Abstract
While much is known about the prevalence of influenza viruses in North America and Eurasia, their prevalence in birds and mammals in South America is largely unknown. To fill this knowledge gap and provide a baseline for future ecology and epidemiology studies, we conducted 2 years of influenza surveillance in the eastern plains (Los Llanos) region of Colombia. Real-time reverse transcriptase polymerase chain reaction (RT-PCR) identified influenza viruses in wild birds, domestic poultry, swine and horses. Prevalence ranged from 2.6% to 13.4% across species. Swine showed the highest prevalence and were infected primarily with 2009 pandemic H1N1 (pH1N1) viruses genetically related to those in humans. In addition, we isolated H5N2 viruses from two resident species of whistling ducks (genus Dendrocygna) that differed completely from previous South American isolates, instead genetically resembling North American wild bird viruses. Both strains caused low pathogenicity in chickens and mammals. The prevalence and subtype diversity of influenza viruses isolated from diverse species within a small area of Colombia highlights the need for enhanced surveillance throughout South America, including monitoring of the potential transmissibility of low-pathogenic H5N2 viruses from wild birds to domestic poultry and the emergence of reassortant viruses in domestic swine.
Keywords: Colombia, H1N1, H5N2, influenza, pandemic, risk assessment, reassortment, surveillance
Introduction
Outbreaks of influenza A viruses cause morbidity and mortality in mammals and birds worldwide. Although it remains difficult to prevent or even predict new influenza outbreaks, surveillance in animals and birds can facilitate early recognition of new threats.1 Given the number of unique viruses emerging from animals and birds, surveillance efforts should include a diverse range of wild and domestic animals.2
While there are extensive influenza surveillance efforts in many parts of the world, the prevalence and diversity of influenza viruses in South America remains largely unknown, especially in Colombia,2 the second most biologically diverse country and home to approximately 10% of the world's species.3,4 Colombia's biodiversity reflects its varied ecosystems, including tropical rainforests, coastal cloud forests and open savannas. Colombia also has diverse avifauna, including more than 1800 resident species; further, its location on three major migratory routes makes it a stop-over site for approximately 180 migratory bird species.5,6 Colombian wetlands provide habitat for at least 98.3% of the migratory waterfowl and 57% of the resident waterfowl in the country.7 Additionally, Colombia has active swine and poultry industries that include domestic husbandry and live animal markets, providing the optimal setting for mixing of wild birds and domestic animals.
With the exception of a report of avian H9N2 influenza infection in asymptomatic broiler flocks in Tolima in the mid-2000s,8 there have been no studies of the prevalence of influenza viruses in domestic animals or wild birds in Colombia. We therefore undertook a 2-year surveillance study in the Llanos region of Colombia, a neotropical savanna in the Orinoco river basin. This savanna is considered one of the world's richest tropical grasslands; it has numerous ecosystems that provide habitat to a large number of resident and migratory birds and diverse agricultural species.9 The prevalence of influenza viruses in diverse species within a small area of Colombia highlights the need for enhanced surveillance throughout South America, including monitoring of the potential transmission of low-pathogenic H5N2 viruses from wild birds to domestic poultry.
Materials and methods
Surveillance sites and sample collection
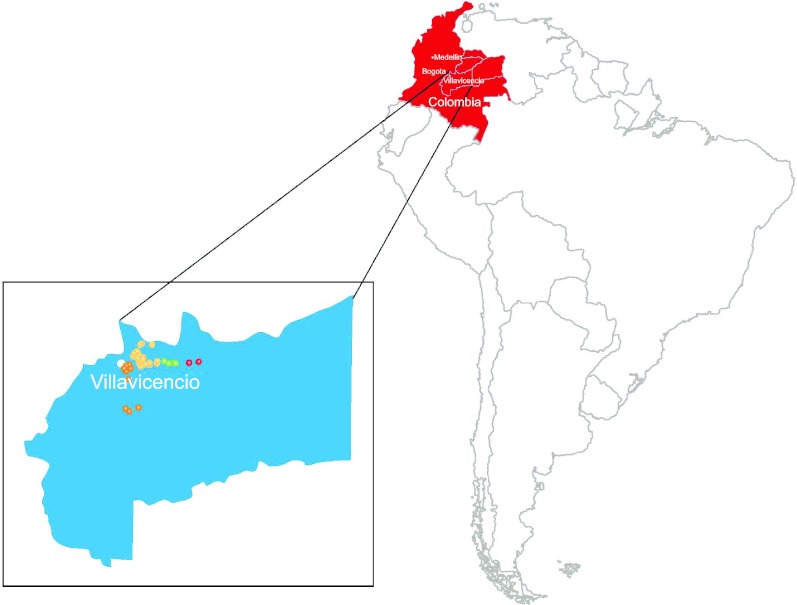
All sampling activities were performed or supervised by trained veterinarians and approved by the St Jude Children's Research Hospital Institutional Animal Care and Use Committee. The study was conducted between 2010 and 2012 in the Los Llanos region of Colombia, within a 90-km radius around Villavicencio (coordinates N04°04'23.3'' and W73°34'54.8'') in Meta province (Figure 1). Samples were collected with single-use polyester sterile swabs and stored separately in single plastic cryovials containing 1 mL of phosphate-buffered saline with 50% glycerol, penicillin 10 000 IU/mL, streptomycin 5 mg/mL, gentamicin sulfate 1 mg/mL, kanamycin sulfate 700 µg/mL and amphotericin B 10 µg/mL (Sigma Chemical Co, St Louis, MO, USA). Samples were stored on ice at 4 °C for a maximum of 2 days before long-term storage at −70 °C.
Figure 1.
Geographical location of sampling sites in Colombia. Colored points correspond to the sampling sites in each location in Meta Province. Smaller inset shows the Llanos region. Red=Puerto Lopez, green=Pachaquiaro, yellow=Villavicencio and orange=Ariari.
Wild birds
Two thousand and thirteen fecal samples were collected from wild birds at nine sites within 4 areas representing different ecosystems, habitats and landscapes: (i) piedmont or foot slope savanna; (ii) plains; (iii) wetlands; and (iv) rice fields. Specific sampling points were selected within each of the nine sites according to the following criteria: (i) records of the presence of resident and migratory waterfowl; (ii) the presence of resting or feeding areas for groups or flocks of wild birds; and (iii) interactions among humans, wild birds, and domestic animals. Each site was sampled at least twice per year.
Domestic poultry
One thousand one hundred and eighty-eight cloacal swabs and fecal samples were collected as previously described10,11 from domestic poultry at 11 sampling sites that included backyard poultry operations, small farms and slaughterhouses, Each site was sampled at least once per year.
Horses
Two hundred and twenty nasopharyngeal swabs were collected from horses at seven sampling sites, including farms and stables, as previously described.12 Each site was sampled at least once per year.
Swine
Six hundred and seventy-eight nasopharyngeal swabs were collected from swine at five sites, including farms and slaughterhouses, as previously described.11,13 Each site was sampled at least once per year.
