Abstract
Preterm birth may be affected by the interaction of residential air pollution with neighborhood economic hardship. The authors examined variations in traffic-related pollution exposure—measured by distance-weighted traffic density—using a framework reflecting the social and physical environments. An adverse social environment was conceptualized as low socioeconomic status (SES) neighborhoods—census tracts with concentrated poverty, unemployment, and dependence on public assistance. An adverse physical environment was depicted by the winter season, when thermal inversions trap motor vehicle pollutants, thereby increasing traffic-related air pollution. Los Angeles County, California, birth records from 1994 to 1996 were linked to traffic counts, census data, and ambient air pollution measures. The authors fit multivariate logistic models of preterm birth, stratified by neighborhood SES and third pregnancy trimester season. Traffic-related air pollution exposure disproportionately affected low SES neighborhoods in the winter. Further, in these poorer neighborhoods, the winter season evidenced increased susceptibility among women with known risk factors. Health insurance was most beneficial to women residing in neighborhoods exposed to economic hardship and an adverse physical environment. Reducing preterm births warrants a concerted effort of social, economic, and environmental policies, focused on not only individual risk factors but also the reduction of localized air pollution, expansion of health-care coverage, and improvement of neighborhood resources.
Keywords: air pollution, premature birth, socioeconomic factors
In the United States, nearly 440,000 babies are born prematurely each year, levying a considerable cost burden to the health care system and emotional and financial strain to the families affected. Preterm birth is the second leading cause of infant death and a major contributor to early childhood morbidity. Over the last two decades, the rate of preterm births increased from 9.4 percent to nearly 12 percent (1, 2), prompting several national and community initiatives to address preterm births as the top obstetric problem in the United States today. Although the exact causes of preterm birth are still unknown, many studies have identified vulnerable groups according to sociodemographic characteristics: infants of African-American mothers, younger or older mothers, and mothers with lower levels of educational attainment (3-7).
Researchers have begun to study the individual’s neighborhood in addition to individual-level characteristics associated with preterm birth. While individual-level attributes are immutable or difficult to change, policies and interventions at the community level can influence neighborhood conditions associated with adverse health effects. Moreover, even if individual-level attributes are modifiable, such as earlier initiation of prenatal care and access to health insurance, this change has not resulted in considerable improvements in preterm birth rates over the past years (8). There is mounting evidence that, in addition to individual-level factors, the residential area or neighborhood may confer additional risks or provide benefits that affect birth outcomes (9-16). However, most of these studies have focused on only the social, political, and economic conditions in a neighborhood, absent of measures depicting the physical environment that may exacerbate biologic and psychosocial stressors associated with preterm birth.
The call for a comprehensive examination of the physical and social environment was recently articulated by O’Neill et al. (17). They hypothesized that low socioeconomic status (SES) neighborhoods and communities may not only experience increased levels of air pollution but also have more vulnerable inhabitants who are more susceptible to these exposure effects because of compromised health status and a lack of resources, including adequate health care. Yet to date few studies have explicitly explored the interplay of individual characteristics and pollution exposure within neighborhoods with varying neighborhood socioeconomic resources.
In this spatial variation study, we examined preterm birth risk within a framework reflecting both the social and physical environments. We built on previous studies that have linked traffic-related pollution exposure—measured by distance-weighted traffic density (DWTD)—to preterm birth risk (18, 19). “Space” was defined by the degree of neighborhood economic hardship (the social environment) and by distinct meteorologic seasonal conditions in Los Angeles that correlate strongly with traffic-related air pollution (the physical environment). We conceptualized an “adverse” social environment as neighborhoods with concentrated poverty, unemployment, and dependence on income from public assistance, whereas an adverse physical environment manifests as wintertime thermal inversions that trap motor vehicle pollutants. We explored whether and to what extent these adverse conditions in the social and physical environments might increase the susceptibility for preterm delivery among vulnerable women or potentially modify the effectiveness of protective factors such as health insurance.
MATERIALS AND METHODS
Data sources
We linked Los Angeles County, California, birth records to 1990 US Census summary tape file 3 data, traffic count information from the California Department of Transportation, and ambient air pollution data from the South Coast Air Quality Management District. Our sample was drawn from a population of births during 1994–1996 to mothers residing in 112 of the 269 total Los Angeles County ZIP codes. These 112 ZIP codes met the selection criteria of being situated in areas within a 3.2-km radius intersected by freeways and major arterials and with collectors or monitoring stations. From this source population, we identified all preterm infants (n = 25,974), and for each ZIP code and birth year, we selected an approximately equal number of controls from among normal weight, full-term infants, yielding a total of 59,700 eligible study subjects. We excluded 8,767 infants who had missing or unlinkable addresses, infants weighing less than 500 g, infants weighing greater than 5,000 g, and/or births with unreliable values for gestational age (<90 days and >320 days). Of the remaining 50,933 subjects, we then sequentially excluded 2,801 multiple births (both cesarean section and normal deliveries) and 10,699 singleton deliveries by cesarean section. Electively scheduled cesarean sections are unlikely to be related to exposures that occur prior to birth, such as air pollution, while emergency cesarean sections very well may be. Elective cesarean sections are also endogenous with preterm birth risk. Since we could not distinguish the reasons behind cesarean sections in our data, they were excluded from our analysis. Finally, 86 subjects with missing covariate values were excluded. A total of 37,347 eligible subjects remained for analysis.
