Abstract
Rickettsia typhi and R. felis are the etiological agents of murine typhus and flea-borne spotted fever, respectively. Both are emerging acute febrile zoonotic diseases for which fleas are vectors; they also have similar clinical characteristics and global distribution. In 2005, we identified the circulation of murine typhus in 6 towns within the mountainous coffee-growing area north of Caldas, Colombia. We now report the specific seroprevalence against R. typhi and R. felis, and associated risk factors in 7 towns of this province. The combined seroprevalence against the 2 flea-borne rickettsioses is the highest yet reported in the literature: 71.7% (17.8% for R. felis, 25.2% for R. typhi, and 28.7% for both). We also report a prospective analysis of 26 patients with a febrile illness compatible with rickettsioses, including murine typhus; 9 of these patients had a rickettsiosis. This supports our sero-epidemiological results and highlights the diagnostic complexity of febrile syndromes in this region.
Key Words: Colombia, Rickettsia, Rickettsia felis, Fleas, Zoonotic diseases
Introduction
Rickettsioses are vector-borne zoonotic infections caused by obligate intracellular bacteria of the genus Rickettsia. They are divided in 4 groups based on their genotypic characteristics: Spotted fever group (R. rickettsii, R. conorii, R. parkeri, and several others), typhus group (R. prowazekii and R. typhi), transitional group (R. felis, R. akari, and R. australis), and the nonpathogenic ancestral group (R. bellii and R. canadensis) (Mansueto et al. 2012). R. typhi (known in the old literature as R. mooseri) and R. felis are the etiological agents of murine typhus and flea-borne spotted fever, respectively. Both bacteria produce a flu-like febrile syndrome, frequently accompanied by rash. For R. typhi, fatality is generally less than 1–2%, with a global distribution with its main vector, the flea Xenopsylla cheopis. R. felis, also globally distributed, is primarily associated with Ctenocephalides fleas (Civen and Ngo 2008, Reif and Macaluso 2009, Eisen and Gage 2012).
Murine typhus, also known as endemic typhus or flea-borne typhus, has been known since the early 20th century and is described as an illness of ports and urban areas where synanthropic rodents, particularly Rattus rattus and R. norvegicus, are classically involved as primary reservoirs and amplifying hosts of both Rickettsia and the flea vector X. cheopis. However, wild and domestic animals and their respective ectoparasites have also been implicated in the disease cycle (Raoult and Parola 2009). The disease is prevalent in many areas of the world, including southeast Asia, southern Europe, the Mediterranean, northern Africa, South America, and the United States (Labruna 2009, Renvoisé and Raoult 2009). In Colombia, it has only been documented in the region of the present study. Reports to the Colombian National Institute of Health show that murine typhus has been recognized since the 1990s and confirmed with the Weil–Felix reaction (an insensitive and nonspecific test); the incidence of the disease between 1992 and 1997 was 1.13/100.000 cases (www.doctorlaverde.com/epidemiologia/Documentos%20compartidos/TIFUS.pdf/). Years later, between May and October, 2005, we reported the first epidemiological study of murine typhus in the North of Caldas using the specific indirect immunofluorescence assay (IFA) (Hidalgo et al. 2008). More recent surveillance data show that murine typhus is still a prevalent disease (www.ins.gov.co/?idcategoria=85465#/, www.ins.gov.co/?idcategoria=5971#/, www.ins.gov.co/?idcategoria=5988#/; Ramirez et al. 2007).
Murine typhus presents after an incubation period of approximately 7–14 days with acute fever, severe headache, myalgia, arthralgia, and macular or maculopapular rash that affects the trunk and distributes in a centrifugal fashion (present in approximately 50% of cases) (Civen and Ngo 2008).
