Abstract
Introduction
A decreased frequency of unprotected sex during episodes of concurrent relationships may dramatically reduce the role of concurrency in accelerating the spread of HIV. Such a decrease could be the result of coital dilution – the reduction in per-partner coital frequency from additional partners – and/or increased condom use during concurrency. To study the effect of concurrency on the frequency of unprotected sex, we examined sexual behaviour data from three communities with high HIV prevalence around Cape Town, South Africa.
Methods
We conducted a cross-sectional survey from June 2011 to February 2012 using audio computer-assisted self-interviewing to reconstruct one-year sexual histories, with a focus on coital frequency and condom use. Participants were randomly sampled from a previous TB and HIV prevalence survey. Mixed effects logistic and Poisson regression models were fitted to data from 527 sexually active adults reporting on 1210 relationship episodes to evaluate the effect of concurrency status on consistent condom use and coital frequency.
Results
The median of the per-partner weekly average coital frequency was 2 (IQR: 1–3), and consistent condom use was reported for 36% of the relationship episodes. Neither per-partner coital frequency nor consistent condom use changed significantly during episodes of concurrency (aIRR=1.05; 95% confidence interval (CI): 0.99–1.24 and aOR=1.01; 95% CI: 0.38–2.68, respectively). Being male, coloured, having a tertiary education, and having a relationship between 2 weeks and 9 months were associated with higher coital frequencies. Being coloured, and having a relationship lasting for more than 9 months, was associated with inconsistent condom use.
Conclusions
We found no evidence for coital dilution or for increased condom use during concurrent relationship episodes in three communities around Cape Town with high HIV prevalence. Given the low levels of self-reported consistent condom use, our findings suggest that if the frequency of unprotected sex with each of the sexual partners is sustained during concurrent relationships, HIV-positive individuals with concurrent partners may disproportionately contribute to onward HIV transmission.
Keywords: coital dilution, condom use, concurrency, HIV, South Africa, sexual behaviour, sex frequency
Introduction
Concurrent relationships have been defined by the Working Group on Measuring Concurrent Sexual Partnerships of the UNAIDS Reference Group on Estimates, Modelling, and Projections as “overlapping sexual partnerships in which sexual intercourse with one partner occurs between two acts of intercourse with another partner” [1]. The importance of concurrency in driving HIV transmission in hyperendemic settings remains controversial. While some have argued, primarily using modelling studies, that concurrency is a strong facilitator of HIV transmission, or even an essential driver for sustained HIV epidemics [2–4], others have dismissed the concurrency hypothesis, because of perceived flaws in the structure and assumptions of the models used [5] and missing empirical evidence for causal links between levels of concurrency and the local or national HIV prevalence [6–10].
Recently, Sawers et al. concluded that the role of concurrency in accelerating the spread of HIV is dramatically reduced by coital dilution – the reduction in per-partner coital frequency that accompanies the acquisition of additional partners [11]. In general, a decreased frequency of unprotected sex during episodes of concurrent relationships would reduce the transmission-facilitating effect of concurrency. Such a decrease could be the result of coital dilution and/or increased condom use during concurrency [12,13].
Despite the large number of sexual behaviour surveys that have investigated condom use, sex frequency and concurrency in settings with high HIV prevalence, few analyses have specifically focused on condom use and sex frequency in concurrent versus monogamous relationship episodes [14]. In this paper, we aim to address this gap by examining self-reported data on coital frequency and condom use during monogamous and concurrent relationship episodes from an egocentric sexual network survey in three communities with high HIV prevalence around Cape Town, South Africa. Besides the concurrency status, we explore associations with a wide range of demographic and relationship characteristics, to identify other, potentially more important factors that influence coital frequency and condom use.
Methods
Study design and setting
We conducted a cross-sectional survey (n=878) from June 2011 to February 2012 in three urban disadvantaged communities in the greater Cape Town area to study associations between HIV status, sexual connectedness and age-disparity. The study design and protocol is explained in detail elsewhere [15]. In brief, the survey explored one-year sexual histories, with a focus on start and end dates of periods of sexual activity, age differences between sexual partners, sex frequency, condom use and the use of alcohol and recreational drugs. The questionnaire was administered in a safe and confidential mobile interview space, using audio computer-assisted self-interview (ACASI) technology on touch screen computers. ACASI has the benefit of providing privacy to participants and avoids the white coat effect when answering questions about sensitive topics. The ACASI featured a choice of languages and visual feedback of temporal information. All study communities participated in a previous TB/HIV surveillance study, from which HIV test results were anonymously linked to the survey dataset [16]. A list of participants from the TB/HIV surveillance study was generated for each of the three communities, and the names and associated addresses were randomly reordered. Field workers visited the homes of candidate survey participants in the order that they were placed on the list.
Of 1857 people randomly sampled from the TB/HIV surveillance study sampling frame, we were able to find 1115 (60.0% contact rate). For 197 people, the reason for non-retrieval after three attempts is unknown, while for, respectively, 511 and 34, relocation to an unknown new address and death were documented. Eighty-seven candidate participants were excluded, primarily due to visual or physical impairments that rendered participation in the study impossible. Of the remaining 1028, 878 (85.4% response rate) consented to participate.