Virus detection and isolation
Viral RNA was extracted from 50 µL samples on a Kingfisher Flex Magnetic Particle Processor (Thermo Fisher Scientific, Waltham, MA USA) by using the Ambion MagMAX-96 AI/ND Viral RNA Isolation kit (Life Technologies Corporation, Grand Island, NY, USA). RNA was screened by using a Bio-Rad CFX96 Real-Time PCR Detection System on a C1000 Thermocycler (Bio-Rad, Hercules, CA, USA), with TaqMan Fast Virus 1-Step Master Mix (Applied Biosystems, Foster City, CA, USA) and primers/probe specific for the influenza M gene (CDC, Atlanta, GA, USA).14 Samples with a fluorescence cycle threshold value <40 were considered positive. Efforts were made to isolate virus from all real-time reverse transcriptase polymerase chain reaction (RT-PCR)-positive samples in either embryonated chicken eggs or cell culture, as previously described.15,16 Virus titers were determined by the method of Reed and Munch17 on the basis of the 50% tissue culture infectious dose (TCID50) in Madin–Darby canine kidney (MDCK) cells or the 50% egg infectious dose (EID50).
Sequencing and phylogenetic analysis
Reverse transcription of viral RNA from the original sample, followed by PCR with specific primers (primer sequences available upon request) for each gene segment, was performed as described previously.18 Sanger sequencing was performed by the St Jude Hartwell Center and sequences were aligned by using the ClustalW and Bioedit programs.19,20 The eight gene segments were phylogenetically analyzed on the basis of their nucleotide sequences. Phylogenetic analysis used MEGA version 5.05 software with the neighbor-joining method, Kimura two-parameter model.21 Virus strains were clustered on the basis of nucleotides, and only dominant clusters were used to infer phylogenetic relationships. The nucleotide sequences obtained in this study are available from Genbank under accession numbers KC703309 to KC703350.
Cells
MDCK cells were cultured in Eagle's minimum essential medium (Gibco-Invitrogen, Carlsbad, CA, USA) supplemented with 2 mM glutamine and 10% fetal bovine serum (Gemini BioProducts, West Sacramento, CA, USA) and grown at 37 °C in 5% CO2. Well-differentiated (transepithelial resistance >1000) primary normal human bronchial epithelial (NHBE) cells were purchased from MatTek Corp. (Ashland, MA, USA), maintained by daily washing with 0.9% sodium chloride, and incubated at the air-liquid interface at 37 °C and 5% CO2. The basal surfaces remained in contact with AIR 100 growth medium (MatTek Corp.), which was replaced every 24 h.
In vitro virus replication
MDCK cells were infected at a multiplicity of infection (MOI) of 0.01 for 1 h at 37 °C. Cells were washed three times to remove unbound virus and cultured in appropriate medium containing 0.075% bovine serum albumin and 1 µg/mL L-1-tosylamide-2-phenylethyl chloromethyl ketone-treated trypsin. Aliquots of culture supernatants were collected at 24 and 48 h post-infection (pi) and immediately stored at –70 °C. For infection of NHBE cells, basal medium was removed and replaced with Dulbecco's modified eagle medium. The apical surface was washed twice and incubated with fresh, serum-free Dulbecco's modified eagle medium containing virus for 2 h at 37 °C, after which both apical and basal medium was removed and fresh growth medium was added to the basal chamber. At 6, 24, 48, 72 and 96 hpi, Dulbecco's modified eagle medium was added to the apical surface and the culture was incubated for 30 min at 37 °C. The medium was collected and stored at –80 °C for virus titration.
Animal experiments
All experiments and procedures were approved by the Animal Care and Use Committee at St Jude Children's Research Hospital.
Mice
Six- to eight-week-old female BALB/c mice (n=10; Jackson Laboratory, Bar Harbor, ME, USA) were lightly anesthetized with isoflurane and intranasally inoculated with 105 TCID50 of virus in 25 µL phosphate-buffered saline. Mice were monitored daily for clinical signs of infection22 and weighed every 48 h. At different times, three mice were euthanized and tissues were harvested. The large lung lobe was washed and immediately stored in 10% buffered formalin for histological analysis. The remaining lobe and extrapulmonary tissues were homogenized in 1 mL phosphate-buffered saline for virus titration.
Chickens
One-day-old white leghorn hatchlings (n=10; Charles Rivers, Wilmington, MA, USA) were provided food and water ad libitum and raised under specific pathogen-free conditions for 8 weeks before use. To determine the intravenous pathogenicity index (IVPI), 8-week-old chickens (n=5 per group) were intravenously inoculated with a 1:10 dilution of egg-grown virus in a volume of 100 µL. Animals were monitored for signs of illness for 10 days and scored (0=healthy, 1=ill, 2=severely ill, 3=dead) according to the World Health Organization Manual on Influenza Diagnosis and Surveillance.23 The IVPI was calculated from the mean score and used to assign one of three pathogenicity indices: highly pathogenic, non-pathogenic or intermediate.24 To determine virus shedding and pathogenicity after inoculation via natural routes, 8-week-old specific pathogen-free chickens (n=5 per group) were infected by intraocular, intranasal and intratracheal inoculation with 106 EID50 of virus in a volume of 0.5 mL and monitored daily for clinical signs of infection. To assess virus shedding, cloacal and tracheal swabs were collected from all birds every 48 h for 12 days. Swabs were stored in 1 mL (cloacal) or 0.5 mL (tracheal) viral transport medium at –70 °C for virus titration in eggs.
Statistical analysis
Experimental data were analyzed by using JMP Statistical Software (SAS Institute, Cary, NC, USA) and the statistical software package in Prism (GraphPad, La Jolla, CA, USA). Nonparametric data were compared by using the Kruskal–Wallis test. Normally distributed data were analyzed by two-way ANOVA with virus and day post-infection as main effects. Student's t-test was used for post hoc comparison of groups. Differences were considered to be statistically significant at P<0.05 (α=0.05 was prospectively selected).
To determine whether location or seasonal/climatic conditions affected viral prevalence within each species, we grouped the surveillance sites into four general locations (Villavicencio, Ariari, Puerto Lopez and Pachaquiaro) and established two periods, dry season (December–March) and rainy season (April–November), on the basis of historical climate records (mean temperature, rainfall, and relative humidity for the past 20 years, published by the Meteorological and Environmental Studies Institute of Colombia). Viral prevalence was compared across species by using the Pearson χ2 test or Tukey's multiple comparison test in Excel 2007 (Microsoft Corporation, Redmond, WA, USA). Differences were considered statistically significant at P<0.05.
Results
Prevalence of influenza viruses in the Llanos region of Colombia
During 2010–2012, we collected more than 4000 swab samples from horses, swine, domestic poultry and wild birds at various sites within the Llanos region (Figure 1) and screened RNA in the samples by real-time RT-PCR. As shown in Table 1, 13.4% of swine, 4.1% of horses, 3.6% of wild birds and 2.6% of poultry tested were influenza-positive. The proportion of positive samples differed significantly by species, location and even collection season (P<0.05). The Villavicencio region had the highest rate of positive samples (6.3%, n=2389), followed by Puerto Lopez (5.0%, n=378), Ariari (2.9%, n=382) and Pachaquiaro (2.53%, n=949). Samples collected during the rainy season (April–October, 6.9%) were significantly more likely to be positive than those collected during the dry season (November–March, 2.9%) (P<0.05).
