Abstract
Aim
The aim of this study was to assess the prevalence and patterns of exposure to antidepressants before, during and after pregnancy in a cohort including all pregnant women in Denmark between 1997 and 2010.
Methods
We performed a retrospective cohort study including 912 322 pregnancies. Information was retrieved from the Danish Birth Registry and The Register of Medicinal Product Statistics to identify women redeeming an antidepressant prescription during pregnancy. Exposure periods were based on standard treatment doses and dispensed pack sizes.
Results
We identified 19 740 pregnancies exposed to an antidepressant at some point during pregnancy. The rate of exposure increased from 0.2% in 1997 to 3.2% in 2010. We found that the rate of exposure was halved during the first 3 months of pregnancy. In contrast, we describe a clear increase in exposure after pregnancy among pre-delivery treatment-naïve women.
Conclusions
In spite of uncertainty concerning antidepressants’ safety during pregnancy we find a 16-fold increase in exposure rates between 1997 and 2010. The rates describe a sharp decrease in exposure during pregnancy that is probably caused by physicians’ hesitation to prescribe antidepressants and women’s fear of unwanted effects on the unborn child. More studies are needed to clarify the consequences of antidepressant discontinuation during pregnancy.
Introduction
It is estimated that approximately 20% of women of childbearing age (25–45 years), [1], [2] and up to 15% of pregnant women suffer from depressive symptoms [3], [4]. Untreated depression can have serious consequences for the mother, the newly born and their family. Depression during pregnancy is associated with preterm delivery, low birth weight, epidural analgesia, caesarean section, intensive ward admission, and disturbances in the child’s neurocognitive and socioemotional development [4]–[8]. Untreated depression during pregnancy is associated with a 6-fold risk increase of postpartum depression [4], [9].
Research dealing with the consumption of antidepressants and subsequent pregnancy outcomes has indicated an increased risk of congenital malformations, and more notably heart defects [10]–[22]. However, the results are conflicting [12], [14], [17]–[19], [23]–[33] and studies including up to a million pregnancies indicate little risk of congenital malformations [12], [17], [19], [31], [32], or the possibility of confounding by indication [34]. On the other hand, studies show a clear association between SSRI use and persistent pulmonary hypertension of the newborn [35], and no association with perinatal mortality [36], [37].
It is important to know the prevalence of prenatal exposure to antidepressants in order to estimate its potential public health consequences. Therefore, we set out to quantify the percentage of pregnant women in treatment with antidepressants in Denmark. We assessed temporal trends over the years 1997–2010, and use in relation to pregnancy. Additionally, we looked at maternal characteristics associated with antidepressant exposure.
Materials and Methods
We identified all pregnant women exposed to an antidepressant in Denmark between 1997 and 2010 using the Danish Medical Birth Registry and the Register of Medicinal Product Statistics.
Study Population
The study population comprised all women giving birth in Denmark between 1st January, 1997 and 1st January, 2010 (n = 920 639). All citizens in Denmark have a unique personal civil registration number that enables individual-level linkage of information across nationwide registries [38]. Linkage between three of these registries was used in the present study. All births between 1997 and 2010 were identified using the Danish Medical Birth Registry, which contains a unique identification number for the mother, father and child, age and prior births as well as birth length, death and cause of death, sex and gestational age of the offspring [39]. Time of conception is based on ultrasound estimates or information on the date of the last menstrual period. Data on all hospitalizations was retrieved from The Danish National Hospital Register [40]. The registry includes admission and discharge dates, and hospitalization discharge diagnoses coded according to the International Classification of Diseases, 10th revision (ICD-10). The Register of Medicinal Product Statistics was used to draw information on every prescription dispensed from Danish pharmacies since 1997 [41]. Registered information includes type of drug, strength, quantity dispensed, and dispense dates. The international Anatomical Therapeutic Chemical (ATC) classification system was used to code all antidepressants. Danish pharmacies are required to register all dispensed prescriptions as part of the national healthcare reimbursement scheme for drug expenses. This ensures high rates of registration [42].
Subjects were divided into quartiles according to their annual household gross income during the year of birth. Education was divided into three groups according to the highest obtained level of education.
Information on smoking and body mass index (BMI) was obtained from the Danish Medical Birth Registry Smoking was divided into five classes according to the number of daily cigarettes: no smoking, 1–10, 11–20, and >20. Information on BMI was only available from 1st January 2004, and divided into 4 classes according to kg/m2: <18.5, 18.5–24.9, 25.0–29.9, and >29.9.
Identification of Antidepressant Pharmacotherapy
Patients being treated with antidepressants were included if they claimed one of the antidepressants listed in table 1. The following antidepressants were not included in our study due to low exposure rates (n<10): nefazodone (N06AX06), ruboxetine (N06AX18), duloxetine (N06AX21), moclobemid (N06AG02), doxepin (N06AA12). Bupropion (N06AX12) was not included since its indication in Denmark is smoking cessation. We allowed for exposure to multiple antidepressants.
Table 1. Antidepressants included in the study.
| Antidepressant | ATC code |
| SSRIs | N06AB |
| Citalopram | N06AB04 |
| Escitalopram | N06AB10 |
| Fluvoxamine | N06AB08 |
| Fluoxetine | N06AB03 |
| Paroxetine | N06AB05 |
| Sertraline | N06AB06 |
| TCAs | N06AA |
| Amitriptylin | N06AA09 |
| Clomipramin | N06AA04 |
| Dosulepin | N06AA16 |
| Imipramin | N06AA02 |
| Nortriptylin | N06AA09 |
| Other | N06AX |
| Mianserin | N06AX03 |
| Mirtazapine | N06AX11 |
| Venlafaxine | N06AX16 |
Table shows the generic names and their corresponding ATC codes for antidepressants included in the present study. SSRI: Selective Serotonine Reuptake Inhibitor; TCA: Tri Cyclic Antidepressant (Non-selective Monoamine Reuptake Inhibitor).