Birth outcome
Preterm birth was a dichotomous outcome, specified as infants delivered at less than 37 completed weeks of gestation compared with all term infants.
Economic hardship stratifications
Economic hardship measures, such as poverty and unemployment rates, have been shown to be “implicated” in adverse birth outcomes. As a barometer of neighborhood disadvantage, economic hardship reflects poor levels of social resources that may be connected with the sequence of events that culminate in an adverse birth outcome (11, 20). We therefore selected three federally defined “economic hardship” measures (unemployment, income from public assistance, and family poverty) to depict neighborhood SES (21, 22).
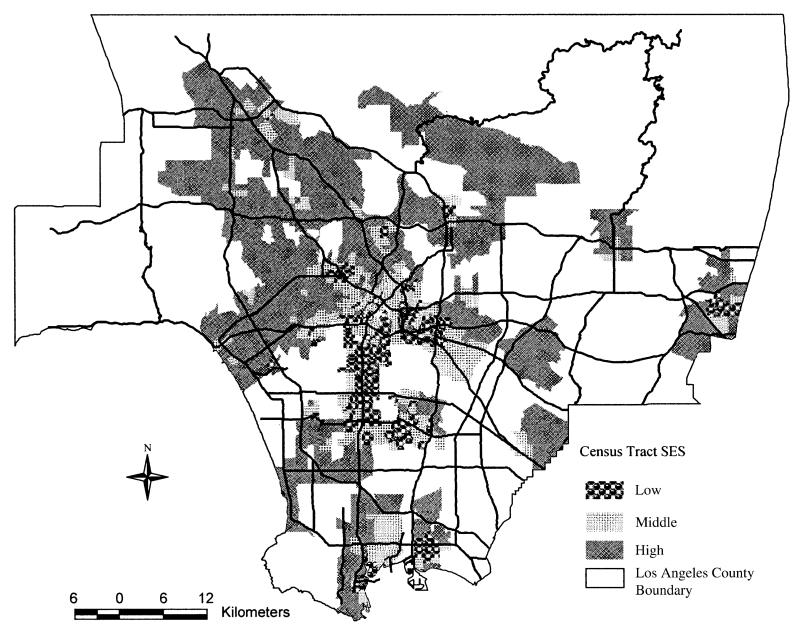
Neighborhoods were defined as census tracts (n = 863), a designation that captures homogeneous economic and demographic characteristics (12, 13). For each census tract, we computed the percentages of unemployed persons in the civilian labor force, households with public assistance income, and families with income below the poverty line. We stratified the sample into high, middle, and low SES neighborhoods. Low SES neighborhoods were census tracts meeting all three criteria: greater than 10 percent unemployment, greater than 20 percent of families in poverty, and greater than 15 percent of individuals receiving public assistance. High SES neighborhoods were defined as meeting all of the following criteria: census tracts with 10 percent or less of the population unemployed, 20 percent or less of the families living in poverty, and 15 percent or less of the individuals receiving income from public assistance. Cutoff points for the low (high) SES neighborhoods correspond to neighborhoods above (below) the mean levels of each of these economic hardship indicators. The middle SES neighborhoods constituted the remaining census tracts (figure 1).
FIGURE 1.
Study subjects’ residential location, by neighborhood socioeconomic status (SES) and location of freeways and highways, Los Angeles County, California, 1994–1996.
Traffic-related air pollution measure
Traffic is a major source of localized pollution in Los Angeles. Previous studies have suggested that compounds in motor vehicle exhaust adversely affect fetal development (18, 19). In a recent commentary on air pollution and poverty, Lipfert stated that, “to the extent that outdoor air quality may be implicated, the culprits are much more likely to be local primary pollutants …” (23, p. 3). Depending on proximity to traffic sources, residential air pollution exposure in southern California can vary widely, not only between neighborhoods but also within neighborhoods (24). To capture localized variation in pollution exposure within neighborhoods, we focused on traffic density measures. Specifically, we used the DWTD as our traffic-related pollution exposure measure. DWTD is intended to measure localized exposure to traffic exhaust by proximity to the source, that is, exposure to primary motor vehicle emissions before they have dispersed and undergone atmospheric transformations. The method for computing DWTD is described in detail elsewhere (18). Briefly, maternal addresses were geocoded using ArcView geographic information system software (ESRI, Redlands, California), and these data, together with the annual average daily traffic counts, were used to calculate the DWTD based on proximity to roadways. We categorized the DWTD into percentiles on the basis of the distribution in the total population (<20th percentile (referent), 20th–<80th percentile, and ≥80th percentile).
