Abstract
It is now privately acknowledged that there may be little if any perceptible impact of the national Bacille Calmette–Guerin (BCG) vaccination program on disease prevalence, despite the extensive coverage of the newborn infant population and likely benefit in the early years of life. A better preventive vaccine than BCG is now being sought by Chinese researchers. Urgency has been added to the control problem by the emergence of multidrug-resistant tuberculosis (TB). Furthermore, expensive second-line drugs seem unlikely to be made available by the government to treat drug-resistant cases, so attention in addition has turned to the potential of immunotherapy as an adjunct to chemotherapy. Research trends are summarized here.
Keywords: immunotherapies, tuberculosis, vaccines
Introduction
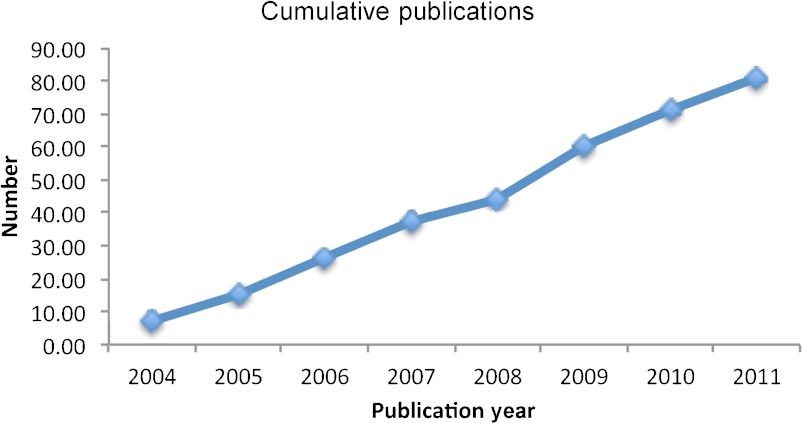
There has been a striking upsurge in tuberculosis (TB) vaccine research in China in recent years. More than 80 papers reporting such research have been published since 2004 (Figure 1), many in English Language Journals. This has been driven and funded largely by Chinese Government agencies, since the scale of the TB problem and the difficulties in implementing fully effective control measures were recognized.1,2,3 There seemingly has been little commercial interest. In considering the published output, we can note that there are at least two additional restricting factors limiting the progress of the field in China: few research groups have access to facilities for safely working with animals infected with a dangerous pathogenic organism such as the tubercle bacillus; infrastructure for undertaking vaccine clinical trials to international standards is sparse. In consequence, the universal problem of how to select among the promising approaches and candidate vaccines is particularly acute in China. Nevertheless, the basic research problems are being tackled with some enthusiasm and creativity, and the new 5-year program to improve TB control that was announced by the Chinese Ministry of Health on 1 April 2009 will have an impact. The antigens investigated to date and the locations of research groups are listed in Tables 1 and 2, respectively.
Figure 1.
The number of TB vaccine research publications by Chinese Research Groups, 2004–2011.
Table 1. TB antigens tested.
| Antigens | References |
|---|---|
| ESAT6 | 6, 9, 10, 12–15, 19, 25, 29, 30, 32, 35, 36, 39, 41–45, 50, 52–56, 64, 67, 68, 71, 80, 82 |
| 85B | 7, 14, 15, 27–29, 31, 32, 48, 51, 53–56, 59–61. 63–65, 67, 68, 70, 72, 78, 84 |
| MPT64 | 17, 33, 34, 45, 48, 51, 54, 55, 59–61, 65, 66, 72, 78, 84 |
| Ag85A | 32, 37–41, 50, 67, 80, 82, 83 |
| hsp65 | 4, 32, 46, 69, 76, 85 |
| CFP10 | 10, 19, 25, 30, 32, 71 |
| Mtb8.4 | 23, 31, 48, 49, 51, 62 |
| MPT83 | 56, 59–61, 72 |
| hsp16.3 (hspX) | 16, 47, 49, 71 |
| 38-kDa | 25, 31, 33 |
| MPT63 | 54, 55 |
| BCG | 5, 11 |
| M. vaccae | 73, 74 |
| rec. M. smegmatis | 75 |
| MTB48 | 25 |
| MPT70 | 65 |
| TB10.4 | 65 |
| CFP21 | 66 |
| hsp70 | 77 |
| Rv1009 | 18 |
| Rv1987 | 26 |
| Rv2450 | 20 |
| Rv3425 | 7, 22 |
| Rv3772 | 21 |
| Rv3807c | 26 |
| Rv3887c | 26 |
| MPB64 | 68 |
| M. bovis RD-1 to RD-16 | 24 |
Table 2. The leading cities for TB vaccine research.