To estimate exposure prevalence we calculated dosages for each individual in the cohort, based on dispense date of each prescription, strength and number of tablets prescribed. For each prescription, we calculated an exposure period based on the average dosage of up to seven previous consecutive prescriptions. If the prescription was the first in a series, we calculated exposure time by using the standard daily dose for the drug. The standard daily dose was selected for each available medication strength in accordance with the accepted standard daily therapeutic dose [43]. The number of dispensed pills was divided by the daily dosage to calculate treatment periods. We assumed a treatment period to be continuous, for a series of prescriptions, if this was compatible with at least the minimal dose of the prescribed tablets (i.e. one daily tablet). We defined treatment breaks shorter than 60 days as being in treatment. This was done to take subjects with lower daily dosages than anticipated into account. We chose 60 days á priori, because it seemed a reasonable amount of days to account for subjects decreasing dosage for a period of time or using stored medication. To ensure that the a priori period of 60 days was reasonable, we estimated exposure prevalence with treatment breaks of 30 or 90 days as being in treatment. The estimates did not differ. We assumed treatment periods to continue during hospitalization. We have previously used this method to calculate treatment periods during pregnancy [34], [36].
We defined exposure to antidepressants during a given period as presence of one or more days of treatment. If treatment extended over two or more periods (i.e. two trimesters), exposure was considered to have occurred in all affected periods.
Ethics
Registries were linked and personal data analysed on computers held by Statistics Denmark, where data was made available with encrypted personal information [43]. This ensured that no individuals could be identified. In Denmark The Act on Processing of Personal Data does not require ethical permission or obtained written informed consent for anonymised retrospective registry studies. The present study has been approved by The Danish Data Protection Agency (No. 2008-41-2517).
Statistical Analysis
All analyses and data management were performed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
We used frequencies and percentage to present baseline characteristics. To assess differences in baseline characteristics for categorical variables we used chi-square tests. Statistical significance was defined as p<0.05. All statistical tests were two sided.
Results
Material Overview
We identified 912 322 pregnancies resulting in a birth between 1997 and 2010, of which 19 740 were exposed to an antidepressant at some point during pregnancy. Table 2 shows the number and basic characteristics of pregnant women treated with antidepressants divided into 3 categories according to exposure at any time during pregnancy: SSRI (n = 16 928), TCA (n = 1 297) and other antidepressants (n = 3 135).
Table 2. Basic characteristics for women exposed to an antidepressant during pregnancy.
| SSRI | TCA | Others | Any AD | No exposure | ||
| (N = 16 928) | (N = 1297) | (N = 3135) | (N = 19740) | (N = 892582) | ||
| Characteristic | n (%) | n (%) | n (%) | n (%) | n (%) | p-value |
| Education | <0.001 | |||||
| Unskilled | 7645 (45.16) | 557 (42.95) | 1572 (50.14) | 8991 (45.55) | 291155 (32.62) | |
| Skilled | 4524 (26.72) | 393 (30.30) | 818 (26.09) | 5287 (26.78) | 265794 (29.78) | |
| Higher | 4345 (25.67) | 312 (24.06) | 647 (20.64) | 4950 (25.08) | 295149 (33.07) | |
| Missing values | 414 (2.45) | 35 (2.70) | 98 (3.13) | 512 (2.59) | 40484 (4.54) | |
| Annual household income | <0.001 | |||||
| Less than $ 62 192 | 6174 (36.47) | 402 (30.99) | 1315 (41.95) | 7248 (36.72) | 216452 (24.25) | |
| $ 62 192–$ 89 140 | 4313 (25.48) | 405 (31.23) | 836 (26.67) | 5081 (25.74) | 218620 (24.49) | |
| $ 89 141–$ 126 344 | 3290 (19.44) | 244 (18.81) | 510 (16.27) | 3768 (19.09) | 219935 (24.64) | |
| $ 126 345 or greater | 2816 (16.64) | 225 (17.35) | 391 (12.47) | 3215 (16.29) | 220490 (24.70) | |
| Missing values | 335 (1.98) | 21 (1.62) | 92 (2.93) | 428 (2.17) | 1785 (0.20) | |
| Age (years) | <0.001 | |||||
| <20 | 530 (3.13) | 15 (1.16) | 97 (3.09) | 599 (3.03) | 24447 (2.74) | |
| 21–25 | 2748 (16.23) | 163 (12.57) | 538 (17.16) | 3185 (16.13) | 135330 (15.16) | |
| 26–30 | 5486 (32.41) | 374 (28.84) | 995 (31.74) | 6338 (32.11) | 335476 (37.58) | |
| 31–35 | 5396 (31.88) | 441 (34.00) | 963 (30.72) | 6308 (31.96) | 286027 (32.04) | |
| >35 | 2768 (16.35) | 304 (23.44) | 542 (17.29) | 3310 (16.77) | 111302 (12.47) | |
| Missing values | 0 (−) | 0 (−) | 0 (−) | 0 (−) | 0 (−) | |
| Parity | <0.001 | |||||
| 1 | 7430 (43.89) | 497 (38.32) | 1397 (44.56) | 8646 (43.8) | 389794 (43.67) | |
| 2 | 5483 (32.39) | 386 (29.76) | 860 (27.43) | 6255 (31.69) | 327381 (36.68) | |
| >2 | 3858 (22.79) | 402 (30.99) | 849 (27.08) | 4658 (23.6) | 169875 (19.03) | |
| Missing values | 157 (0.93) | 12 (0.93) | 29 (0.93) | 181 (0.92) | 5532 (0.62) | |
| Daily cigarettes | <0.001 | |||||
| 0 | 11147 (65.85) | 859 (66.23) | 1869 (59.62) | 12890 (65.3) | 705637 (79.06) | |
| 1–10 | 4245 (25.08) | 315 (24.29) | 937 (29.89) | 5043 (25.55) | 130280 (14.60) | |
| 11–20 | 294 (1.74) | 19 (1.46) | 71 (2.26) | 350 (1.77) | 5240 (0.59) | |
| >20 | 680 (4.02) | 47 (3.62) | 138 (4.40) | 793 (4.02) | 22269 (2.49) | |
| Missing values | 562 (3.33) | 57 (4.39) | 120 (3.83) | 664 (3.37) | 29156 (3.27) | |
| BMI (kg/m2) | <0.001 | |||||
| <18.5 | 811 (4.79) | 34 (2.62) | 154 (4.91) | 932 (4.72) | 27743 (3.11) | |
| 18.5–24.9 | 6279 (37.09) | 361 (27.83) | 1156 (36.87) | 7202 (36.48) | 247064 (27.68) | |
| 25.0–29.9 | 2678 (15.82) | 187 (14.42) | 574 (18.31) | 3123 (15.82) | 85611 (9.59) | |
| 30 | 2078 (12.28) | 153 (11.80) | 435 (13.88) | 2414 (12.23) | 47632 (5.34) | |
| Missing values | 5082 (30.02) | 562 (43.33) | 816 (26.03) | 6069 (30.74) | 484532 (54.28) |
Table shows the number (n) of pregnant women within each subcategory. Some women were exposed to several antidepressants during pregnancy. Number in parenthesis denotes percentage of pregnant women within each exposure. Information on BMI was only available for women giving birth after 1 January 2004. Chi-square tests were used to assess the overall p value for the group comparison between unexposed and women exposed to “any AD”.BMI, body mass index; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressants; AD, antidepressant.
