Abstract
Pyogenic granuloma is a benign lesion and usually occurs after trauma. Disseminated pyogenic granuloma, is a rare form of pyogenic granuloma. There are 9 cases of disseminated pyogenic granuloma in literature and most of them are hot milk burns. First case describes an 18- month-old girl who developed disseminated pyogenic granulomas on her right cheek, neck, and right nasal ala. Lesions on her right cheek and neck were excised and sutured primarily. Lesion on right nasal ala was excised and repaired with full thickness skin graft. Second case describes a 7-years- old boy who developed pyogenic granulomas on his left forearm. These lesions were excised and sutured primarily. In both cases lesions were developed after scald burn. During 6-month follow-up, no recurrence was observed in both cases.
Keywords: Pyogenic granuloma, burn
Introduction
Pyogenic granuloma (PG) is a proliferation of capillaries arising at the site of trauma. An association infection may occur, but the condition is not an infectious process [1]. This lesion is a common acquired vascular tumor in the pediatric age group. They are rare before the age of 6 months, generally occurring in older children (mean age, 6, 7 years) [2].
Pyogenic granulomas have a pliable surface and bleed easily. They occur most often on the face and distal extremities, probably because of the higher incidence of minor trauma at these sites. There have been several reports of solitary PG after trauma. Nevertheless, the eruptive, disseminated form of PG, which is characterized by sudden development of abundant bleeding, angiomatous papules secondary to a second degree burn, is extremely rare [3-8] For these reasons, we report two cases of a child with PG that developed after second degree scald burn.
Case report
First case
A 2-year-old girl presented with multiple PGs on her face and neck. The patient had second degree scald on her face and neck playing near an oven. The patient was followed in another facility by daily dressing using Thiocilline skin pomade (Bacitracin 500IU/g, Neomycin sulfate 5mg/g) After 2 weeks of daily dressing changes, wound healing occurred. During 15- day follow up, pappulomatos lesions developed on the patient’s right cheek, neck, and right nasal edge (Figure 1). Lesions had symptoms of intermittent bleeding and growth. A month after the injury, the patient was presented to the outpatient clinic for examination of this lesion. She was admitted to the hospital for pyogenic granuloma pre-diagnosis. On admission there were polypoid, soft, bleeding surface lesions with irregular margins on the right cheek, right neck and right nasal ala at a size of 4x2 cm, 2x1 cm, and 0.5x1 cm respectively. The patient was operated 3 days after admission. The lesions on her right cheek and neck were excised and primarily sutured. The lesion on the right alar wing was excised and fixed with a full thickness skin graft (FTSG) harvested from the post auricular region. Histopathological examination showed stratified squamous epithelium with intense inflammatory cell proliferation and many vessel structures (Figure 2A) showing immune reaction with CD34 (Figure 2B) varying in size. No recurrence was observed during 6- month follow-up (Figure 3).
Figure 1.

The appearance of the disseminated pyogenic granulomas on the patient’s right cheek, neck and nasal ala when she was admitted to our hospital 6 weeks after burn injury.
Figure 2.
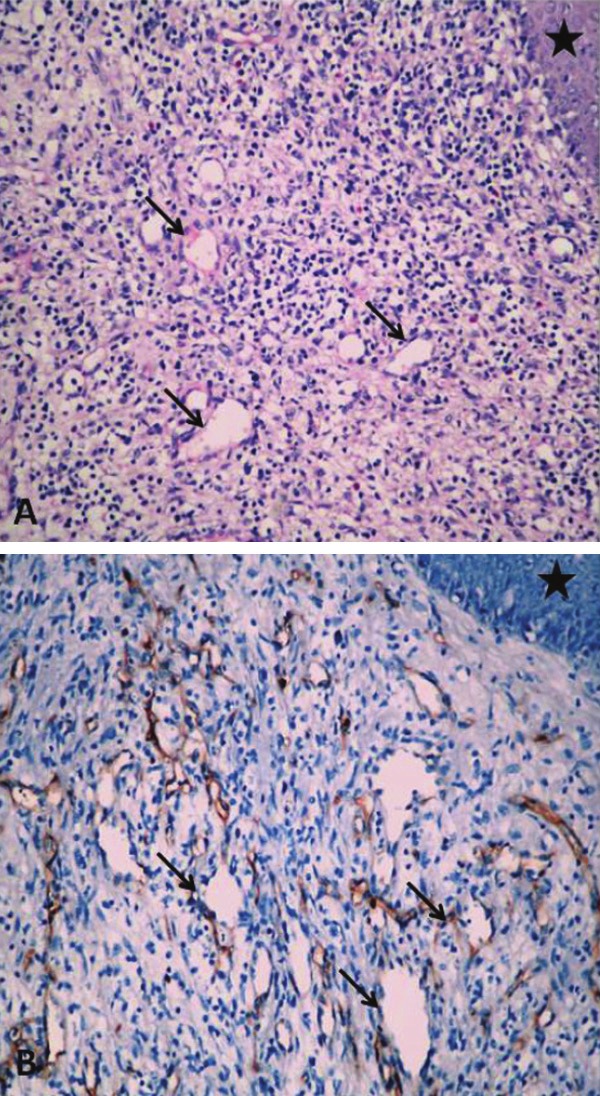
A. Stratified squamous epithelium (star) with intense inflammatory cell proliferation and many vessel structures. B. Immunoreactivity of vascular structures under Stratified squamous epithelium (star) with CD 34 showing immunoreactivity with CD 34.