Flea-borne spotted fever (also known as cat flea typhus) was described recently as a human infection. The clinical characteristics are very similar to murine typhus, except that an inoculation eschar is occasionally found; no fatalities have been reported (Raoult and Parola 2009, Reif and Macaluso 2009). The cat flea (Ctenocephalides felis) appears to be the main vector and reservoir of R. felis with a prevalence of infection of 4–90%. The cosmopolitan condition of C. felis and its mammalian hosts (cats and dogs) probably explains the multiple reports arising from many countries: Egypt, France, Germany, South Korea, Spain, Taiwan, Thailand, United States, Mexico, and Brazil; this is clearly an emerging rickettsioses of medical importance (Perez-Osorio et al. 2008, Reif and Macaluso 2009). It is, however, likely to be underdiagnosed and underreported (just like murine typhus and other rickettsioses) because of the absence of commercially available diagnostic methods that can be applied during the acute stage. Furthermore, serological diagnosis is complicated by cross-reactivity of the human humoral immune response against different rickettsiae (Raoult and Parola 2009, Lim et al. 2012).
The aims of our study were to: (1) Evaluate whether R. felis is also part of the diagnostic spectrum in the same region where we previously confirmed the circulation of murine typhus; and (2) determine the probable etiology of febrile cases compatible with rickettsioses, including murine typhus.
Materials and Methods
Geographical area
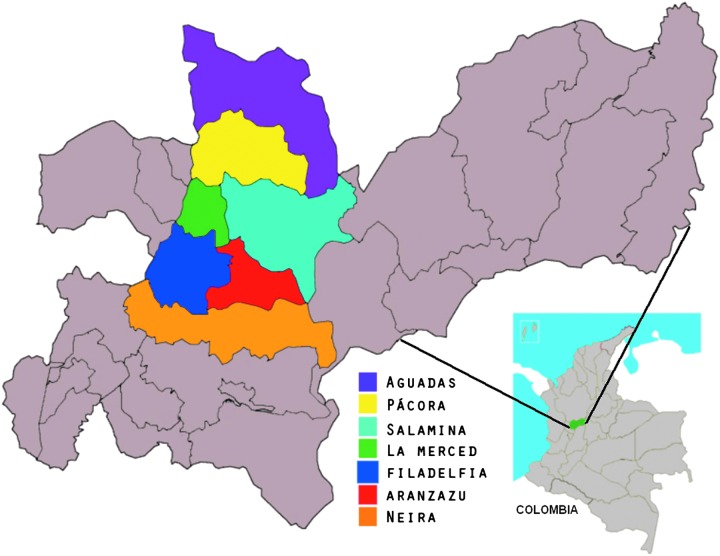
The study was carried out in the northern region of the Province of Caldas (midwestern area of Colombia, central branch of the Andes). This province has 27 subregions with a large town in each one of them. The main economic activity is agriculture. For our study, a total of 7 towns were included (Aguadas, Aranzazu, Filadelfia, La Merced, Neira, Pacora, and Salamina) because of their status as a disease endemic area from previous studies (Fig. 1).
FIG. 1.
Map of Caldas province and towns (in colors) included in the study. (Color image is available at www.liebertpub.com/vbz).
Samples
The study was approved by the Ethics Committee of Pontificia Universidad Javeriana, Bogota, Colombia. Participation in the study was voluntary, and subjects were included after informed consent. According to population census, the total number of inhabitants in the 7 towns was 96,183. With an allowable error of 10% and 95% confidence, we estimated a sample size of 682 people (taking into account a general seroprevalence of 19%) in urban and rural areas of the region. Blood samples were obtained by health staff of the Health Directorate of Caldas between July, 2010, and July, 2011. For each volunteer, we collected the following data: Age, gender, location of residence (urban or rural), housing type according to construction material, history of flea bite, recognized presence of rodents at home, presence of pets and opossums, contact with other animals, and tick bites. Serum was separated and sent under refrigeration to the Special Bacteriology laboratory at Pontificia Universidad Javeriana (Bogotá) where the sera were stored at −20°C for later analysis by IFA (immunoglobulin G [IgG] antibodies against R. typhi and R. felis).
