Abstract
Aim: To determine the types of functional disabilities in adult and paediatric burns survivors, with specific emphasis on potential risk and socio-economic factors of burn disabilities present in Ghana. Patients and Methods: The descriptive study was carried out in Komfo Anokye Teaching Hospital, Kumasi, Ghana from May 2011 to April 2012. Burn survivors who came for follow-up visits after been discharged home and had functional disability were the participants of the study. They were physically examined and interviewed using a pre-tested questionnaire after their informed consent/or that of their parents (in the cases of paediatrics burns survivors) was sought. Results: A total of 70 participants consented for the study. Their ages ranged from 8/12 – 78 years, with a mean age of 12±1.7 years. Majority (60.0%, N=42) of the participants had third degree burns. The nature of disabilities of participants were mostly scar contractures (42.9%, N=30) of which 36.7% (N=11) had impeded arm elevation; 23.3% (N=7) could not fold the palm or move the digits. From the multiple regression analysis risk factors for burn victim to have disability were paediatric age (OR=11.1, P=0.043), third degree of burn (OR=6.2, P=0.001) and anatomical part affected (OR=18.3, P=0.031). Socio-economic factors that affected burn disability victims were nuclear family compensation (OR=4.2, P=0.021), community mockery/stigmatization (OR=0.1, P=0.052) and caretakers time and finance (OR=5.2, P=0.033). Conclusion: The commonest functional disabilities recorded were scar contractions of the axilla region which had impeded the ability of the patients to lift the arm. Risk factors for burns disability included childhood age, third degree of burn incurred and anatomical part affected. Social factors influencing the lives of burn survivors with disability were good family and negative community interactions. Significant economical factors recorded were caretakers’ time and financial constrains.
Keywords: Functional disability, burns survivors, risk factors, social burden, economic burden
Introduction
Globally, the incidence of burns severe enough to require medical attention was nearly 11 million people and ranked fourth in all injuries, higher than the combined incidence of tuberculosis and HIV infections [1]. Fortunately, although burns and fires account for over 300,000 deaths each year throughout the world, the vast majority of burns are not fatal. Nonetheless, fire-related burns are also among the leading causes of disability-adjusted life years lost in low-and middle-income countries (LMIC) [1]. The World Health Organization (WHO) figures state that 833,773 African children, under the age of five, suffered fire related injuries or deaths in the year 2000. Fire related mortality rates in Africa (6.1 per 100 000 population) are much more common when compared to those seen in high-income countries (just 1.0 deaths per 100 000 population) [2].
Morbidity and mortality due to fire and flames have declined worldwide in the past decades. However, 90% of burn deaths occur in LMIC, where prevention programs are uncommon and the quality of acute care is inconsistent [1,3]. Even in high-income countries, burns occur disproportionately to racial and ethnic minorities such that socioeconomic status, more than cultural or educational factors, account for most of the increased burn susceptibility. Risk factors for burns include those related to socioeconomic status, race and ethnicity, age, and gender, as well as those factors pertaining to region of residence, intent of injury and co-morbidity [1].
Although burns remain a common public health problem among Ghanaians, very little is known about burn-related functional disabilities [4]. Burns are a major cause of death and disability and are associated with significant national healthcare resource utilization. Burns often require long periods of rehabilitation, multiple skin grafts, and extensive physical therapy. Not only can burn-related injuries leave patients with lifelong physical disabilities but burns can also result in severe psychological and emotional distress due to scarring, which often also result in significant burdens for the patients’ families and caregivers [1,4]. Burns are associated with relatively high mortality and morbidity worldwide, especially in the developing countries [5,6]. There are approximately 1500 burns cases in Ghana annually and a sizeable fraction of these burns occur in large scale disasters caused by petrol-related fires [4,7-11]. Burns are among the top 10 external causes of death in South Africa, and in 2004 burns violence was the leading cause of unnatural death in children aged 1-4 years [8].
Third degree burns cause deeper injuries to the skin and can lead to scarring and functional limitations. Fourth degree burns result in injuries to muscles and bone and can lead to scarring, functional limitations and amputations [2]. The commonest causes of severe burns are open fire. Scaring can be a significant issue in recovery from burns. Prominent scars are classified as either hypertrophic scars or keloids. Also, severe burns may result in respiratory damage, muscle damage or amputations [8]. With advances in medical and surgical care, increasing numbers of patients are surviving severe burn injuries generally [12-15]. According to the study of Esselman et al., severe burns and other critical illnesses, as well as their requisite therapies expose patients to extreme physiological and psychological stressors [14]. Therefore, functional limitations are potential concerns in these patients. In this article, an overview of the burn cases and functional disabilities in adult and paediatric burns survivors, with specific emphasis on potential risk factors and socio-economic effects of burn disabilities present in Kumasi, Ghana will be provided.