Maternal Characteristics
Pregnant women treated with antidepressants were characterized by being older, having more prior pregnancies, having lower annual household income, having a shorter educational career, smoking more and having a higher BMI than unexposed women (table 2).
Exposure Rates, 1997–2010
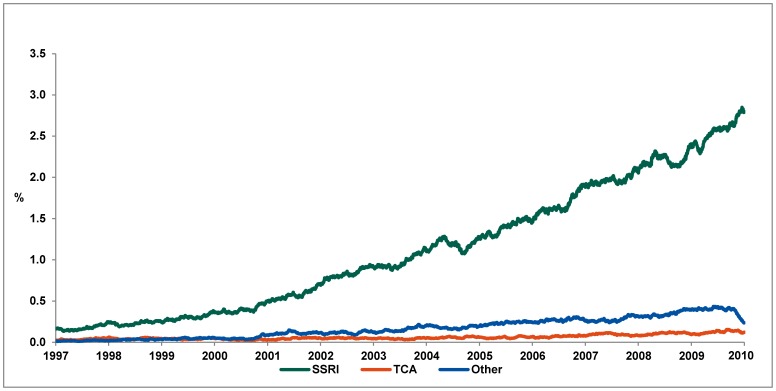
Between January 1997 and January 2010 the percentage of pregnant women exposed to an antidepressant increased from 0.2% in early 1997 to 3.2% in December 2009 (figure 1). This 16-fold increase was sustained by the increase in exposure to SSRIs that accounted for 88.7% of exposure among pregnant women in December 2009. TCAs and other antidepressants accounted for 3.8% and 7.5% respectively.
Figure 1. Point prevalence of pregnant women in treatment with an antidepressant based on estimated treatment periods.
SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressants; AD, antidepressant.
For the specific SSRIs we see a change in choice of treatment between 1997 and 2009. In 1997, Citalopram (48.6%) and Fluoxetine (31.9%) were the preferred SSRIs during pregnancy, followed by Sertraline (9.7%) and Paroxetine (9.7%). In 2002 34.0% of pregnancies were exposed to fluoxetine, 26.9% to citalopram, 20.3% to sertraline, 18.5% to paroxetine and 0.3% to escitalopram. In December 2009 the prevalence changed; fluoxetine (15.7%), citalopram (47.4%), sertraline (26.8%), paroxetine (1.8%) and escitalopram (8.2%).
The prevalence of exposure to TCAs remained steady since 1997 at an average of 0.03% of pregnancies. Amitriptyline and nortriptyline represented over 70% of TCA exposure.
Exposure to other antidepressants increased in the study period reaching a maximum peak point prevalence of 0.4% of pregnant women in August 2009. We observed an abrupt fall in prevalence at the end of 2009. The most common exposure among other antidepressants was venlafaxine, with 63.0% of total exposure in the study period, followed by mirtazapine (19.8%) and mianserin (7.0%).
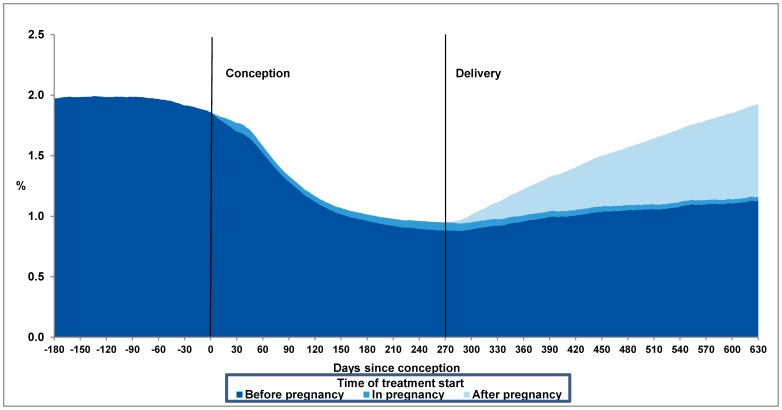
Exposure in Relation to Pregnancy
At the time of conception, 16 962 (1.86%) of all pregnancies were exposed to an antidepressant, of these, 51% were still exposed at the time of delivery. The greatest decrease in antidepressant exposure is consistent with the period of pregnancy recognition (1–3 months after conception) (figure 2). Table 3 shows the number of exposed women during each trimester. 1694 (0.19%) pre-pregnancy treatment naïve women commenced treatment with an antidepressant at some point during pregnancy. Within the first six months after delivery 5 053 (0.55%) commenced treatment among women who had never been in treatment with an antidepressant before the time of delivery. Within 12 months the number had risen to 11 151 (1.22%) (table 4). In contrast to women exposed to antidepressants during pregnancy, these women were younger than unexposed women (p<0.001). They have however, a lower annual household income, a shorter educational career, smoke more and have a higher BMI than unexposed women (p<0.001). Figure 2 shows exposure prevalence to any antidepressant before, during and after pregnancy for all pregnancies in the cohort.
Figure 2. Percentage of pregnant women in treatment with an antidepressant for each day from 180 days before conception to 630 days after conception (approximately 1 year after mean time of delivery).
The figure is divided into three areas of different color indicating the period of treatment start; before (dark blue), during (blue) or after pregnancy (light blue).