| Main author affiliation | References |
|---|---|
| Beijing | |
| National Lab of Protein Engineering & Plant Genetic Engineering, Peking University | 54–56, 59–61, 65, 72, 84 |
| Institute for Tuberculosis Research, Second Hospital Affiliated to 309 General Hospital of the PLA | 12, 25, 28, 80, 83 |
| National Institute for Control of Pharmaceutical & Biological Products | 71 |
| Chengdu | |
| West China Center of Medical Science, Sichuan University School of Basic Medicine | 9, 10, 52 |
| Sichuan University, Chengdu | 41 |
| Chinese Cochrane Center, Chinese Evidence Based Medicine Center, West China Hospital, Sichuan University | 73, 74 |
| Chongqing | |
| Clinical Immunology Department, Chongqing University of Medical Sciences | 13 |
| Department of Pathobiology, Chongqing Medical University | 75 |
| Department of Microbiology, Chongqing University of Medical Sciences | 57, 58 |
| Department of Microbiology and Immunology, Chongqing University of Medical Sciences | 78, 79 |
| Haikou | |
| Department of Laboratory Medicine, Affiliated Xinhua Hospital of Hainan Medical College | 31, 62, 63 |
| Harbin | |
| Harbin Veterinary Research Institute, Chinese Academy of Agricultural Science | 68 |
| Hong Kong | |
| Department of Pediatrics & Adolescent Medicine, Faculty of Medicine, University of Hong Kong | 5 |
| Jinan | |
| Institute of Basic Medicine, Shandong Academy of Medical Sciences | 27 |
| Lanzhou | |
| Institute of Pathogenic Biology, Lanzhou University | 23 |
| School of Basic Medical Sciences, Lanzhou University | 48 |
| Luzhou | |
| Department of Infectious Disease, Affiliated Hospital of Luzhou Medical College | 77 |
| Nanjing | |
| School of Basic Medical Sciences, South East University | 38–40 |
| Shanghai | |
| Institute of Genetics, Fudan University | 7, 15, 21, 22, 24, 51 |
| Ship Environmental Health Division, Institute of Naval Medicine Research | 33, 42 |
| College of Basic Medical Sciences, Second Military Medical University | 33–36 |
| Vaccine Research Laboratory, Shanghai H&G Biotechnology Co. Inc. | 43, 44 |
| Shanghai Public Health Clinical Center, Fudan University | 85 |
| Shenyang | |
| Department of Immunology, China Medical University | 37 |
| Wuhan | |
| Department of Immunology, Medical School of Wuhan University | 4, 32, 53, 70 |
| Department of Pathogen Biology, Huazhong University of Science & Technology, Tongji Medical College | 50, 66, 67 |
| Center for Proteomics Research, College of Life Science & Technology, Huazhong Agricultural University | 26 |
| Xi'An | |
| Fourth Military Medical University | 6, 16–20, 45–47, 64, 69, 76 |
| Research Center of Laboratory Animals, Fourth Military Medical University | 30 |
TB immunity
A substantial body of work has gone into characterizing the immune responses to be found in TB infection and following vaccination. The twin purposes of identifying candidate antigens for use in vaccines and diagnostic tests and of defining immunological markers for latent infection and disease states drive these studies. These studies have not always been followed up with tests of protective or therapeutic efficacy in animal infection models.
The increased immunogenicity of mouse dendritic cells transfected with antigen heat shock protein 65 (hsp65) has been tested in Wuhan4 and in Hong Kong, and differences have been found in the polarizing effect of intracellular Mycobacterium bovis Bacille Calmette–Guerin (BCG) vaccine bacteria on antigen presentation by human adult and cord blood dendritic cells.5 Various forms of recombinant BCG expressing early secreted antigen 6 of Mycobacterium tuberculosis (ESAT6),6 or antigen 85B (Ag85B) and antigen Rv3425,7 or Ag85B and ESAT6 with tumor-necrosis factor-α,8 or ESAT6 and human granulocyte macrophage-colony stimulating factor (GM-CSF)9 have shown enhanced immunogenicity. Recombinant M. smegmatis expressing M. tuberculosis culture filtrate protein 10 (CFP10)/ESAT6 fusion protein was found stimulatory for macrophage inducible nitric oxide synthetase.10 Recombinant M. smegmatis and BCG strains have been made that can express cloned antigens at a range of different levels under the control of modified FurA gene promoters.11 Other BCG recombinants expressing ESAT6,12 ESAT6/interleukin 2 (IL-2)13 or Ag85B/ESAT6 fusions14 have been made.
A range of known antigens has been tested for immunogenicity as mixtures, fusion proteins and peptides. These include chimeric Ag85B/ESAT6 with adjuvants monophosphoryl lipid A (MPL) and trehalose 6,6'-dimycolate,15 hsp16.3 with dimethyl-dioctadecyl-ammonium bromide/MPL (DDA/MPL) adjuvant,16 fusion protein M. tuberculosis protein 64 (MPT64)–ESAT6,17 resuscitation-promoting factor B (Rv1009),18 or CFP10, ESAT6 or RpfE (Rv2450) with nitrocellulose,19,20 or Rv377221 and Rv342522 with incomplete Freund's adjuvant; or Ag85B/MPT64190–198/Mtb8.4 plus a novel adjuvant of DDA with BCG extract.23 In-silico analysis of putative MHC Class 1-restricted epitopes present in antigens encoded within the region of difference 1 (RD-1) to RD-16 regions of M. bovis genome has revealed potential high-affinity HLA binders24 and profiles of human humoral responses to 38-kDa, MTB48, CFP10/ESAT6 antigens have been defined.25 Screening of human immune sera against an expression library of M. tuberculosis open reading frames revealed three novel antigens among the top 20 most strongly recognized: Rv1987, Rv3807c and Rv3887c.26
More than a dozen studies have used DNA vaccination as a means of delivering antigens in immunogenicity tests. Many have shown Th1-biased immunogenicity without additional adjuvanting, for example with Ag85B,27,28 Ag85B/ESAT6 fusion,29 ESAT6/CFP10 fusion,30 Mtb8.4/38-kDa/Ag85B fusion31 and epitopes from ESAT6, Ag85A, CFP10 and Ag85B inserted within hsp65.32 Targeting the expressed product for degradation via the ubiquitin pathway has been used to enhance MHC Class 1 presentation of epitopes from MPT64 and 38-kDa,33 MPT64,34 and ESAT6.35,36 Liposome associated Ag85A DNA vaccine was shown to be immunogenic with oral delivery.37 Enhanced responses to encoded antigens have been obtained by additionally encoding cytokines, such as interleukin 21 (IL-21), with Ag85A38 or Ag85A/ESAT6,39 and GM-CSF with Ag85A.40 Inclusion of DNA expressing IL-12 enhanced prime/boost responses to BCG and to plasmids expressing Ag85A and ESAT6.41 ESAT6 DNA priming and protein boosting has also been shown to give enhanced Th1 responses.42,43,44
TB prophylaxis