Table 1. Influenza prevalence by species.
| Host (scientific name) | Number screened | Number positive | Percent positive | Number subtyped |
|---|---|---|---|---|
| Poultry | ||||
| Chicken (Gallus gallus domesticus) | 1003 | 28 | 2.79 | |
| Muscovy duck (Cairina moschata) | 12 | 0 | 0 | |
| Japanese quail (Coturnix japonica) | 84 | 1 | 1.19 | |
| Domestic goose (Anser anser domesticus) | 2 | 0 | 0 | |
| Domestic duck (Anas platyrhynchos domestica) | 87 | 2 | 2.30 | |
| Total | 1188 | 31 | 2.61 | |
| Horse | ||||
| Horse (Equus ferus caballus) | 220 | 9 | 4.09 | |
| Swine | ||||
| Swine (Sus scrofa domesticus) | 678 | 91 | 13.42 | 33 |
| Wild bird | ||||
| Various species | 2013 | 73 | 3.63 | 2 |
The majority of positive horse swabs were collected at a farm in the Ariari region, while the majority of positive swine and poultry swabs were collected at an abattoir in the Villavicencio region. This abattoir regularly purchases animals from farms throughout the province, limiting our ability to identify the origins of positive animals. The majority of positive poultry samples were from domestic chickens (Gallus gallus domesticus, n=1003), which also had the highest prevalence of influenza infection among poultry (2.8%). Positive samples were also collected from a Japanese quail (Coturix japonica) and from domestic ducks (Anas platyrhynchos domestica). Unfortunately, attempts to isolate viruses from positive horse and poultry swabs and to identify their subtypes were unsuccessful, a not unexpected result given the sensitivity of real-time RT-PCR. The majority of samples had cycle threshold (Ct) values around 37–39, whereas isolation is ideally achieved at or below a cycle threshold value of 33.25,26,27
Detection of pandemic H1N1 (pH1N1) influenza virus in swine
Of the 91 positive swine samples (Table 1), the majority (91.2%) were obtained on two separate dates at an abattoir and 2.5% were collected on farms. None of the animals exhibited clinical signs of infection. We were able to subtype 33 positive samples by conventional RT-PCR and Sanger sequencing and found that all were pH1N1 virus.
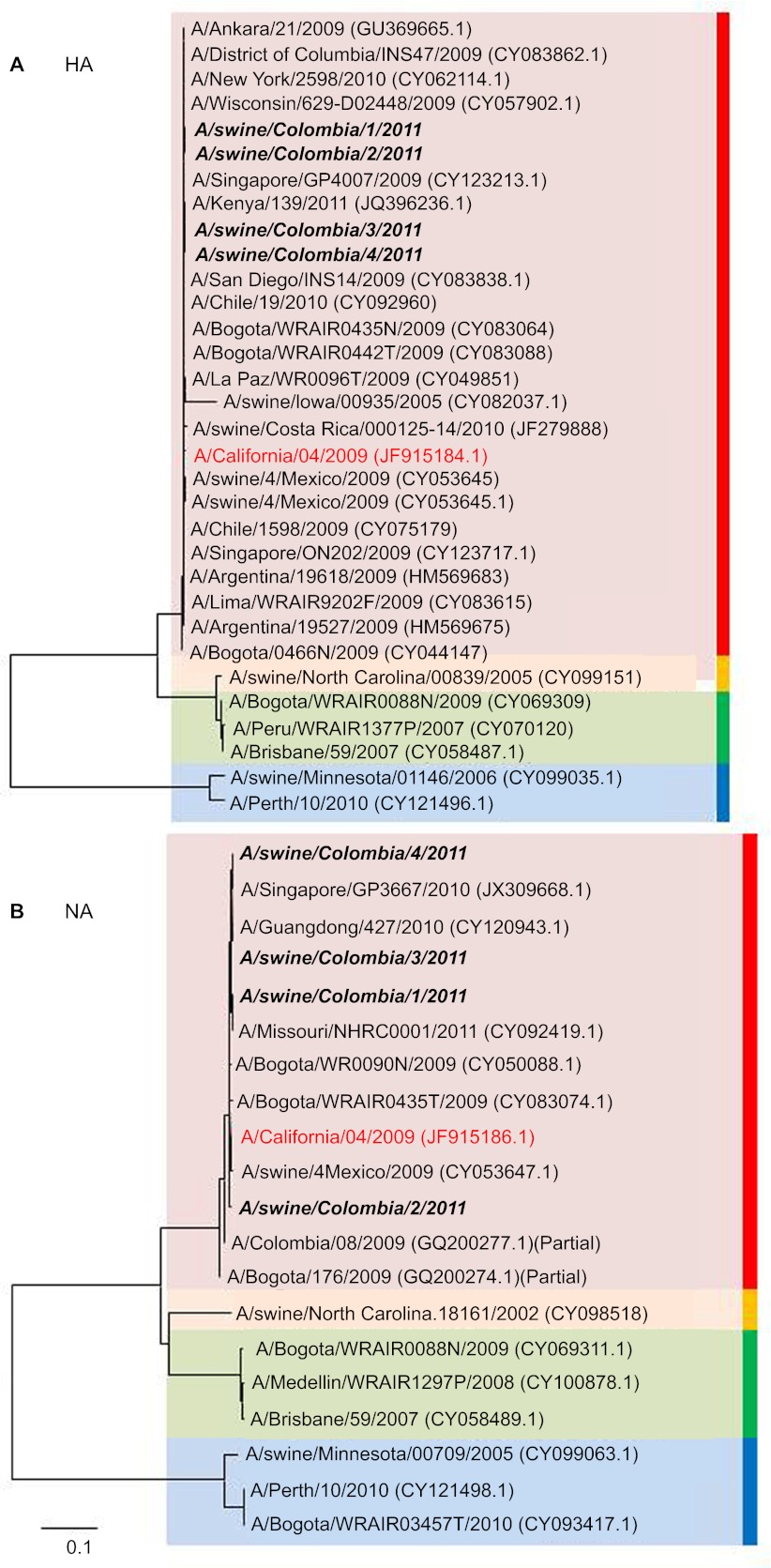
To determine whether any of the swine pH1N1 viruses were reassortants, we performed full-length sequencing of RNA from positive swabs. Phylogenetic analysis of four different samples confirmed that the pigs were infected with unaltered pH1N1 virus; genetic identity to other pH1N1 viruses ranged from 97% to 100%. The Colombian swine viruses clustered with other human and swine pH1N1 isolates (Figure 2 and Supplementary Figure S1). The hemagglutinin (HA) sequences of viruses from the first and second sampling dates differed from one another and differed significantly from the HAs of known pH1N1 pandemic strains (bootstrap values of 85 and 75, respectively) (Figure 2A). Similarly, the NS, NP and PA sequences showed temporal clustering (Supplementary Figures S1B–S1D). The NA sequences of pH1N1 showed no specific phylogenetic pattern (Figure 2B), nor did the M, PB1 or PB2 sequences (Supplementary Figures S1A, S1E and S1F). The M genes of three of the four isolates appeared to form a subclade different from those of other pH1N1 viruses (Supplementary Figure S1D), although additional viruses must be analyzed to confirm this finding. To our knowledge, this is the first report of pH1N1 virus in Colombian swine. Further, these findings differ from our early-2010 seroepidemiology study showing antibodies against classical swine H3N2 viruses in the Los Llanos swine (unpublished data). These findings demonstrate the need for ongoing surveillance, most importantly to ensure that Colombian pigs are not shedding reassortant pH1N1 and H3N2 viruses like those currently found in North American swine herds.28,29
Figure 2.
