Abstract
Oral bisphosphonates reduce fracture risk in osteoporotic patients but are often associated with poor compliance, which may impair their antifracture effects. This post-hoc analysis assessed the time-to-onset and persistence of the antifracture effect of zoledronic acid, a once-yearly bisphosphonate infusion, in women with osteoporosis.
Data from 9355 women who were randomized in two placebo-controlled pivotal trials were included. Endpoints included reduction in the rate of any clinical fracture at 6, 12, 18, 24, and 36 months in the zoledronic acid group compared with placebo, and the year-by-year incidence of all clinical fractures over 3 years. Cox proportional hazards regression was used to determine the timing of onset of antifracture efficacy. A generalized estimating equation model was used to assess fracture reduction for the 3 consecutive years of treatment, thereby evaluating persistence of effect. Safety results from women in the two studies were collated. Zoledronic acid reduced the risk of all clinical fractures at 12 months (hazard ratio, 0.75; 95% confidence interval [CI], 0.61–0.92; p=0.0050) with significant reductions maintained at all subsequent timepoints. Year-by-year analysis showed that zoledronic acid reduced the risk for all clinical fractures compared with the placebo group in each of the 3 years (year 1: odds ratio [OR], 0.74, 95% CI, 0.60–0.91, p=0.0044; year 2: OR, 0.53, 95% CI, 0.42–0.66, p<0.0001; year 3: OR, 0.61, 95% CI, 0.48–0.77, p<0.0001). This antifracture effect was persistent over 3 years, with the reductions in year 2 and 3 slightly larger than in year 1 (p=0.097).
This analysis shows that zoledronic acid offers significant protection from clinical fractures as early as 12 months. When administered annually, its beneficial effects persist for at least 3 years.
Keywords: fractures, postmenopausal osteoporosis, reaction time, zoledronic acid, bone mineral density
Introduction
Oral bisphosphonates, which are frequently used for the treatment of osteoporosis, have been widely shown to provide fracture protection for women with osteoporosis.(1-6) However, the dosing requirements associated with oral administration of these drugs may reduce patient compliance, thereby affecting the time-to-onset and the persistence of antifracture effect.(7,8) Clinical studies have shown that oral bisphosphonates can reduce fracture risk within 1 year of initiation of therapy. Risedronate significantly reduced vertebral and nonvertebral fracture risk within 6 months of initiation,(6,9) and alendronate significantly reduced the risk of clinical vertebral, any clinical and nonvertebral fractures within 12, 18 and 24 months, respectively.(5) These results, however, are taken from clinical trials, where treatment compliance is higher than in real-world settings. The time-to-onset of these therapies in clinical practice may, therefore, be different.
A waning of the antifracture effect with oral bisphosphonates over time may also be due to poor compliance. Studies have shown that compliance with daily, weekly or monthly oral bisphosphonate treatment was suboptimal even after one year of treatment.(10,11) Given that poor compliance is associated with increased fracture risk,(10,11) it is possible that some patients prescribed with an oral bisphosphonate may experience a decline in fracture protective effect over time. With strontium ranelate, there were numerical between-year differences in fracture risk reductions over the Spinal Osteoporosis Therapeutic Intervention (SOTI) study period, suggesting a potential waning of antifracture effect over time.(13) Nevertheless, year-by-year analyses have not been published for any of these therapies and no conclusions can be drawn about potential loss of efficacy associated with suboptimal adherence.
Zoledronic acid is a bisphosphonate that is administered once yearly, by intravenous infusion. The antifracture efficacy of zoledronic acid has been demonstrated in the Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly Pivotal Fracture Trial (HORIZON-PFT) and the HORIZON Recurrent Fracture Trial (HORIZON-RFT), which showed that zoledronic acid 5 mg significantly reduced fracture risk in postmenopausal women with osteoporosis and in men and women with prior low-trauma hip fracture.(14,15) However, neither of these studies investigated the time-to-onset or the year-by-year antifracture effect of zoledronic acid. This analysis pooled data from all female patients in the HORIZON-PFT and -RFT to examine the time-to-onset of antifracture efficacy with zoledronic acid and to evaluate the persistence of this effect, by analyzing the incidence of clinical fractures within each year of treatment.