Seasonal effects
We additionally conducted stratified analyses by third trimester season: women whose third trimesters fell during the winter months (November–April) versus women whose third trimesters fell during the summer months (May–October). In Los Angeles County, the “winter” months (November–April) correspond to a fall in temperature, ranging from 54 to 60°F (12.2–15.6°C), and the “summer” months (May–October) correspond to higher average temperatures, ranging from 63 to 73°F (17.2–22.8°C) (25). Higher local concentrations of primary exhaust particles and gases from traffic are expected to occur during the winter because of more stagnant air conditions and temperature inversions that limit the dilution and dispersion of emissions; summertime meteorology allows for more rapid mixing and dispersion of these pollutants. While ozone and secondary particles are more elevated in the summer because of increased sunlight’s fueling photochemical reactions, we and others have not observed an effect of ozone on this outcome. We therefore infer that a more “adverse” localized physical environment occurs in the winter when carbon monoxide and primary particles—pollutants directly emitted from vehicle tailpipes—are accumulating near sources.
Our traffic-related pollution measure of interest, DWTD, could also be confounded by background ambient air pollution. We used air pollution data collected at 11 South Coast Air Quality Management District monitoring stations to determine annual average background concentrations of carbon monoxide, ozone, nitrogen dioxide, and particulate matter with a diameter of less than 10 μm for each subject’s home (based on hourly measurements for gases and 24-hour average measurements taken every sixth day for the specified particulate matter); “background” is defined as pollutant concentrations after dispersion and transport away from sources, including roadways. Annual rather than seasonal averages were computed to represent background pollution levels experienced during the year the baby was born. Annual averages are more likely to reflect longer term true background levels of ambient air pollution over larger areas given exposure misclassification when extrapolating exposures for women living farther than 3.2 km from a station.
All models included covariates that have been previously identified as risk factors for preterm birth, including maternal age (categorized as <20, 20–29, 30–34, ≥35 years), maternal race/ethnicity (African American, White, Hispanic, other races), infant’s sex, previous low birth weight or preterm infant, parity, and interval since previous livebirth. We used maternal education (0–8, 9–11, 12, 13–15, ≥16 years), payment source for delivery (government insurance, private insurance, self-pay/uninsured), and initiation of prenatal care (during first trimester, after first trimester/never) as indicators of individual-level SES and protective factors. We included year-of-birth indicators to account for secular variations in preterm birth rates. Unfortunately, birth certificates from California do not contain data on smoking behavior during pregnancy.
Statistical methods
We fit six separate models to capture the interaction of individual covariates with neighborhood SES and season environments: 1) low SES/summer; 2) low SES/winter; 3) middle SES/summer; 4) middle SES/winter; 5) high SES/summer; and 6) high SES/winter. To examine whether our results were sensitive to residual confounding by unmeasured area-level factors, we fit two-level logistic models with a random intercept for each census tract. We fit these models using both empirical Bayesisan and “semi-Bayesian” procedures (26, 27); for the latter, we chose a range of values for the second-level variance that reflected our prior beliefs about the variability in the random intercepts. Our results were robust to these different specifications (results available from authors); we therefore present the results from our one-level analysis.
RESULTS
Higher proportions of women who were White, were older when giving birth, had at least a high school education, had private health insurance, and received early prenatal care lived in high SES neighborhoods (table 1). Higher neighborhood SES was also associated with more homes being located in residential areas with low traffic-related air pollution.