Materials and methods
Study setting
The Komfo Anokye Teaching Hospital (KATH) in Kumasi is the second-largest hospital in Ghana and the only tertiary health institution in the middle belt of the country. It is the main referral hospital for the Ashanti, Brong Ahafo, the Northern, Upper West and Upper East regions of the country. The hospital was built in 1954 as the Kumasi Central Hospital, latter renamed Komfo Anokye Hospital and was converted into a teaching hospital in 1975, affiliated to the School of Medical Sciences (SMS) of the Kwame Nkrumah University of Science and Technology (KNUST). The hospital currently has 1000 beds, with an annual hospital attendance of about 679,050 patients made up of both out- and in-patients (KATH Biostatistics Unit, 2012).
The KATH Accident and Emergency (A&E) Centre, established in 2009, houses the Reconstructive Plastic Surgery & Burns Unit, among other units, is made up of a total of 160 ventilated bed capacity. These units are well equipped with all necessary tools to attend to any A&E case Severe burn injury patients are initially attended to by the Emergency Physician team-on-duty before been referred to the Plastic Surgery team-on-duty. The surgeon or his resident/registrar gets to the patient within the shortest possible time and makes the decision to admit the patient to a specific burns ward for management.
Data collection
The information for the study was obtained from burn survivors who came for follow-up visits after been discharged home from May 2011 to April 2012, had functional disability and consented for the study. They were physically examined and interviewed for the study after their informed consent/or that of their parents (in the cases of paediatrics burns survivors) was sought. The questionnaire used in the study was designed, pre-tested and necessary adjustments made by the investigator before been utilized in the study. The questionnaire had four sections to enable the investigator to assess changes the disability had brought in their lives. The sections were:
A) Demographic features which include: age, sex, occupation, aetiology of burns, degree of burn incurred and the Total Burn Surface Area (TBSA).
B) Status of disability which includes: the nature of disability, anatomic position affected, the time lag between occurrence and disability/disfigurement.
C) The social burden caused by the disability, which includes the effect of disability on their social interaction and social belief.
D) The economic burden caused by the disability, also includes compensation for injury, social security, dependence on other people for survival.
Ethical clearance
Ethical approval for the study was obtained from the Committee on Human Research, Publications and Ethics of the School of Medical Sciences, Kwame Nkrumah University of Science and Technology and Komfo Anokye Teaching Hospital.
Data analysis
This information was displayed in tables and graphs and analyzed with SPSS version 18.0 (SPSS, Inc., Chicago, IL, USA).
Results
Demographic characteristics of participants
A total of 70 participants, out of a total of 82 patients, consented for the study and their ages ranged from 8/12–78 years, with a mean age of 12±1.7 years Figure 1). Females (52.9%, N=37) outnumbered males (47.1%, N=33). In terms of occupation, most (70.0%, N=49) of the participants were unemployed – i.e. babies, pupils, students, adult unemployed, the old aged; while, Businessmen/Traders (11.4%, N=8), Artisans (7.1%, N=5), Farmers (4.4%, N=3) and Others (7.1%, N=5) – Tutors, Auditor, Cooks- were the employed participants. Few (19.0%, N=4) of these pre-burn workers were ready to return to their work.
Figure 1.
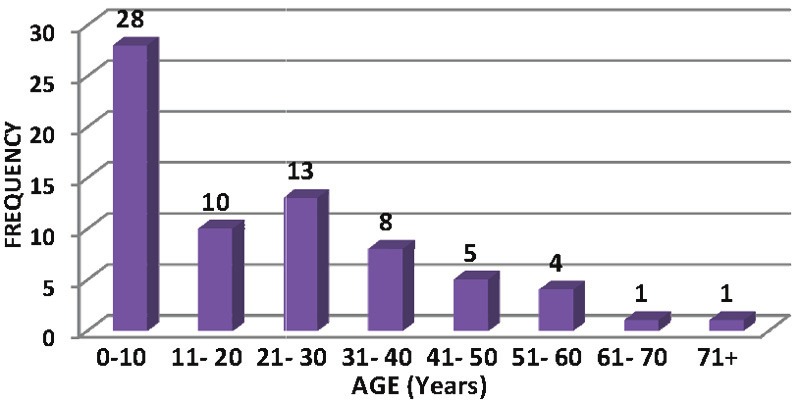
Age distribution of participants.