Figure 3.

Postoperative view of patient after 2 months.
Second case
A 7-year-old boy presented with pyogenic granuloma on his forearm. The patient had second degree burn with boiling water. The patient was followed on outpatient basis by daily dressing using Thiocilline (Bacitracin 500IU/g, Neomycin sulfate 5mg/g) skin pomade. After 2 weeks, wound healing occurred, but papillomatous lesions developed on the patient’s left forearm (Figure 4). Lesions showed intermittent bleeding and growth. Three weeks after the injury, the patient was presented to the outpatient clinic for examination of this lesion. He was admitted to the hospital for pyogenic granuloma pre-diagnosis. On admission, there were papillomatous, soft, bleeding surface lesions on the left forearm. The patient was operated 3 days after admission. All the lesions were excised and primarily sutured. Histopathological examination revealed pyogenic granuloma. No recurrence was observed during 6- month follow-up (Figure 5).
Figure 4.

The appearance of the disseminated pyogenic granulomas on the patient’s left forearm when he was admitted to our hospital 3 weeks after burn injury.
Figure 5.

Postoperative view of the patient.
Discussion
Pyogenic granuloma, which is also known as Lobular capillary hemangioma, was first identified by Poncet and Dor in 1897 [3]. While etiology of pyogenic granuloma is unclear, trauma, infections, elevation in female sex hormone levels, viral oncogenes, microscopic arteriovenous anastomosis, and growth factors are shown as possible factors [9-11]. Burn is a frequent trauma; however, development of pyogenic granuloma afterwards is rare. Literature research revealed that only 9 patients had pyogenic granuloma with burn trauma. The details on these patients are given in Table 1. Of these patients, hot milk burn constitutes the most frequent etiology. In our two patients, pyogenic granuloma developed after second degree scald burn, but no pyogenic granuloma development due to scald burn has been reported before.
Table 1.
Reported pyogenic granuloma developed on burned skin area
| Age | Sex | Etiology | Location of burn | Degree of burn | |
|---|---|---|---|---|---|
| Male (M)/Female (F) | |||||
| Özbayoğlu et al, 2011 | 8 | M | Flame | Trunk | Second |
| Ceyhan et al, 2007 | 12 | M | Unknown | Arm | Second |
| Bozkurt et al, 2006 | 2 | M | Boiling milk | Forearm | Second |
| Aliağaoğlu et al, 2006 | 5 | F | Unknown | Arm | Second |
| Ceyhan et al, 1997 | 18 | F | Boiling milk | Arm | Second |
| Momeni et al, 1995 | 18 | M | Boiling milk | Trunk | Second |
| 5 | F | Boiling milk | Trunk | Second | |
| 35 | F | Boiling milk | Trunk | Second | |
| Kaminsky et al, 1978 | 15 | F | Boiling milk | Trunk | Second |
Multiple disseminated pyogenic granuloma is a rare form of PG and generally seen after traumas such as burns. Pathogenesis of this variant is not fully understood. Some research revealed that bacteria, fungi, and viruses play a role [3-8]. However, there is not an exact proof that these organisms cause PG. Another theory suggests that milk proteins or an unknown component in milk triggers PG development since a large number of patients with hot milk burns developed PG [4]. However, in our patient, the etiology was hot water burn. Therefore, other mechanisms after burn trauma are responsible for PG development rather than the etiologic agent that caused the burn.
Differential diagnosis for pyogenic granuloma includes many benign and malign lesions such as amelanotic melanoma, angiosarcoma, basal cell carcinoma, kaposi sarcoma, hemangioma, bacillary angiomatosis, metastatic visceral malignancies, and granulation tissue [12]. The lesions in our patient were similar to excessive granulation tissue. Differential diagnosis was made based on the histopathologic examination.