TABLE 1.
Characteristics of study subjects by neighborhood socioeconomic status and season, Los Angeles County, California, 1994–1996*
| Low SES†,‡ |
Middle SES§ |
High SES¶ |
||||
|---|---|---|---|---|---|---|
| Summer | Winter | Summer | Winter | Summer | Winter | |
| Traffic-related pollution exposure | ||||||
| Distance-weighted traffic density (%) | ||||||
| <20th percentile | 16 | 16 | 21 | 20 | 23 | 23 |
| 20–<80th percentile | 64 | 64 | 60 | 60 | 56 | 57 |
| ≥80th percentile | 20 | 20 | 19 | 20 | 21 | 20 |
| Risk factors | ||||||
| Maternal race/ethnicity (%) | ||||||
| White | 3 | 2 | 4 | 4 | 27 | 28 |
| Hispanic | 83 | 82 | 81 | 80 | 53 | 52 |
| African American | 13 | 14 | 8 | 9 | 7 | 11 |
| Other | 2 | 2 | 7 | 7 | 12 | 12 |
| Maternal age (%) | ||||||
| <20 years | 21 | 20 | 17 | 17 | 11 | 12 |
| 20–29 years | 55 | 55 | 55 | 56 | 49 | 50 |
| 30–34 years | 15 | 16 | 18 | 17 | 25 | 24 |
| ≥35 years | 10 | 9 | 11 | 10 | 15 | 14 |
| Protective factors | ||||||
| Maternal education (%) | ||||||
| <9 years | 35 | 36 | 31 | 31 | 15 | 14 |
| 9–11 years | 33 | 32 | 29 | 29 | 18 | 19 |
| 12 years | 23 | 22 | 25 | 24 | 27 | 27 |
| 13–15 years | 7 | 8 | 10 | 10 | 18 | 19 |
| ≥16 years | 2 | 2 | 5 | 5 | 21 | 20 |
| Payment for delivery (%) | ||||||
| Private insurance | 15 | 16 | 23 | 24 | 49 | 51 |
| Government insurance | 83 | 82 | 74 | 74 | 47 | 45 |
| Self/uninsured | 1 | 1 | 3 | 2 | 4 | 4 |
| Prenatal care (%) | ||||||
| None/after first trimester | 28 | 28 | 26 | 27 | 18 | 20 |
| During first trimester | 71 | 71 | 74 | 72 | 82 | 80 |
| Control variables | ||||||
| Infant’s sex (%) | ||||||
| Male | 51 | 51 | 51 | 51 | 51 | 51 |
| Female | 49 | 49 | 49 | 49 | 49 | 49 |
| Parity (%) | ||||||
| 1st birth | 35 | 35 | 37 | 37 | 44 | 45 |
| 2nd or subsequent birth | 65 | 65 | 63 | 63 | 56 | 55 |
| Time since previous livebirth (%) | ||||||
| ≤12 months | 3 | 3 | 3 | 3 | 2 | 2 |
| >12 months | 96 | 96 | 97 | 97 | 97 | 98 |
| Previous LBW† or preterm infant (%) | ||||||
| 0 | 99 | 99 | 99 | 99 | 99 | 99 |
| ≥1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Year of birth (%) | ||||||
| 1994 | 34 | 35 | 33 | 34 | 32 | 33 |
| 1995 | 35 | 34 | 35 | 35 | 35 | 35 |
| 1996 | 30 | 30 | 32 | 31 | 34 | 32 |
| Live near freeway (%) | 14 | 15 | 13 | 12 | 14 | 13 |
| Background annual average pollutants (mean (SD†)) |
||||||
| Carbon monoxide, ppm | 2.0 (0.4) | 1.8 (0.5) | 1.7 (0.5) | |||
| PM10,† μg/m3 | 4.0 (0.4) | 4.0 (0.4) | 3.9 (0.4) | |||
| Nitrogen dioxide, pphm† | 4.4 (0.4) | 4.1 (0.7) | 3.6 (0.7) | |||
| Ozone, pphm | 1.7 (0.3) | 1.9 (0.4) | 2.3 (0.4) | |||
Some percentages may not sum to 100% because of missing values or rounding.
SES, socioeconomic status; LBW, low birth weight; SD, standard deviation; PM10, particulate matter with a diameter of <10 μm; pphm, parts per hundred million of air by volume.
No. of observations for “low SES”: summer (n = 5,482); winter (n = 5,545).
No. of observations for “middle SES”: summer (n = 5,779); winter (n = 5,859).
No. of observations for “high SES”: summer (n = 7,534); winter (n = 7,148).
Low SES neighborhoods had the highest percentage of preterm births (table 2). Traffic-related air pollution in low SES neighborhoods in the winter was associated with the highest proportion of preterm births, compared with other SES/season strata. Low and middle SES neighborhoods in the winter had greater proportions of preterm deliveries among African-American mothers. Preterm deliveries were also very high among uninsured women in low SES neighborhoods in the winter.
TABLE 2.
Proportion of preterm births for selected characteristics, by neighborhood socioeconomic status and season, Los Angeles County, California, 1994–1996
| Low SES* (mean (SD*)) |
Middle SES (mean (SD)) |
High SES (mean (SD)) |
||||
|---|---|---|---|---|---|---|
| Summer | Winter | Summer | Winter | Summer | Winter | |
| Preterm births | 0.38 (0.49) | 0.39 (0.49) | 0.36 (0.48) | 0.38 (0.49) | 0.32 (0.47) | 0.34 (0.47) |
| Traffic-related pollution exposure DWTD* percentile |
||||||
| <20th | 0.38 (0.49) | 0.37 (0.48) | 0.35 (0.48) | 0.36 (0.48) | 0.32 (0.47) | 0.34 (0.47) |
| 20th–<80th | 0.38 (0.49) | 0.39 (0.49) | 0.36 (0.48) | 0.38 (0.49) | 0.32 (0.47) | 0.33 (0.47) |