The TBSA incurred by participants ranged from 9% - 76%, with an interquartile range of 25%. In terms of degree of burns, majority (60.0%, N=42) of the participant had third degree burns (Table 1).
Table 1.
Total Burn Surface Area (TBSA) and Burns Degree
| TBSA (%) | Frequency (N) | No. of patients with degree of burn | ||
|---|---|---|---|---|
|
| ||||
| Second | Third | Fourth | ||
| 1-10 | 3 | 0 | 3 | 0 |
| 11-20 | 9 | 2 | 6 | 1 |
| 21-30 | 19 | 5 | 12 | 2 |
| 31-40 | 11 | 6 | 5 | 0 |
| 41-50 | 22 | 8 | 13 | 1 |
| 51-60 | 2 | 0 | 2 | 0 |
| 61-70 | 3 | 3 | 0 | 0 |
| 71-80 | 1 | 0 | 1 | 0 |
| 81+ | 0 | 0 | 0 | 0 |
| Total | 70 | 24 | 42 | 4 |
Flame was the highest (N=34) aetiology of burns recorded, followed by scald (N=27) (Figure 2).
Figure 2.
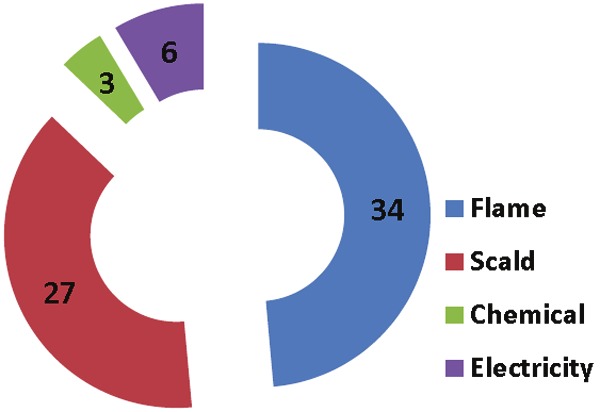
Aetiology of burns recorded in the study.
Status of disabilities of participants
The nature of disabilities of participants were mostly scar contractures (42.9%, N=30) of which 36.7% (N=11) had impeded arm elevation, 23.3% (N=7) cannot fold the palm or move the digits, disfigurements (35.7%, N=25) – mostly the face, head and neck, trunk- and both (21.4%, N=15); few (7.1%, N=5) of the disabilities were permanent i.e. nothing could be done in KATH to replace/correct it and these were mostly amputations (Tables 2 and 3), whilst the majority were all temporal. Almost all (91.4%, N=64) the participants/or their parents in the case of paediatric burn survivors- admitted having psychological and emotional distress after recovery from the burns calamity; i.e. shyness to expose the deformed parts of the body; fear for been mocked or rejected by friends/colleagues at school or workplace; itching and painful sensation of the keloidal body parts.
Table 2.
Types of scar contracture incurred by participants
| Type of disabilities | Frequency (N) | Impairment |
|---|---|---|
| Scar Contracture | ||
| Axillary | 11 | Impeded elevation of arm |
| Palm & digits | 7 | Inability to fold palm and digits |
| Wrist | 1 | Rigid wrist |
| Elbow joint | 2 | Inability to flex the elbow |
| Neck | 1 | Rigid neck |
| Knee joint | 3 | Inability to bend the knee |
| Foot & toes | 5 | Inability to move the foot and toes |
| Total | 30 |
Table 3.
Types of disfigurement incurred by participants
| Type of Disabilities | Frequency (N) |
|---|---|
| Disfigurement | |
| Amputation | 3 |
| Keloid | 11 |
| Hyper/Hypo-pigmentation | 8 |
| Loss of auricle | 1 |
| Loss of breast | 1 |
| Loss of nose | 1 |
| Total | 25 |
In terms of parts of the body of participants which were functionally disabled, those with only a part affected were the majority (62.9%,N=44), those with ‘three and more’ parts disabled were the next majority (20.0%, N=14) and those with two body parts affected were the least (17.1%, N=11) recorded (Figures 3, 4, 5, 6, and 7). The time lag between occurrence and state of disability ranged from 1 - 105 weeks, with an interquartile range of 16.4 weeks.