The 682 volunteer subjects were distributed by subregion as follows: 68 in Aguadas, 198 in Aranzazu, 46 in Filadelfia, 8 in La Merced, 203 in Neira, 45 in Pacora, and 114 in Salamina. The sociodemographic characteristics of the sampled population are shown in Table 1.
Table 1.
Distribution of Sociodemographic Characteristics of the 7 Towns Studied
| |
Total |
R. felis only IgG ≥1:64 |
R. typhi only IgG ≥1:64 |
Cross-reactivea |
||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| All | 682 | 100 | 122 | 17.8 | 172 | 25.2 | 196 | 28.7 |
| Gender | ||||||||
| Women | 492 | 72.1 | 91 | 18.4 | 122 | 24.8 | 137 | 27.8 |
| Men | 190 | 27.9 | 31 | 16.3 | 50 | 26.3 | 59 | 31.1 |
| Age (years) | ||||||||
| <16 | 25 | 3.7 | 3 | 12 | 2 | 8 | 5 | 20 |
| 16–30 | 165 | 24.2 | 36 | 21.8 | 32 | 19.4 | 45 | 27.3 |
| 31–45 | 190 | 27.9 | 38 | 19.4 | 51 | 17.6 | 44 | 15.2 |
| 46–65 | 224 | 32.8 | 34 | 15.1 | 63 | 28.2 | 79 | 35.3 |
| >65 | 78 | 11.4 | 11 | 14.1 | 24 | 30.8 | 23 | 29.5 |
| Residence area | ||||||||
| Urban | 337 | 49.4 | 68 | 20.1 | 78 | 23.1 | 90 | 26.7 |
| Rural | 344 | 50.4 | 54 | 15.6 | 94 | 27.3 | 105 | 30.5 |
| No data | 1 | 0.1 | 0 | 0 | 0 | 0 | 1 | 100 |
Immunoglobulin G antibodies present at a titer of at least 1:64 against both species of flea-borne Rickettsia (R. felis and R. typhi).
We also performed a small prospective study simultaneously with sampling for the seroprevalence study. This portion of the study was also approved by the same Ethics Committee and was administered with informed consent. We evaluated patients with febrile illness compatible with a case definition for rickettsioses, including murine typhus described in the “typhus vigilance protocol” produced by the Transmissible Diseases Group (zoonoses functional team) of the National Institute of Health of Colombia (www.vigepi.com.co/sivigila/pdf/protocolos/780p%20tif.pdf/) and in consensus with the medical and health professionals of these towns. We obtained acute serum samples at the time of consultation with fever, and a second sample 2–3 weeks later (convalescent samples). We tested all patients for respiratory virus infection (identification and screening kit by IFA for adenovirus, A and B influenza virus, 1, 2, and 3 parainfluenza virus, and respiratory syncytial virus), dengue (E-DEN01M, Dengue IgM Capture ELISA Panbio), Leptospira (E-LEP01M, Leptospira IgM ELISA Panbio diagnostic), R typhi (IgG antibodies against R. typhi antigen, Wilmington strain), R. felis (IgG antibodies against R. felis antigen, Pedreira strain), and rickettsiae of the spotted fever group (IgG antibodies against R. rickettsii, Taiaçu strain). For the serological diagnostic confirmation of a rickettsiosis, we used a minimum of a four-fold increase in anti-Rickettsia IgG titers between the acute and convalescent serum samples as recommended by Centers for Disease Control and Prevention (CDC) (Chapman et al. 2006).