Methods
Study design and patients
We performed a pooled post-hoc analysis of data from all women who were randomized in the multinational randomized, double-blind, placebo-controlled HORIZON-PFT and HORIZON-RFT. Full methods have been published previously(14,15) but are summarized here in brief. The HORIZON-PFT enrolled postmenopausal women aged 65–89 years who had either a femoral neck T-score ≤–2.5 or a T-score ≤–1.5 plus radiological evidence of at least two mild or one moderate vertebral fracture at baseline.(14) HORIZON-RFT enrolled patients aged ≥50 years who had undergone surgical repair of a hip fracture that had been sustained with minimal trauma (i.e. a fall from standing height or lower) in the previous 90 days.(15) Previous use of bisphosphonates with sufficient washout was permitted.
In each study, patients received a 15-minute intravenous infusion of zoledronic acid 5 mg or placebo. In the HORIZON-PFT, treatments were administered at baseline, 12 and 24 months, and patients monitored for a total of 3 years.(14) In the HORIZON-RFT, treatments were administered within 90 days after surgical repair of the hip fracture and every 12 months thereafter for the duration of the study (median duration of follow-up, 1.9 years).(15) Patients also received supplemental calcium and vitamin D for the duration of the trial in which they were enrolled.
Both studies were reviewed by the Independent Ethics Committee or Institutional Review Board at each participating centre and were conducted according to the ethical principles of the Declaration of Helsinki (1989)(16) and local applicable laws and regulations. Informed consent was obtained from all patients.
Endpoints for this analysis
The endpoints for the time-to-onset of antifracture effect analysis were the cumulative reductions in the rate of any clinical, clinical vertebral and nonvertebral fracture (excluding facial/skull and digital fractures [fractures due to excessive trauma were also excluded in subjects enrolled in the HORIZON-PFT]) at 6, 12, 18, 24, and 36 months in the zoledronic acid group compared with the placebo group.
The endpoints of the persistence of effect analysis were the year-by-year incidence of these three fracture types over 3 years. Criteria for fracture classification have been defined previously.(14,15) Year-by-year incidence of morphometric vertebral fractures was also analysed for patients in the HORIZON-PFT. Definition of an incident morphometric vertebral fracture was described previously.(14)
Statistical analysis
Efficacy
Time-to-onset of antifracture effect
Kaplan-Meier analysis was used to determine the cumulative proportion of patients with each type of fracture at individual timepoints. A Cox proportional hazards regression model, stratified by study (HORIZON-PFT or HORIZON-RFT), was used to determine the statistical significance at each timepoint (6, 12, 18, 24, or 36 months) of the between-treatment difference in the cumulative incidence of each category of fracture (any clinical fracture, clinical vertebral fracture, nonvertebral fracture). The time-to-onset was defined as the first timepoint at which results showed a significant difference between treatment groups (at p<0.05). Additional analyses adjusted for age and number of infusions were also performed to account for differences between the HORIZON-PFT and HORIZON-RFT. All patients were included at all timepoints.
Persistence of antifracture effect
Persistence of antifracture effect over time was investigated by determining the incidence of each type of fracture (any clinical, clinical vertebral or nonvertebral, morphometric vertebral) in each treatment group within each year of the studies (years 1, 2, and 3). Determination of fracture incidence was subject to the following rules to ensure that the data were not cumulative:
A patient who experienced a new fracture in more than 1 year was recorded in each of those years;
A patient who experienced multiple fractures within the same year was recorded only once in that year;
A patient who experienced a fracture in 1 year of the study but not in a subsequent year was recorded only in the year in which the patient fractured.