Phylogenetic trees of the HA (A) and NA (B) genes of influenza viruses isolated from swine in the Llanos region of Colombia. Trees were generated by using the neighbor-joining method in MEGA software. Trees are based on full genetic sequences of representative pandemic H1N1 (red), classical swine H1N1 (yellow), seasonal human H1N1 (green) and seasonal human and swine H3N2 (blue) viruses. Swine isolates are shown in black italics. An archetypal 2009 pandemic H1N1 strain (A/California/04/2009) is shown in red. Scale bars represent the number of substitutions per site.
Isolation of H5N2 influenza virus from whistling ducks
To date, there have been no reports of influenza viruses in Colombian wild bird populations. Of the 2013 samples collected from diverse wild bird species throughout the Llanos region (Supplementary Table S1), 58 (∼3.0%) were positive. Although most of the positive samples were derived from mixed or unknown species, positive samples were identified in the Anseriformes, Charadriiformes, Passeriformes and Pelicaniformes orders. Two influenza viruses were isolated from resident whistling ducks (genus Dendrocygna): A/black bellied whistling duck/Colombia/1/2011 (A/BBWD/Colombia/1/2011) and A/white faced whistling duck/Colombia/1/2011 (A/WFWD/Colombia/1/2011).
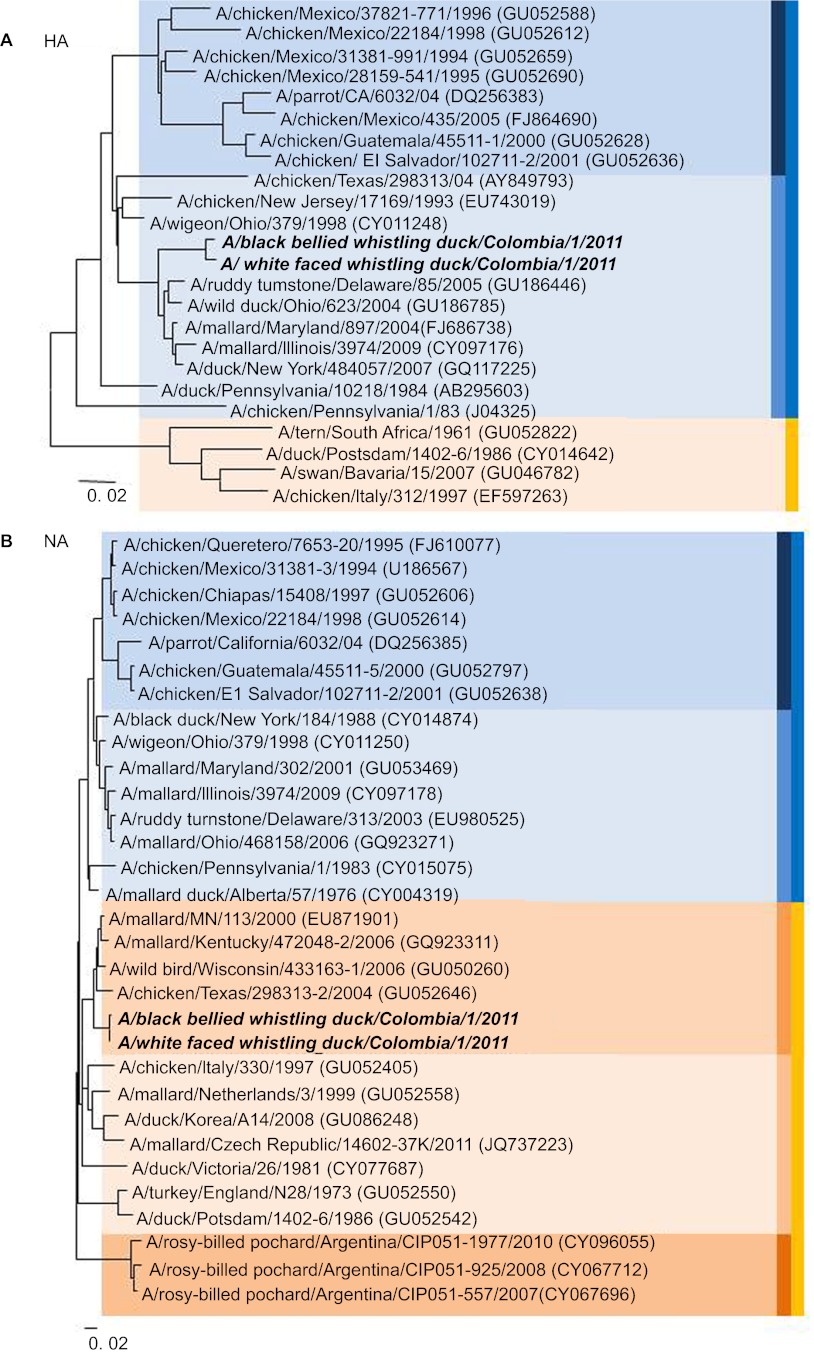
For comparison of the Colombian wild bird viruses with other avian influenza viruses, we performed full-length sequencing on the viral isolates followed by phylogenetic analysis (Figure 3 and Supplementary Figure S2). In analyses of all gene segments, the two Colombian H5N2 viruses were more closely related to each other than to any other influenza virus, and they formed clusters significantly distinct from those of the other strains analyzed. The gene segments of both viruses clustered with North American avian influenza viruses rather than with Central or South American avian influenza viruses (Figure 3); comparison of their relation to the North American vs. non-North American H5 lineages yielded a robust bootstrap value of 100. This finding may reflect the scarcity of influenza data from wild birds in Central and South America.
Figure 3.
Phylogenetic trees of the HA (A) and NA (B) genes of H5N2 influenza viruses isolated from whistling ducks in the Llanos region of Colombia. Trees were generated by using the neighbor-joining method in MEGA software. The HA tree is based on full genetic sequences from representative H5N2 viruses from Central/South America (dark blue), North America (light blue) and Eurasia/Oceania (yellow). The NA tree is based on full genetic sequences of representative HxN2 viruses from Central America (dark blue), North America (light blue/light orange), South America (dark orange) and Eurasia/Oceania (light yellow) and is divided into short (blue) and long (yellow) stalk lengths. Strains characterized in this study are shown in black italics. Scale bars represent the number of substitutions per site.
In the HA gene analysis, the closest relative was an H5N2 virus isolated from a wild duck in Ohio in 2004 (96% nucleotide similarity) (Figure 3A and Supplementary Table S2). Like other viruses in the North American lineage, the Colombian H5 viruses had a deduced amino-acid sequence of PQRETR*GLF at the multibasic cleavage site, a receptor binding domain suggesting avian specificity and inability to replicate in the absence of trypsin (signifying low pathogenicity) (Table 2). Like the HA segment, the NA genes of the Colombian viruses were more similar to each other than to any other strain or cluster in the North American clade of N2 viruses containing long NA stalks (Figure 3B and Table 2). The nearest relative to both strains was identified by the N2 sequence of A/mallard/MN/1/2000 (96% nucleotide similarity). The internal genes of the two isolates had 90%–98% sequence identity with those of their nearest relatives (Supplementary Table S2).