Participants and variables
Of the 878 survey respondents, 679 (77.3%) had at least one relationship in the last 12 months. These respondents reported on a total of 1567 relationship episodes from 1128 relationships. Relationship episodes with missing data for coital frequency (n=193), condom use (n=5), respondent age (n=3), partner age (n=24) respondent gender (n=49), race (n=5), completed education level (n=1) or employment status (n=2) were excluded. Furthermore, episodes were excluded if the respondents did not sleep with their partner in the past year (n=14) and if the reported ages of respondents were <18 years or >70 years (n=42). In the context of the South African HIV epidemic, the HIV prevalence is considerably higher in black and coloured communities than it is in other racial groups [17]. Our survey was conducted in communities with high HIV prevalence, and consequently, very few people of Indian or white race were included in our sample. Therefore, 19 episodes from three respondents were excluded if the respondents were white, Indian or unknown race, leaving only episodes of black and coloured respondents in the analysis. The term coloured refers to a racial category in South Africa, and consists of racially mixed descendants of Europeans, indigenous populations and slaves from South and East Asia.
For up to five main partners and 15 casual partners, participants indicated the periods (episodes) they were in the relationship on a touch screen timeline [15]. A participant could select multiple different time periods for each partner. The dependent variables, frequency of intercourse and condom use, were asked for each episode indicated on the timeline. Periods of a week or longer during which participants indicated not having slept with a particular partner were counted as “breaks” between relationship episodes. For each relationship episode, participants were asked what the weekly average number of sex acts was (0, 1, 2, … 13, 14, 15, >15) and how frequently they used condoms during sexual intercourse (always, sometimes, never). For each round of questions concerning a particular episode, the timing of the episode was highlighted on the touch screen timeline.
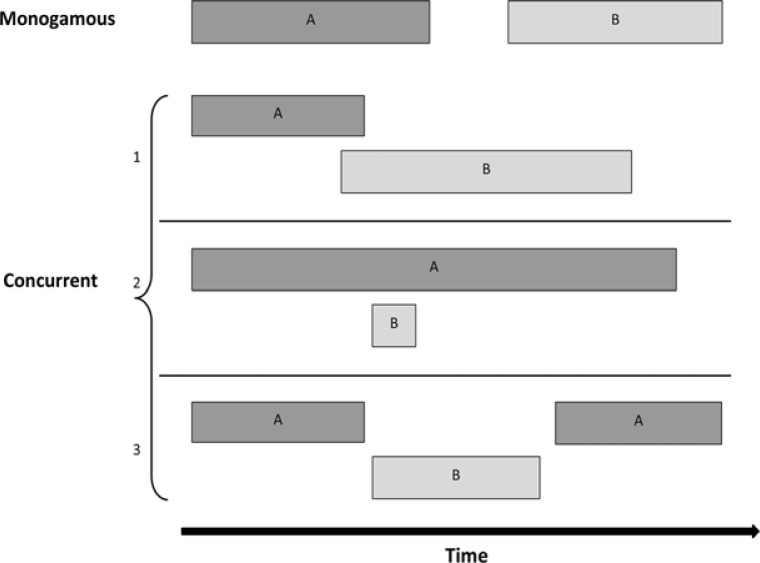
Figure 1 outlines how the concurrency status of each relationship episode was derived from the relationship history time line. Building on the defining characteristic of concurrency that individuals return to a previous partner (A) after having had intercourse with another partner (B), any episode for which this condition was true, was considered concurrent in the primary analysis [1]. Under this definition, as proposed by UNAIDS, 1A, 1B, 2A, 2B and 3B are concurrent episodes. However, this definition may be problematic as it lacks any indication of time scale over which the presence of overlap should be evaluated. Consequently, apparently very different kinds of “overlap” are grouped into the category of concurrent episodes, ranging from a situation in which participants move back and forth between sexual partners multiple times per week for many consecutive weeks, to a situation in which participants alternate between multiple partners, but none of the episodes actually overlap (relationship type 3 in Figure 1). To explore how sensitive our results are to the definition of concurrency, we conducted two parallel analyses. In the first analysis, we applied the literal definition of concurrency according to the UNAIDS reference group (relation episodes 1A, 1B, 2A, 2B and 3B in Figure 1 defined as concurrent). In the second analysis, we only define episodes as concurrent if there is an actual temporal overlap of at least one week (3B in Figure 1 no longer included).
Figure 1.
Schematic representation of monogamous and concurrent relationship episodes.
In addition to concurrency status, candidate explanatory variables for the variation in coital frequency and condom use included age (≤25/26–40/>40), race (coloured/black), religion (Christian/other religion/not religious), employment status (employed/unemployed), completed education level (none or primary/secondary/tertiary), age difference between partners (0–4/5–10/>10), relationship duration (≤1 week/2 weeks to 9 months/>9 months) and partner type (casual/main).
Statistical analysis
First, the coital frequency and condom use data were tabulated and visualized by concurrency status and partner type, and descriptive summary statistics were calculated for all variables under investigation. Next, mixed effects logistic regression and mixed effects Poisson regression models were used to evaluate the effect of concurrency status, on consistent condom use and coital frequency, respectively. These models take into account the correlated nature of the data and variability in the data that stems from both inter- and intra-subject differences in repeated measurements (respondents may report on multiple relationships, which may each consist of multiple relationship episodes) [18]. Backward elimination procedures, based on likelihood ratio tests and Akaike's Information Criterion (AIC), were applied to assess whether employment status, completed education level, religion, age difference between partners, partner type and relationship duration were statistically independent correlates of coital frequency and consistent condom use, after adjusting for concurrency status, race, sex and age.
Ethical approval
The study was approved by the Stellenbosch University Health Research Ethics Committee (N11/03/093). Written, informed consent was obtained for each respondent prior to administration of the questionnaire.
Results
After exclusions, 1210 relationship episodes from 828 relationships reported by 527 sexually active respondents were retained. Tables 1 and 2 describe the demographic characteristics of these respondents and key attributes of their reported relationship episodes respectively.