Serological technique
Human serum samples were screened at a diagnostic dilution of 1:64 by indirect IFA for the presence of IgG-specific antibodies using antigen slides containing the appropriate antigen. After incubation of the serum dilutions for 30 min at 37°C in a moist chamber, the slides were washed with phosphate-buffered saline (PBS). The human antibodies were detected with fluorescein isothiocyanate (FITC)-conjugated, affinity-purified, goat anti-human IgG, Fc-gamma fragment–specific (Jackson ImmunoResearch Laboratories, West Grove, PA) at a 1:400 dilution (as determined by checkerboard titration). The slides were incubated with the conjugate antibody at 37°C for 30 min in a moist chamber and washed again with PBS. Evans Blue (Sigma Chemical Company, St. Louis, MO) was added as a counterstain. Coverslips were mounted in glycerol–PBS (9:1) buffer (pH 9.0), and slides were examined using a wide-field fluorescence microscope with appropriate filters to detect the emission of fluorescein. Positive and negative control sera were obtained from Focus Technologies (IF0112 and IF0115, respectively; Cypress, CA). Intense green fluorescence of small bacilli (the rickettsiae) within the cells at 1:64 dilution was considered to be a positive reaction. In negative reactions, the cells were tinted red and did not display any fluorescence. Results were confirmed by 2 independent observers. Furthermore, positive serum samples for flea-borne rickettsiae were screened with R. rickettsii slides. Cross-reaction was only observed in 15.8% of positive samples for R. felis (23/145); cross-reaction was not found in R. typhi samples.
Statistical analysis
The software application SPSS 18 Inc. was used. The chi-squared test was performed to establish associations between sociodemographic variables and expositional risk factors with seropositivity; a p value<0.05 was considered significant. To evaluate the possible association between house type and seropositivity for R. typhi and/or R. felis, odds ratios (OR) and confidence intervals (CI) of 95% were determined.
Results
Among 682 sampled volunteers, 122 (17.8%) had IgG antibodies that reacted exclusively against R. felis at a titer of 1:64 or greater and 172 (25.2%) had IgG antibodies that reacted exclusively against R. typhi antigen at the diagnostic titer of 1:64 or more. A third subgroup of volunteers, 196 (28.7%), had cross-reactive IgG antibodies against both R. felis and R. typhi.
The seroprevalence for R. felis was higher in women, in the age range of 16–30 years, and in the urban area; for R. typhi, the seroprevalence was higher in men, in the age group over 65 years old, and in the rural area. On the other hand, the seroprevalence in the samples with cross-reactivity was higher in men in the age range of 46–65 years old and in the rural area (Table 1). The towns with the highest seroprevalence were Pacora, Salamina, and Neira (33.3% for R. felis, 37.7% for R. typhi, and 33% for both, respectively) (Table 2).
Table 2.
Seroprevalence against Rickettsia felis, Rickettsia typhi, or Both Species According to Location
| |
R. felis only |
R. typhi only |
Cross-reactivea |
|---|---|---|---|
| Town | n (%) | n (%) | n (%) |
| Neira (n=203) | 41 (20.1) | 44 (21.7) | 67 (33) |
| Aranzazu (n=198) | 26 (13.1) | 53 (26.8) | 62 (31.3) |
| Salamina (n=114) | 15 (13.1) | 43 (37.7) | 25 (21.9) |
| Aguadas (n=68) | 13 (19.1) | 12 (17.6) | 17(25) |
| Filadelfia (n=46) | 12 (26) | 11 (23.9) | 13 (28.3) |
| Pacora (n=45) | 15 (33.3) | 6 (13.3) | 11 (24.4) |
| La Merced (n=8) | 0 (0) | 3 (37.5) | 1 (12.5) |
| Total (n=682) | 122 (17.8) | 172 (25.2) | 196 (28.7) |
Immunoglobulin G antibodies present at a titer of 1:64 against both species of flea-borne Rickettsia (R. felis and R.typhi).
We did not identify associations with housing type (bahareque with wood floor, bahareque with cement floor, bahareque with dirt floor, concrete with cement floor, concrete with wood floor, wattle housing, basement housing) or exposure risk factors (flea or tick bite antecedent, presence of rodents at home, presence of pets at home, presence of opossums in peridomestic area, and contact with other animals). Bahareque is a structural material consisting of bamboo canes or any other type of cane tied together and glued with mud.