Table 3. Number of women exposed to an antidepressant during pregnancy.
| Trimester | |||
| First | Second | Third | |
| Any antidepressant | 18273 | 13039 | 9721 |
| SSRI | 15403 (84.29) | 11370 (87.20) | 8641 (88.89) |
| Citalopram | 6657 (36.43) | 4306 (33.02) | 2850 (29.32) |
| Escitalopram | 1539 (8.42) | 722 (5.54) | 344 (3.54) |
| Fluoxetine | 3898 (21.33) | 3618 (27.75) | 2927 (30.11) |
| Paroxetine | 1779 (9.74) | 1164 (8.93) | 816 (8.39) |
| Sertraline | 3059 (16.74) | 2565 (19.67) | 2328 (23.95) |
| TCA | 1101 (6.03) | 748 (5.74) | 479 (4.93) |
| Amitriptyline | 578 (3.16) | 292 (2.24) | 120 (1.23) |
| Clomipramin | 125 (0.68) | 89 (0.68) | 57 (0.59) |
| Dosulepin | 40 (0.22) | 42 (0.32) | 36 (0.37) |
| Imipramin | 61 (0.33) | 32 (0.25) | 15 (0.15) |
| Nortriptyiline | 327 (1.79) | 308 (2.36) | 254 (2.61) |
| Other | 3039 (16.63) | 1655 (12.69) | 934 (9.61) |
| Mianserin | 270 (1.48) | 113 (0.87) | 57 (0.59) |
| Mirtazapine | 876 (4.79) | 348 (2.67) | 142 (1.46) |
| Venlafaxine | 1687 (9.23) | 1109 (8.51) | 703 (7.23) |
Number in parenthesis is the percentage of ‘any antidepressant’. Sum of percentages adds up to more than 100% due to some pregnancies being exposed to more than one antidepressant in the given period. SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressants; AD, antidepressant.
Table 4. Pre-pregnancy treatment-naïve women exposed to an antidepressant.
| Start during pregnancy | Start after pregnancy | ||
| 0–6 months | 0–12 months | ||
| Any antidepressant | 1694 | 5053 | 11151 |
| SSRI | 1416 (83.59) | 4246 (0.47) | 9304 (1.02) |
| Citalopram | 489 (28.87) | 1936 (0.21) | 4588 (0.50) |
| Escitalopram | 78 (4.60) | 495 (0.05) | 1235 (0.14) |
| Fluoxetine | 499 (29.46) | 367 (0.04) | 825 (0.09) |
| Paroxetine | 107 (6.32) | 487 (0.05) | 1083 (0.12) |
| Sertraline | 363 (21.43) | 1130 (0.12) | 2167 (0.24) |
| TCA | 155 (9.15) | 265 (0.03) | 704 (0.08) |
| Amitriptyline | 71 (4.19) | 136 (0.01) | 426 (0.05) |
| Clomipramin | 9 (0.53) | 18 (0.00) | 48 (0.01) |
| Dosulepin | 10 (0.59) | 10 (0.00) | 25 (0.00) |
| Imipramin | 20 (1.18) | 22 (0.00) | 62 (0.01) |
| Nortriptyiline | 48 (2.83) | 93 (0.01) | 188 (0.02) |
| Other | 183 (10.80) | 901 (0.10) | 2295 (0.25) |
| Mianserin | 28 (1.65) | 136 (0.01) | 348 (0.04) |
| Mirtazapine | 108 (6.38) | 513 (0.06) | 1191 (0.13) |
| Venlafaxine | 45 (2.66) | 263 (0.03) | 800 (0.09) |
Number of pre-pregnancy treatment-naive women exposed to an antidepressant during and after pregnancy. Number in parenthesis is the percentage of ‘any antidepressant’. Sum of percentages adds up to more than 100% due to some pregnancies being exposed to more than one antidepressant in the given period. SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressants; AD, antidepressant.
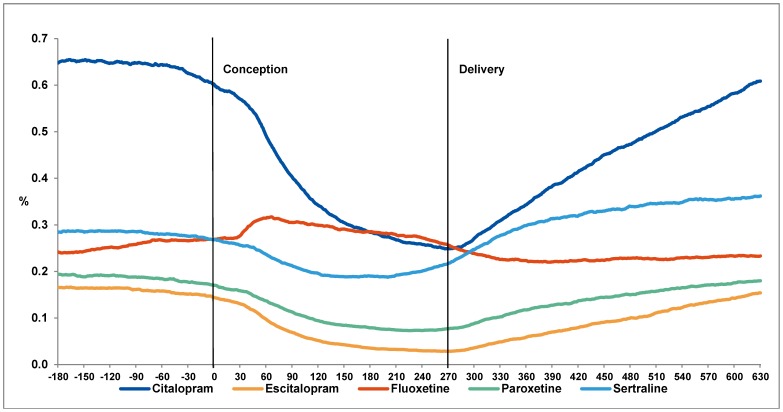
This pattern of exposure from 6 months before to 12 months after pregnancy was similar for the individual antidepressants, except for fluoxetine (figure 3). For fluoxetine, we saw a rise in prevalence after conception followed by a slight decrease until delivery.
Figure 3. Percentage of pregnant women in treatment with an SSRI for each day from 180 days before conception to 630 days after conception (approximately 1 year after mean time of delivery).
Lines depict the different types of SSRIs.
Exposure to more than one antidepressant
We identified 3388 (0.37%) pregnancies exposed to more than one antidepressant during pregnancy; 2995 to two, 364 to three and 29 to four different antidepressants.
We identified 1 629 (0.18%) pregnancies exposed to two SSRIs at some time during pregnancy. The most frequently used combinations during pregnancy were fluoxetine and citalopram (n = 663), and fluoxetine and sertraline (n = 554). We identified 62 pregnancies exposed to mirtazapine and venlafaxine among pregnancies exposed to other antidepressants, but no pregnancies exposed to two TCA’s during pregnancy.
Antidepressant switch during pregnancy
While 43.3% (n = 8552) stopped antidepressant treatment during pregnancy, 11.3% (n = 2224) of pregnant women switched to a different antidepressant; 6.8% during the first trimester and 4.5% during the second trimester. Among those who switched treatment, the preferred new antidepressant was fluoxetine (41.7%) followed by citalopram (20.5%) and sertraline (19.1%).
Few pregnant women switched antidepressant from fluoxetine (6%), sertraline (6%) or citalopram (8%), compared to mianserin (42%), escitalopram (25%) or mirtazapine (26%).