Table 1.
Individual characteristics of participants in three urban Cape Town communities (aged 18–70 in 2011/2012)
| N | n 527 |
% |
|---|---|---|
| Age | ||
| 18–25 years | 120 | 22.8 |
| 26–40 years | 242 | 45.9 |
| >40 years | 165 | 31.3 |
| Gender | ||
| Male | 163 | 30.9 |
| Female | 364 | 69.1 |
| Race | ||
| Coloured | 108 | 20.5 |
| Black | 419 | 79.5 |
| Education level | ||
| None or primary | 162 | 30.7 |
| Secondary | 347 | 65.8 |
| Tertiary | 18 | 3.4 |
| Employment status | ||
| Employed | 404 | 76.7 |
| Unemployed | 123 | 23.3 |
| Religion | ||
| Christian | 350 | 66.4 |
| Not religious | 148 | 28.1 |
| Other religion | 29 | 5.5 |
| Numbers of partners last year | ||
| 1 | 377 | 71.5 |
| 2 | 79 | 15.0 |
| 3 | 37 | 7.0 |
| >3 | 27 | 5.1 |
| Casual partners last year | ||
| Yes | 91 | 17.3 |
| No | 436 | 82.7 |
Table 2.
Attributes of relationship episodes from 520 participants in three urban Cape Town communities
| N | n 1210 |
% |
|---|---|---|
| Partner type | ||
| Main partner | 992 | 82.0 |
| Casual partner | 218 | 18.0 |
| Concurrency statusa | ||
| Monogamous | 704 | 58.2 |
| Concurrent | 506 | 41.8 |
| Concurrency statusb | ||
| Monogamous | 719 | 59.4 |
| Concurrent | 491 | 40.6 |
| Condom use | ||
| Never | 382 | 31.6 |
| Sometimes | 391 | 32.3 |
| Always | 437 | 36.1 |
| Duration | ||
| ≤1 week | 362 | 29.9 |
| 2 weeks to 9 months | 490 | 40.5 |
| >9 months | 358 | 29.6 |
| Age difference between partners | ||
| <5 years | 880 | 72.7 |
| 5–10 years | 221 | 18.3 |
| >10 years | 109 | 9.0 |
| Average Coital frequency per episode | ||
| 1 | 382 | 29.8 |
| 2 | 378 | 30.8 |
| 3 | 233 | 18.2 |
| >3 | 217 | 21.2 |
UNAIDS defined as any overlapping episode in which sexual intercourse with one partner occurs between two acts of intercourse with another partner. (Relationship episode types 1A, 1B, 2A, 2B, 3B from Figure 1.)
Our modified definition of concurrency, which excludes relationship episode type 3B from Figure 1.
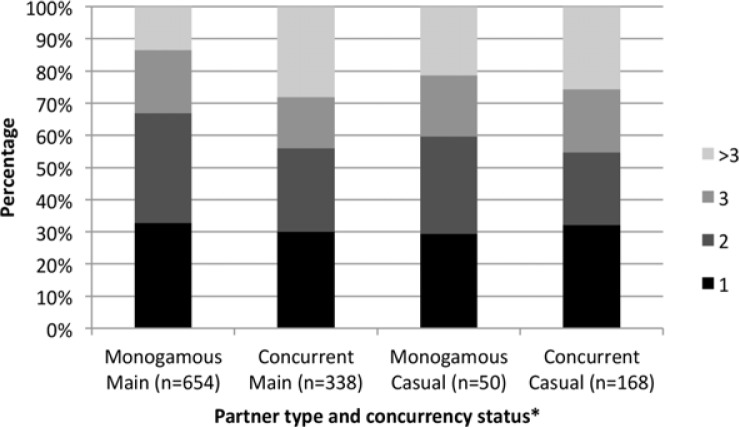
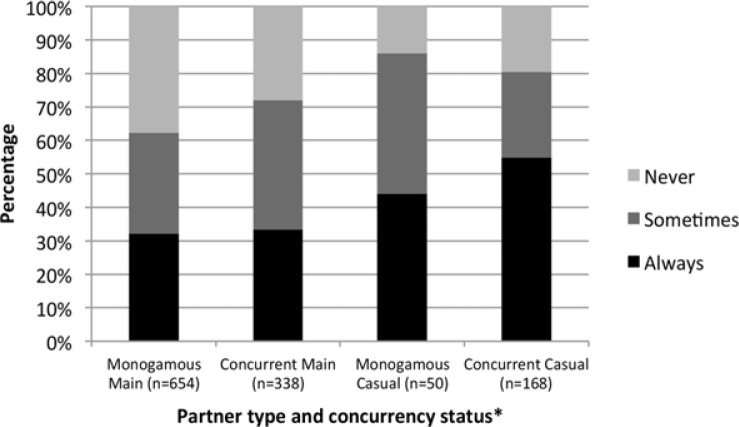
The majority of respondents were black (80%) and female (69%). While females were clearly represented in higher numbers than males in our survey, the fraction of female respondents in our survey was not very different from that in the sampling frame (62%). Most respondents only reported one sexual partner in the last year (72%), and the vast majority of relationship episodes involved a main partner (82%). Forty-two percent (506/1210) of all episodes were concurrent according to the UNAIDS definition, while 41% (491/1210) were concurrent according to our modified definition. The median of the per-partner average coital frequency was two sex acts per week (IQR: 1–3; mean: 2.5), and consistent condom use (always used condoms) was reported in 36% of episodes. Only 28% (146/527) of the study sample reported consistent condom use in all episodes with all partners of the last year. Figures 2 and 3 depict average weekly coital frequency and condom use reported in each of the 1210 episodes, by concurrency status and partner type.