Table 2. Characteristics of the Colombian H5N2 avian viruses isolated.
| Virus | Subtype | Pathogenicity | Multibasic cleavage sitea | Growth without trypsin | NA stalklength | Reference |
|---|---|---|---|---|---|---|
| A/Chicken/Queretaro/14588-19/1995 | H5N2 | HP | PQRKRKTR*GLF | Yes | Short | 54 |
| A/tern/South Africa/1961 | H5N3 | HP | PQRETRRQKR*GLF | Yes | Long | 50 |
| A/Chicken/Pennsylvania/1/1983 | H5N2 | HP | PQKKKR*GLF | Yes | Short | 55 |
| A/Chicken/Mexico/26654-1374/1994 | H5N2 | LP | PQRETR*GLF | No | Short | 54 |
| A/mallard/Bavaria/1/2005 | H5N2 | LP | PQRETR*GLF | No | Long | 50 |
| A/WFWD/Colombia/1/2011 | H5N2 | LP | PQRETR*GLF | No | Long | |
| A/BBWD/Colombia/1/2011 | H5N2 | LP | PQRETR*GLF | No | Long |
Deduced amino-acid sequence.
Pathogenicity and replication of the Colombian H5N2 isolates in poultry
To evaluate the pathogenicity of the Colombian H5N2 viruses in chickens, groups of 6-week-old chickens (n=5/virus) were inoculated by natural route with the Colombian viruses and monitored for clinical signs of infection. Cloacal and tracheal swabs were collected for 8 days pi (Table 3). Although none of the chickens exhibited clinical signs of disease, 20% of those inoculated with A/WFWD/Colombia/1/2011 shed virus from the cloaca through day 4 pi, with a peak virus titer of 105.5 EID50/mL at day 2 pi (Table 3). Similarly, 40% of birds inoculated with A/BBWD/Colombia/1/2011 shed virus cloacally at day 2 pi (peak titer of 104 EID50/mL); only one bird was shedding by day 4 pi. There was no cloacal shedding after day 4, and no birds shed virus from the trachea. Both of the Colombian H5N2 viruses were nonpathogenic in chickens, with an intravenous pathogenicity index of 0 (Table 3).
Table 3. Growth and pathogenicity of the Colombian H5N2 viruses in chickens.
| Swab titer1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Virus | Trachea | Cloaca | IVPI | ||||||
| 2 dpi | 4 dpi | 6 dpi | 8 dpi | 2 dpi | 4 dpi | 6 dpi | 8 dpi | ||
| A/WFWD/Colombia/1/2011 | 0 (0/5)2 | 0 (0/5) | 0 (0/5) | 0 (0/5) | 5.5 (1/5) | 4.5 (1/5) | 0 (0/5) | 0 (0/5) | 0 |
| A/BBWD/Colombia/1/2011 | 0 (0/5) | 0 (0/5) | 0 (0/5) | 0 (0/5) | 4 (2/5) | 5.25 (1/5) | 0 (0/5) | 0 (0/5) | 0 |
Abbreviations: dpi, days post-infection; IVPI, intravenous pathogenicity index.
Log10 EID50/mL. Data are the average of 5 animals/group. Values in parenthesis are the number shedding/number tested.
Values of 0 were below the limit of detection (<1 log10 EID50/100 µL).
Replication of the Colombian H5N2 isolates in vitro and in mice
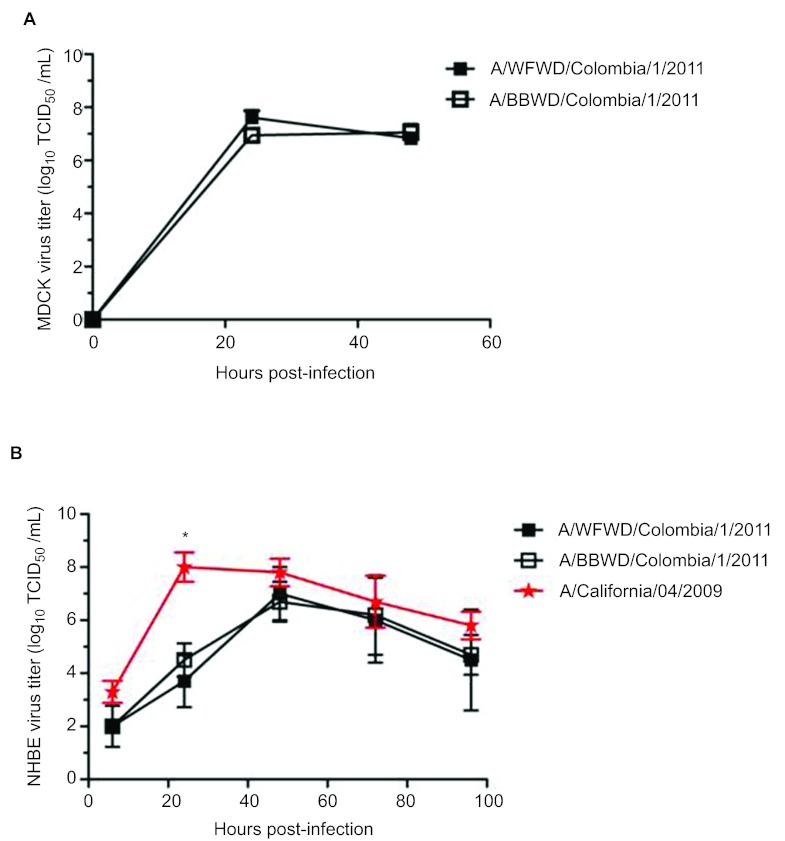
To assess replication in mammalian cells, MDCK and NHBE cells grown in an air-liquid interface were infected with the Colombian viruses at an MOI=0.01, and viral titers were monitored. Both viruses had comparable titers at 24 and 48 hpi in MDCK cells, reaching approximately 107 TCID50/mL by 24 hpi (Figure 4A). Surprisingly, the viruses also replicated in NHBE cells, although their kinetics were slower than those of the A/California/04/2009 (CA/09) H1N1 virus (Figure 4B). Titers of the Colombian viruses were 4 logs lower than those of CA/09 at 24 hpi, but were comparable by 48 hpi. These findings suggest that the Colombian avian viruses can replicate in mammalian cells.
Figure 4.
Replication of Colombian H5N2 viruses in vitro. MDCK (A) cells were infected at an MOI of 0.01, culture supernatants were collected at 0, 24 and 48 hpi, and virus was titrated as TCID50. (B) NHBE cells were maintained in culture at an air/liquid interface and infected at an MOI of 0.1. At 6, 24, 48 72 and 96 hpi, medium was added to the apical surface. Medium was collected after 30 min, and virus was titrated in triplicate as TCID50. Error bars represent the standard error of the mean. * P<0.05.