| ≥80th | 0.38 (0.48) | 0.41 (0.49) | 0.39 (0.49) | 0.40 (0.49) | 0.32 (0.47) | 0.36 (0.48) |
| Race | ||||||
| African American | 0.48 (0.50) | 0.47 (0.50) | 0.41 (0.49) | 0.49 (0.50) | 0.40 (0.49) | 0.39 (0.49) |
| Hispanic/Latino | 0.37 (0.48) | 0.38 (0.49) | 0.37 (0.48) | 0.38 (0.49) | 0.34 (0.47) | 0.35 (0.48) |
| Other race | 0.36 (0.48) | 0.30 (0.46) | 0.31 (0.46) | 0.33 (0.47) | 0.31 (0.46) | 0.32 (0.47) |
| White | 0.39 (0.49) | 0.29 (0.45) | 0.34 (0.47) | 0.27 (0.44) | 0.28 (0.45) | 0.29 (0.46) |
| Maternal age | ||||||
| <20 years | 0.42 (0.49) | 0.46 (0.50) | 0.42 (0.49) | 0.45 (0.50) | 0.35 (0.48) | 0.41 (0.49) |
| ≥35 years | 0.43 (0.50) | 0.47 (0.50) | 0.42 (0.49) | 0.39 (0.49) | 0.34 (0.47) | 0.34 (0.47) |
| Maternal education | ||||||
| <9 years | 0.40 (0.49) | 0.40 (0.49) | 0.39 (0.49) | 0.38 (0.49) | 0.37 (0.48) | 0.36 (0.48) |
| ≥16 years | 0.29 (0.46) | 0.29 (0.46) | 0.29 (0.46) | 0.30 (0.46) | 0.28 (0.45) | 0.28 (0.45) |
| Health insurance | ||||||
| Government insurance | 0.39 (0.49) | 0.40 (0.49) | 0.37 (0.48) | 0.39 (0.49) | 0.35 (0.48) | 0.37 (0.48) |
| Private insurance | 0.32 (0.47) | 0.33 (0.47) | 0.34 (0.47) | 0.35 (0.48) | 0.30 (0.46) | 0.31 (0.46) |
| No coverage | 0.36 (0.48) | 0.50 (0.50) | 0.41 (0.49) | 0.35 (0.48) | 0.31 (0.46) | 0.30 (0.46) |
| Prenatal care | ||||||
| First trimester | 0.37 (0.48) | 0.37 (0.48) | 0.35 (0.48) | 0.36 (0.48) | 0.31 (0.46) | 0.32 (0.47) |
| Later/none | 0.40 (0.49) | 0.42 (0.49) | 0.39 (0.49) | 0.44 (0.50) | 0.38 (0.49) | 0.41 (0.49) |
SES, socioeconomic status; SD, standard deviation; DWTD, distance-weighted traffic density.
The effects of traffic-related pollution exposure were most pronounced in the low SES neighborhoods during winter (table 3). Within the low SES area, those who lived in locations with higher traffic-related pollution exposure (80th percentile or higher) compared with those who lived in less trafficked locations (below the 20th percentile) had 30 percent increased odds of a preterm delivery. In middle SES neighborhoods, DWTD was associated with 18–19 percent increased odds of preterm birth during both seasons. In contrast, residential proximity to high traffic did not increase preterm delivery risk in women living in high SES neighborhoods.
TABLE 3.
Estimated odds ratios and 95% confidence intervals from the multivariate logistic regression model for preterm birth risk by neighborhood socioeconomic status and season, Los Angeles County, California, 1994–1996*
| Low SES† |
Middle SES |
High SES |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Summer |
Winter |
Summer |
Winter |
Summer |
Winter |
|||||||
| Odds ratio |
95% confidence interval |
Odds ratio |
95% confidence interval |
Odds ratio |
95% confidence interval |
Odds ratio |
95% confidence interval |
Odds ratio |
95% confidence interval |
Odds ratio |
95% confidence interval |
|
| Traffic-related pollution exposure |
||||||||||||
| DWTD† ≥80th vs. <20th percentile |
0.93 | 0.76, 1.13 | 1.30 | 1.07, 1.58 | 1.19 | 0.99, 1.43 | 1.18 | 0.99, 1.41 | 0.93 | 0.80, 1.09 | 1.00 | 0.85, 1.17 |
| Risk factors | ||||||||||||
| African American vs. White |
1.35 | 0.92, 1.99 | 2.21 | 1.46, 3.35 | 1.32 | 0.94, 1.85 | 2.58 | 1.81, 3.68 | 1.58 | 1.28, 1.94 | 1.32 | 1.06, 1.62 |
| Hispanic/Latino vs. White |
0.78 | 0.54, 1.12 | 1.41 | 0.95, 2.09 | 1.01 | 0.76, 1.34 | 1.62 | 1.19, 2.21 | 1.14 | 0.98, 1.31 | 1.09 | 0.95, 1.27 |
| Maternal age <20 vs. 20–30 years |
1.27 | 1.08, 1.49 | 1.40 | 1.19, 1.64 | 1.28 | 1.09, 1.51 | 1.29 | 1.09, 1.51 | 1.02 | 0.85, 1.21 | 1.23 | 1.03, 1.46 |
| Maternal age ≥35 vs. 20–30 years |
1.30 | 1.07, 1.59 | 1.65 | 1.35, 2.02 | 1.50 | 1.24, 1.81 | 1.17 | 0.97, 1.42 | 1.28 | 1.09, 1.50 | 1.24 | 1.05, 1.45 |
| Maternal education <9 vs. 12 years |
1.23 | 1.05, 1.45 | 1.19 | 1.01,1.40 | 1.15 | 0.98, 1.34 | 1.08 | 0.92, 1.26 | 1.19 | 1.01, 1.41 | 1.01 | 0.85, 1.21 |
| Protective factors | ||||||||||||
| Maternal education ≥16 vs. 12 years |
0.75 | 0.48, 1.18 | 0.79 | 0.48, 1.30 | 0.78 | 0.58, 1.05 | 0.89 | 0.66, 1.20 | 0.85 | 0.72, 1.01 | 0.84 | 0.70, 0.99 |
| Government insurance vs. no coverage |
1.17 | 0.73, 1.89 | 0.61 | 0.39, 0.96 | 0.80 | 0.58, 1.10 | 1.13 | 0.75, 1.69 | 1.12 | 0.85, 1.47 | 1.33 | 1.00, 1.76 |
| Private insurance vs. no coverage |
0.86 | 0.53, 1.42 | 0.50 | 0.31, 0.79 | 0.75 | 0.54, 1.05 | 1.03 | 0.68, 1.56 | 1.03 | 0.79, 1.35 | 1.12 | 0.84, 1.48 |