The clinical fracture (any clinical, clinical vertebral or nonvertebral fractures, excluding facial/skull and digital fractures [fractures due to excessive trauma were also excluded in subjects enrolled in the HORIZON-PFT]) incidence data were evaluated using a generalized estimating equation model with study, treatment, year, and treatment-by-year interaction as factors. Additional analyses adjusted for age and number of infusions were also performed to account for differences between the HORIZON-PFT and HORIZON-RFT. The morphometric vertebral fracture incidence data from in the HORIZON-PFT were evaluated using a generalized estimating equation model with prevalent fracture status, treatment, year, and treatment-by-year interaction as factors. All patients were included up to the time of last visit. The treatment-by-year interaction p-value assessed the year-by-year difference of treatment effect (with p<0.1 indicating a possible interaction). The generalized estimating equation model was also used to generate an estimate of the odds ratio for fracture (zoledronic acid vs. placebo) for each year of the study. Compound symmetry was assumed for the error structure of this study.
Results
Data from 9355 women were included in the analysis, including 1619 women who were randomized in the HORIZON-RFT and 7736 postmenopausal women who were randomized in the HORIZON-PFT. Baseline characteristics were similar between treatment groups in both the HORIZON-PFT and -RFT (Table 1).
Table 1.
Baseline patient characteristics and demographics in HORIZON-PFT patients and in female patients enrolled in the HORIZON-RFT
| HORIZON-PFT* | HORIZON-RFT | |||
|---|---|---|---|---|
|
|
||||
| Variable | Placebo, N=3861 |
Zoledronic acid, N=3875 |
Placebo, N=802 |
Zoledronic acid, N=817 |
| Age, years ±SD | 73.0±5.40 | 73.1±5.34 | 75.2±9.60 | 75.0±9.15 |
|
Body mass index,
kg/m2±SD |
25.4±4.3 | 25.1±4.3 | 24.8±4.57 | 24.8±4.48 |
| Region, n (%) | ||||
| Western Europe | 1162 (30.1) | 1160 (29.9) | 270 (33.7) | 279 (34.1) |
| Eastern Europe | 772 (20.0) | 774 (20.0) | 195 (24.3) | 210 (25.7) |
| North America | 765 (19.8)† | 766 (19.8)† | 229 (28.5) | 216 (26.4) |
| Latin America | 622 (16.1) | 625 (16.1) | 108 (13.5) | 112 (13.7) |
| Asia | 540 (14.0) | 550 (14.2) | NA | NA |
| Femoral neck T-score, n (%) | ||||
| ≤−2.5 | 2734 (70.8) | 2814 (72.6) | 342 (42.6) | 354 (43.3) |
| >2.5 to −1.5 | 1073 (27.8) | 1002 (25.9) | 277 (34.5) | 269 (32.9) |
| >1.5 | 38 (1.0) | 35 (0.9) | 84 (10.5) | 91 (11.1) |
| Missing | 16 (0.4) | 24 (0.6) | 99 (12.3) | 103 (12.6) |
29 patients from the HORIZON-PFT were excluded from this pooled analysis as they were enrolled at a site whose participation was terminated during the study.
Plus Oceania.
BMD, bone mineral density; HORIZON-PFT, Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly Pivotal Fracture Trial; HORIZON-RFT, Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly Recurrent Fracture Trial; NA, not applicable; SD, standard deviation.
Time-to-onset of antifracture effect
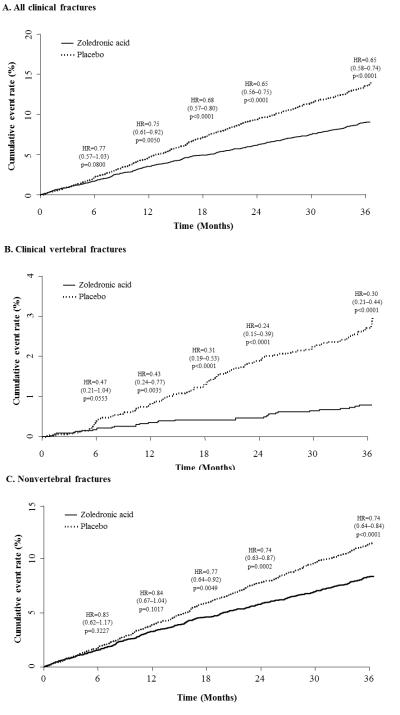
The risk of any clinical fracture was significantly reduced with zoledronic acid treatment at 12 months (hazard ratio [HR], 0.75; 95% confidence interval [CI], 0.61–0.92; p=0.0050). This significant fracture risk reduction was maintained at all subsequent time points (Figure 1A). There was also a trend towards a reduction in risk after 6 months (HR, 0.77; 95% CI, 0.57–1.03; p=0.0800).