Figure 2.
Distribution of coital frequency, by partner type and concurrency status.
*Using the UNAIDS definition.
Figure 3.
Distribution of condom use, by partner type and concurrency status.
*Using the UNAIDS definition.
Figure 2 shows no immediately obvious, stark differences in coital frequencies in monogamous versus concurrent episodes. In the mixed effects regression analysis, presented in Table 3, there was no evidence for concurrency being associated with a lower average coital frequency. Rather, both definitions showed a slight, albeit non-significant, increase in coital frequency during concurrent episodes (UNAIDS definition: aIRR=1.05; 95% confidence interval (CI): 0.99–1.24 and modified definition: aIRR=1.04; 95% CI: 0.98–1.23). Being female (aIRR=0.83; 95% CI: 0.72–0.91), coloured (aIRR=1.34; 95% CI: 1.13–1.48), obtaining a tertiary education (aIRR=1.44; 95% CI: 1.12–1.96), having a relationship of 2 weeks to 9 months in duration (aIRR=1.15; 95% CI: 1.05–1.30) and belonging to an “other” religion (aIRR=1.27; 95% CI: 1.11–1.77) were shown to have a significant association with coital frequency in the model using the UNAIDS definition of concurrency. Using our modified concurrency definition did not qualitatively change these estimates.
Table 3.
Adjusted incident rate ratios for coital frequency using mixed effects models
| UNAIDS concurrency definitiona | Our modified concurrency definitionb | |||
|---|---|---|---|---|
|
|
|
|||
| aIRR | 95% CI for aIRR | aIRR | 95% CI for aIRR | |
| Concurrent | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.05 | 0.99–1.24 | 1.04 | 0.98–1.23 |
| Age | ||||
| 18–25 years | 1.00 | 1.00 | ||
| 25–40 years | 1.03 | 0.87–1.13 | 1.03 | 0.87–1.13 |
| >40 years | 0.98 | 0.81–1.11 | 0.98 | 0.81–1.11 |
| Gender | ||||
| Male | 1.00 | 1.00 | ||
| Female | 0.83 | 0.72–0.91 | 0.81 | 0.72–0.91 |
| Race | ||||
| Black | 1.00 | 1.00 | ||
| Coloured | 1.34 | 1.13–1.48 | 1.34 | 1.13–1.48 |
| Partner type | ||||
| Main | 1.00 | 1.00 | ||
| Casual | 1.00 | 0.94–1.21 | 1.07 | 0.94–1.21 |
| Education | ||||
| None or primary | 1.00 | 1.00 | ||
| Secondary | 1.12 | 0.94–1.22 | 1.12 | 0.94–1.22 |
| Tertiary | 1.44 | 1.12–1.96 | 1.45 | 1.12–1.96 |
| Duration | ||||
| ≤1 week | 1.00 | 1.00 | ||
| 2 weeks to 9 months | 1.15 | 1.05–1.30 | 1.17 | 1.05–1.30 |
| >9 months | 1.07 | 0.95–1.22 | 1.08 | 0.95–1.23 |
| Religion | ||||
| Christian | 1.00 | 1.00 | ||
| Not religious | 1.03 | 0.94–1.19 | 1.04 | 0.94–1.19 |
| Other | 1.27 | 1.11–1.77 | 1.28 | 1.11–1.77 |
aIRR, adjusted incident rate ratio; CI, confidence interval.
Defined as any overlapping episode in which sexual intercourse with one partner occurs between two acts of intercourse with another partner. (Relationship episode types 1A, 1B, 2A, 2B, 3B from Figure 1.)
Excludes relationship episode type 3B from Figure 1.
The condom use outcomes shown in Figure 3 indicate higher consistent condom use in concurrent episodes with casual partners (55%; 44% in monogamous episodes), and similarly low levels of condom use in episodes with main partners, regardless of concurrency status (32–33%). In the mixed effects regression analysis, presented in Table 4, concurrency was not significantly associated with consistent condom use (UNAIDS definition: aOR=1.01; 95% CI: 0.38–2.68 and modified definition: aOR=1.48; 95% CI: 0.58–3.79), but race and relationship duration were. Being coloured (aOR=0.08; 95% CI: 0.01–0.63) and having a relationship duration of more than 9 months (aOR=0.08; 95% CI: 0.03–0.20) were associated with consistent condom use in the model using the UNAIDS definition of concurrency. Similarly to the coital frequency analysis, using our modified concurrency definition did not qualitatively change these estimates. Initial data exploration suggested that partner type was associated with consistent condom use as well, and that there might be effect modification of concurrency status by partner type and by gender. However, partner type could not be included in the final model because of quasi complete separation in the data tables. Furthermore, adding the interaction terms separately, did not improve model fit, and hence these interaction terms were not included in the final model.
Table 4.
Adjusted odds ratios for consistent condom use using mixed effects models
| UNAIDS concurrency definitiona | Our modified concurrency definitionb | |||
|---|---|---|---|---|
|
|
|
|||
| aOR | 95% CI for aOR | aOR | 95% CI for aOR | |
| Concurrent | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.01 | 0.38–2.68 | 1.48 | 0.58–3.79 |
| Age | ||||
| 18–25 years | 1.00 | 1.00 | ||
| 25–40 years | 1.52 | 0.32–7.19 | 1.49 | 0.31–7.24 |
| >40 years | 0.87 | 0.15–4.94 | 0.90 | 0.15–5.31 |
| Gender | ||||
| Male | 1.00 | 1.00 | ||
| Female | 1.07 | 0.27–4.21 | 1.14 | 0.28–4.59 |
| Race | ||||
| Black | 1.00 | 1.00 | ||
| Coloured | 0.08 | 0.01–0.63 | 0.08 | 0.01–0.68 |
| Duration | ||||
| ≤1 week | 1.00 | 1.00 | ||
| 2 weeks to 9 months | 0.46 | 0.21–1.01 | 0.42 | 0.18–0.95 |
| >9 months | 0.08 | 0.03–0.20 | 0.07 | 0.03–0.19 |
aOR, adjusted odds ratio; CI, confidence interval.