| First trimester prenatal care vs. later/none |
0.91 | 0.80, 1.03 | 0.86 | 0.76, 0.98 | 0.87 | 0.76, 0.98 | 0.75 | 0.67, 0.85 | 0.79 | 0.69, 0.90 | 0.75 | 0.66, 0.86 |
Adjusted for infant’s sex, previous low birth weight or preterm infant, parity, interval since previous livebirth, year of birth, carbon monoxide, nitrogen dioxide, particulate matter with a diameter of <10 μm, and nitrogen trioxide.
SES, socioeconomic status; DWTD, distance-weighted traffic density.
Relative to Whites, African Americans had higher odds of preterm deliveries whether or not they lived in high or low SES areas (table 3). We found the strongest effects for preterm birth among the African-American women who gave birth during the winter in the low SES neighborhoods (odds ratio (OR) = 2.21, 95 percent confidence interval (CI): 1.46, 3.35) and middle SES neighborhoods (OR = 2.58, 95 percent CI: 1.81, 3.68). Hispanic mothers living in middle SES areas experienced a 62 percent elevated odds of a preterm delivery during winter, while they otherwise did not experience higher risks than did White women.
Women younger than 20 years of age compared with women aged 20–30 years faced 23–40 percent higher odds for preterm delivery in all season/SES strata except during the summer in high SES neighborhoods. Young mothers had the highest likelihood of delivering preterm in the low SES neighborhoods during winter (OR = 1.40, 95 percent CI: 1.19, 1.64). In general, women who delivered at 35 or more years of age also had higher odds (17–65 percent) compared with the referent age group. Their greatest odds increase was observed in the low SES neighborhoods in winter (OR = 1.65, 95 percent CI: 1.35, 2.02).
A low level of education (fewer than 9 years compared with 12 years of schooling) increased the odds of a preterm delivery by 19–23 percent, but only among women in low SES neighborhoods and in high SES neighborhoods in the summer. Attaining the highest educational level was protective only in the high SES neighborhoods.
Compared with no coverage, government health insurance (OR = 0.61, 95 percent CI: 0.39, 0.96), principally Medicaid, and private health coverage (OR = 0.50, 95 percent CI: 0.31, 0.79) had the strongest protective effect against preterm birth in low SES neighborhoods during winter. We found the opposite effect in high SES neighborhoods during winter: Women with government insurance had generally higher odds of preterm deliveries.
DISCUSSION
We examined preterm birth within a comprehensive framework of the social and physical environments and individual-level risk and protective factors. Specifically, we explored whether preterm birth risk may be affected by the interaction of residential traffic-related air pollution exposure (DWTD) with neighborhood economic hardship.
We found that DWTD had the greatest adverse effect in the low SES areas during the winter season. Our findings also suggest that middle SES neighborhoods experienced an adverse effect in the summer and winter. However, we found no effect in high SES neighborhoods regardless of season. High SES neighborhoods might differ from low and middle SES neighborhoods with respect to a number of factors influencing exposure to a local pollution source such as traffic: 1) cars are newer and create less pollution in high SES neighborhoods, whereas low SES areas may be frequented by a greater percentage of older, high emitting gasoline or diesel vehicles; or 2) homes are newer, better insulated, equipped with air conditioning, and set back farther from the curb on larger residential lots so that pollution from highly trafficked roads does not affect the indoor environment as it does in low SES neighborhoods. Thus, one could argue that our traffic density measure does not reflect the same locally increased exposure from traffic at a home in high compared with low SES neighborhoods. On the other hand, conditions during the winter months seem to result in increased effect estimates only in low and middle SES areas. This may suggest a combination of greater vulnerability for women living in these neighborhoods and higher localized exposures from traffic exhaust, even when adjusting for general differences in air pollution levels measured at background stations.