Figure 1.
Kaplan-Meier plots of cumulative all clinical (A), clinical vertebral (B) and nonvertebral fracture (C) event rates from month 0 to month 36 in female patients in HORIZON-PFT and HORIZON-RFT.
Bracketed values are 95% confidence intervals.
HORIZON-PFT, Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly Pivotal Fracture Trial; HORIZON-RFT, Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly Recurrent Fracture Trial; HR, hazard ratio; PBO, placebo; ZOL, zoledronic acid.
The pattern of risk for clinical vertebral fractures was similar to that for any clinical fracture, with a significant reduction evident at month 12 (HR, 0.43; 95% CI, 0.24–0.77; p=0.0035) (Figure 1B), and a trend towards reduction in risk at 6 months (HR, 0.47; 95% CI, 0.21–1.04; p=0.0553).
A trend towards a reduction in nonvertebral fracture risk was evident from 6 months onwards but this did not become statistically significant until 18 months after treatment initiation (HR, 0.77; 95% CI, 0.64–0.92; p=0.0049; Figure 1C).
Similar results were seen for additional analyses adjusted for age and number of infusions. Significant fracture risk reductions with zoledronic acid were seen at 12 months for any clinical fractures (p=0.0039) and clinical vertebral fractures (p=0.0049), and at 18 months for nonvertebral fractures (p=0.0036).
Persistence of antifracture effect
The incidence of clinical fractures was significantly lower in the zoledronic acid group than in the placebo group in each of the 3 years, although the treatment-by-year interaction suggested a potential interaction (p=0.097). The odds ratio (OR) for zoledronic acid compared with placebo was 0.74 in year 1 (95% CI, 0.60–0.91; p=0.0044), 0.53 in year 2 (95% CI, 0.42–0.66; p<0.0001), and 0.61 in year 3 (95% CI, 0.48–0.77; p<0.0001)[Figure 2]. The overall OR of any clinical fracture over 3 years for zoledronic acid compared with placebo was 0.62 (95% CI: 0.54–0.71; p<0.0001).
Figure 2.
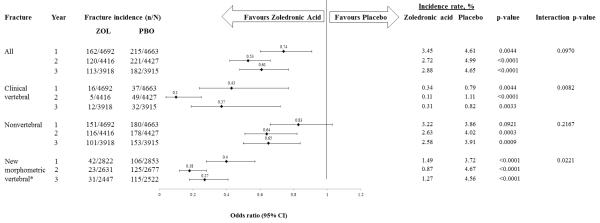
Incidence rates and odds ratio estimates of various types of clinical fractures in patients receiving zoledronic acid versus those receiving placebo in HORIZON-PFT and HORIZON-RFT female patients.
*Include women from the HORIZON-PFT only; new morphometric vertebral fracture data were not collected in the HORIZON-RFT.
The incidence of clinical vertebral fractures was also significantly lower in the zoledronic acid group than the placebo group in each of the 3 years (Figure 2). A slightly higher reduction in the incidence of clinical vertebral fracture with zoledronic acid was seen at year 2 compared with years 1 and 3, resulting in a significant between-year difference in treatment effect (p=0.0082). The overall risk of clinical vertebral fracture over 3 years was significantly lower in the zoledronic acid group than in the placebo group (OR, 0.25; 95% CI, 0.16–0.38; p<0.0001).
Zoledronic acid reduced the risk for nonvertebral fractures compared with placebo over 3 years (OR, 0.70; 95% CI, 0.61–0.81; p<0.0001). Year-by-year analysis showed that this nonvertebral fracture protective effect was significant in years 2 (p=0.0003) and 3 (p=0.0009) but not in year 1 (p=0.0921; Figure 2). There was no significant between-year difference in the effect of zoledronic acid on nonvertebral fractures (interaction p=0.2167).