Many antigen preparations have been tested for their capacity to protect against challenge infection with virulent M. tuberculosis. Subcutaneous ESAT6/CFP10,19 or ESAT6/MPT6417,45 fusion proteins on nitrocellulose protected mice against H37Rv challenge, but not as effectively as BCG. hsp65/IL-2 fusion protein was found to elicit better protection than hsp65 given with DDA/MPL adjuvant and protection was equivalent to that produced by BCG.46 Similarly, either hspX, a dormancy associated antigen, or synthetic epitope 91–104 gave protection equivalent to BCG when given with DDA/MPL.47 Ag85B/MPT64190–198/Mtb8.4 fusion protein with DDA adjuvant boosted protection against challenge in BCG primed mice.48 A similar fusion protein in which Mtb8.4 was replaced by hspX gave a similar boost, but boosting with a mixture of the two fusion proteins was even better.49 A fusion protein of ESAT6 and Ag85A also significantly boosted protection against H37Rv in mice.50
Recombinant BCG expressing the Ag85B/MPT64190–198/Mtb8.4 fusion protein gave slightly better protection to mice against H37Rv challenge than parent BCG or BCG expressing rAg85B alone.51 Recombinant BCG expressing a fusion protein of human interleukin (hIL)-12p70 and ESAT6 showed increased immunogenicity but less protective effect.52 Recombinant Salmonella typhimurium that both expressed ESAT6/Ag85B fusion protein and delivered it as a DNA vaccine when given orogastrically gave protection similar to subcutaneous BCG and the combination was superior to either vaccine alone.53
Protection by DNA vaccination has been tested by many groups. The earliest reports indicated protection in mice superior to BCG when a divalent construct expressing both Ag85B and MPT64,54 or a mixture of plasmids expressing Ag85B, MPT64, MPT63 and ESAT654,55 was used. The protection given by a mixture of three plasmids expressing MPT83, Ag85B and ESAT6 was enhanced by including DDA adjuvant56 and an encoded fusion protein of Ag85B and MPT64 was superior to the separately encoded antigens.57,58 Encapsulation in poly(lactide-co-glycolide) microspheres with DDA enhanced the protective efficacy in mice of DNA-encoding Ag85B/MPT64/MPT83 fusion antigen,59 and strikingly the DNA mixed with DDA was superior to BCG in protecting cattle against challenge.60 Inclusion of a plasmid expressing IL-2 improved protection by this plasmid61 or by plasmid expressing Mtb8.4.62 Plasmids expressing Ag85B,28,63 Ag85B/ESAT629,64 or fusion proteins Mtb8.4/38-kDa/Ag85B31 have given protection similar to BCG in mouse model challenge infections. A mixture of plasmids encoding Ag85B, MPT64, MPT70 and TB10.4 boosted protection by BCG,65 as did a plasmid expressing a CFP21/MPT64 fusion protein.66 Ag85B or Ag85A were superior to ESAT6 when compared separately for protection as DNA vaccines.67 DNA expressing a fusion of MPB64/Ag85B/ESAT6 was superior to a mixture of plasmids expressing the separate antigens and gave protection equivalent to BCG.68 The protective effect of DNA expressing hsp65 against BCG challenge was enhanced by incorporating epitopes of ESAT6, Ag85A/B and CFP10 within the hsp65 backbone.32 The protective effect of hsp65 DNA against H37Rv challenge was increased by expression as a fusion with hIL-2, but did not surpass that of BCG.69 Expression of Ag85B fused to bovine herpes virus 1 VP22 protein, which facilitates dissemination of antigen to adjacent cells, resulted in protection against H37Rv challenge in mice that was better than protection by BCG.70 Few studies have been conducted with animals other than mice: a mixture of Ag85B, hspX and CFP10/ESAT6 fusion together with CpG and AlOH as adjuvant was immunogenic in mice but gave little protection against challenge with H37Rv in guinea pigs;71 in contrast, combined DNA vaccines encoding antigens Ag85B, MPT64 and MPT83 given with DDA appeared to be better than BCG in protecting cattle.72
TB therapy
Interest in therapeutic vaccination has been sustained by clinical studies of a commercial Chinese product, M. vaccae extract. Recent meta-analyses of published data concluded that this product gave significant benefit in preventing TB in people at high risk (13 studies),73 but there was only a minor benefit from treating new TB cases (54 studies).74 In a unique and contrasting approach, a recombinant M. smegmatis delivering DNA expressing human granulysin and murine IL-12 was recently found to be therapeutic against H37Rv infection.75
Most research into therapeutic vaccines for TB has focused on the use of naked DNA vaccination. hsp65 DNA had a significant therapeutic effect against H37Rv in mice and the fusion hsp65/IL-2 was significantly better.76 Treatment of infected mice with a DNA vaccine expressing a fusion protein of mycobacterial hsp70 and leukocyte cluster of differentiation antigen 80 substantially reduced acid-fast bacteria and pathology in liver and spleen, whereas BCG had no effect.77 Although treatment with DNA expressing Ag85B was therapeutic, treatment with DNA expressing MPT64 was not, and the mixture was less effective than the Ag85B vaccine on its own,78 and inclusion of DNA expressing IL-12 gave a slight additional benefit.79 Studies of treatment of multidrug-resistant TB in mice have given encouraging results. Mice infected with a clinical isolate resistant to isoniazid and rifampicin responded well to treatment with the drugs plus DNA expressing chimeric Ag85A/ESAT6,80 and appeared to respond better to treatment with the drugs plus DNA expressing Ag85A than to the DNA vaccine alone;81 Ag85A DNA alone was at least as effective as Ag85A plus rifampicin in treating mice infected with a strain resistant to rifampicin and isoniazid, Ag85A/ESAT6 DNA was less effective82 and Ag85A DNA worked in combination with pyrazinamide.83 An immunogenic mixture of DNA vaccines expressing Ag85B, MPT64 and MPT83 has been found to work as a potent adjunct to isoniazid plus pyrazinamide therapy in mice84 and to be therapeutic in cattle infected with M. bovis, reducing both pathology and bacterial numbers; a mixture expressing Ag85B, MPT64 and hsp65 was similarly effective.72 Inclusion of immunostimulatory nucleotide motifs in the gene transcript enhanced the therapeutic efficacy of a plasmid expressing hsp65 when tested against H37Rv in mice.85
Conclusions
It is evident in considering this body of recent TB vaccine research in China that much of it has been tactical in nature, establishing credentials both nationally and internationally, and building new research bases. Additionally, there are creative and insightful studies of particular relevance to the needs of China. Researchers are now able to exploit cutting edge technologies in designing new TB vaccines and are increasingly able to test the vaccines in relevant animal models of infection. The evidence that DNA vaccines can provide effective therapy for TB in cattle72 may be a significant pointer to the future. The potential benefits of adding immunotherapies/therapeutic vaccines to TB chemotherapy have been recognized in China, but both preventive and therapeutic approaches against human TB await development of clinical trial capacity for their proper assessment.