Indeed, our results indicate that the susceptibility for preterm birth among vulnerable groups varied by neighborhood SES and season. As reported previously (15, 26, 28, 29), we found that the odds of a preterm delivery were increased among African Americans, Hispanics, and younger or older mothers, with the biggest disparity in low and middle SES neighborhoods during winter. We found that African-American women face higher odds for preterm birth across all SES strata. However, in the more economically deprived neighborhoods, African-American women’s increased odds of preterm delivery during winter suggest their added susceptibility to the changes in the conditions of the physical environment. Thus, for areas affected with the cumulative adverse effects of the social and physical environments, the implication of our study is that economic development programs need to be in tandem with environmental regulation to effectively reduce preterm births.
We found that the vulnerable groups, particularly African-American mothers, still faced increased odds of a preterm birth, despite living in high SES neighborhoods. This may be attributable to several unmeasured factors: 1) there may be race-based differential access to health services and other neighborhood resources that may be more disparate in high SES neighborhoods (27), or 2) individual-level social and cultural differences may result in variations in an individual’s transformation of available neighborhood resources that lead to better birth outcomes (30). Our study was not designed to identify the source of these neighborhood stressors, but our results suggest that social processes and their influence on a preterm birth outcome differ by neighborhood SES. This may indicate that a postulated biologic susceptibility for the outcome related to race and maturity/exhaustion of the maternal reproductive system is heightened when either the physical or the social environment is less supportive (8).
Our findings concur with those from previous studies suggesting that education, prenatal care, and health insurance might mitigate the risk for preterm delivery (1, 31-33). Lacking a high school diploma was associated with increased risk, but mostly in the low SES communities. We found a positive though weak association of the protective effect of high maternal education in the low and middle SES neighborhoods, perhaps because very few women (2-5 percent) had 16 or more years of schooling in these strata. Government and private health insurance, compared with the self-paying/uninsured, appeared to benefit women, but only in low, and not in high, SES neighborhoods. This suggests that in high SES neighborhoods, government insurance, principally Medicaid, acted as a marker for lower-income mothers: Relative to self-paying/uninsured women in the high SES neighborhoods, these women were financially disadvantaged. Members of more economically advantaged neighborhoods may have higher levels of education and can avail themselves of more choices in neighborhood resources, so that insurance coverage has less importance and consequently has less impact (34). In contrast, in the low SES neighborhoods, women with government insurance may have been economically better off compared with the self-paying/uninsured women in their neighborhoods. In low SES neighborhoods, private coverage, like government insurance, conferred a protective effect. Although health insurance is clearly a marker for many unmeasured SES advantages, our results are suggestive that health insurance, whether government or private, appears to be effective only in the most economically deprived areas. This is consistent with the economic hypothesis that the marginal effect of health insurance in improving health outcomes diminishes in higher income areas because beneficial outcomes are already maximized (35). Early initiation of prenatal care had a beneficial effect in all neighborhood settings and seasons, with no marked neighborhood SES gradient. Thus, the quality of prenatal care across different SES neighborhoods may be consistent across neighborhoods in its effectiveness in reducing preterm births. However, access may still be an issue since fewer women in the low and middle SES neighborhoods received prenatal care during the first trimester than in the high SES neighborhoods.
Study limitations include a potential bias arising from two sources in our final sample of study subjects. First, since the study sample included only 112 of the 269 Los Angeles ZIP codes, it may not be representative of the entire county. However, our results have focused policy implications because they are generalizable to many urban areas that are affected by traffic. Second, our inability to map all eligible subjects may have also resulted in exclusion of a higher proportion of cases than controls, but then our DWTD estimates would be biased toward the null.
We defaulted to census tracts as a plausible though admittedly imperfect definition of neighborhoods, but this is a methodological issue grappled with by neighborhood effects research in general (12, 36). More importantly, our neighborhood SES measure of economic hardship reflected neighborhood economic conditions that may constrain a pregnant woman’s choices and decisions, thereby influencing her pregnancy outcome. Our results are only suggestive of unobserved social processes that take place between the woman and her residential community. Increasingly, studies have attempted to evaluate previously unmeasured neighborhood dynamics through hypothesized neighborhood mechanisms, for example, perceived safety in a neighborhood associated with the level of maternal stress during pregnancy, and the social exchange/voluntarism/trust in a community that may reduce a woman’s stress (11, 37). For a future analysis, we plan to link more recent birth record data in Los Angeles County to data from the population-based California Health Interview Survey 2003 (38). This survey collected information on neighborhood social support and cohesion similar to the questions used by the Project on Human Development in Chicago Neighborhoods (39). Another limitation of our analysis is the omission of relevant variables not collected in the California birth certificate data, such as maternal smoking during pregnancy. Our recent survey of 2,500 randomly selected women who gave birth during 2003 in the ZIP code areas we studied will provide the important information absent in our current analysis, including individual- and household-level information on maternal smoking, exposure to second hand smoke, occupation, commute, indoor/outdoor living patterns, and perceived discrimination.
We posited that, during winter, the physical environment is more adverse due to increased air pollution near traffic sources when winter thermal inversions trap exhaust (40, 41). However, the localized physical environment may also be more adverse because infection rates are higher during the winter (16, 42, 43). Wintertime pollution conditions may thus act indirectly or synergistically with infectious agents in increasing a pregnant woman’s susceptibility to pollution-related reproductive failures and, consequently, preterm births (44-47).