For the additional analyses adjusted for age and number of infusions, zoledronic acid was associated with significantly lower risks for any clinical and clinical vertebral fractures at each of the 3 years (p<0.005 for each year for both fracture types), with ORs at year 2 smaller than those at year 1 or 3 (any clinical fracture, interaction p=0.0971; clinical vertebral fracture, interaction p=0.0082). Nonvertebral fracture incidences were also significantly lower in the zoledronic acid group than the placebo group in year 2 and 3 (p<0.001) and there was no significant between-year difference in the fracture protective effect of zoledronic acid over 3 years (interaction p=0.2162).
Among patients in the HORIZON-PFT and consistent with the published data, zoledronic acid significantly reduced the risk of new morphometric vertebral fracture compared with placebo. This reduction was significant at each of the 3 years according to the year-by-year analysis (p<0.001 for all). However, the OR of new morphometric vertebral fracture at year 2 and 3 were smaller than that at year 1 (0.18 and 0.27 vs. 0.40), which gave a significant between-year difference (interaction p=0.0221).
Discussion
This analysis of pooled data from two multinational, randomized, double-blind, placebo-controlled trials suggests that annual administration of zoledronic acid reduces the risk of all clinical fractures and of clinical vertebral fractures within the first year after administration, and the effect is persistent over at least 3 years. Year-by-year analysis also showed that zoledronic acid significantly reduced new morphometric vertebral fracture in each of the 3 years of the HORIZON-PFT. Once-yearly infusions of zoledronic acid reduce the risk for nonvertebral fracture within 18 months of treatment initiation, with the effect maintained at all subsequent time points. The difference between the onset of effect with zoledronic acid in clinical vertebral and nonvertebral fracture is consistent with that seen with other antiresorptive agents, such as alendronate.(5) A possible explanation is that the rapid reduction in bone resorption seen with potent antiresorptive agents(17) is sufficient to decrease risk of vertebral fracture whereas an increase in BMD, which requires more time after initial exposure to therapy, is required to decrease risk of nonvertebral fracture.
Clinical trials of skeletal antiresorptive agents typically evaluate antifracture efficacy by determining the cumulative fracture incidence or risk reduction from baseline to end of study. While this allows the assessment of overall efficacy over a treatment course, it does not allow identification of a difference in treatment efficacy between different treatment intervals (year 1 vs. year 2, etc.). Consequently, it is difficult to assess whether there is a differential effect of the therapy in the earlier and later years of the study. Persistence of antifracture effect has been investigated for raloxifene in an analysis that compared the treatment effects in study year 4 with cumulative results from years 1 to 3.(18) Although the study confirmed that the reductions in fracture continued for at least as long as 4 years, because cumulative results were used for the first 3 years, the year-on-year therapeutic effect during the initial course of treatment could not be determined. In the SOTI trial, strontium ranelate reduced vertebral fracture risk by 49% by the end of year 1, 41% by year 3 and 35% by year 4.(13) Whilst there was no direct year-by-year comparison, the numerical differences may suggest a potential waning of antifracture effect over time.
The current analysis, the first year-by-year analysis with an osteoporosis agent, has shown that zoledronic acid demonstrates consistently significant year-on-year risk reduction for any clinical fracture and clinical vertebral fracture. The year-by-year interaction p-value for any clinical fracture suggests a potential difference in zoledronic acid’s antifracture effect between years. However, the overlapping CIs of the year-by-year treatment effect and that the OR estimates were slightly lower in year 2 and 3 than in year 1, confirms that the antifracture effect of zoledronic acid does not decrease over time. For clinical vertebral fracture, a greater reduction in the incidence of clinical vertebral fracture with zoledronic acid was seen at year 2 compared with year 1 and 3. Similar results were seen with morphometric vertebral fractures among patients in the HORIZON-PFT. We cannot determine whether these larger reductions seen are clinically meaningful or a chance finding. Given that the differences are small and the year 3 findings were similar to year 1, it suggests that there is no waning of effect over time with zoledronic acid.