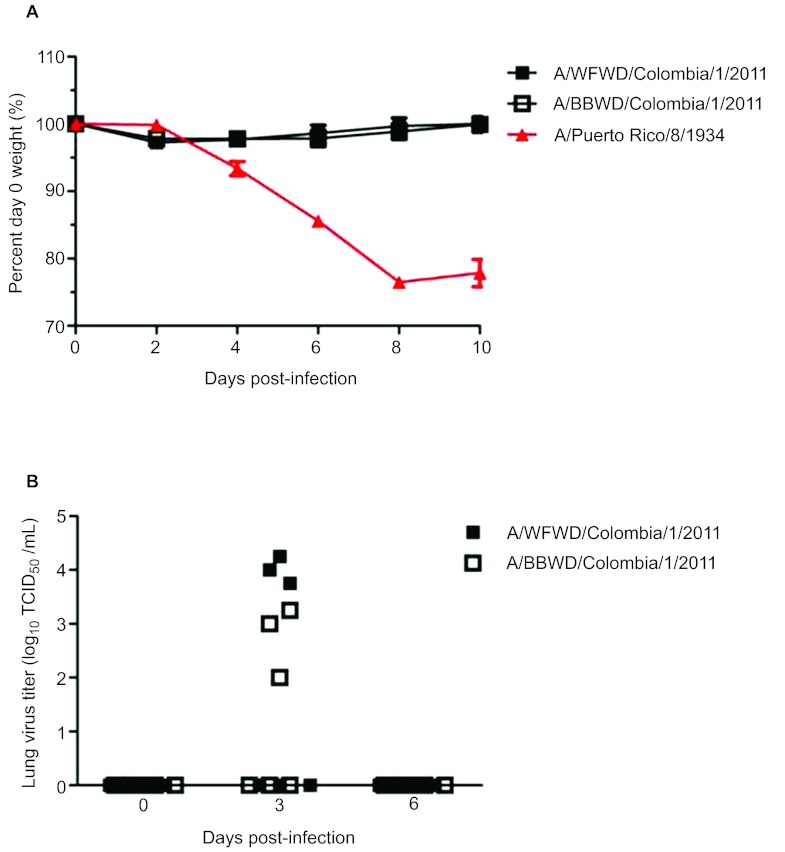
To assess pathogenicity in mammals, groups of ten 6- to 8-week-old female Balb/c mice were intranasally inoculated with 105 TCID50 of the Colombian viruses or of A/Puerto Rico/8/1934 (PR8) H1N1 virus, and weight loss and viral titers were monitored for 10 days. Unlike PR8 virus, neither Colombian H5 virus caused significant weight loss (Figure 5A); low viral titers were observed at day 3 pi, and virus was completely cleared by day 6 pi (Figure 5B). No significant histological lesions were observed in the lungs of mice inoculated with either strain (data not shown). These findings did not justify tests of the pathogenicity and transmission of these viruses in a ferret model. In summary, although the Colombian H5 viruses replicated in mammalian cell culture, they replicated only to a minor extent in inoculated mice and did not cause morbidity.
Figure 5.
Pathogenicity of Colombian H5N2 viruses in vivo. Female 6- to 8-week-old BALB/c mice (n=10) were infected intranasally with 105 TCID50 of the indicated viruses, and weight loss (A) was monitored for 14 dpi. (B) 0, 3 and 6 days after infection, lungs were collected from three mice per group and virus in homogenates was titrated as TCID50. Data represent the mean of at least two separate experiments. Error bars represent the standard error of the mean.
Discussion
Few other studies have investigated the prevalence of influenza viruses in diverse species in Colombia. The Llanos region, one of the world's richest tropical grasslands, provides habitat to a large number of resident and migratory birds.9 There is also extensive agriculture in the area, creating unique environment in which diverse species of migratory waterfowl are in contact with horses, swine and poultry, especially via backyard farming. For this reason, it was not surprising to find real-time RT-PCR evidence of influenza virus infection in a wide range of species.
Swine showed the highest prevalence of infection (13.4%), a rate much higher than the estimated prevalence of 4% in North American swine herds (personal communication, RJ Webby, St Jude Children's Research Hospital). Anti-influenza antibodies have previously been identified in swine in Brazil, Argentina, Venezuela, Chile and Colombia.30,31 However, only one other study has identified influenza infection (with a human H3N2 virus) in Colombian swine.31 Early during our surveillance (February 2010), we found antibodies to classical swine H3N2 viruses in swine in the Llanos region. However, by December 2010, pH1N1 virus was the only strain detected. Given that the swine viruses were identical to circulating human pH1N1 strains, they may have been introduced into swine by reverse zoonosis. The different sampling dates and the formation of two distinct clusters within the pH1N1 branch suggest two such events. As the majority of our surveillance was performed at abattoirs, we cannot comment on clinical disease in the swine herds, although it is interesting that most of the positive samples identified were from two separate herds of piglets, in which more than 80% were positive by real-time RT-PCR.
It raises concern that we found evidence of more recent infection of swine herds throughout Colombia with both pH1N1 and classical swine H3N2 viruses. In many parts of the world, there is evidence of continued reassortment between pH1N1 and classical swine H3N2 and H1N1 viruses. Several of these reassortants have crossed into humans,28,29,32,33,34,35,36 the most recent being the novel reassortant H3N2 viruses currently infecting humans in the United States.28,29,37,38,39 Similarly, swine in Argentina have been found to be infected with pH1N1 and seasonal human reassortants.40 These findings highlight the need for surveillance throughout Latin America to elucidate the extent of influenza prevalence and strain-specific prevalence in swine and the potential transmissibility of reassortants from swine to humans.
We also found that 2.6% of poultry and 3.6% of wild birds tested were positive for influenza virus. Both viruses and antibodies have been isolated previously from wild birds and poultry in South America, including H7 and H9 subtypes in Argentina, Chile, Bolivia, Colombia, Peru and Brazil.8,41,42,43,44,45,46 However, our study is the first to isolate H5 viruses in South America. H5-positive sera previously reported in Chilean poultry farms were later linked to a contaminated batch of vaccine.45 Our low-pathogenic H5N2 viruses were isolated from two species of resident whistling ducks, which are fairly common in Colombia both east and west of the Andes and are generally found in freshwater ponds, marshes and flooded fields.47 In Nigeria, white-faced whistling ducks were found to be healthy carriers of highly pathogenic H5N2 viruses.48,49,50 Both white-faced and black-bellied whistling ducks are generally considered non-migratory resident species; therefore, these viruses may have been introduced by migratory birds wintering in Colombia. Further, all of the virus genes from both white-faced and black-bellied whistling ducks clustered with sequences from wild migratory birds of the North American lineage (nucleotide similarity, 90%–98%), unlike the Argentinian H6 viruses that clearly evolved from South American-lineage viruses.44,51 Alternatively, the Colombian viruses may be part of a larger ‘South American' lineage yet to be identified by surveillance in South American wild birds.
Although the H5N2 viruses were low-pathogenic (IVPI scores of 0) in chickens,52 they replicated and were cloacally shed by 20% of inoculated chickens through day 4 pi. While the proportion of chickens shedding virus and the replication kinetics matched those of other low-pathogenic H5N2 strains,53 the efficient replication of these viruses indicated that they have the potential to spread if introduced into domestic poultry populations; therefore, they warrant continued surveillance.
The Colombian H5 viruses replicated efficiently in MDCK and NHBE cells; however, H5N2 virus infection was associated with little to no morbidity and limited viral replication in Balb/c mice. These findings suggest that the Colombian H5N2 viruses isolated from wild birds do not require immediate intervention, because (i) they do not contain the multibasic cleavage site or stalk deletion associated with highly pathogenic viruses; (ii) they were not highly pathogenic in inoculated chickens; and (iii) they do not replicate efficiently in a mammalian model. However, these studies highlight the need for continued influenza virus surveillance in Colombia and throughout South America.