Discussion
We have described patterns of exposure to specific antidepressant among all pregnant women in Denmark between 1997 and 2010. We found an increase in prevalence of exposure during the study period from 0.2% to 3.2%. Furthermore we described a decrease in exposure to antidepressants related to the time of pregnancy recognition, and a steep increase in exposure among pre-pregnancy treatment-naïve after delivery.
Exposure Rates, 1997–2010
The increase in prevalence over the years is comparable to studies from other countries, although our estimates are considerably lower [44]–[49]. Two studies from the USA describe prevalences of 7.6% in 2005 [45] and 13.3% in 2003 [47]. Two studies from The Netherlands reported prevalences of 2% between 2000 and 2003c and 3% in 2004 [46]. The first three studies were based on health insurance records and the fourth on data from a Dutch region. One study from the UK estimated a prevalence of 3.3% in 2006, based on data from general practices [49]. None of the mentioned studies were based on nation-wide cohorts as the present study. Differences in prevalence could be accounted for by study methodology, and socio-demographic differences.
The increasing exposure to antidepressant during pregnancy until 2010 was mainly due to redemption of SSRIs, where citalopram was the most frequently used SSRI in 2009. Use of paroxetine has stagnated since 2004, and accounted for only 5.3% of SSRI use in 2008 (figure 2), and could be due to reports published in 2005 by the FDA associating paroxetine with heart defects [50]. Use of TCAs and other antidepressants increased at a more moderate rate between 1997 and 2010.
One possible reason for this increase over the last 13 years is the widening of the therapeutic indications for antidepressants to include anxiety disorders, premenstrual syndrome, posttraumatic stress disorders, migraine prophylaxis, pain and eating disorders [51]. We hypothesize that a second reason could be a more liberal prescription of antidepressants during pregnancy. In spite of many studies reporting increased risks of congenital malformations associated with antidepressants, the absolute risk increases are low. On the other hand, in spite of doctor recommendation, only 35% of pregnant women reported to be willing to take antidepressants during pregnancy in an American study [52]. Thirdly, it has been suggested that influence by the pharmaceutical industry could play a role in the increased use of antidepressants during pregnancy [53].
Increased rates of exposure to some newer antidepressants (e.g. escitalopram) will open for the possibility of safety studies on these drugs and their possible association with less frequent pregnancy outcomes (e.g. specific congenital malformations and persistent pulmonary hypertension of the newborn).
Use in Relation to Pregnancy
Overall, at the time of pregnancy recognition we see a considerable decrease in prevalence of SSRI exposure, and an increase after delivery.
Approximately half of all pregnancies discontinued treatment during pregnancy, which is in accordance with previously published literature [46], [49], [54]–[57]. In our study, this decrease was not found for fluoxetine, for which the prevalence increased. This could indicate a switch in treatment to fluoxetine when pregnancy is detected, which is in accordance with recommendations from The Danish Society of Obstetrics and Gynecology (DSOG). DSOG recommends the use of fluoxetine or sertraline during pregnancy [58] which could explain why exposure to sertraline decreased only 26.5% during pregnancy in contrast to citalopram (60.7%), escitalopram (81.4%) and paroxetine (56.0%). During the first year after pregnancy (period of lactation) we see the steepest increase in use for citalopram (figure 3), which is not in accordance with DSOGs guidelines for treatment during lactation. During lactation DSOG recommends the use sertraline or paroxetine [58].
During pregnancy only 1694 (0.19%) treatment-naïve women commenced use of an antidepressant. This could indicate physicians and women’s reluctance towards starting treatment during pregnancy, unless symptoms are severe. It is of note that most of these women continued treatment at least one year after delivery (figure 2).
Pregnancy does not seem to protect against the risk of depression relapse [59]. Discontinuation of antidepressant treatment during pregnancy is associated with a 5-fold increase in the risk of relapse of depression during pregnancy compared to women who maintained their medication [60] and is estimated to create a substantial economic burden on society due to added use of the health care system by mother and child [61]. The cause of discontinuation could be fear of harm to the fetus or physicians’ recommendations [62]. In our study, 27% of women discontinuing treatment during pregnancy resumed treatment within one year after delivery. This could indicate a low rate of relapse in our Danish cohort comprising antidepressant users without information on depression severity. On the other hand, only 1.25% of treatment-naïve women commenced antidepressant treatment during the first year after delivery.
Strengths and Limitations
We had no information on compliance or the women’s intention of commencing a treatment shortly after redemption of an antidepressant. This could lead to an overestimation of treatment periods. However, a Dutch study estimated that the majority of pregnant women redeeming a prescription take their medication [63]. A small Danish study estimated that compliance in Denmark is 80% for antidepressant treatment during pregnancy [64]. We did not have information on women discontinuing their treatment to commence treatment with herbal medications against depression (e.g. St John’s Wort). Importantly, information on drug use for women experiencing a spontaneous or provoked abortion was not available in our databases, and exposure rates during pregnancy could differ from those reported in our study.
The main strength of our study is the completeness of the registries, including nearly all births in Denmark and the mothers’ drug redemptions in the study period. 97.5% of all redeemed prescriptions are included in The Register of Medicinal Product Statistics [42]. All prescriptions recorded in this registry have been redeemed and paid for, which increases the probability of exposure. All redeemed prescriptions in Denmark are, by law, required to be registered as part of the national healthcare reimbursement scheme. Information is recorded prospectively and not based on questionnaires or interviews, which eliminates recall bias. Data gathered from the registries include information on drug-names and quantities redeemed. This information is difficult to obtain through questionnaires or interviews of women who have to remember use of medications over a long period of time [65]–[68].
Although the overall prevalence of antidepressant use through the last 13 years has increased, half of all pregnant women discontinue their use during pregnancy, probably due to uncertainty of the safety of antidepressants. Based on these findings it seems important for women of childbearing age and physicians to have information of high standards to help them in treatment decisions during pregnancy.