Defined as any overlapping episode in which sexual intercourse with one partner occurs between two acts of intercourse with another partner. (Relationship episode types 1A, 1B, 2A, 2B, 3B from Figure 1).
Excludes relationship episode type 3B from Figure 1.
Discussion
Our findings have implications both for the debate around the role of concurrency in the spread of HIV, and more generally for priority setting in HIV prevention. The key factors that determine the role of concurrency in HIV transmission dynamics include: prevalence of concurrent relationships, duration of concurrent episodes, variability of HIV infectiousness with time since infection, connectedness of the entire sexual network and differences in frequencies of HIV exposures (unprotected sex acts) during monogamous versus concurrent episodes [2,10,12,19–21]. Given the large effect of sex frequency and consistent condom use on transmission risk, both coital dilution and increases in consistent condom use could substantially reduce the effect of concurrency on HIV transmission.
This study does not lend support to the coital dilution hypothesis, nor does is it suggest increased condom use during periods of concurrency, after adjusting for confounding variables. Instead, in our study sample of black and coloured respondents from three communities around Cape Town with high HIV prevalence, the coital frequency was higher, but not significantly higher, in concurrent compared to monogamous relationship episodes, regardless of the definition of concurrency. This finding is at odds with the survey findings from sub-Saharan Africa cited by Sawers et al. [4,11,22]. It is worth pointing out that Sawers et al. make incorrect inferences from Morris et al. [4] and Harrison et al. [22] by confusing and conflating concurrency status (monogamous versus concurrent) with relationship type (primary versus secondary). We believe the apparent discrepancies between these two studies cited by Sawers et al. and ours can be explained by differences in how coital frequency was measured and how concurrency status was assigned. In our survey, participants could indicate multiple relationship episodes with the same partner, with a resolution of one-week time blocks. This allowed us to observe relationships that consisted of multiple, disjointed episodes (14% of main relationships (n=92) and 13% of casual relationships (n=22)) instead of one continuous time period.
Morris's categorization into “more frequent” and “less frequent” concurrent partners by design creates differences in sex frequency between different sexual partners. However, Morris's analysis does not confirm that coital frequencies are lower in concurrent versus monogamous relationships. Moreover, in the surveys reported by Morris et al. participants were asked how many acts of sex they had over the course of the year for “primary” (more frequent) and “secondary” (less frequent) concurrent partnerships, assuming that these partnerships occurred as one continuous episode throughout the year with no gaps. Thus, the survey failed to take into account that some partnerships may have a low cumulative number of sex acts, but consist of one or many short episodes, during which the average coital frequency is high. In the same way, Harrison et al. failed to identify relationship episodes and measure coital frequency within each episode. Crucially, they did not restrict analysis of the time since last sex act with the last two sexual partners to respondents who were still in on-going relationships with both these partners. Lack of knowledge of the concurrency status in this analysis of time since last sex act, precludes estimation of the effect of concurrency status on per-partner coital frequency. Sawers et al. may therefore have incorrectly inferred coital dilution from larger times since last sex with the second most recent partner.
To our knowledge, this is one of few studies that have attempted to identify behavioural and demographic correlates of coital frequency in concurrent and monogamous relationships [2,23–25]. In our study sample, being coloured, male and having a tertiary education; being in a relationship for a period of 2 weeks to 9 months; and belong to an “other” religion were independent, individual-level predictors of higher coital frequency.
Our crude estimators for consistent condom use in monogamous and concurrent relationship episodes (Figure 3) compare well with related statistics previously reported. In a survey among young black people around Cape Town, 44% of men with a history of concurrency reported consistent condom use [26]. Further, Chopra et al. reported more consistent condom use with casual partners than with “steady” partners in a cohort of young Cape Town men of whom 98% reported concurrent relationships in the last three months [27]. Similarly, Maher et al. observed that condom use with concurrent partners was more frequent if partnerships were casual instead of “regular”, non-spousal [7].
Results from the mixed effects regression analysis do not provide evidence for increased condom use during concurrency. Other studies, however, have found significant associations between condom use and concurrency status. Of note, Steffenson et al. found that in South African men and women aged 15–24, those who had at least one concurrent relationship in the last year (“concurrents”) used condoms less frequently than people in monogamous relationships (“monogamists”) [28]. The discrepancy between their study results and ours might be accounted for by the fact that our analysis was done at the level of relationship episodes, and compares all of the monogamous to all of the concurrent episodes, while adjusting for a range of confounding variables. In contrast, Steffenson et al. measured concurrency status at the level of an individual and then compared condom use during only the most recent relationship in “concurrents” and “monogamists”. They, therefore, were not able to accurately determine if concurrent relationships, much less concurrent episodes, are associated with less consistent condom use. Another study, conducted by Kasamba et al., explored condom use in spousal and extra-spousal partnerships and found that men who had extra-spousal partnerships were more likely to have ever used condoms with their spouse [29]. Direct comparison with our findings is limited by the fact that they measured “ever having used condoms” and classified relationships into spousal and extra-spousal relationships. We measured “always used a condom” rather than “ever used a condom” because it is a more meaningful indicator of HIV risk aversion.