References
- Announcement of the national tuberculosis prevention and control plan (2001–2010). State Council of the People's Republic of China, General Office: Beijing, China, 2001. Document No. 75.
- Zhao FZ, Zhao Y, Liu XQ. Tuberculosis control in China. Tuberculosis. 2003;83:15–20. doi: 10.1016/s1472-9792(02)00074-4. [DOI] [PubMed] [Google Scholar]
- Wang LD, Liu JJ, Chin DP. Progress in tuberculosis control and the evolving public-health system in China. The Lancet. 2007;369:691–696. doi: 10.1016/S0140-6736(07)60316-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei YZ, Liu SW, Xia F. Initial research of dendritic cell vaccine against tuberculosis. Med J Wuhan Univ. 2005;26:747–752. [Google Scholar]
- Liu EM, Law HK, Lau YL. Mycobacterium bovis bacillus Calmette–Guerin treated human cord blood monocyte-derived dendritic cells polarize naive T cells into a tolerogenic phenotype in newborns. World J Pediat. 2010;6:132–140. doi: 10.1007/s12519-010-0019-0. [DOI] [PubMed] [Google Scholar]
- Wang LM, Shi CH, Fan XL, Xue Y, Bai YL, Xu ZK. Expression and immunogenicity of recombinant Mycobacterium bovis bacillus Calmette–Guerin strains secreting the antigen ESAT-6 from Mycobacterium tuberculosis. Chin Med J (Engl) 2007;120:1220–1225. [PubMed] [Google Scholar]
- Wang JL, Qie YQ, Zhu BD, et al. Evaluation of a recombinant BCG expressing antigen Ag85B and PPE protein Rv3425 from DNA segment RD11 of Mycobacterium tuberculosis in C57BL/6 mice. Med Microbiol Immunol (Berl) 2009;198:5–11. doi: 10.1007/s00430-008-0098-x. [DOI] [PubMed] [Google Scholar]
- Shen HB, Wang C, Yang EZ, et al. Novel recombinant BCG coexpressing Ag85B, ESAT-6 and mouse TNF-alpha induces significantly enhanced cellular immune and antibody responses in C57BL/6 mice. Microbiol Immunol. 2010;54:435–441. doi: 10.1111/j.1348-0421.2010.00232.x. [DOI] [PubMed] [Google Scholar]
- Yang XL, Bao L, Deng YH. A novel recombinant Mycobacterium bovis bacillus Calmette–Guerin strain expressing human granulocyte macrophage colony-stimulating factor and Mycobacterium tuberculosis early secretory antigenic target 6 complex augments Th1 immunity. Acta Biochim Biophys Sin. 2011;43:511–518. doi: 10.1093/abbs/gmr045. [DOI] [PubMed] [Google Scholar]
- Li Y, Bao L, Zhang HD, Shang ZL, Zhong Q, Li YS. Expression of M. tuberculosis CFP-10/ESAT-6 fusion gene in M. smegmatis and its immunogenicity. Chin J Med Microbiol. 2006;26:1076–1079. [Google Scholar]
- Fan XY, Ma H, Guo J, et al. A novel differential expression system for gene modulation in Mycobacteria. Plasmid. 2009;61:39–46. doi: 10.1016/j.plasmid.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Zhang LX, Wu XQ, Dong EJ. Construction and identification of ESAT6 recombinant BCG vaccine. J Pract Med. 2009;25:517–520. [Google Scholar]
- Fan XF, Wang LM, Lu XY, Tu ZG, Shi CH, Xu ZK. Cloning and expression of the fusion protein of interleukin-2 and ESAT6 in Mycobacterium bovis Bacillus Calmette Guerin strain. Chin Med J (Engl) 2005;118:762–765. [PubMed] [Google Scholar]
- Shi CH, Xu ZK, Zhu DS, Li Y, Bai YL, Xue Y. Screening and construction of recombinant BCG strains expressing the Ag85B–ESAT6 fusion protein. Chin J Tuberculosis Respir Dis. 2005;28:254–257. [PubMed] [Google Scholar]
- Xu Y, Wang B, Chen J, et al. Chimaeric protein improved immunogenicity compared with fusion protein of Ag85B and ESAT-6 antigens of Mycobacterium tuberculosis. . Scand J Immunol. 2006;64:476–481. doi: 10.1111/j.1365-3083.2006.01812.x. [DOI] [PubMed] [Google Scholar]
- Shi CH, Zhang TF, Zhu DS, et al. The Immunological response induced by Mycobacterium tuberculosis heat shock protein 16.3 and its synthetic peptide in mice. Chin J Tuberculosis Respir Dis. 2009;32:603–607. [PubMed] [Google Scholar]
- Shi CH, An JZ, Tang XF, et al. Immune responses and protective efficacy induced in mice by Mycobacterium tuberculosis MPT64–ESAT-6 fusion protein. J 4th Mil Med Univ. 2006;27:769–771. [Google Scholar]
- Fan AL, Shi CH, Su MQ, et al. Immunological properties of Rv1009 domain from Mycobacterium tuberculosis. . Chin J Lab Med. 2007;31:1282–1286. [Google Scholar]
- Zhang H, Shi CH, Xue Y, Bai YL, Wang LM, Xu ZK. Immune response and protective efficacy induced by fusion protein ESAT6–CFP10 of M. tuberculosis in mice. Chin J Cell Molec Immunol. 2006;22:443–446. [PubMed] [Google Scholar]
