Recent changes in human lifestyles have led to a global epidemic of insulin-resistant type 2 diabetes (1). Type 2 diabetes is a multisystem disorder characterized by the disruption of insulin signaling pathways critical to the integration of tissue repair and nutrient homeostasis that results in loss of protection against a range of chronic disorders of human health including arterial atherosclerosis (2). As a result, type 2 diabetes is a major cause of myocardial infarction, stroke, and peripheral vascular disease affecting millions of individuals worldwide. Insulin resistance, characterized by an initial compensatory increase in insulin production, is a progressive disorder that can differentially affect organs, tissues, cells, and intracellular signaling pathways at different stages of the disease (3).
It has recently emerged that in addition to its classical target tissues including liver, skeletal muscle, and adipose tissue, insulin resistance can occur in the endothelium where insulin has been shown to stimulate the release of the signaling radical nitric oxide (NO) (4). As a result, the endothelium, which was previously thought to be an inert lining of the blood vessel, is now established as a highly active organ that regulates a multitude of processes critical to vascular function (5).
NO, a metabolite of L-arginine to L-citrulline conversion by endothelial NO synthase (eNOS), is released by the endothelium in response to cues such as shear stress and growth factors and has a favorable effect on inflammation (6), thrombosis (7), vascular tone (8), and oxidative stress (9). A decrement in NO bioavailability may occur as a result of reduced biosynthesis and/or increased degradation by reactive oxygen species, a situation frequently described as oxidative stress (10). We have shown that insulin resistance specifically in the endothelium reduces NO bioavailability and increases the generation of potentially toxic levels of free radicals such as superoxide (11,12); this supports the hypothesis that insulin resistance at the level of the endothelium contributes to accelerated vascular disease seen in individuals with type 2 diabetes, and argues for the idea that it is a legitimate therapeutic target to treat diabetes-related atherosclerosis, as suggested by Rask-Madsen et al. (13).
The compelling evidence supporting a relationship between insulin resistance and atherosclerosis has led to the development of therapies targeting insulin resistance. Peroxisome proliferator–activated receptor (PPAR)-γ is the target of the thiazolidinediones, agents that have been shown to enhance insulin sensitivity that have been used in patients with type 2 diabetes (14). However, doubts regarding the cardiovascular safety of the PPAR-γ agonist rosiglitazone have recently emerged (15). Questions remain regarding whether or not enhancing insulin sensitivity in the vascular wall of patients with type 2 diabetes is an appropriate therapeutic strategy.
Two comprehensive studies from the laboratory of Domenico Accili (16,17) have begun to address this question. By deleting the three isoforms of FoxO specifically in the endothelium, Accili and colleagues generated a model in which the restraining effect of the FoxOs on endothelial insulin signaling is removed. The FoxO transcription factors (encoded by FoxO1, FoxO3a, and FoxO4) are downstream of Akt (a critical node in insulin-mediated NO release) and inhibit eNOS expression. Moreover, negative feedback effects of FoxOs on upstream insulin signaling elements such as Akt can also dampen insulin signaling. Endothelium-specific FoxO-deficient mice (VECKO) therefore provide a useful model to examine the effect of increased insulin action in the endothelium at different stages of type 2 diabetes.
In a model of advanced atherosclerosis and metabolic dysfunction (VECKO mice crossed onto an atherosclerosis-prone LDL receptor–deficient (Ldlr−/−) background), the Accili laboratory demonstrated that the deletion of all three FoxO isoforms in the endothelium has a potentially favorable effect on the development of vascular dysfunction and atherosclerosis (17). VECKO/Ldlr−/− mice fed a Western-style diet in comparison with Ldlr−/− mice with all three isoforms of FoxO intact demonstrated increased arterial relaxation in response to acetylcholine, indicative of increased bioavailability of NO. Consistent with these findings, VECKO/Ldlr−/− mice had reduced endothelial inflammation, reduced oxidative stress, and less atherosclerosis. By contrast, in this model of metabolic and vascular dysfunction, no beneficial effect on metabolic parameters or glucose homeostasis was shown. These data present a relatively straightforward paradigm whereby increasing insulin sensitivity in the endothelium has a favorable effect on NO bioavailability and atherosclerosis.
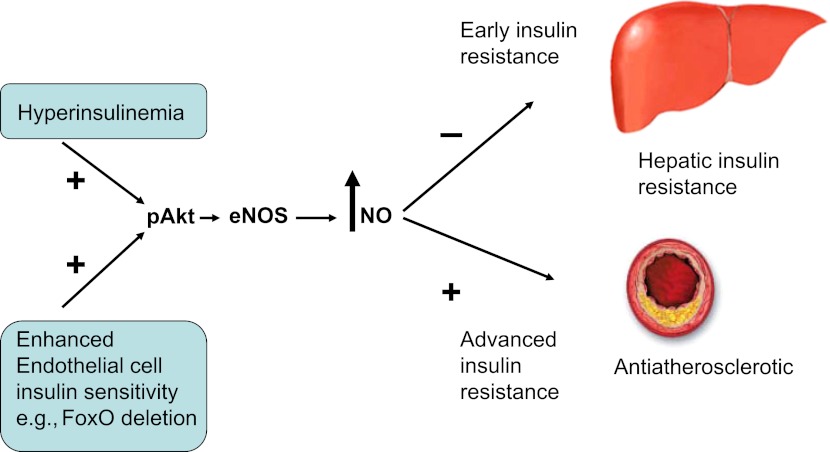
In the second part of the story, which is highlighted in this issue of Diabetes, a more complex picture emerges. Tsuchiya and Accili (16) examined the effect of the deletion of the FoxOs in mouse endothelium against a C57BL/6 background and standard chow diet. Intriguingly, standard chow–fed VECKO mice were glucose intolerant and had reduced insulin sensitivity; the defect in insulin action was identified as being in the liver. As expected, increasing insulin sensitivity in liver endothelial cells by deleting the FoxOs increased eNOS-derived NO. Surprisingly, NO reduced hepatic insulin sensitivity by tyrosine nitration of the insulin receptor in hepatocytes. Further experiments confirmed the source of the NO as eNOS rather than the inducible isoform iNOS, which has been shown to have a pathophysiological role in obesity-related insulin resistance (18). Complementary studies of hyperinsulinemia produced similar results, and inhibiting eNOS in a model of early insulin resistance had favorable effects on glucose homeostasis. It should be noted that the effect of FoxO deletion on endothelial cell function in the aorta or other arteries was not examined; it would be interesting to know whether or not—despite insulin resistance and glucose intolerance—FoxO deletion in the endothelium has a favorable effect on endothelial cell function in atherosclerosis-prone vessels (Fig. 1).