Implications of our findings for HIV prevention efforts follow primarily from the observation that consistent condom use was generally low, especially in relationships with main partners. Consistent condom use is known to be extremely hard to achieve in long-term, trusting relationships [30], even if they involve transactional sex [31]. Although consistent condom use was more frequently reported with casual partners, as was also seen elsewhere [32,33], there is still a lot of potential for averting HIV transmissions in casual relationships, especially since casual partners may carry a higher burden of sexually transmitted infections, which are known to facilitate HIV transmission [34–37].
Our study has four main limitations. First, in our study, respondents could only report one average weekly coital frequency per episode, regardless of the episode's duration. Consequently, this self-reported average would only be affected minimally, if at all, if coital frequency was temporarily lower during times of concurrency with an episode that overlapped the index episode for a small fraction. Second, left and right censoring of relationships may have led to misclassification of some episodes as monogamous because we had no knowledge of future episodes and episodes that took place more than a year before the survey. Third, the candidate individual-level predictor variables (i.e. religion, employment status, education level, age, sex and race) we explored were asked only at the time of the survey, but used to predict past behaviour (i.e. coital frequency and condom use). Theoretically, these variables may not have stayed constant over the one-year relationship history window. Lastly, our survey data may be subject to bias due to possible dependent errors in reporting concurrency, coital frequency and condom use. We do note, however, that this bias may also have been present in the egocentric survey data that was cited by Sawers et al. to support the coital dilution hypothesis. Hence, this bias alone cannot explain the difference between our observations and those cited previously in support of coital dilution.
Despite these limitations, our study had several strengths, which we believe support the accuracy of our results. Rather than face-to-face interviewing, the survey was conducted using ACASI. While comparisons of ACASI and more traditional survey methods have been mixed, several studies that compared ACASI methods with face-to-face interviews in the African context have indicated that participants are more likely to report sexual risk behaviours while using ACASI [38–42]. In addition, we have performed a dedicated analysis of the user-friendliness, privacy and truthfulness of our ACASI instrument. The key conclusion of this paper is that most participants in our survey found the ACASI modality to be acceptable, private, and user-friendly. Moreover, our results indicate less social desirability bias when reporting on multiple, concurrent partners, than in the face-to-face interviews used in Demographic and Health Surveys done in Southern Africa [43]. Furthermore, respondents were asked to place the episodes for each of their relationships in the past year directly on a timeline, progressively from the oldest to the most recent relationship. Thus, the timeline and the episodes of earlier relationships provided visual reference points, which facilitated internal consistency of a respondent's relationship history [44,45]. Finally, our study is unique in that it allowed participants to define their relationships as a series of episodes, which more accurately portrays how people engage in relationships. In reality, relationships are not always continuous: they often have periods of sexual activity and inactivity, and sexual behaviours may not be the same for each new period of a relationship.
Conclusions
In conclusion, we found no evidence for coital dilution, i.e. for a decreased per-partner sex frequency, or for increased condom use during concurrent relationship episodes in three communities around Cape Town with high HIV prevalence, after adjusting for confounding variables. Instead, concurrency was associated with a slight, borderline-significant (at α=0.05) increase in coital frequency. The main implication of our findings for the concurrency debate is that, if the frequency of unprotected sex with each of the sexual partners is sustained during concurrent relationships, HIV-positive individuals with concurrent partners may disproportionately contribute to onward HIV transmission. Additional analyses from other geographic and epidemiological settings are needed to create a larger body of evidence related to coital frequency and condom use in monogamous and concurrent relationship episodes, and more generally, to deepen our understanding of the determinants of coital frequency and consistent condom use.
Acknowledgements
The authors wish to thank the survey respondents for their participation in this study. We are also indebted to the research assistants for countless hours of dedicated fieldwork and to the Desmond Tutu TB Centre at Stellenbosch University for their guidance in coordination and planning of this cross-sectional sexual behaviour survey.
Funding sources: The Flemish Interuniversity Council (VLIR) and the Flemish Scientific Research Fund (FWO) provided financial support for the survey. WD, RB and AW received funding from the Canadian International Development Agency (CIDA). FM was funded by FWO, and NH acknowledges support from the University of Antwerp scientific chair in Evidence-Based Vaccinology, financed in 2009–2012 by an unrestricted donation from Pfizer.
Competing interests
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Authors' contributions
WD, ND, RB, MT, AW and NH jointly designed the ACASI survey. RB coordinated data collection. FM and RB conducted the statistical analysis. NH supervised the data analysis. WD and RB wrote the first draft manuscript. All authors contributed during the editing process and approved the final, submitted manuscript.