- Xue Y, Bai YL, Gao H, Wang LM, Xu ZK. Immune responses induced by Mycobacterium tuberculosis Rv2450 protein in mice. Chin J Cell Molec Immunol. 2007;23:921–923. [PubMed] [Google Scholar]
- Zhang M, Xu Y, Qie YQ, et al. Humoral and cellulr immune responses in mice induced by trehalose-6-phosphate phosphatase from Mycobacterium tuberculosis. . J Microbes Infect. 2006;1:144–148. [Google Scholar]
- Wang JL, Qie YQ, Zhang HM, et al. PPE protein (Rv3425) from DNA segment RD11 of Mycobacterium tuberculosis: a novel immunodominant antigen of Mycobacterium tuberculosis induces humoral and cellular immune responses in mice. Microbiol Immunol. 2008;52:224–230. doi: 10.1111/j.1348-0421.2008.00029.x. [DOI] [PubMed] [Google Scholar]
- Song NN, Wang BX, Shi DS, et al. Dimethyldioctyl ammonium bromide-BCG polysaccharide nucleic acid adjuvant enhanced the immunogenicity of a Mycobacterium tuberculosis subunit vaccine. Chin J Tuberculosis Respir Dis. 2009;32:513–516. [PubMed] [Google Scholar]
- Wang JL, Zhang HM, Wang HH. Analysis of predicted CD8+ T cell epitopes from proteins encoded by the specific RD regions of Mycobacterium tuberculosis for vaccine development and specific diagnosis. Mol Biol Rep. 2010;37:1793–1799. doi: 10.1007/s11033-009-9613-4. [DOI] [PubMed] [Google Scholar]
- Wu XQ, Yang YR, Zhang JX, et al. Humoral Immune Responses against the Mycobacterium tuberculosis 38-Kilodalton, MTB48, and CFP-10/ESAT-6 Antigens in Tuberculosis. Clin Vacc Immunol. 2010;17:372–375. doi: 10.1128/CVI.00287-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li YQ, Zeng JM, Shi JF, et al. A Proteome-scale identification of novel antigenic proteins in Mycobacterium tuberculosis toward diagnostic and vaccine development. J Proteome Res. 2010;9:4812–4822. doi: 10.1021/pr1005108. [DOI] [PubMed] [Google Scholar]
- You L, Zhao Y, Gao CH. Construction of Ag85B DNA vaccine for Mycobacterium tuberculosis and its immunogenicities. Chin J Tuberculosis Respir Dis. 2001;24:736–739. [PubMed] [Google Scholar]
- Hu J, Wu XQ, Wang LH, Zheng Y. The construction, immunogenicity and protective efficacy of tuberculosis Ag85B DNA vaccine. Sci Technol Eng. 2006;6:1765–1771. [Google Scholar]
- Shi CH, Wang XW, Zhang H, Xu ZK, Li Y, Yuan LT. Immune responses and protective efficacy induced by 85B antigen and early secreted antigenic target-6 kDa antigen fusion protein secreted by recombinant bacille Calmette–Guerin. Acta Biochim Biophys Sin. 2007;39:290–296. doi: 10.1111/j.1745-7270.2007.00281.x. [DOI] [PubMed] [Google Scholar]
- Zhang H, Shi CH, Wang LM, Xue Y, Bai YL, Xu ZK. Immunogenicity of DNA vaccine expressing ESAT6–CFP10 fusion protein of Mycobacterium tuberculosis. . J 4th Mil Med Univ. 2007;28:489–492. [Google Scholar]
- Liu JB, Zhu ZY, Wang HB. Y X, Zhang CF, Zhang Y. Construction and immunoprotection of the TB DNA vaccine expressing Mycobacterium tuberculosis Mtb8.4–38000–Ag85B fusion protein. Immunological J. 2006;22:47–50. [Google Scholar]
- Gao HF, Yue Y, Hu LK, Xu W, Xiong SD. A novel DNA vaccine containing multiple TB-specific epitopes casted in a natural structure (ECANS) confers protective immunity against pulmonary mycobacterial challenge. Vaccine. 2009;27:5313–5319. doi: 10.1016/j.vaccine.2009.06.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang QM, Sun SH, Hu ZL, et al. Epitope DNA vaccines against tuberculosis: spacers and ubiquitin modulates cellular immune responses elicited by epitope DNA vaccine. Scand J Immunol. 2004;60:219–225. doi: 10.1111/j.0300-9475.2004.01442.x. [DOI] [PubMed] [Google Scholar]
- Wang QM, Sun SH, Kang L. Construction of ubiquitin-Mycobacterium tuberculosis PMT64 fusion gene DNA vaccine and its cellular immunological efficacy in mice. Acad J 2nd Mil Med Univ. 2007;29:117–121. [Google Scholar]
- Wang QM, Yin M, Zhang JC, Hu JQ, He Y, Sun SH. Ubiquitin and ESAT6 antigen fusion gene DNA vaccine induced stronger cellular immune response in mice. Acad J 2nd Mil Med Univ. 2007;28:261–265. [Google Scholar]
- Wang QM, Kang L, Wang XH. Improved cellular immune response elicited by a ubiquitin-fused ESAT-6 DNA vaccine against Mycobacterium tuberculosis. . Microbiol Immunol. 2009;53:384–390. doi: 10.1111/j.1348-0421.2009.00138.x. [DOI] [PubMed] [Google Scholar]