FIG. 1.
Schemata showing divergent effects of increased endothelial cell insulin sensitivity or hyperinsulinemia on NO bioavailability. Negative effect of increased NO on hepatic glucose homeostasis in early insulin resistance and favorable effect on atherosclerosis in more advanced metabolic disease.
So where does the phenotype of the endothelium-specific FoxO-deficient mouse leave us? The new data support insulin sensitization in the vascular endothelium as a useful strategy in advanced vascular disease. The data from mice without the severe insult of hypercholesterolemia are more challenging to reconcile with our current way of thinking about NO and type 2 diabetes. With the important caveat that the effect of different mechanisms of enhancing insulin sensitivity in the endothelium other than the deletion of FoxOs need to be examined, Tsuchiya and Accili (16) show that, in the case of NO and hepatic glucose homeostasis, it is possible to get too much of a good thing. Their results raise the exciting possibility that the hyperinsulinemia of early insulin resistance is a legitimate therapeutic target.
ACKNOWLEDGMENTS
The work from M.T.K.'s laboratory is supported by the British Heart Foundation.
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 1478.
REFERENCES
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4–14 [DOI] [PubMed] [Google Scholar]
- 2.Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet 2006;368:29–36 [DOI] [PubMed] [Google Scholar]
- 3.Jiang ZY, Lin YW, Clemont A, et al. Characterization of selective resistance to insulin signaling in the vasculature of obese Zucker (fa/fa) rats. J Clin Invest 1999;104:447–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muniyappa R, Montagnani M, Koh KK, Quon MJ. Cardiovascular actions of insulin. Endocr Rev 2007;28:463–491 [DOI] [PubMed] [Google Scholar]
- 5.Kearney MT, Duncan ER, Kahn M, Wheatcroft SB. Insulin resistance and endothelial cell dysfunction: studies in mammalian models. Exp Physiol 2008;93:158–163 [DOI] [PubMed] [Google Scholar]
- 6.Clapp BR, Hingorani AD, Kharbanda RK, et al. Inflammation-induced endothelial dysfunction involves reduced nitric oxide bioavailability and increased oxidant stress. Cardiovasc Res 2004;64:172–178 [DOI] [PubMed] [Google Scholar]
- 7.Schäfer A, Wiesmann F, Neubauer S, Eigenthaler M, Bauersachs J, Channon KM. Rapid regulation of platelet activation in vivo by nitric oxide. Circulation 2004;109:1819–1822 [DOI] [PubMed] [Google Scholar]
- 8.Creager MA, Cooke JP, Mendelsohn ME, et al. Impaired vasodilation of forearm resistance vessels in hypercholesterolemic humans. J Clin Invest 1990;86:228–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monastyrskaya E, Folarin N, Malyshev I, Green C, Andreeva L. Application of the nitric oxide donor SNAP to cardiomyocytes in culture provides protection against oxidative stress. Nitric Oxide 2002;7:127–131 [DOI] [PubMed] [Google Scholar]
- 10.Cai H, Harrison DG. Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res 2000;87:840–844 [DOI] [PubMed] [Google Scholar]
- 11.Duncan ER, Crossey PA, Walker S, et al. Effect of endothelium-specific insulin resistance on endothelial function in vivo. Diabetes 2008;57:3307–3314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sukumar P, Viswambharan H, Imrie H, et al. Nox2 NADPH oxidase has a critical role in insulin resistance–related endothelial cell dysfunction. Diabetes. 1 February 2013 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rask-Madsen C, Li Q, Freund B, et al. Loss of insulin signaling in vascular endothelial cells accelerates atherosclerosis in apolipoprotein E null mice. Cell Metab 2010;11:379–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kahn CR, Chen L, Cohen SE. Unraveling the mechanism of action of thiazolidinediones. J Clin Invest 2000;106:1305–1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med 2007;356:2457–2471 [DOI] [PubMed] [Google Scholar]
- 16.Tsuchiya K, Accili D. Liver sinusoidal endothelial cells link hyperinsulinemia to hepatic insulin resistance. Diabetes 2013;62:1478–1489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsuchiya K, Tanaka J, Shuiqing Y, et al. FoxOs integrate pleiotropic actions of insulin in vascular endothelium to protect mice from atherosclerosis. Cell Metab 2012;15:372–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Noronha BT, Li J-M, Wheatcroft SB, Shah AM, Kearney MT. Inducible nitric oxide synthase has divergent effects on vascular and metabolic function in obesity. Diabetes 2005;54:1082–1089 [DOI] [PubMed] [Google Scholar]