH, Vallejo R, Wargo BW. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: part 2--guidance. Pain Physician. 2012;15:S67–116. [PubMed] [Google Scholar]
- Martins SS, Fenton MC, Keyes KM, Blanco C, Zhu H, Storr CL. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol. Med. 2012;42:1261–1272. doi: 10.1017/S0033291711002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE. Correlates of nonmedical use of prescription benzodiazepine anxiolytics: results from a national survey of U.S. college students. Drug Alcohol Depend. 2005;79:53–62. doi: 10.1016/j.drugalcdep.2004.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer EC, Rybin D, Saitz R, Samet JH, Schwartz SL, Butler SF, Liebschutz JM. Identifying prescription opioid use disorder in primary care: diagnostic characteristics of the Current Opioid Misuse Measure (COMM). Pain. 2011;152:397–402. doi: 10.1016/j.pain.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch. Gen. Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Olfson M, Kessler RC, Berglund PA, Lin E. Psychiatric disorder onset and first treatment contact in the United States and Ontario. Am. J. Psychiatry. 1998;155:1415–1422. doi: 10.1176/ajp.155.10.1415. [DOI] [PubMed] [Google Scholar]
- Olfson M, Liu SM, Grant BF, Blanco C. Influence of comorbid mental disorders on time to seeking treatment for major depressive disorder. Med. Care. 2012;50:227–232. doi: 10.1097/MLR.0b013e318241eb5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perron BE, Mowbray OP, Glass JE, Delva J, Vaughn MG, Howard MO. Differences in service utilization and barriers among Blacks, Hispanics, and Whites with drug use disorders. Subst. Abuse Treat. Prev. Policy. 2009;4:3. doi: 10.1186/1747-597X-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickles A, Pickering K, Simonoff E, Silberg J, Meyer J, Maes H. Genetic “clocks” and “soft” events: a twin model for pubertal development and other recalled sequences of developmental milestones, transitions, or ages at onset. Behav. Genet. 1998;28:243–253. doi: 10.1023/a:1021615228995. [DOI] [PubMed] [Google Scholar]
- Rigg KK, Ibanez GE. Motivations for non-medical prescription drug use: a mixed methods analysis. J. Subst. Abuse Treat. 39:236–247. doi: 10.1016/j.jsat.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogler LH, Cortes DE. Help-seeking pathways: a unifying concept in mental health care. Am. J. Psychiatry. 1993;150:554–561. doi: 10.1176/ajp.150.4.554. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam GA, Stitzer MA. Clinical characteristics of treatment-seeking prescription opioid versus heroin using adolescents with opioid use disorder. Drug Alcohol Depend. 2009;101:13–19. doi: 10.1016/j.drugalcdep.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trescot AM, Boswell MV, Atluri SL, Hansen HC, Deer TR, Abdi S, Jasper JF, Singh V, Jordan AE, Johnson BW, Cicala RS, Dunbar EE, Helm S, 2nd, Varley KG, Suchdev PK, Swicegood JR, Calodney AK, Ogoke BA, Minore WS, Manchikanti L. Opioid guidelines in the management of chronic non-cancer pain. Pain Physician. 2006;9:1–39. [PubMed] [Google Scholar]
- Trescot AM, Helm S, Hansen H, Benyamin R, Glaser SE, Adlaka R, Patel S, Manchikanti L. Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians’ (ASIPP) Guidelines. Pain Physician. 2008;11:S5–S62. [PubMed] [Google Scholar]
- Tse SS, Walsh AE. How does work work for people with bipolar affective disorder? Occup. Ther. Int. 2001;8:210–225. doi: 10.1002/oti.147. [DOI] [PubMed] [Google Scholar]
- Vaingankar JA, Rekhi G, Subramaniam M, Abdin E, Chong SA. Age of onset of life-time mental disorders and treatment contact. Soc. Psychiatr Epidemiol. 2012 doi: 10.1007/s00127-012-0601-y. in press. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund PA, Olfson M, Kessler RC. Delays in initial treatment contact after first onset of a mental disorder. Health Serv. Res. 2004;39:393–415. doi: 10.1111/j.1475-6773.2004.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Potter JS, Provost SE, Huang Z, Jacobs P, Hasson A, Lindblad R, Connery HS, Prather K, Ling W. A multi-site, two-phase, Prescription Opioid Addiction Treatment Study (POATS): rationale, design, and methodology. Contemp. Clin. Trials. 2010;31:189–199. doi: 10.1016/j.cct.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AG, Birnbaum HG, Mareva MN, Daher M, Vallow S, Schein J, Katz N. Direct costs of opioid abuse in an insured population in the United States. J. Manag. Care Pharm. 2005;11:469–479. doi: 10.18553/jmcp.2005.11.6.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: position statement. Drug Alcohol Depend. 2003;69:215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]