We also studied paired sera (acute and convalescent) from 26 patients with a febrile illness compatible with rickettsioses, including murine typhus (acute fever with intense headache, chills, prostration, and generalized pain with or without maculopapular rash). The results are summarized in Table 3. Two of these patients had a diagnosis of murine typhus based on at least a 4-fold increase in anti-R. typhi IgG antibodies between the acute and convalescent sera without reactivity against other rickettsiae. One patient had flea-borne spotted fever as determined by a 4-fold increase in anti-R. felis IgG titers between the acute and convalescent sera without cross-reactivity against other rickettsiae. One patient had diagnostic titers of a flea-borne rickettsioses, but it was not possible to discern the etiology because the difference in the convalescent sero-reactivity was of only 1 titer between R. typhi and R. felis (although it was higher for the later). Interestingly, 5 other patients had a tick-borne spotted fever based on the serological response against R. rickettsii antigen and the absence of IgG against flea-borne rickettsiae; however, it is not possible to establish the exact etiology because different tick-borne spotted fevers produce highly cross-reactive antibody responses. Two of the patients without a rickettsiosis were positive for anti-Leptospira IgM and 1 for anti-dengue IgM. None of the patients were positive for respiratory viruses.
Table 3.
Positive Results of Diagnostic Tests Performed on 26 Paired Serum Samples from Patients with a Febrile Syndrome Compatible with Rickettsioses, Including Murine Typhus
| |
|
IFA R. typhi* |
IFA R. felisa |
IFA R. rickettsiia |
Leptospira |
Virus dengue |
|||
|---|---|---|---|---|---|---|---|---|---|
| Gender | Precedence | Acute- phase titer | Convalescent-phase titer | Acute- phase titer | Convalescent-phase titer | Acute-phase titer | Convalescent-phase titer | IgM | IgM |
| Female | Filadelfia | <1:64 | 1:1024 | 1:64 | 1:64 | <1:64 | <1:64 | Negative | Negative |
| Female | Salamina | 1:256 | 1:2048 | <1:64 | <1:64 | <1:64 | <1:64 | Positive | Negative |
| Female | Aguadas | <1:64 | <1:64 | 1:256 | 1:1024 | 1:64 | 1:64 | Negative | Negative |
| Male | Salamina | 1:64 | 1:256 | 1:128 | 1:512 | <1:64 | 1:64 | Negative | Negative |
| Male | Aguadas | <1:64 | <1:64 | <1:64 | 1:64 | 1:64 | 1:256 | Negative | Positive |
| Male | Aguadas | <1:64 | <1:64 | <1:64 | <1:64 | 1:64 | 1:256 | Negative | Negative |
| Male | Salamina | <1:64 | <1:64 | <1:64 | <1:64 | 1:64 | 1:256 | Negative | Negative |
| Male | Salamina | <1:64 | <1:64 | <1:64 | <1:64 | 1:256 | 1:1024 | Negative | Negative |
| Female | Salamina | <1:64 | <1:64 | <1:64 | <1:64 | 1:64 | 1:256 | Negative | Negative |
| Male | Salamina | <1:64 | <1:64 | <1:64 | 1:64 | <1:64 | <1:64 | Positive | Negative |
| Female | Salamina | <1:64 | <1:64 | <1:64 | <1:64 | <1:64 | <1:64 | Positive | Negative |
| Male | Salamina | <1:64 | <1:64 | <1:64 | <1:64 | 1:64 | 1:64 | Negative | Positive |
Note that a difference of two titers between the acute and convalescent samples is equivalent to a 4-fold increase (two 2-fold dilutions) and is considered diagnostic.
Discussion
Murine typhus and flea-borne spotted fever cause febrile diseases throughout the world. However, seroprevalence studies addressing these 2 entities in humans are very uncommon, particularly in the Americas. Herein, we present serological evidence of the co-circulation of the 2 known flea-borne rickettsiae, R. felis and R. typhi, and tick-borne spotted fever rickettsiae north of Caldas, Colombia, a region that we had previously shown to be endemic for murine typhus (Hidalgo et al. 2008).