The persistence of zoledronic acid’s antifracture effect may be due to a number of factors. Zoledronic acid has a higher adsorption affinity constant for hydroxyapatite, which may contribute to a longer duration of effect and allow less frequent dosing than other clinically used bisphosphonates.(19) Treatment compliance probably plays a major role in the persistence of antifracture effect demonstrated for zoledronic acid in this study. As the dosing schedule of zoledronic acid is once-yearly, it is anticipated that the good compliance associated with zoledronic acid in clinical trials will translate into the ‘real-world’ setting. This contrasts with daily, weekly, or monthly oral bisphosphonate dosing regimens which are, on balance, much more difficult for patients to maintain.(7,11,12,20,21) A recent study in 22,363 new users of weekly or monthly bisphosphonates found 57% of subjects were noncompliant after 12 months.(11) Treatment non-compliance has been shown to be associated with reduced antifracture efficacy compared with full compliance.(10,12,20–24) For instance, in a study that included bisphosphonate-naïve patients who were prescribed with daily or weekly alendronate, it was found that each 1% decrease of the medication possession ratio (MPR) was associated with an 0.4% increase in risk of hip fracture at 12 months.(10) A separate study showed that for oral bisphosphonates with a daily or weekly dosing regimen, noncompliant use was associated with a 45% increased fracture risk compared with compliant use (defined as MPR ≥80%).(23) A recent review of the consequences of nonadherence to osteoporosis therapy also concluded that patients who were noncompliant with treatment have increased risk of fracture regardless of the efficacy of the treatment prescribed.(24) Furthermore, compliance with oral bisphosphonate therapy typically decreases with time after treatment initiation,(21) a factor that could lead to lack of persistence of antifracture effect.
This post-hoc analysis has limitations and the findings should be interpreted in the context of its design. The results for each year may not be directly comparable: the characteristics of patients at the start of years 2 and 3 differ from those at baseline and may no longer be comparable between randomized groups; and the patient numbers and populations at years 1, 2 and 3 differ due to the different lengths of follow-up of patients in the two studies. In addition, the wide confidence intervals (as seen in Figure 2) suggest that the analyses may not be optimally powered given that the original studies were designed to evaluate cumulative effects. Specifically, the lack of statistical significance for any clinical fracture and clinical vertebral fracture at 6 months is likely related to sample size and the limited number of fractures for these outcomes at this early time point. However, these limitations should not detract from the study’s main findings, which demonstrate the early onset and persistence of zoledronic acid’s antifracture effect. Future analyses that could add to our knowledge of the time-to-onset and duration of efficacy of this and other bisphosphonates include retrospective analyses involving larger groups of patients with the same condition or involving only male or mixed-sex populations, as well as a prospective trial specifically designed to investigate the year-on-year antifracture effects of bisphosphonates.
Conclusions
This analysis showed that in women with osteoporosis or a recent low-trauma hip fracture, zoledronic acid significantly reduced clinical fracture risk after one to two doses of therapy. With repeated dosing, zoledronic acid had a persistent year-by-year therapeutic effect for at least 3 years.
Acknowledgements
The analysis, the HORIZON-PFT(14) and the HORIZON-RFT (15) were sponsored by Novartis Pharma AG, Basel, Switzerland. The authors wish to thank the patients who took part in the studies and the investigators and staff at participating clinical centers.
The authors would like to acknowledge Magdalene Chu of BioScience Communications, London, for editorial assistance provided during the preparation of this manuscript with support from Novartis.
Footnotes
Authors’ roles Study design: SB, DB, PM. Study conduct: PM, DB. Data collection: GS, PM, DB. Data interpretation: SB, GS, PM, DB. Drafting manuscript: SB, GS, DB. Revising manuscript content: SB, RE, GS, PM, FC, JC, IR, KL, FC, DV, DB.
Disclosure This analysis was sponsored by Novartis Pharma AG.
Dr Boonen is senior clinical investigator of the Fund for Scientific Research, Flanders, Belgium (F.W.O.-Vlaanderen) and holder of the Leuven University Chair in Gerontology and Geriatrics. His institution, the University of Leuven, has received fees for Dr Boonen’s consultancy from Amgen, Novartis and Servier, and board memberships from Amgen, Novartis, Servier, and Warner Chilcott. These fundings were unrelated to the study discussed in this manuscript. The University has also received investigator fee for inclusion and follow up of study subjects in the trial discussed in the current manuscript. There was no compensation in relation to the current manuscript.