Funding Statement
The Research Project was partially sponsored by the Capital Region of Copenhagen and the Danish Agency for Science, Technology and Innovation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Grigoriadis S, Robinson GE (2007) Gender issues in depression. Ann Clin Psychiatry 19: 247–255 787699661 [pii];10.1080/10401230701653294 [doi]. [DOI] [PubMed] [Google Scholar]
- 2. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, et al. (2003) The epidemiology of major depressive disorder - Results from the National Comorbidity Survey Replication (NCS-R). Jama-Journal of the American Medical Association 289: 3095–3105. [DOI] [PubMed] [Google Scholar]
- 3. Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR (2004) Prevalence of depression during pregnancy: systematic review. Obstet Gynecol 103: 698–709 10.1097/01.AOG.0000116689.75396.5f [doi];103/4/698 [pii]. [DOI] [PubMed] [Google Scholar]
- 4. Chatillon O, Even C (2010) [Antepartum depression: Prevalence, diagnosis and treatment.]. Encephale 36: 443–451 S0013-7006(10)00041-2 [pii];10.1016/j.encep.2010.02.004 [doi]. [DOI] [PubMed] [Google Scholar]
- 5. Bonari L, Pinto N, Ahn E, Einarson A, Steiner M, et al. (2004) Perinatal risks of untreated depression during pregnancy. Can J Psychiatry 49: 726–735. [DOI] [PubMed] [Google Scholar]
- 6. Talati A, Wickramaratne PJ, Pilowsky DJ, Alpert JE, Cerda G, et al. (2007) Remission of maternal depression and child symptoms among single mothers: a STAR*D-Child report. Soc Psychiatry Psychiatr Epidemiol 42: 962–971 10.1007/s00127-007-0262-4 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, et al. (2006) Offspring of depressed parents: 20 years later. Am J Psychiatry 163: 1001–1008 163/6/1001 [pii];10.1176/appi.ajp.163.6.1001 [doi]. [DOI] [PubMed] [Google Scholar]
- 8. Chung TKH, Lau TK, Yip ASK, Chiu HFK, Lee DTS (2001) Antepartum Depressive Symptomatology Is Associated With Adverse Obstetric and Neonatal Outcomes. Psychosom Med 63: 830–834. [DOI] [PubMed] [Google Scholar]
- 9. Beck CT, Records K, Rice M (2006) Further development of the Postpartum Depression Predictors Inventory-Revised. J Obstet Gynecol Neonatal Nurs 35: 735–745 JOGN94 [pii];10.1111/j.1552–6909.2006.00094.x [doi]. [DOI] [PubMed] [Google Scholar]
- 10. Alwan S, Reefhuis J, Rasmussen SA, Olney RS, Friedman JM (2007) Use of selective serotonin-reuptake inhibitors in pregnancy and the risk of birth defects. N Engl J Med 356: 2684–2692 356/26/2684 [pii];10.1056/NEJMoa066584 [doi]. [DOI] [PubMed] [Google Scholar]
- 11. Louik C, Lin AE, Werler MM, Hernandez-Diaz S, Mitchell AA (2007) First-trimester use of selective serotonin-reuptake inhibitors and the risk of birth defects. N Engl J Med 356: 2675–2683 356/26/2675 [pii];10.1056/NEJMoa067407 [doi]. [DOI] [PubMed] [Google Scholar]
- 12. Malm H, Artama M, Gissler M, Ritvanen A (2011) Selective serotonin reuptake inhibitors and risk for major congenital anomalies. Obstet Gynecol 118: 111–120 10.1097/AOG.0b013e318220edcc [doi]. [DOI] [PubMed] [Google Scholar]
- 13. Bakker MK, Kerstjens-Frederikse WS, Buys CH, de Walle HE, de Jong-van den Berg LT (2010) First-trimester use of paroxetine and congenital heart defects: a population-based case-control study. Birth Defects Res A Clin Mol Teratol 88: 94–100 10.1002/bdra.20641 [doi]. [DOI] [PubMed] [Google Scholar]
- 14. Berard A, Ramos E, Rey E, Blais L, St-Andre M, et al. (2007) First trimester exposure to paroxetine and risk of cardiac malformations in infants: the importance of dosage. Birth Defects Res B Dev Reprod Toxicol 80: 18–27 10.1002/bdrb.20099 [doi]. [DOI] [PubMed] [Google Scholar]
- 15. Cole JA, Ephross SA, Cosmatos IS, Walker AM (2007) Paroxetine in the first trimester and the prevalence of congenital malformations. Pharmacoepidemiol Drug Saf 16: 1075–1085 10.1002/pds.1463 [doi]. [DOI] [PubMed] [Google Scholar]
- 16. Diav-Citrin O, Shechtman S, Weinbaum D, Wajnberg R, Avgil M, et al. (2008) Paroxetine and fluoxetine in pregnancy: a prospective, multicentre, controlled, observational study. Br J Clin Pharmacol 66: 695–705 BCP3261 [pii];10.1111/j.1365–2125.2008.03261.x [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kallen BA, Otterblad OP (2007) Maternal use of selective serotonin re-uptake inhibitors in early pregnancy and infant congenital malformations. Birth Defects Res A Clin Mol Teratol 79: 301–308 10.1002/bdra.20327 [doi]. [DOI] [PubMed] [Google Scholar]
- 18. Pedersen LH, Henriksen TB, Vestergaard M, Olsen J, Bech BH (2009) Selective serotonin reuptake inhibitors in pregnancy and congenital malformations: population based cohort study. BMJ 339: b3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reis M, Kallen B (2010) Delivery outcome after maternal use of antidepressant drugs in pregnancy: an update using Swedish data. Psychol Med 1–11. S0033291709992194 [pii];10.1017/S0033291709992194 [doi]. [DOI] [PubMed]
- 20. Wichman CL, Moore KM, Lang TR, Sauver JLS, Heise RH, et al. (2009) Congenital Heart Disease Associated With Selective Serotonin Reuptake Inhibitor Use During Pregnancy. Mayo Clinic Proceedings 84: 23–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wogelius P, Norgaard M, Gislum M, Pedersen L, Munk E, et al. (2006) Maternal use of selective serotonin reuptake inhibitors and risk of congenital malformations. Epidemiology 17: 701–704 10.1097/01.ede.0000239581.76793.ae [doi]. [DOI] [PubMed] [Google Scholar]