The seroprevalence against flea-borne rickettsioses in the 7 towns investigated was the highest yet reported in the literature; 71.7% was distributed as follows—17.8% for R. felis, 25.2% for R. typhi, and 28.7% for both. Other reports in the literature showed seroprevalence values as low as 2% for R. typhi in northern Greece (Alexiou et al. 2002) or 1.1% for R. typhi in Minas Gerais, Brazil (Gonçalves et al. 2005). On the other hand, higher seroprevalence values have been reported from other countries. A seroprevalence of 10.3% for the typhus group was reported from the Peruvian Amazon Basin (Forshey et al. 2010). A study in Spain showed a seroprevalence against R. typhi and R. felis of 3.8–18% and 3.2–6.5%, respectively (Bernabeu-Wittel et al. 2006, Nogueras et al. 2006, Bolaños-Rivero et al. 2011). The only other report with higher seroprevalence for one of the pathogens reported here is one from northeast Bosnia-Herzegovina for R. typhi (37.7%) (Punda-Polic et al. 1995).
Given the fact that we identified many individuals with exclusive reactivity against either R. felis or R. typhi, but not both, we suspect that those with diagnostic titers for both rickettsiae were infected by both rickettsial species in the past. Of course, broad cross-reactivity of the humoral immune response in some individuals is an alternative explanation, and the circulation of tick-borne spotted fever rickettsiae could certainly be a contributing factor (Raoult and Parola 2009).
Our findings by age, gender, and home location (rural vs. urban) are comparable to those from Canary Islands and the south of Spain (Bernabeu-Wittel et al. 2006, Bolaños-Rivero et al. 2011), where age older than 45 years old is a factor associated with R. typhi seropositivity and age around 30 years old is associated with positive titers against R. felis. It is also worth highlighting the trend for higher rates of seropositivity against R. typhi in men and in the rural areas (Lledó et al. 2001, Nogueras et al. 2006, Bolaños-Rivero et al. 2011). The potential association with place of residence merits further investigation because it could be explained by the role of other host animals such as opossums, cats, and dogs (Hii et al. 2011) or the activity of other flea species different from X. cheopis (Eisen and Gage 2012). Such extension of the range of possible infection sources could explain the changing behavior of flea-borne rickettsioses from urban disease to a suburban or even rural infection (Civen and Ngo 2008).
The high frequency of confirmed rickettsioses (9 cases: 4 caused by flea-borne rickettsiae and 5 caused by tick-borne spotted fever group rickettsiae) among the 26 patients with a febrile syndrome compatible with rickettsioses partially mirrors our seroprevalence findings, although the frequency is lower than in the sampled population. Because the reagents, microscope, and raters used for both studies were the same, we believe that the differences in the seroprevalence of the prospective and retrospective studies are due to chance. Interestingly, in addition to flea-borne rickettsioses, we identified patients with other rickettsial spotted fevers, likely tick-borne. Those cases were probably not caused by Rickettsia rickettsii because the cases were not severe, so the positive antibodies against R. rickettsii antigen are possibly due to the well-known cross-reactivity within the spotted fever group. We should also mention that antibodies against R. typhi are highly cross-reactive with R. prowazekii, the agent of epidemic typhus; however, we do not believe that this disease is present in this region because the infections have not been severe and because the vector, the human body louse, was not identified.
Similar to other reports (Blacksell et al. 2007, Parker et al. 2007), we found evidence of possible coinfection with R. typhi and Leptospira in 1 patient diagnosed with murine typhus. This is probably explained by the role of synanthropic rodents in the ecology and transmission of both diseases. In future studies, we will explore this possibility together with in-depth analyses of vectors and their associated pathogens.