Figure 3.

A. A participant with a temporal right axillary disability and anterior trunk depigmentation; B. Post release of contracture.
Figure 4.

A participant with disfigurement and amputation.
Figure 5.

A participant with amputation.
Figure 6.

A participant with hypertrophic scars.
Figure 7.

A participant with multiple disabilities/disfigurements.
Social burden caused by the disability
The effect of disability on their social interaction was assessed in terms of the nuclear family, relatives and the community (work/school/residential areas). Almost all (N=66) the participants/or parents for pediatric burn survivors- claimed the nuclear family was sad and had compassion for them. Few (N=4) admitted their nuclear family feared for their (participants’) current situation. Most (87.1%, N=61) of the participants claimed their relatives had compassion for them; 10.0% (N=7) of the participants claimed their relatives mocked them and 2.9% (N=2) of them reported to have been excluded in all external family activities by their relatives.
The community assessment also reveals that, majority (80.0%, N=56) of the participants admitted their community had compassion for them. However, 15.7% (N=11) reported to have been mocked by their community, and 4.3% (N=3) of them claimed to have been stigmatized.
With the issues of social belief, few (8.6%, N=6) participants claimed their situation had effects on their religion.
Economic burden caused by disability
In terms of economic burden caused by the disability, minority (N=7) of the participants claimed to have received a form of compensation for injury from co-tenants and/or their church. Also only 12.9% (N=9) of them had social security. The most common effect on caretakers/parent’s work was time constraints (51.4%, N=36) - i.e. their personal activities had been affected, since they had to take their spouse or child to KATH for wound dressing and also be with them at home to support them hence they did not have personal time on their own, followed by financial constraints (41.4%, N=29) – i.e. the work of the caretakers had been negatively affected, since they could not trade, farm or go to work as usual, hence recorded negative productivity of caretakers and others (7.2%, N=5) – included; affected proposed business travels, business meetings, etc.
Potential factors that influenced burns survivors with disability
Multiple regression analysis was used to determine factors associated with burns disability. Using the type of participants’ disability as the dependent factors the following variables were involved in the analysis: demographic features (age, sex, occupation, TBSA, degree of burn, aetiology) and status of the disability (anatomi cal parts, time lag) as shown in Table 4.
Table 4.
Risk factors that influence the development of disability in burn survivals
| Factor | Odd Ratio | 95% CI | P-value |
|---|---|---|---|
| Demographic feature | |||
| Age (0-10) | 11.1 | 0.79-156.5 | 0.043 |
| Sex | 0.2 | 0.36-8.3 | 1.564* |
| Occupation | 1.4 | 4.16-168.3 | 0.546 |
| TBSA | 2.8 | 0.52-13.2 | 0.059 |
| Degree of burn (third) | 6.2 | 0.29-73.7 | 0.001* |
| Aetiology | 0.4 | 0.51-13.6 | 2.310 |
| Status of disability | |||
| Anatomical parts (Axillary/Head/Neck) | 18.3 | 0.97-135.2 | 0.031* |
| Time lag | 0.6 | 0.81-35.4 | 2.013 |
Donates significant value (P< 0.05).
Also, with a similar dependent, another regression analysis was performed to determine socio-economic factors that affected the participants (Table 5). A probability value (P-value) of less than 0.05 was considered to be statistically significant at 95% confidence interval.
Table 5.
Socio-economic factors that affect burn survivals
| Factor | Odd Ratio | 95% CI | P-value |
|---|---|---|---|
| Social burden | |||
| Interaction | |||
| Nuclear Family (compensation) | 4.2 | 0.55-10.2 | 0.021* |
| Relatives | 0.3 | 0.29-8.12 | 0.096 |
| Community (mockery/Stigmatization) | 0.1 | 0.32-7.8 | 0.052* |
| Belief | 0.5 | 0.12-14.0 | 3.014 |
| Economic burden | |||
| Compensation | 0.4 | 0.51-25.3 | 0.069 |
| Social Security | 0.2 | 0.99-32.1 | 6.012 |
| Caretakers (Time & finance) | 5.2 | 0.85-54.6 | 0.033* |
Donates significant value (P< 0.05).