Supplementary Information for this article can be found on Emerging Microbes and Infections's website (http://www.nature.com/emi/).
Acknowledgments
We thank Scott Krauss, Dr Mariette Ducatez, Dr Pam McKenzie, Dr Paul Thomas, Dr Pradyot Dash, Jerry Parker, Rich Elia and Bridgett Sharp (St Jude Children's Research Hospital, USA) for reagents and technical assistance. We also thank Dr Robert Webster and Dr Richard Webby (St Jude Children's Research Hospital, USA) for insightful discussion and experimental suggestions and Dr Paula Cancino, DVM (Colombian Association of Pig Farmers, Colombia) and Dr Julian Morales, DVM (Universidad de Los Llanos, Colombia) for logistic assistance. Finally, we thank the people who participated in field work: the veterinary students from the Universidad de Los Llanos and the Universidad Cooperativa de Colombia in Colombia, Johanna Murillo (the Corporacion Llanera de Ornitologia y de la Naturaleza—KOTSALA, Colombia), Adolfo Vasquez (the Corpotropica Corporation, Colombia), and the farmers, owners and keepers of the domestic animals. This work was supported in part by the NIH NIAID contract number HHSN266200700005C and the American Lebanese Syrian Associated Charities.
Supplementary Information
References
- Fouchier RA, Osterhaus AD, Brown IH. Animal influenza virus surveillance. Vaccine. 2003;21:1754–1757. doi: 10.1016/s0264-410x(03)00067-7. [DOI] [PubMed] [Google Scholar]
- Butler D. Flu surveillance lacking. Nature. 2012;483:520–522. doi: 10.1038/483520a. [DOI] [PubMed] [Google Scholar]
- Myers N, Mittermeier RA, Mittermeier CG, da Fonseca GA, Kent J. Biodiversity hotspots for conservation priorities. Nature. 2000;403:853–858. doi: 10.1038/35002501. [DOI] [PubMed] [Google Scholar]
- Orme CD, Davies RG, Burgess M, et al. Global hotspots of species richness are not congruent with endemism or threat. Nature. 2005;436:1016–1019. doi: 10.1038/nature03850. [DOI] [PubMed] [Google Scholar]
- Stotz DF, Fitzpatrick JW, Parker TA, Moskovitz DK. Neotropical birds, ecology and conservation. Chicago; IL: University of Chicago Press; 1996. [Google Scholar]
- González-Prieto AM, Hobson KA, Bayly NJ, Gómez C. Geographic origins and timing of fall migration of the Veery in northern Colombia. Condor. 2011;113:860–868. [Google Scholar]
- Cruz RES.Los humedales y la ocupación de aves en los cultivos de arroz Foro Arrocero Latinoamericano 2003925–28.Spanish. [Google Scholar]
- Senne DA. Avian influenza in North and South America, 2002–2005. Avian Dis. 2007;51:167–173. doi: 10.1637/7621-042606R1.1. [DOI] [PubMed] [Google Scholar]
- The Nature ConservancyColombia: the Llanos grasslands. Arlingtion, VA; The Nature Conservancy; 2011. Available at: http://www.nature.org/ourinitiatives/regions/southamerica/colombia/placesweprotect/llanos-grasslands.xml (accessed 17 November 2012). [Google Scholar]
- Negovetich NJ, Feeroz MM, Jones-Engel L, et al. Live bird markets of Bangladesh: H9N2 viruses and the near absence of highly pathogenic H5N1 Influenza. PLoS ONE. 2011;6:e19311. doi: 10.1371/journal.pone.0019311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. WHO manual on animal diagnosis and surveillance. Geneva; WHO; 2002. Available at: http://www.who.int/vaccine_research/diseases/influenza/WHO_manual_on_animal-diagnosis_and_surveillance_2002_5.pdf (accessed 1 January 2013). [Google Scholar]
- Diaz-Mendez A, Viel L, Hewson J, et al. Surveillance of equine respiratory viruses in Ontario. Can J Vet Res. 2010;74:271–278. [PMC free article] [PubMed] [Google Scholar]
- Couacy-Hymann E, Kouakou VA, Aplogan GL, et al. Surveillance for influenza viruses in poultry and swine, west Africa, 2006–2008. Emerg Infect Dis. 2012;18:1446–1452. doi: 10.3201/eid1809.111296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. CDC protocol of realtime RT-PCR for swine influenza A(H1N1). Geneva; WHO; 2009. Available at: http://www.who.int/csr/resources/publications/swineflu/CDCrealtimeRTPCRprotocol_20090428.pdf (accessed 1 January 2013). [Google Scholar]
- Moresco KA, Stallnecht DE, Swayne DE. Evaluation and attempted optimization of avian embryos and cell culture methods for efficient isolation and propagation of low pathogenicity avian influenza viruses. Avian Dis. 2010;54:622–626. doi: 10.1637/8837-040309-Reg.1. [DOI] [PubMed] [Google Scholar]
- Lira J, Moresco KA, Stallknecht DE, Swayne DE, Fisher DS. Single and combination diagnostic test efficiency and cost analysis for detection and isolation of avian influenza virus from wild bird cloacal swabs. Avian Dis. 2010;54:606–612. doi: 10.1637/8838-040309-Reg.1. [DOI] [PubMed] [Google Scholar]
- Reed LJ, Meunch H. A simple method of estimating fifty percent endpoints. Am J Hygiene. 1938;27:493–497. [Google Scholar]
- Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. Universal primer set for the full-length amplification of all influenza A viruses. Arch Virol. 2001;146:2275–2289. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]
- Chenna R, Sugawara H, Koike T, et al. Multiple sequence alignment with the Clustal series of programs. Nucleic Acids Res. 2003;31:3497–3500. doi: 10.1093/nar/gkg500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall TA. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp Ser. 1999;41:95–98. [Google Scholar]
- Kumar S, Nei M, Dudley J, Tamura K. MEGA: a biologist-centric software for evolutionary analysis of DNA and protein sequences. Brief Bioinform. 2008;9:299–306. doi: 10.1093/bib/bbn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton DB. A systematic approach for establishing humane endpoints. Ilar J. 2000;41:80–86. doi: 10.1093/ilar.41.2.80. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Manual for the laboratory diagnosis and virological surveillance of influenza. Geneva; WHO Press; 2011 [Google Scholar]
- Office International des Épizooties. Manual of diagnostic tests and vaccines for terrestrial animals. Paris; OIE; 2012 [Google Scholar]
- Munster VJ, Baas C, Lexmond P, et al. Spatial, temporal, and species variation in prevalence of influenza A viruses in wild migratory birds. PLoS Pathog. 2007;3:e61. doi: 10.1371/journal.ppat.0030061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferro PJ, Budke CM, Peterson MJ, et al. Multiyear surveillance for avian influenza virus in waterfowl from wintering grounds, Texas coast, USA. Emerg Infect Dis. 2010;16:1224–1230. doi: 10.3201/eid1608.091864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moresco KA, Stallknecht DE, Swayne DE. Evaluation of different embryonating bird eggs and cell cultures for isolation efficiency of avian influenza A virus and avian paramyxovirus serotype 1 from real-time reverse transcription polymerase chain reaction-positive wild bird surveillance samples. J Vet Diagn Invest. 2012;24:563–567. doi: 10.1177/1040638712440991. [DOI] [PubMed] [Google Scholar]