- 22. Wurst KE, Poole C, Ephross SA, Olshan AF (2010) First trimester paroxetine use and the prevalence of congenital, specifically cardiac, defects: a meta-analysis of epidemiological studies. Birth Defects Res A Clin Mol Teratol 88: 159–170 10.1002/bdra.20627 [doi]. [DOI] [PubMed] [Google Scholar]
- 23. Malm H, Klaukka T, Neuvonen PJ (2005) Risks associated with selective serotonin reuptake inhibitors in pregnancy. Obstet Gynecol 106: 1289–1296 106/6/1289 [pii];10.1097/01.AOG.0000187302.61812.53 [doi]. [DOI] [PubMed] [Google Scholar]
- 24.Kulin NA, Pastuszak A, Sage SR, Schick-Boschetto B, Spivey G, et al.. (1998) Pregnancy outcome following maternal use of the new selective serotonin reuptake inhibitors: a prospective controlled multicenter study. JAMA 279: 609–610. jbr71201 [pii]. [DOI] [PubMed]
- 25. Ramos E, St-Andre M, Rey E, Oraichi D, Berard A (2008) Duration of antidepressant use during pregnancy and risk of major congenital malformations. The British Journal of Psychiatry 192: 344–350. [DOI] [PubMed] [Google Scholar]
- 26. Einarson A, Choi J, Einarson TR, Koren G (2009) Incidence of major malformations in infants following antidepressant exposure in pregnancy: results of a large prospective cohort study. Can J Psychiatry 54: 242–246. [DOI] [PubMed] [Google Scholar]
- 27. Davis RL, Rubanowice D, McPhillips H, Raebel MA, Andrade SE, et al. (2007) Risks of congenital malformations and perinatal events among infants exposed to antidepressant medications during pregnancy. Pharmacoepidemiol Drug Saf 16: 1086–1094 10.1002/pds.1462 [doi]. [DOI] [PubMed] [Google Scholar]
- 28. Oberlander TF, Warburton W, Misri S, Riggs W, Aghajanian J, et al. (2008) Major congenital malformations following prenatal exposure to serotonin reuptake inhibitors and benzodiazepines using population-based health data. Birth Defects Res B Dev Reprod Toxicol 83: 68–76 10.1002/bdrb.20144 [doi]. [DOI] [PubMed] [Google Scholar]
- 29. Simon GE, Cunningham ML, Davis RL (2002) Outcomes of Prenatal Antidepressant Exposure. Am J Psychiatry 159: 2055–2061. [DOI] [PubMed] [Google Scholar]
- 30. Wen SW, Yang Q, Garner P, Fraser W, Olatunbosun O, et al. (2006) Selective serotonin reuptake inhibitors and adverse pregnancy outcomes. Am J Obstet Gynecol 194: 961–966 S0002–9378(06)00225-0 [pii];10.1016/j.ajog.2006.02.019 [doi]. [DOI] [PubMed] [Google Scholar]
- 31.Ericson A, Kallen B, Wiholm B (1999) Delivery outcome after the use of antidepressants in early pregnancy. Eur J Clin Pharmacol 55: 503–508. 90550503.228 [pii]. [DOI] [PubMed]
- 32. Kallen B, Otterblad Olausson P (2006) Antidepressant drugs during pregnancy and infant congenital heart defect. Reproductive Toxicology 21: 221–222 doi: 10.1016/j.reprotox.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 33. Lennestal RM, Kallen BM (2007) Delivery Outcome in Relation to Maternal Use of Some Recently Introduced Antidepressants. [Article]. Journal of Clinical Psychopharmacology 27: 607–613. [DOI] [PubMed] [Google Scholar]
- 34.Jimenez-Solem E, Andersen JT, Petersen M, Broedbaek K, Jensen JK, et al.. (2012) Exposure to selective serotonin reuptake inhibitors and the risk of congenital malformations: a nationwide cohort study. BMJ Open 2. bmjopen-2012-001148 [pii];10.1136/bmjopen-2012-001148 [doi]. [DOI] [PMC free article] [PubMed]
- 35. Kieler H, Artama M, Engeland A, Ericsson O, Furu K, et al. (2012) Selective serotonin reuptake inhibitors during pregnancy and risk of persistent pulmonary hypertension in the newborn: population based cohort study from the five Nordic countries. BMJ 344: d8012. [DOI] [PubMed] [Google Scholar]
- 36.Jimenez-Solem E, Andersen JT, Petersen M, Broedbaek K, Lander AR, et al.. (2013) SSRI Use During Pregnancy and Risk of Stillbirth and Neonatal Mortality. Am J Psychiatry. 1566972 [pii];10.1176/appi.ajp.2012.11081251 [doi]. [DOI] [PubMed]
- 37. Stephansson O, Kieler H, Haglund B, Artama M, Engeland A, et al. (2013) Selective serotonin reuptake inhibitors during pregnancy and risk of stillbirth and infant mortality. JAMA 309: 48–54 1555130 fda[pii];10.1001/jama.2012.153812 [doi]. [DOI] [PubMed] [Google Scholar]
- 38.Pedersen CB, Gotzsche H, Moller JO, Mortensen PB (2006) The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull 53: 441–449. DMB3816 [pii]. [PubMed]
- 39. Knudsen LB (1998) The Danish Fertility Database. Dan Med Bull 45: 221–225. [PubMed] [Google Scholar]
- 40. Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH (1999) The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 46: 263–268. [PubMed] [Google Scholar]
- 41. Gaist D, Sorensen HT, Hallas J (1997) The Danish prescription registries. Dan Med Bull 44: 445–448. [PubMed] [Google Scholar]
- 42. Sorensen HT, Hansen I, Ejlersen E, Sabroe S, Hamburger H (1996) Identification of patients treated with strong analgesics: an assessment of two Danish information systems with respect to epidemiological research. J Med Syst 20: 57–65. [DOI] [PubMed] [Google Scholar]
- 43.Statistics Denmark (2008) Containing detailed statistical information on the Danish Society. Available: http://www.dst.dk/en. Accessed 2013 March.