- Wang DA, Xu J, Feng YH, et al. Liposomal oral DNA vaccine (mycobacterium DNA) elicits immune response. Vaccine. 2010;28:3134–3142. doi: 10.1016/j.vaccine.2010.02.058. [DOI] [PubMed] [Google Scholar]
- Dou J, Tang Q, Zhao FS, et al. Comparison of immune responses induced in mice by vaccination with DNA vaccine constructs expressing mycobacterial antigen 85A and interleukin-21 and bacillus Galmette–Guerin. Immunol Invest. 2008;37:113–127. doi: 10.1080/08820130701690741. [DOI] [PubMed] [Google Scholar]
- Li JL, Yu FL, Wang YQ, et al. Constructing nucleic acid vaccine expressing fusion antigens of Mycobacterium tuberculosis Ag85A and ESAT-6, and interleukin 21 as well as studying its immune effect in mice. Lett Biotech. 2009;20:765–768. [Google Scholar]
- Dou J, Tang Q, Yu FL, et al. Investigation of immunogenic effect of the BCG priming and Ag85A–GM-CSF boosting in Balb/c mice model. Immunobiol. 2010;215:133–142. doi: 10.1016/j.imbio.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Bao L, Gao L, Bao Y. Immunogenicity of interleukin 12 and DNA vaccine prime-BCG boost against Mycobacterium tuberculosis. Int J Infect Dis. 2010;14:e446. [PubMed] [Google Scholar]
- Wang QM, Sun SH, Hu ZL, Yin M, Xiao CJ, Zhang JC. Improved immunogenicity of a tuberculosis DNA vaccine encoding ESAT6 by DNA priming and protein boosting. Vaccine. 2004;22:3622–3627. doi: 10.1016/j.vaccine.2004.03.029. [DOI] [PubMed] [Google Scholar]
- Li ZM, Song D, Zhang HY, et al. Improved humoral immunity against tuberculosis ESAT-6 antigen by chimeric DNA prime and protein boost strategy. DNA Cell Biol. 2006;25:25–30. doi: 10.1089/dna.2006.25.25. [DOI] [PubMed] [Google Scholar]
- Li ZM, Zhang HY, Fan XY, et al. DNA electroporation prime and protein boost strategy enhances humoral immunity of tuberculosis DNA vaccines in mice and non-human primates. Vaccine. 2006;24:4565–4568. doi: 10.1016/j.vaccine.2005.08.021. [DOI] [PubMed] [Google Scholar]
- Bai Y, Xue Y, Gao H, et al. Expression and purification of Mycobacterium tuberculosis ESAT-6 and MPT64 fusion protein and its immunoprophylactic potential in mouse model. Protein Expr Purif. 2008;59:189–196. doi: 10.1016/j.pep.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Shi C, Yuan S, Zhang H, Zhang T, Wang L, Xu Z. Cell-mediated immune responses and protective efficacy against infection with Mycobacterium tuberculosis induced by hsp65 and hIL-2 fusion protein in mice. Scand J Immunol. 2009;69:140–149. doi: 10.1111/j.1365-3083.2008.02207.x. [DOI] [PubMed] [Google Scholar]
- Shi C, Zhang H, Zhang T, et al. New alternative vaccine component against Mycobacterium tuberculosis-heat shock protein 16.3 or its T-cell epitope. Scand J Immunol. 2009;70:465–474. doi: 10.1111/j.1365-3083.2009.02325.x. [DOI] [PubMed] [Google Scholar]
- Luo Y, Wang BX, Hu LN, et al. Fusion protein Ag85B–MPT64190–198–Mtb8.4 has higher immunogenicity than Ag85B with capacity to boost BCG-primed immunity against Mycobacterium tuberculosis in mice. Vaccine. 2009;27:6179–6185. doi: 10.1016/j.vaccine.2009.08.018. [DOI] [PubMed] [Google Scholar]
- Li Q, Yu H, Zhang Y, et al. Immunogenicity and protective efficacy of a fusion protein vaccine consisting of antigen Ag85B and HspX against Mycobacterium tuberculosis infection in mice. Scand J Immunol. 2011;73:568–576. doi: 10.1111/j.1365-3083.2011.02531.x. [DOI] [PubMed] [Google Scholar]
- Lu J, Wang C, Zhou ZG, et al. Immunogenicity and protective efficacy against murine tuberculosis of a prime-boost regimen with BCG and a DNA vaccine expressing ESAT-6 and Ag85A fusion protein. Clin Dev Immunol. 2011;2011:617892. doi: 10.1155/2011/617892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qie YQ, Wang JL, Liu W, et al. More vaccine efficacy studies on the recombinant bacille Calmette–Guerin Co-expressing Ag85B, Mpt64190–198 and Mtb8.4. Scand J Immunol. 2009;69:342–350. doi: 10.1111/j.1365-3083.2009.02231.x. [DOI] [PubMed] [Google Scholar]
- Deng YH, Bao L, Yang XL. Evaluation of immunogenicity and protective efficacy against Mycobacterium tuberculosis infection elicited by recombinant Mycobacterium bovis BCG expressing human Interleukin-12p70 and Early Secretory Antigen Target-6 fusion protein. Microbiol Immunol. 2011;55:798–808. doi: 10.1111/j.1348-0421.2011.00376.x. [DOI] [PubMed] [Google Scholar]