In conclusion, despite having made a convenience sampling, our study shows an important approximation to the high seroprevalence of flea-borne rickettsial diseases in the north of Caldas, Colombia. Furthermore, the prospective component of our study highlights the diagnostic complexity of flu-like syndromes in areas like that described here where zoonoses and vector-borne diseases (i.e., rickettsioses, leptospirosis, dengue, and other infections not tested here) are the rule rather than the exception (Blacksell et al. 2007, Parker et al. 2007, Suarez et al. 2008, Villar et al. 2010). Many of these diseases, particularly rickettsioses, do not have commercially available diagnostic tests that can be used during the acute stage of the disease. There is a critical need to address the public health of these populations because some of these diseases, including rickettsioses and leptospirosis, are treatable with antibiotics. Thus, significant morbidity and mortality could be reduced at the same time that the economic impact of lost work is minimized.
Acknowledgments
This research was supported by grant 003532 from Pontificia Universidad Javeriana to M. Hidalgo. The authors thank Andrea Rodríguez López for a preliminary review of the English. The authors thank Becton, Dickinson and Company for the donation of material for sampling.
Author Disclosure Statement
The authors declare that no conflicts of interest exist.
References
- Alexiou S. Manika K. Arvanitiduo M. Antoniadis A. Prevalence of Rickettsia conorii and Rickettsia typhi infections in population of Northern Greece. Am J Trop Med Hyg. 2002;66:76–79. doi: 10.4269/ajtmh.2002.66.76. [DOI] [PubMed] [Google Scholar]
- Bernabeu-Wittel M. del Toro M. Noguera M. Muniain M, et al. Seroepidemiological study of Rickettsia felis, Rickettsia typhi, and Rickettsia conorii infection among the population of souther Spain. Eur J Clin Microbiol Infect Dis. 2006;25:375–381. doi: 10.1007/s10096-006-0147-6. [DOI] [PubMed] [Google Scholar]
- Blacksell S. Sharma N. Phumratanaprapin W. Jenjaroen K, et al. Serological and blood culture investigations of Nepalese fever patients. Trans R Soc Trop Med Hyg. 2007;101:686–690. doi: 10.1016/j.trstmh.2007.02.015. [DOI] [PubMed] [Google Scholar]
- Bolaños-Rivero M. Santana-Rodríguez E. Angel-Moreno A. Hernández-Cabrera M, et al. Seroprevalence of Rickettsia typhi and Rickettsia conorii infections in the Canary Islands (Spain) Int J Infect Dis. 2011;15:481–485. doi: 10.1016/j.ijid.2011.03.019. [DOI] [PubMed] [Google Scholar]
- Chapman AS. Bakken JS. Folk SM. Paddock CD, et al. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever, ehrlichioses, and anaplasmosis—United States: A practical guide for physicians and other health-care and public health professionals. MMWR Recomm Rep. 2006;55:1–27. [PubMed] [Google Scholar]
- Civen R. Ngo V. Murine typhus: An unrecognized suburban vectorborne disease. Clin Infect Dis. 2008;46:913–918. doi: 10.1086/527443. [DOI] [PubMed] [Google Scholar]
- Eisen R. Gage K. Transmission of flea-borne zoonotic agents. Annu Rev Entomol. 2012;57:61–82. doi: 10.1146/annurev-ento-120710-100717. [DOI] [PubMed] [Google Scholar]