Dr Eastell has received grant and honoraria for speaking and consultancy from Novartis, Amgen, Sanofi-Aventis, Lilly, Organon, Pfizer, and Procter & Gamble Pharmaceuticals.
Dr Claessens states that he has no conflicts of interest to declare.
Dr Vanderschueren is a senior clinical investigator supported by the Clinical Research Fund of the University Hospitals Leuven, Belgium.
Dr Cosman has received honoraria for consulting, advising and/or speaking from Amgen, Eli Lilly, Merck and Novartis and grants from Eli Lilly and Novartis.
Dr Cauley has received consultancy fees and grants from Novartis and Merck. Her institution, the University of Pittsburgh, has received funds for conducting clinical studies.
Dr Su and Dr Mesenbrink are full-time Novartis employees and holds shares and stock options in Novartis.
Dr Lyles has received honoraria/royalties, grants and contracts, and fees for board membership, speaker bureaus and consultancy from Novartis. He is also the inventor for US patent application ‘Medication kits and formulations for preventing, treating or reducing secondary fractures after previous fracture’ (No. 12532285), coinventor for US patent application ‘Methods for preventing or reducing secondary fractures after hip fracture’ (No. 20050272707) and coinventor for US patent application ‘Bisphosphonate composition and methods for treating heart failure’.
Dr Black has received research grants from Merck, Novartis and Roche. He also has received consulting or advisory board fees from Eli Lilly, Amgen, Zosano, Radius and Nycomed.
References
- 1.Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 2.Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, Voqt T, Wallace R, Yates AJ, LaCroix AZ. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA. 1998;280:2077–2082. doi: 10.1001/jama.280.24.2077. [DOI] [PubMed] [Google Scholar]
- 3.Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH, III, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999;282:1344–1352. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 4.Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int. 2000;11:83–91. doi: 10.1007/s001980050010. [DOI] [PubMed] [Google Scholar]
- 5.Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR, Fracture Intervention Trial Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85:4118–4124. doi: 10.1210/jcem.85.11.6953. [DOI] [PubMed] [Google Scholar]
- 6.Harrington JT, Ste-Marie LG, Brandi ML, Civitelli R, Fardellone P, Grauer A, Barton I, Boonen S. Risedronate rapidly reduces the risk for nonvertebral fractures in women with postmenopausal osteoporosis. Calcif Tissue Int. 2004;74:129–135. doi: 10.1007/s00223-003-0042-4. [DOI] [PubMed] [Google Scholar]
- 7.Huas D, Debiais F, Blotman F, Cortet B, Mercier F, Rousseaux C, Berger V, Gaudin AF, Cotté FE. Compliance and treatment satisfaction of post menopausal women treated for osteoporosis. Compliance with osteoporosis treatment. BMC Womens Health. 2010;10:26. doi: 10.1186/1472-6874-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tosteson AN, Grove MR, Hammond CS, Moncur MM, Ray GT, Hebert GM, Pressman AR, Ettinger B. Early discontinuation of treatment for osteoporosis. Am J Med. 2003;115:209–216. doi: 10.1016/s0002-9343(03)00362-0. [DOI] [PubMed] [Google Scholar]
- 9.Roux C, Seeman R, Eastell R, Adachi J, Jackson RD, Felsenberg D, Songcharoen S, Rizzoli R, DiMunno O, Horlait S, Valent D, Watts NB. Efficacy of risedronate on clinical vertebral fractures within six months. Curr Med Res Opin. 2004;20:433–439. doi: 10.1185/030079903125003125. [DOI] [PubMed] [Google Scholar]
- 10.Rabenda V, Mertens R, Fabri V, Vanoverloop J, Sumkay F, Vannecke C, Deswaef A, Verpooten GA, Reginster JY. Adherence to bisphosphonates therapy and hip fracture risk in osteoporotic women. Osteoporos Int. 2008;19:811–818. doi: 10.1007/s00198-007-0506-x. [DOI] [PubMed] [Google Scholar]