- Wang QL, Pan Q, Ma YF, et al. An attenuated Salmonella-vectored vaccine elicits protective immunity against Mycobacterium tuberculosis. . Vaccine. 2009;27:6712–6722. doi: 10.1016/j.vaccine.2009.08.096. [DOI] [PubMed] [Google Scholar]
- Tian X, Cai H, Zhu YX. Protection of mice with a divalent tuberculosis DNA vaccine encoding antigens Ag85B and MPT64. Acta Biochim Biophys Sin (Shanghai) 2004;36:269–276. doi: 10.1093/abbs/36.4.269. [DOI] [PubMed] [Google Scholar]
- Cai H, Tian X, Hu XD, et al. Immunogenicity and protective efficacy study using combination of four tuberculosis DNA vaccines. Sci China Ser C-Life Sci. 2003;46:495–498. doi: 10.1360/02yc0121. [DOI] [PubMed] [Google Scholar]
- Cai H, Tian X, Hu XD, Zhuang YH, Zhu YX. Combined DNA vaccines formulated in DDA enhance protective immunity against tuberculosis. DNA Cell Biol. 2004;23:450–456. doi: 10.1089/1044549041474742. [DOI] [PubMed] [Google Scholar]
- Luo XD, Zhu DY, Chen Q, Jiang Y, Jiang S, Yang CS. A study of the protective effect of the DNA vaccine encoding tubercle antigen 85B with MPT64 in mice challenged with Mycobacterium tuberculosis. . Chin J Tuberculosis Respir Dis. 2004;27:611–616. [PubMed] [Google Scholar]
- Luo XD, Zhu DY, Jiang S, Chen Q, Jiang Y. The estimation of protective efficacy of the fusion gene vaccine encoding tubercle antigen 85B and MPT64 in mice challenged with Mycobacterium tuberculosis. . Natl Med J Chin. 2004;84:687–691. [PubMed] [Google Scholar]
- Cai H, Hu XD, Yu DH, Li SX, Tian X, Zhu YX. Combined DNA vaccine encapsulated in microspheres enhanced protection efficacy against Mycobacterium tuberculosis infection of mice. Vaccine. 2005;23:4167–4174. doi: 10.1016/j.vaccine.2005.03.024. [DOI] [PubMed] [Google Scholar]
- Cai H, Tian X, Hu XD, Li SX, Yu DH, Zhu YX. Combined DNA vaccines formulated either in DDA or in saline protect cattle from Mycobacterium bovis infection. Vaccine. 2005;23:3887–3895. doi: 10.1016/j.vaccine.2005.03.025. [DOI] [PubMed] [Google Scholar]
- Cai H, Yu DH, Tian X, Zhu YX. Coadministration of interleukin 2 plasmid DNA with combined DNA vaccines significantly enhances the protective efficacy against Mycobacterium tuberculosis. . DNA Cell Biol. 2005;24:605–613. doi: 10.1089/dna.2005.24.605. [DOI] [PubMed] [Google Scholar]
- Zhu ZY, Xie Y, Wang HB, et al. Protective efficacy of co-immunization of T DNA vaccine pVS84 and plasmid pIL2 equivalent to that of BCG. Chin J Zoonoses. 2006;22:318–321. [Google Scholar]
- Liu JB, Zhu ZY, Wang HB, Xie Y, Zhang CF, Zhang Y. Construction of the eukaryotic expression plasmid pVS85B expressing the protective antigen Ag85B of Mycobacterium tuberculosis and its immunoprotective studies. Curr Immunol. 2006;26:121–126. [Google Scholar]
- Shi CH, Wang XW, Zhang H, Zhang TF, Wang LM, Xu ZK. Immune responses and protective efficacy of the gene vaccine expressing Ag85B and ESAT6 fusion protein from Mycobacterium tuberculosis. DNA Cell Biol. 2008;27:199–207. doi: 10.1089/dna.2007.0648. [DOI] [PubMed] [Google Scholar]
- Li M, Yu DH, Cai H. DNA prime-BCG boost vaccination strategy improved the protective efficacy against M-tuberculosis H37Rv in mice. Prog Biochem Biophys. 2007;34:746–753. [Google Scholar]
- Wang C, Chen ZH, Fu RL, et al. A DNA vaccine expressing CFP21 and MPT64 fusion protein enhances BCG-induced protective immunity against Mycobacterium tuberculosis infection in mice. Med Microbiol Immunol (Berl) 2011;200:165–175. doi: 10.1007/s00430-011-0188-z. [DOI] [PubMed] [Google Scholar]
- Fan XL, Gao Q, Fu RL. Differential immunogenicity and protective efficacy of DNA vaccines expressing proteins of Mycobacterium tuberculosis in a mouse model. Microbiol Res. 2009;164:374–382. doi: 10.1016/j.micres.2007.04.006. [DOI] [PubMed] [Google Scholar]
- Liu SG, Gong Q, Wang CL, et al. A novel DNA vaccine for protective immunity against virulent Mycobacterium bovis in mice. Immunol Lett. 2008;117:136–145. doi: 10.1016/j.imlet.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Wang LM, Bai YL, Shi CH, et al. Immunogenicity and protective efficacy of a DNA vaccine encoding the fusion protein of mycobacterium heat shock protein 65 (Hsp65) with human interleukin-2 against Mycobacterium tuberculosis in BALB/c mice. APMIS. 2008;116:1071–1081. doi: 10.1111/j.1600-0463.2008.01095.x. [DOI] [PubMed] [Google Scholar]