- Forshey B. Stewart A. Morrison A. Gálvez H, et al. Epidemiology of spotted fever group and typhus group rickettsial infection in the Amazon Basin of Peru. Am J Trop Med Hyg. 2010;82:683–690. doi: 10.4269/ajtmh.2010.09-0355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonçalves P. Brigatte M. Greco D. Antibodies to Rickettsia rickettsii, Rickettsia typhi, Coxiella burnetii, Bartonella henselae, Bartonella quintana, and Ehrlichia chaffeensis among healthy population in Minas Gerais, Brazil. Mem Inst Oswaldo Cruz. 2005;100:853–859. doi: 10.1590/s0074-02762005000800006. [DOI] [PubMed] [Google Scholar]
- Hidalgo M. Salguero E. De la Ossa A. Sánchez R, et al. Short report: Murine typhus in Caldas, Colombia. Am J Trop Med Hyg. 2008;78:321–322. [PubMed] [Google Scholar]
- Hii SF. Kopp SR. Abdad MY. Thompson MF, et al. Molecular evidence supports the role of dogs as potential reservoirs for Rickettsia felis. Vector Borne Zoonotic Dis. 2011;11:1007–1012. doi: 10.1089/vbz.2010.0270. [DOI] [PubMed] [Google Scholar]
- Labruna M. Ecology of Rickettsia in South America. Ann NY Acad Sci. 2009;166:156–166. doi: 10.1111/j.1749-6632.2009.04516.x. [DOI] [PubMed] [Google Scholar]
- Lim M. Brady H. Hambling T. Sexton K, et al. Rickettsia felis infections, New Zealand. Emerg Infect Dis. 2012;18:167–169. doi: 10.3201/eid1801.110996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lledó M. Gegúndez J. Beltrán M. Prevalence of antibodies to Rickettsia typhi in an area of the center of Spain. Eur J Epidemiol. 2001;17:927–928. doi: 10.1023/a:1016248630809. [DOI] [PubMed] [Google Scholar]
- Mansueto P. Vitale G. Cascio A. Seidita A, et al. New Insight into Immunity and Immunopathology of Rickettsial Diseases. Clin Dev Immunol. 2012:2–26. doi: 10.1155/2012/967852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nogueras M. Cardeñosa N. Sanfeliu I. Muñoz T, et al. Short report: Serological evidence of infection with Rickettsia typhi and Rickettsia felis among human population of Catalonia, in the northeast of Spain. Am J Trop Med Hyg. 2006;74:123–126. [PubMed] [Google Scholar]
- Parker T. Murray C. Richards A. Samir A, et al. Concurrent infections in acute febrile illness patients in Egypt. Am J Trop Med Hyg. 2007;77:390–392. [PubMed] [Google Scholar]
- Perez-Osorio C. Zavala-Velazquez J. Arias J. Zavala-Castro J. Rickettsia felis as emergent global threat for humans. Emerg Infect Dis. 2008;14:1019–1023. doi: 10.3201/eid1407.071656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punda-Polic V. Leko-Grbic J. Radulovic S. Prevalence of antibodies to rickettsiae in the north-western part of Bosnia and Herzegovina. Eur J Epidemiol. 1995;11:697–699. doi: 10.1007/BF01720305. [DOI] [PubMed] [Google Scholar]
- Ramírez, N, Galvis, O, Agudelo, A, Velásquez, R, et al. Tifus murino en el Cairo-Valle ¿Brote o condición endémica emergente? Investigaciones andina. 2007;9:5–13. [Google Scholar]
- Raoult D. Parola P. New York: Informa Healthcare; 2009. Rickettsial Diseases; pp. 37–46. 87–96. [Google Scholar]
- Reif K. Macaluso K. Ecology of Rickettsia felis: A Review. J Med Entomol. 2009;46:723–736. doi: 10.1603/033.046.0402. [DOI] [PubMed] [Google Scholar]
- Renvoisé A. Raoult D. An update on Rickettsiosis. Med Mal Infect. 2009;39:71–81. doi: 10.1016/j.medmal.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Suarez R. Hidalgo M. Niño N. González M, et al. Primera edición. Bogotá D.C.: Colombia: Ediciones Uniandes; 2008. Las Rickettsias como agentes etiológicos de entidades febriles no diagnosticadas en Colombia; pp. 23–42. [Google Scholar]
- Villar L. Valbuena G. Hidalgo M. González M, et al. Etiología del síndrome febril agudo inespecífico en un área urbana colombiana endémica para dengue. Infectio. 2010;14:22–23. [Google Scholar]