Treatment choices include cryotherapy, curettage and shaving, cauterization, pulsed-dye laser and surgical excision for PG. In a study on 408 patients by Giblin et al, recurrence was founded minimum by surgical excision and primary closure [13]. In another study involving 178 patients, by Patrice et al, the patients treated with surgical excision showed no recurrence, while 43.5% of the patients treated with cauterization only or tangential excision and cauterization showed recurrence [2].
In both patient, the lesions were surgically excised and primarily closed. However, in the first patient defect occurred after excision of the lesion on the right alar wing was inappropriate for primary closure due to its size. Therefore, defect closure was achieved through FTSG taken from postauricular region. No recurrence was observed in both cases during 6-month follow up.
Disseminated PG due to burn is very rare. Etiologic agent in most of the patients reported is milk. Disseminated PG development is first reported after scald burn. These lesions were successfully treated by primary closure and FTSG.
References
- 1.Netscher D, Spira M, Cohen V. Nonhemangiomatous vascular lesions. In: Achauer BM, editor. Plastic Surgery Indications, Operations and Outcomes. 1 edition. Missouri: Mosby; 2000. p. 310. [Google Scholar]
- 2.Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267–276. doi: 10.1111/j.1525-1470.1991.tb00931.x. [DOI] [PubMed] [Google Scholar]
- 3.Ceyhan AM, Basak PY, Akkaya VB, Yildirim M, Kapucuoglu N. A case of multiple, eruptive pyogenic granuloma developed on a region of the burned skin: can erythromycin be a treatment option? J Burn Care Res. 2007;28:754–757. doi: 10.1097/BCR.0B013E318148CB3F. [DOI] [PubMed] [Google Scholar]
- 4.Bozkurt M, Kulahci Y, Zor F, Askar I. Multiple giant disseminated pyogenic granuloma in a burn lesion. J Burn Care Res. 2006;27:247–249. doi: 10.1097/01.BCR.0000202642.08806.B7. [DOI] [PubMed] [Google Scholar]
- 5.Aliagaoglu C, Bakan V, Atasoy M, Toker S. Pyogenic granuloma with multiple and satellite involvement after a burn in a 5-year-old child. J Dermatol. 2006;33:150–152. doi: 10.1111/j.1346-8138.2006.00033.x. [DOI] [PubMed] [Google Scholar]
- 6.Ceyhan M, Erdem G, Kotiloglu E, Kale G, Talim B, Kanra G, Basaran I. Pyogenic granuloma with multiple dissemination in a burn lesion. Pediatr Dermatol. 1997;14:213–215. doi: 10.1111/j.1525-1470.1997.tb00240.x. [DOI] [PubMed] [Google Scholar]
- 7.Momeni AZ, Enshaieh S, Sodifi M, Aminjawaheri M. Multiple giant disseminated pyogenic granuloma in three patients burned by boiling milk. Int J Dermatol. 1995;34:707–710. doi: 10.1111/j.1365-4362.1995.tb04658.x. [DOI] [PubMed] [Google Scholar]
- 8.de Kaminsky AR, Otero AC, Kaminsky CA, Shaw M, Formentini E, Abulafia Multiple disseminated pyogenic granuloma. Br J Dermatol. 1978;98:461–464. doi: 10.1111/j.1365-2133.1978.tb06542.x. [DOI] [PubMed] [Google Scholar]
- 9.Mooney MA, Janniger CK. Pyogenic granuloma. Cutis. 1995;55:133–136. [PubMed] [Google Scholar]
- 10.Pagliai KA, Cohen BA. Pyogenic granuloma in children. Pediatr Dermatol. 2004;21:10–13. doi: 10.1111/j.0736-8046.2004.21102.x. [DOI] [PubMed] [Google Scholar]
- 11.Lin RL, Janniger CK. Pyogenic granuloma. Cutis. 2004;74:229–233. [PubMed] [Google Scholar]
- 12.Zaballos P, Llambrich A, Cuellar F, Puig S, Malvehy J. Dermoscopic findings in pyogenic granuloma. Br J Dermatol. 2006;154:1108–1111. doi: 10.1111/j.1365-2133.2006.07193.x. [DOI] [PubMed] [Google Scholar]
- 13.Giblin AV, Clover AJ, Athanassopoulos A, Budny PG. Pyogenic granuloma - the quest for optimum treatment: audit of treatment of 408 cases. J Plast Reconstr Aesthet Surg. 2007;60:1030–1035. doi: 10.1016/j.bjps.2006.10.018. [DOI] [PubMed] [Google Scholar]