Discussion
Other studies from many geographic areas have noted the prevalence of disfigurement (keloids) from burns in children and adults as ranging from 4% to 9% [3,16-19]. In the study of Fordjuoh et al. with Ghanaian children as participants for World Health Organization (WHO), a 17.4% prevalence of burn-related functional disabilities, mostly keloids, was recorded [8]. In this study however, keloids and axillary scar contractures had the same prevalence of 15.7%. The supportive argument of burn-related keloids been the commonest category of disfigurement had also been proved by the study. The higher rate of keloid formation from burn scars in this region may be genetic. Moreover, burns-related functional disabilities such as axillary scar contractures as the findings of the study reveals should be also looked at, since with prompt care in the management of axillary scar contractures prevention of the condition could have been possible. This fact had been also emphasized in the contracture study of Adu in KATH; the author reported that good positioning of the burned patient, especially for major and deeper burns of the hands, head and neck is an effective way to prevent contractures [20]. Splinting is used if the patient is not able to voluntarily maintain proper positions. Passive movements of the joints are done when patients cannot co-operate; as soon as they can co-operate active exercises are encouraged. Early excision and skin grafting of deeper wounds, or skin grafting of any burn wound of more than 3 weeks duration effectively reduces the chances of development of contractures [20-22].
In studies of burn survivors, many risk factors associated with functional disabilities had been reported. These include: female gender, pre-burn affective [23], anxiety disorders, burn injury characteristics (e.g., TBSA burned, location of burn) [14,24], personality characteristics, and coping styles have been found to be fairly consistent predictors of subsequent depressive symptoms [24,25]. Again, in the pediatric burn survivors’ study of Dimitry et al., it was reported that increased burn size and female gender were associated with functional disabilities [12]. In a study in Ghana, the findings of Fordjuoh et al. revealed that burn-related functional disabilities were greatest for burns that required more than 30 days to heal (OR=5.80, 95% CI=3.07, 10.99), while burns to anatomical parts such as the head/neck region involved a fourfold increased risk (OR=3.44, 95% CI=1.71, 6.93). The odds ratios for days required for healing and depth of burn (OR=3.04, 95% CI=1.12, 8.22) increased significantly. Relative to children newborn to 11 months of age, the odds of developing functional disabilities decreased for children 12 to 35 months old and then increased steadily with age, peaking in those 48 to 59 months old [8]. In the present study, the findings demonstrated that age (0-10 years), degree of burn and anatomical parts (axillary/head/neck) were found to be potential risk factors associated with functional disabilities; the other demographic features were irrelevant in this study as opposed to that of the others [23-25] (Table 4). The childhood age as a risk factor in burn-related disabilities in the study is in line with that of Fordjuoh et al. and others [8]. Therefore, in addition to educating families about augmenting the level of supervision of children, especially in the kitchen where most burns occur, serious efforts at identifying other burn-causing environmental factors in future studies may be important. The establishment of community programmes is one way of ensuring adequate child supervision and general child wellbeing, particularly for children in fire prone areas. Another important risk factor identified in this study was degree of burn survivors. Although, Dimitry et al [12], Esselman et al [14] and others [23,24] identified TBSA burned as a risk factor in their studies, the present study found no significant relationship between TBSA burned and disability, even though a positive odd ratio of 2.8 for TBSA was obtained in the study. Thus, this study buttresses the findings of Fordjuoh et al. which identified an increase significant between degree of burn and disability [8]. The discrepancy may be associated to the difference in the study sites: the formers were in developed countries while, the latter was Ghanaian based; hence TBSA may play an essential factor in the determination of burn-related disabilities in developed countries, degree of burn should be taken into much consideration in the prevention of burn-related disabilities in countries such as Ghana. Again, anatomical parts affected by burns were an identified risk factor in the study. Similarly, studies such as that of Saxe et al. [23] and Fordjuoh et al. [8] reported anatomical parts affected by burns as a significant factor to consider when burn disability is concern. This reported risk factor is vital in both developed and developing countries and to alleviate disabilities such as scar contractures immediate and proper burn injury management procedures as elaborated in the study of Adu should be welcomed [20].