- 11.Devine J, Trice S, Finney Z, Yarger S, Nwokeji E, Linton A, Davies W. A retrospective analysis of extended-interval dosing and the impact on bisphosphonate compliance in the US Military Health System. Osteoporos Int. 2011 doi: 10.1007/s00198-011-1729-4. DOI: 10.1007/s00198-011-1729-4. [DOI] [PubMed] [Google Scholar]
- 12.Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, Silverman S. Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc. 2006;81:1013–1022. doi: 10.4065/81.8.1013. [DOI] [PubMed] [Google Scholar]
- 13.Roux C, Fechtenbaum J, Kolta S, Isaia G, Andia JB, Devogelaer JP. Strontium ranelate reduces the risk of vertebral fracture in young postmenopausal women with severe osteoporosis. Ann Rheum Dis. 2008;67:1736–1738. doi: 10.1136/ard.2008.094516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR, HORIZON Pivotal Fracture Trial Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 15.Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S, HORIZON Recurrent Fracture Trial Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799–1809. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Medical Association [accessed 24 January 2012];Declaration of Helsinki: ethical principle for medical research involving human subjects. 41th WMA General Assembly, Hong Kong. 1989 http://www.wma.net/en/30publications/10policies/b3/index.html.
- 17.Saag K, Lindsay R, Kriegman A, Beamer E, Zhou W. A single zoledronic acid infusion reduces bone resorption markers more rapidly than weekly oral alendronate in postmenopausal women with low bone mineral density. Bone. 2007;40:1238–1243. doi: 10.1016/j.bone.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 18.Delmas PD, Ensrud KE, Adachi JD, Harper KD, Sarkar S, Gennari C, Reginster JY, Pols HA, Recker RR, Harris ST, Wu W, Genant HK, Black DM, Eastell R, Multiple Outcomes of Raloxifene Evaluation Investigators Efficacy of raloxifene on vertebral fracture risk reduction in postmenopausal women with osteoporosis: four-year results from a randomized clinical trial. J Clin Endocrinol Metab. 2002;87:3609–3617. doi: 10.1210/jcem.87.8.8750. [DOI] [PubMed] [Google Scholar]
- 19.Nancollas GH, Tang R, Phipps RJ, Henneman Z, Gulde S, Wu W, Mangood A, Russell RG, Ebetino FH. Novel insights into actions of bisphosphonates on bone: differences in interactions with hydroxyapatite. Bone. 2006;38:617–627. doi: 10.1016/j.bone.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Gallagher AM, Rietbrock S, Olson M, van Staa TP. Fracture outcomes related to persistence and compliance with oral bisphosphonates. J Bone Miner Res. 2008;23:1569–1575. doi: 10.1359/jbmr.080510. [DOI] [PubMed] [Google Scholar]
- 21.Hadji P, Claus V, Ziller V, Intorcia M, Kostev K, Steinle T. GRAND: the German retrospective cohort analysis on compliance and persistence and the associated risk of fractures in osteoporotic women treated with oral bisphosphonates. Osteoporos Int. 2011 doi: 10.1007/s00198-011-1535-z. DOI 10.1007/s00198-011-1535-z. [DOI] [PubMed] [Google Scholar]
- 22.Hoer A, Seidlitz C, Gothe H, Schiffhorst G, Olson M, Hadji P, Häussler B. Influence on persistence and adherence with oral bisphosphonates on fracture rates in osteoporosis. Patient Prefer Adherence. 2009;3:25–30. [PMC free article] [PubMed] [Google Scholar]
- 23.Penning-van Beest FJA, Erkens JA, Olson M, Herings RMC. Loss of treatment benefit due to low compliance with bisphosphonate therapy. Osteoporos Int. 2008;19:511–517. doi: 10.1007/s00198-007-0466-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adachi JD, Josse RG, Russell RG. If you don’t take it - it can’t work: the consequences of not being treated or nonadherence to osteoporosis therapy. Ther Clin Risk Manag. 2011;7:181–198. doi: 10.2147/TCRM.S17513. [DOI] [PMC free article] [PubMed] [Google Scholar]