References
- 1.UNAIDS Reference Group on Estimates Modelling and Projections: Working Group on Measuring Concurrent Sexual Partnerships. HIV: consensus indicators are needed for concurrency. Lancet. 2010;375(9715):621–2. doi: 10.1016/S0140-6736(09)62040-7. [DOI] [PubMed] [Google Scholar]
- 2.Goodreau SM, Cassels S, Kasprzyk D, Montano DE, Greek A, Morris M. Concurrent partnerships, acute infection and HIV epidemic dynamics among young adults in Zimbabwe. AIDS Behav. 2012;16(2):312–22. doi: 10.1007/s10461-010-9858-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mah TL, Shelton JD. Concurrency revisited: increasing and compelling epidemiological evidence. J Int AIDS Soc. 2011;14:33. doi: 10.1186/1758-2652-14-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris M, Epstein H, Wawer M. Timing is everything: international variations in historical sexual partnership concurrency and HIV prevalence. PLoS One. 2010;5(11):e14092. doi: 10.1371/journal.pone.0014092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lurie MN, Rosenthal S. Concurrent partnerships as a driver of the HIV epidemic in sub-Saharan Africa? The evidence is limited. AIDS Behav. 2010;14:17–24. doi: 10.1007/s10461-009-9583-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lagarde E, Auvert B, Carael M, Laourou M, Ferry B, Akam E, et al. Concurrent sexual partnerships and HIV prevalence in five urban communities of sub-Saharan Africa. AIDS. 2001;15(7):877–84. doi: 10.1097/00002030-200105040-00008. [DOI] [PubMed] [Google Scholar]
- 7.Maher D, Waswa L, Karabarinde A, Baisley K. Concurrent sexual partnerships and associated factors: a cross-sectional population-based survey in a rural community in Africa with a generalised HIV epidemic. BMC Public Health. 2011;11:651. doi: 10.1186/1471-2458-11-651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mishra V, Binami-Van Assche S. DHS Working papers. Calverton, Maryland: Macro International Inc; 2009. Concurrent sexual partnerships and HIV infection: evidence from national population-based surveys. [Google Scholar]
- 9.Tanser F, Barnighausen T, Hund L, Garnett GP, McGrath N, Newell ML. Effect of concurrent sexual partnerships on rate of new HIV infections in a high-prevalence, rural South African population: a cohort study. Lancet. 2011;378(9787):247–55. doi: 10.1016/S0140-6736(11)60779-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawers L, Stillwaggon E. Concurrent sexual partnerships do not explain the HIV epidemics in Africa: a systematic review of the evidence. J Int AIDS Soc. 2010;13:34. doi: 10.1186/1758-2652-13-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sawers L, Isaac AG, Stillwaggon E. HIV and concurrent sexual partnerships: modelling the role of coital dilution. J Int AIDS Soc. 2011;14:44. doi: 10.1186/1758-2652-14-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boily MC, Alary M, Baggaley RF. Neglected issues and hypotheses regarding the impact of sexual concurrency on HIV and sexually transmitted infections. AIDS Behav. 2012;16(2):304–11. doi: 10.1007/s10461-011-9887-0. [DOI] [PubMed] [Google Scholar]
- 13.Reniers G, Watkins S. Polygyny and the spread of HIV in sub-Saharan Africa: a case of benign concurrency. AIDS. 2010;24(2):299–307. doi: 10.1097/QAD.0b013e328333af03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epstein H, Swidler A, Gray R, Reniers G, Parker W, Parkhurst J, et al. Measuring concurrent partnerships. Lancet. 2010;375:1869. doi: 10.1016/S0140-6736(10)60864-1. [DOI] [PubMed] [Google Scholar]
- 15.Delva W, Beauclair R, Welte A, Vansteelandt S, Hens N, Aerts M, et al. Age-disparity, sexual connectedness and HIV infection in disadvantaged communities around Cape Town, South Africa: a study protocol. BMC Public Health. 2011;11:616. doi: 10.1186/1471-2458-11-616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayles HM, Sismanidis C, Beyers N, Hayes RJ, Godfrey-Faussett P. ZAMSTAR, The Zambia South Africa TB and HIV Reduction study: design of a 2×2 factorial community randomized trial. Trials. 2008;9:63. doi: 10.1186/1745-6215-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shisana O, Simbayi LC, Rehle T, Zungu NP, Zuma K, Ngogo N, et al. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2008: the health of our children. Cape Town: HSRC Press; 2010. [Google Scholar]
- 18.Cnaan A, Laird NM, Slasor P. Using the general linear mixed model to analyse unbalanced repeated measures and longitudinal data. Stat Med. 1997;16(20):2349–80. doi: 10.1002/(sici)1097-0258(19971030)16:20<2349::aid-sim667>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 19.Eaton JW, Hallett TB, Garnett GP. Concurrent sexual partnerships and primary HIV infection: a critical interaction. AIDS Behav. 2011;15(4):687–92. doi: 10.1007/s10461-010-9787-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Powers KA, Hoffman IF, Ghani AC, Hosseinipour MC, Pilcher CD, Price MA, et al. Sexual partnership patterns in Malawi: implications for HIV/STI transmission. Sex Transm Dis. [Research Support, N.I.H., Extramural] 2011;38(7):657–66. doi: 10.1097/OLQ.0b013e31820cb223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kretzschmar M, White RG, Carael M. Concurrency is more complex than it seems. AIDS. 2009;24:313–5. doi: 10.1097/QAD.0b013e328333eb9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harrison A, Cleland J, Frohlich J. Young people's sexual partnerships in KwaZulu-Natal, South Africa: patterns, contextual influences, and HIV risk. Stud Fam Plann. 2008;39(4):295–308. doi: 10.1111/j.1728-4465.2008.00176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Westoff CF. Recent trends in rates of sexual activity in sub-Saharan Africa. J Biosoc Sci. 2007;39(6):895–904. doi: 10.1017/S0021932007001848. [DOI] [PubMed] [Google Scholar]
- 24.Reniers G, Tfaily R. Polygyny, partnership concurrency, and HIV transmission in sub-Saharan Africa. Demography. 2012;49:1075–101. doi: 10.1007/s13524-012-0114-z. [DOI] [PubMed] [Google Scholar]