Socio-economically, adult burn injury survivors with functional disabilities have been found to have impairments in productivity and return to work [14,26,27]. This phenomenon was also identified in the study where, 81.0% of the pre-burn workers among the participants did not have the courage to return to their workplace due to the disability. Also, adult burn injury survivors with functional disabilities have diminished health-related quality of life (HRQOL) [14,27]. Dimitry et al., reported that lack of return to work post-burn has been found to be associated with pre-burn psychiatric history, pre-burn unemployment, burn severity and burn to a limb [12]. Moreover, body image dissatisfaction, longer hospital admission and amputation predicted diminished HRQOL in burn survivors [14]. Although in this study no association was found relating to shyness, fear and body image dissatisfaction, the findings of the study revealed that majority of the participants had these emotional and psychological distresses. Studies of pediatric burn injury survivors by Dimitry et al. [12] and Dyster-Aas et al. have found that children may experience fewer positive emotions, as well as have increased social withdrawal and somatic complaints [27]. Dimitry et al. in a study of pediatric burn survivors found that TBSA burned and the number of days since hospital discharge was associated with behavioral and social difficulties [12]. Moreover, nuclear family and community social burden in terms of interaction was found to be affected by the functional disability of the participants. The nuclear family (OR=4.2) and community odd ratio (OR=0.1) indicated a positive and negative effects on the participants respectively (Table 5). In this study the social difficulties mentioned in the study of Dimitry et al., may be attributed to mockery and stigmatization posed by the community on the burn survivors with functional disabilities [12]. Also, financial and time constraints were the economic factors that had effect on caretakers of burn survivors with functional disabilities (Table 5). Notwithstanding the fact that few participants claimed to have received some form of compensation, it was not a major effect on the participants in the study as compared to the effect on finance and time of caretakers of the participants.
Conclusion
The commonest functional disabilities recorded were scar contractures (mostly axillary contractures), disfigurements (mostly keloids) and both. Risk factors identified to be associated with burns disability were childhood age, third degree of burn incurred and anatomical part affected. Social factors influencing the lives of burn survivors with disability were family compensation and negative community interactions. Also, significant economic factors identified in the study were caretakers’ time and financial constraints.
Prevention of contractures through proper management and care for burn victims should be emphasized in our health institutions. Public education on the danger and etiology of burns should be encouraged, especially among females and mothers since most of the participants were children. Policies to incorporate burn related education into Ghanaians educational curriculum should be welcomed so as to have direct impact on children of school-going age.
Social welfare and human rights organisations in Ghana should implement policies that will make sure the right of burns survivors with disabilities should not be infringed. The country should have policies where personal insurance of individuals at all ages are made compulsory to enable burns victims and/or their caretakers acquire a form financial compensation.
Acknowledgments
The author sincerely thanks Miss Elizabeth Anthony, a research assistant, who actively collected the data for this study; also sincerely thanking Dr. Paul Saunderson for his valuable suggestions on the manuscript.
Conflict of interest statement
The author has declared no conflict of interest.
References
- 1.Peck MD. Epidemiology of burns throughout the world Part I: Distribution and risk factors. Burns. 2011;37:1087–100. doi: 10.1016/j.burns.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 2.BURNS. Handbook of Disability. Curators of the University of Missouri & RCEP7. 2001 http://www.dps.missouri.edu/resources/Handbook/burns.pdf. [Google Scholar]
- 3.WHO plan for burn care prevention. 2008 http://whqlibdoc.who.int/publications/2008/9789241596299_eng.pdf. [Google Scholar]