- 44. Ververs T, Kaasenbrood H, Visser G, Schobben F, de Jong-van den Berg, et al. (2006) Prevalence and patterns of antidepressant drug use during pregnancy. Eur J Clin Pharmacol 62: 863–870 10.1007/s00228-006-0177-0 [doi]. [DOI] [PubMed] [Google Scholar]
- 45. Andrade SE, Raebel MA, Brown J, Lane K, Livingston J, et al. (2008) Use of antidepressant medications during pregnancy: a multisite study. Am J Obstet Gynecol 198: 194–195 S0002-9378(07)00915-5 [pii];10.1016/j.ajog.2007.07.036 [doi]. [DOI] [PubMed] [Google Scholar]
- 46. Bakker MK, Kolling P, van den Berg PB, de Walle HE, de Jong van den Berg LT (2008) Increase in use of selective serotonin reuptake inhibitors in pregnancy during the last decade, a population-based cohort study from the Netherlands. Br J Clin Pharmacol 65: 600–606 BCP3048 [pii];10.1111/j.1365–2125.2007.03048.x [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cooper WO, Willy ME, Pont SJ, Ray WA (2007) Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol 196: 544–545 S0002-9378(07)00144-5 [pii];10.1016/j.ajog.2007.01.033 [doi]. [DOI] [PubMed] [Google Scholar]
- 48. Wichman CL, Fothergill A, Moore KM, Lang TR, Heise RH, et al. (2008) Recent trends in selective serotonin reuptake inhibitor use in pregnancy. J Clin Psychopharmacol 28: 714–716 10.1097/JCP.0b013e31818b53fd [doi];00004714–200812000–00027 [pii]. [DOI] [PubMed] [Google Scholar]
- 49.Petersen I, Gilbert RE, Evans SJ, Man SL, Nazareth I (2011) Pregnancy as a major determinant for discontinuation of antidepressants: an analysis of data from The Health Improvement Network. J Clin Psychiatry. 10.4088/JCP.10m06090blu [doi]. [DOI] [PubMed]
- 50.FDA (2009) FDA Advising of Risk of Birth Defects with Paxil. Available: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2005/ucm108527.htm. Accessed 2013 March.
- 51. Schatzberg AF (2000) New indications for antidepressants. J Clin Psychiatry 61 Suppl 119–17. [PubMed] [Google Scholar]
- 52. Goodman JH (2009) Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth 36: 60–69 BIR296 [pii];10.1111/j.1523-536X.2008.00296.x [doi]. [DOI] [PubMed] [Google Scholar]
- 53. De las CC, Sanz E (2004) Do therapeutic indications of antidepressants change from one year to another? Pharmacoepidemiol Drug Saf 13: 309–314 10.1002/pds.891 [doi]. [DOI] [PubMed] [Google Scholar]
- 54.Alwan S, Reefhuis J, Rasmussen SA, Friedman JM, Prevention Study TNBD (2010) Patterns of Antidepressant Medication Use Among Pregnant Women in a United States Population. J Clin Pharmacol 0091270010373928. [DOI] [PubMed]
- 55.Munk-Olsen T, Gasse C, Laursen TM (2012) Prevalence of antidepressant use and contacts with psychiatrists and psychologists in pregnant and postpartum women. Acta Psychiatr Scand. [DOI] [PubMed]
- 56. Ramos E, Oraichi D, Rey E, Blais L, Berard A (2007) Prevalence and predictors of antidepressant use in a cohort of pregnant women. BJOG 114: 1055–1064 BJO1387 [pii];10.1111/j.1471-0528.2007.01387.x [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Reefhuis J, Rasmussen SA, Friedman JM (2006) Selective serotonin-reuptake inhibitors and persistent pulmonary hypertension of the newborn. N Engl J Med 354: 2188–2190 354/20/2188 [pii];10.1056/NEJMc060602 [doi]. [DOI] [PubMed] [Google Scholar]
- 58.Danish Society of Obstetrics and Gynaecology (2012) [Behandling med serotoningenoptagshæmmere i graviditeten og under amningen] DANISH. www dsog dk.
- 59. Cohen LS, Nonacs RM, Bailey JW, Viguera AC, Reminick AM, et al. (2004) Relapse of depression during pregnancy following antidepressant discontinuation: a preliminary prospective study. Arch Womens Ment Health 7: 217–221 10.1007/s00737-004-0059-3 [doi]. [DOI] [PubMed] [Google Scholar]
- 60. Cohen LS, Altshuler LL, Harlow BL, Nonacs R, Newport DJ, et al. (2006) Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA 295: 499–507 295/5/499 [pii];10.1001/jama.295.5.499 [doi]. [DOI] [PubMed] [Google Scholar]
- 61. O’Brien L, Laporte A, Koren G (2009) Estimating the economic costs of antidepressant discontinuation during pregnancy. Can J Psychiatry 54: 399–408. [DOI] [PubMed] [Google Scholar]
- 62. Einarson A, Selby P, Koren G (2001) Abrupt discontinuation of psychotropic drugs during pregnancy: fear of teratogenic risk and impact of counselling. J Psychiatry Neurosci 26: 44–48. [PMC free article] [PubMed] [Google Scholar]
- 63. de Jong van den Berg LT, Feenstra N, Sorensen HT, Cornel MC (1999) Improvement of drug exposure data in a registration of congenital anomalies. Pilot-study: pharmacist and mother as sources for drug exposure data during pregnancy. EuroMAP Group. Europen Medicine and Pregnancy Group. Teratology 60: 33–36 10.1002/ (SICI).. [DOI] [PubMed] [Google Scholar]
- 64. Olesen C, Sondergaard C, Thrane N, Nielsen GL, de Jong-van den Berg, et al. (2001) Do pregnant women report use of dispensed medications? Epidemiology 12: 497–501. [DOI] [PubMed] [Google Scholar]
- 65. Paganini-Hill A, Ross RK (1982) Reliability of recall of drug usage and other health-related information. Am J Epidemiol 116: 114–122. [DOI] [PubMed] [Google Scholar]
- 66. Tilley BC, Barnes AB, Bergstralh E, Labarthe D, Noller KL, et al. (1985) A comparison of pregnancy history recall and medical records. Implications for retrospective studies. Am J Epidemiol 121: 269–281. [DOI] [PubMed] [Google Scholar]
- 67. Van den Brandt PA, Petri H, Dorant E, Goldbohm RA, Van de Crommert S (1991) Comparison of questionnaire information and pharmacy data on drug use. Pharm Weekbl Sci 13: 91–96. [DOI] [PubMed] [Google Scholar]
- 68. West SL, Savitz DA, Koch G, Strom BL, Guess HA, et al. (1995) Recall accuracy for prescription medications: self-report compared with database information. Am J Epidemiol 142: 1103–1112. [DOI] [PubMed] [Google Scholar]