- Yao WH, Liu SW, Qu XJ, Xiao SB, Liu Y, Liu JY. Enhanced immune response and protection efficacy of a DNA vaccine constructed by linkage of the Mycobacterium tuberculosis Ag85B-encoding gene with the BVP22-encoding gene. J Med Microbiol. 2009;58:462–468. doi: 10.1099/jmm.0.004267-0. [DOI] [PubMed] [Google Scholar]
- Chen L, Xu M, Wang ZY, et al. The development and preliminary evaluation of a new Mycobacterium tuberculosis vaccine comprising Ag85b, HspX and CFP-10:ESAT-6 fusion protein with CpG DNA and aluminum hydroxide adjuvants. FEMS Immunol Med Microbiol. 2010;59:42–52. doi: 10.1111/j.1574-695X.2010.00660.x. [DOI] [PubMed] [Google Scholar]
- Hu XD, Chen ST, Yu DH, Li SX, Cai H. Immunotherapy with combined DNA vaccines is an effective treatment for M. bovis infection in cattle. Vaccine. 2009;27:1317–1322. doi: 10.1016/j.vaccine.2008.12.055. [DOI] [PubMed] [Google Scholar]
- Yang XY, Chen QF, Cui XH, Yu Y, Li YP. Mycobacterium vaccae vaccine to prevent tuberculosis in high risk people: a meta-analysis. J Infect. 2010;60:320–330. doi: 10.1016/j.jinf.2010.02.005. [DOI] [PubMed] [Google Scholar]
- Yang XY, Chen QF, Li YP, Wu SM. Mycobacterium vaccae as adjuvant therapy to antituberculosis chemotherapy in never-treated tuberculosis patients: a meta-analysis. Plos One. 2011;6:e23826. doi: 10.1371/journal.pone.0023826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C, He YL, Zhang L, et al. GLS/IL-12-modified Mycobacterium smegmatis as a novel anti-tuberculosis immunotherapeutic vaccine. Int J Tuberc Lung Dis. 2009;13:1360–1366. [PubMed] [Google Scholar]
- Shi CH, Zhang H, Wang LM, et al. Therapeutic efficacy of a tuberculosis DNA vaccine encoding heat shock protein 65 of Mycobacterium tuberculosis and the human interleukin 2 fusion gene. Tuberculosis. 2009;89:54–61. doi: 10.1016/j.tube.2008.09.005. [DOI] [PubMed] [Google Scholar]
- Shi XL, Li HW, Zhong S. Study on the role of the chimerichsp70/CD80 DNA vaccine for treating infection of Mycobacterium tuberculosis. . Chin J Infect Dis. 2004;22:30–33. [Google Scholar]
- Zhu DY, Jiang S, Luo XD. Therapeutic effects of Ag85B and MPT64 DNA vaccines in a murine model of Mycobacterium tuberculosis infection. Vaccine. 2005;23:4619–4624. doi: 10.1016/j.vaccine.2005.05.035. [DOI] [PubMed] [Google Scholar]
- Jiang S, Zhu DY, Luo XD, Jiang Y, Chen Q.Therapeutic effects of DNA vaccines in a murine model of Mycobacterium tuberculosis infection Zhonghua Jie He He Hu Xi Za Zhi 28305–309.Chinese. [PubMed] [Google Scholar]
- Liang Y, Wu XQ, Zhang JX. Therapeutic effects of chimeric Ag85A/ESAT-6 DNA vaccines combined with chemotherapy in a mouse model infected with multi-drug resistant Mycobacterium tuberculosis. . J Chin Antituberc Assoc. 2007;29:382–385. [Google Scholar]
- Liang Y, Wu XQ, Zhang JX. Therapeutic effects of Ag85A DNA vaccines combined with chemotherapy in a mouse model of MDR Mycobacterium tuberculosis infection. Guangdong Med J. 2007;28:1398–1400. [Google Scholar]
- Liang Y, Wu XQ, Zhang JX, et al. The treatment of mice infected with multi-drug-resistant Mycobacterium tuberculosis using DNA vaccines or in combination with rifampin. Vaccine. 2008;26:4536–4540. doi: 10.1016/j.vaccine.2008.06.066. [DOI] [PubMed] [Google Scholar]
- Liang Y, Wu X, Zhang J, et al. Treatment of multi-drug-resistant tuberculosis in mice with DNA vaccines alone or in combination with chemotherapeutic drugs. Scand J Immunol. 2011;74:42–46. doi: 10.1111/j.1365-3083.2011.02538.x. [DOI] [PubMed] [Google Scholar]
- Yu DH, Hu XD, Cai H. Efficient tuberculosis treatment in mice using chemotherapy and immunotherapy with the combined DNA vaccine encoding Ag85B, MPT-64 and MPT-83. Gene Ther. 2008;15:652–659. doi: 10.1038/gt.2008.13. [DOI] [PubMed] [Google Scholar]
- Wu J, Ma H, Qu Q, et al. Incorporation of immunostimulatory motifs in the transcribed region of a plasmid DNA vaccine enhances Th1 immune responses and therapeutic effect against Mycobacterium tuberculosis in mice. Vaccine. 2011;29:7624–7630. doi: 10.1016/j.vaccine.2011.08.020. [DOI] [PubMed] [Google Scholar]