- Nelson MI, Vincent AL, Kitikoon P, Holmes EC, Gramer MR. Evolution of novel reassortant A/H3N2 influenza viruses in North American swine and humans, 2009–2011. J Virol. 2012;86:8872–8878. doi: 10.1128/JVI.00259-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Notes from the field: outbreak of influenza A (H3N2) virus among persons and swine at a county fair—Indiana, July 2012 MMWR 201261561. [PubMed] [Google Scholar]
- Rajao DS, Alves F, del Puerto HL, et al. Serological evidence of swine influenza in Brazil. Influenza Other Respi Viruses. 2013;7:109–112. doi: 10.1111/j.1750-2659.2012.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio JA, Pena L, Dibárbora M, et al. Outbreak of swine influenza in Argentina reveals a non-contemporary human H3N2 virus highly transmissible among pigs. J Gen Virol. 2011;92:2871–2878. doi: 10.1099/vir.0.036590-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger WS, Gray GC.Swine influenza virus infections in man Curr Top Microbiol Immunol 2012. in press [DOI] [PubMed]
- Pascua PNQ, Song MS, Lee JH, et al. Virulence and transmissibility of H1N2 influenza virus in ferrets imply the continuing threat of triple-reassortant swine viruses. Proc Nat Acad Sci USA. 2012;109:15900–15905. doi: 10.1073/pnas.1205576109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zell R, Scholtissek C, Ludwig S.Genetics, evolution, and the zoonotic capacity of European swine influenza viruses Curr Top Microbiol Immunol 2012. in press [DOI] [PubMed]
- Hiromoto Y, Parchariyanon S, Ketusing N, et al. Isolation of the Pandemic (H1N1) 2009 virus and its reassortant with an H3N2 swine influenza virus from healthy weaning pigs in Thailand in 2011. Virus Res. 2012;169:175–181. doi: 10.1016/j.virusres.2012.07.025. [DOI] [PubMed] [Google Scholar]
- Barman S, Krylov PS, Fabrizio TP, et al. Pathogenicity and transmissibility of North American triple reassortant swine influenza A viruses in ferrets. PLoS Pathog. 2012;8:e1002791. doi: 10.1371/journal.ppat.1002791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killian ML, Swenson SL, Vincent AL, et al. Simultaneous infection of pigs and people with triple-reassortant swine influenza virus H1N1 at a U.S. county fair Zoonoses Public Health 2012. in press [DOI] [PubMed]
- Lindstrom S, Garten R, Balish A, et al. Human infections with novel reassortant influenza A(H3N2)v viruses, United States, 2011. Emerg Infect Dis. 2012;18:834–837. doi: 10.3201/eid1805.111922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce MB, Jayaraman A, Pappas C, et al. Pathogenesis and transmission of swine origin A(H3N2)v influenza viruses in ferrets. Proc Nat Acad Sci USA. 2012;109:3944–3949. doi: 10.1073/pnas.1119945109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereda A, Rimondi A, Cappuccio J, et al. Evidence of reassortment of pandemic H1N1 influenza virus in swine in Argentina: are we facing the expansion of potential epicenters of influenza emergence. Influenza Other Respi Viruses. 2011;5:409–12. doi: 10.1111/j.1750-2659.2011.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senne DA. Avian influenza in North and South America, the Caribbean, and Australia, 2006–2008. Avian Dis. 2010;54:179–186. doi: 10.1637/8921-050809-Review.1. [DOI] [PubMed] [Google Scholar]
- Ghersi BM, Sovero MM, Icochea E, et al. Isolation of low-pathogenic H7N3 avian influenza from wild birds in Peru. J Wildl Dis. 2011;47:792–795. doi: 10.7589/0090-3558-47.3.792. [DOI] [PubMed] [Google Scholar]
- Rimondi A, Xu K, Craig MI, et al. Phylogenetic analysis of H6 influenza viruses isolated from rosy-billed pochards (Netta peposaca) in Argentina reveals the presence of different HA gene clusters. J Virol. 2011;85:13354–13362. doi: 10.1128/JVI.05946-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu K, Ferreri L, Rimondi A, et al. Isolation and characterization of an H9N2 influenza virus isolated in Argentina. Virus Res. 2012;168:41–47. doi: 10.1016/j.virusres.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Max V, Herrera J, Moreira R, Rojas H. Avian influenza in Chile: a successful experience. Avian Dis. 2007;51:363–365. doi: 10.1637/7631-042806R1.1. [DOI] [PubMed] [Google Scholar]
- Spackman E, McCracken KG, Winker K, Swayne DE. H7N3 avian influenza virus found in a South American wild duck is related to the Chilean 2002 poultry outbreak, contains genes from equine and North American wild bird lineages, and is adapted to domestic turkeys. J Virol. 2006;80:7760–7764. doi: 10.1128/JVI.00445-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilty SL, Brown B. A guide to the birds of Colombia. Princeton, NJ; Princeton University Press; 1986. [Google Scholar]
- Olsen B, Munster VJ, Wallensten A, Waldenstrom J, Osterhaus AD, Fouchier RA. Global patterns of influenza a virus in wild birds. Science. 2006;312:384–388. doi: 10.1126/science.1122438. [DOI] [PubMed] [Google Scholar]
- Wallensten A, Munster VJ, Latorre-Margalef N, et al. Surveillance of influenza A virus in migratory waterfowl in northern Europe. Emerg Infect Dis. 2007;13:404–411. doi: 10.3201/eid1303.061130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaidet N, Cattoli G, Hammoumi S, et al. Evidence of infection by H5N2 highly pathogenic avian influenza viruses in healthy wild waterfowl. PLoS Pathog. 2008;4:e1000127. doi: 10.1371/journal.ppat.1000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereda AJ, Uhart M, Perez AA, et al. Avian influenza virus isolated in wild waterfowl in Argentina: evidence of a potentially unique phylogenetic lineage in South America. Virology. 2008;378:363–370. doi: 10.1016/j.virol.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office International des Epizotes. Highly pathogenic avian influenza Manual of diagnostic tests and vaccines for terrestrial animals Paris; OIE; 2006. Chapter 2.3.4. [Google Scholar]
- van der Goot JA, de Jong MC, Koch G, van Boven M. Comparison of the transmission characteristics of low and high pathogenicity avian influenza A virus (H5N2) Epidemiol Infect. 2003;131:1003–1013. doi: 10.1017/s0950268803001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horimoto T, Rivera E, Pearson J, et al. Origin and molecular changes associated with emergence of a highly pathogenic H5N2 influenza virus in Mexico. Virology. 1995;213:223–230. doi: 10.1006/viro.1995.1562. [DOI] [PubMed] [Google Scholar]
- Snoeck CJ, Gerloff NA, Tanasa RI, Abad FX, Muller CP.Influenza virus: highly pathogenic avian influenzaIn: Elschner MC, Cutler SJ, Weidmann M, Butaye P (ed.)BSL3 and BSL4 agents: epidemiology, microbiology, and practical Guidelines. Weinheim; Wiley-Blackwell, ; 2012173–200. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.