- 4.Agbenorku P, Akpaloo J, Farhat BF, Hoyte-Williams PE, Yorke J, Agbenorku M, Yore M, Neumann M. Burn disasters in the middle belt of Ghana from 2007 to 2008 and their consequences. Burns. 2010;36:1309–1315. doi: 10.1016/j.burns.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 5.Lau YS. An insight into burns in a developing country: A Sri Lankan experience. Public Health. 2006;6:958–65. doi: 10.1016/j.puhe.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 6.Kalayi GD. Mortality from burns in Zaria: An experience in a developing economy. East Afr Med J. 2006;83:461–4. doi: 10.4314/eamj.v83i8.9459. [DOI] [PubMed] [Google Scholar]
- 7.Forjuoh SN. Injury control in the developing nations: What can we learn from industrialized countries? Inj Prev. 1996;2:90–1. doi: 10.1136/ip.2.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fordjuoh SN. Burns in low- and middle-income countries: A review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32:529–37. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Ahuja RB, Bhattacharya S. Burns in the developing world and burn disasters. BMJ. 2004;329:447–9. doi: 10.1136/bmj.329.7463.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agbenorku P, Akpaloo J, Yalley D, Appiah A. A New Era in the Management of Burns Trauma in Kumasi, Ghana. Ann Burns Fire Disasters. 2010;30:59–66. [PMC free article] [PubMed] [Google Scholar]
- 11.Agbenorku P. Kumasi: First Ghana Burn Conference 2008/Launch of Ghana Burn Association. Theme: Prevention and management of burns in Ghana - Are we doing it right? Accra, Ghana: Ghana College of Physicians and Surgeons; 2008. Morbidity and mortality data. [Google Scholar]
- 12.Dimitry SD, Wayne JK, Douglas FZ. Psychiatric Morbidity and Functional Impairments in Survivors of Burns, Traumatic Injuries, and ICU Stays for Other Critical Illnesses: A Review of the Literature. Int Rev Psychiatry. 2009;21:531–538. doi: 10.3109/09540260903343877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Angus DC, Carlet J. Surviving intensive care: a report from the 2002 Brussels Roundtable. Intensive Care Med. 2003;29:368–377. doi: 10.1007/s00134-002-1624-8. [DOI] [PubMed] [Google Scholar]
- 14.Esselman PC, Thomas BD, Magyar-Russell G, Fauerbach JA. Burn rehabilitation: state of the science. Am J Phys Med Rehabil. 2006;85:383–413. doi: 10.1097/01.phm.0000202095.51037.a3. [DOI] [PubMed] [Google Scholar]
- 15.Ornato JP, Craren EJ, Nelson NM, Kimball KF. Impact of improved emergency medical services and emergency trauma care on the reduction in mortality from trauma. J Trauma. 1985;25:575–577. doi: 10.1097/00005373-198507000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Leung PC. Pressure treatment for hypertrophic scars. Burns. 1980;6:244–246. [Google Scholar]
- 17.Laditan AA. Accidental scalds and burns in infancy and adulthood. J Trop Pediatr. 1987;33:199–202. doi: 10.1093/tropej/33.4.199. [DOI] [PubMed] [Google Scholar]
- 18.Onuba O, Udoidiok E. The problems and prevention of burns in developing countries. Burns. 1987;13:382–385. doi: 10.1016/0305-4179(87)90128-8. [DOI] [PubMed] [Google Scholar]
- 19.Datubo-Brown DD, Kejeh BM. Burn injuries in Port Harcourt, Nigeria. Burns. 1989;15:152–154. doi: 10.1016/0305-4179(89)90170-8. [DOI] [PubMed] [Google Scholar]
- 20.Adu EJ. Management of Contractures: A Five-Year Experience at Komfo Anokye Teaching Hospital in Kumasi. Ghana Med J. 2011;45:66–72. doi: 10.4314/gmj.v45i2.68931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fanstone R. Physiotherapy and Burn Injuries. Repair Reconstr. 2000;1:17–19. [Google Scholar]
- 22.Olabanji JK, Oladele AO, Ame OO, editors. Challenges of Post-burn Contractures in Ile-Ife; Proceedings from West African College of Surgeons 50th Annual Conference; Nigeria, Calabar: 2010. p. 11. [Google Scholar]
- 23.Saxe GN, Stoddard F, Hall E, Chawla N, Lopez C, Sheridan R, King D, King L, Yehuda R. Pathways to PTSD, part I: children with burns. Am J Psychiatry. 2005;162:1299–1304. doi: 10.1176/appi.ajp.162.7.1299. [DOI] [PubMed] [Google Scholar]
- 24.Thombs BD, Bresnick MG, Magyar-Russell G. Depression in survivors of burn injury: a systematic review. Gen Hosp Psychiatry. 2006;28:494–502. doi: 10.1016/j.genhosppsych.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 25.Dyster-Aas J, Willebrand M, Wikehult B, Gerdin B, Ekselius L. Major depression and posttraumatic stress disorder symptoms following severe burn injury in relation to lifetime psychiatric morbidity. J Trauma. 2008;64:1349–1356. doi: 10.1097/TA.0b013e318047e005. [DOI] [PubMed] [Google Scholar]
- 26.Esselman PC, Ptacek JT, Kowalske K, Cromes GF, deLatuer BJ, Engrav LH. Community integration after burn injuries. J Burn Care Rehabil. 2001;22:221–227. doi: 10.1097/00004630-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Dyster-Aas J, Kildal M, Willebrand M. Return to work and health-related quality of life after burn injury. J Rehabil Med. 2007;39:49–55. doi: 10.2340/16501977-0005. [DOI] [PubMed] [Google Scholar]