- 25.Xu H, Luke N, Zulu EM. Concurrent sexual partnerships among youth in urban Kenya: prevalence and partnership effects. Popul Stud. 2010;64(3):247–61. doi: 10.1080/00324728.2010.507872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maughan-Brown B. Variation in concurrent sexual partnerships and sexually transmitted diseases among African men in cape town, South Africa. Sex Transm Dis. 2012;39(7):537–42. doi: 10.1097/OLQ.0b013e31824cc0c1. [DOI] [PubMed] [Google Scholar]
- 27.Chopra M, Townsend L, Johnston L, Mathews C, Tomlinson M, O'Bra H, et al. Estimating HIV prevalence and risk behaviors among high-risk heterosexual men with multiple sex partners: use of respondent-driven sampling. J Acquir Immune Defic Syndr. 2009;51(1):72–7. doi: 10.1097/QAI.0b013e31819907de. [DOI] [PubMed] [Google Scholar]
- 28.Steffenson AE, Pettifor AE, Seage GR, 3rd, Rees HV, Cleary PD. Concurrent sexual partnerships and human immunodeficiency virus risk among South African youth. Sex Transm Dis. 2011;38(6):459–66. doi: 10.1097/OLQ.0b013e3182080860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kasamba I, Sully E, Weiss HA, Baisley K, Maher D. Extraspousal partnerships in a community in rural Uganda with high HIV prevalence: a cross-sectional population-based study using linked spousal data. J Acquir Immune Defic Syndr. 2011;58(1):108–14. doi: 10.1097/QAI.0b013e318227af4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chimbiri AM. The condom is an ‘intruder’ in marriage: evidence from rural Malawi. Soc Sci Med. 2007;64(5):1102–15. doi: 10.1016/j.socscimed.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 31.Voeten HA, Egesah OB, Varkevisser CM, Habbema JD. Female sex workers and unsafe sex in urban and rural Nyanza, Kenya: regular partners may contribute more to HIV transmission than clients. Trop Med Int Health. 2007;12(2):174–82. doi: 10.1111/j.1365-3156.2006.01776.x. [DOI] [PubMed] [Google Scholar]
- 32.Chimbindi NZ, McGrath N, Herbst K, San Tint K, Newell ML. Socio-demographic determinants of condom use among sexually active young adults in rural KwaZulu-Natal, South Africa. Open AIDS J. 2010;4:88–95. doi: 10.2174/1874613601004010088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Westercamp N, Mattson CL, Madonia M, Moses S, Agot K, Ndinya-Achola JO, et al. Determinants of consistent condom use vary by partner type among young men in Kisumu, Kenya: a multi-level data analysis. AIDS Behav. 2010;14(4):949–59. doi: 10.1007/s10461-008-9458-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Onoya D, Reddy P, Sifunda S, Lang D, Wingood GM, van den Borne B, et al. Transactional sexual relationships, sexually transmitted infection risk, and condom use among young Black Women in peri-urban areas of the Western Cape Province of South Africa. Womens Health Issues. 2012;22(3):e277–82. doi: 10.1016/j.whi.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 35.Wasserheit JN. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992;19(2):61–77. [PubMed] [Google Scholar]
- 36.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75(1):3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mahiane SG, Legeai C, Taljaard D, Latouche A, Puren A, Peillon A, et al. Transmission probabilities of HIV and herpes simplex virus type 2, effect of male circumcision and interaction: a longitudinal study in a township of South Africa. AIDS. 2009;23(3):377–83. doi: 10.1097/qad.0b013e32831c5497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dolezal C, Marhefka SL, Santamaria EK, Leu CS, Brackis-Cott E, Mellins CA. A comparison of audio computer-assisted self-interviews to face-to-face interviews of sexual behavior among perinatally HIV-exposed youth. Arch Sex Behav. 2012;41(2):401–10. doi: 10.1007/s10508-011-9769-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hewett P, Mensch B, Erulkar A. Consistency in the reporting of sexual behavior by adolescent girls in Kenya: a comparison of interviewing methods. Sex Transm Infect. 2004;80(Suppl 2):ii43–8. doi: 10.1136/sti.2004.013250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kissinger P, Rice J, Farley T, Trim S, Jewitt K, Margavio V, et al. Application of computer-assisted interviews to sexual behavior research. Am J Epidemiol. 1999;149(10):950–4. doi: 10.1093/oxfordjournals.aje.a009739. [DOI] [PubMed] [Google Scholar]
- 41.Phillips AE, Gomez GB, Boily MC, Garnett GP. A systematic review and meta-analysis of quantitative interviewing tools to investigate self-reported HIV and STI associated behaviours in low- and middle-income countries. Int J Epidemiol. 2010;39(6):1541–55. doi: 10.1093/ije/dyq114. [DOI] [PubMed] [Google Scholar]
- 42.van der Elst E, Okuku H, Nakamya P, Muhaari A, Davies A, McClelland R, et al. Is audio computer-assisted self-interview (ACASI) useful in risk behavior assessment of female and male sex workers, Mombasa, Kenya? PLoS One. 2009;4(5):e5340. doi: 10.1371/journal.pone.0005340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beauclair R, Meng F, Deprez N, Temmerman M, Welte A, Hens N, et al. Evaluating audio computer assisted self-interviews in urban South African communities: evidence for good suitability and reduced social desirability bias of a cross-sectional survey on sexual behaviour. BMC Med Res Methodol. 2013;13:11. doi: 10.1186/1471-2288-13-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kabiru CW, Luke N, Izugbara CO, Zulu E. The correlates of HIV testing and impacts on sexual behaviour: evidence from a life history study of young people in Kisumu, Kenya. BMC Public Health. 2010;10:412. doi: 10.1186/1471-2458-10-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Luke N, Clark S, Zulu E. The relationship history calendar: improving the scope and quality of data on youth sexual behavior. Demography. 2011;48(3):1151–76. doi: 10.1007/s13524-011-0051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]