Finally, we cannot definitively rule out residual confounding by varying neighborhood characteristics that were unmeasured, such as the presence of a community health center in one neighborhood versus another. Future studies should consider measuring and accounting for supply-side resources on health and social services that may promote healthy pregnancies.
In conclusion, we confirmed that risk for preterm delivery is associated with individual and traffic-related pollution exposure factors previously shown to increase risk. More interestingly, these risks differed by neighborhood SES and by season. A woman’s individual susceptibility to preterm delivery may be altered by the physical environment, the social and economic resources available to her, and her ability to transform these resources into beneficial birth outcomes. Reducing preterm births therefore warrants a concerted effort of social, economic, and environmental policies, focused not only on individual risk factors but also on reducing traffic-related air pollution, expanding health-care coverage, and improving neighborhood resources.
ACKNOWLEDGMENTS
This research was funded by National Institute of Environmental Health Sciences grant R01 ES010960-01.
The authors thank Sander Greenland, Naihua Duan, Fei Yu, and Robert Nordyke for reviewing our conceptual framework and models and for providing statistical advice.
Abbreviations
- CI
confidence interval
- DWTD
distance-weighted traffic density
- OR
odds ratio
- SES
socioeconomic status
Footnotes
Conflict of interest: none declared.
REFERENCES
- 1.Moore ML. Preterm labor and birth: what have we learned in the past two decades? J Obstet Gynecol Neonatal Nurs. 2003;32:638–49. doi: 10.1177/0884217503257367. [DOI] [PubMed] [Google Scholar]
- 2.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2002. Natl Vital Stat Rep. 2003;52:1–113. [PubMed] [Google Scholar]
- 3.da Silva AA, Simoes VM, Barbieri MA, et al. Young maternal age and preterm birth. Paediatr Perinat Epidemiol. 2003;17:332–9. doi: 10.1046/j.1365-3016.2003.00515.x. [DOI] [PubMed] [Google Scholar]
- 4.Berkowitz GS, Blackmore-Prince C, Lapinski RH, et al. Risk factors for preterm birth subtypes. Epidemiology. 1998;9:279–85. [PubMed] [Google Scholar]
- 5.Parker JD, Schoendorf KC, Kiely JL. Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States. Ann Epidemiol. 1994;4:271–8. doi: 10.1016/1047-2797(94)90082-5. [DOI] [PubMed] [Google Scholar]
- 6.Blackmore CA, Ferre CD, Rowley DL, et al. Is race a risk factor or a risk marker for preterm delivery? Ethn Dis. 1993;3:372–7. [PubMed] [Google Scholar]
- 7.Shiono PH, Klebanoff MA. Ethnic differences in preterm and very preterm delivery. Am J Public Health. 1986;76:1317–21. doi: 10.2105/ajph.76.11.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattison D, Wilson S, Coussens C, et al. The role of environmental hazards in premature birth. National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- 9.Kaufman JS, Dole N, Savitz DA, et al. Modeling community-level effects on preterm birth. Ann Epidemiol. 2003;13:377–84. doi: 10.1016/s1047-2797(02)00480-5. [DOI] [PubMed] [Google Scholar]
- 10.English PB, Kharrazi M, Davies S, et al. Changes in the spatial pattern of low birth weight in a southern California county: the role of individual and neighborhood level factors. Soc Sci Med. 2003;56:2073–88. doi: 10.1016/s0277-9536(02)00202-2. [DOI] [PubMed] [Google Scholar]
- 11.Buka SL, Brennan RT, Rich-Edwards JW, et al. Neighborhood support and the birth weight of urban infants. Am J Epidemiol. 2003;157:1–8. doi: 10.1093/aje/kwf170. [DOI] [PubMed] [Google Scholar]
- 12.Krieger N, Chen JT, Waterman PD, et al. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: the Public Health Disparities Geocoding Project (US) J Epidemiol Community Health. 2003;57:186–99. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pickett KE, Ahern JE, Selvin S, et al. Neighborhood socioeconomic status, maternal race and preterm delivery: a case-control study. Ann Epidemiol. 2002;12:410–18. doi: 10.1016/s1047-2797(01)00249-6. [DOI] [PubMed] [Google Scholar]
- 14.O’Campo P, Xue X, Wang MC, et al. Neighborhood risk factors for low birthweight in Baltimore: a multilevel analysis. Am J Public Health. 1997;87:1113–18. doi: 10.2105/ajph.87.7.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rauh VA, Andrews HF, Garfinkel RS. The contribution of maternal age to racial disparities in birthweight: a multilevel perspective. Am J Public Health. 2001;91:1815–24. doi: 10.2105/ajph.91.11.1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luo Z, Kierans W, Wilkins R, et al. Disparities in birth outcomes by neighborhood income: temporal trends in rural and urban areas, British Columbia. Epidemiology. 2004;15:679–86. doi: 10.1097/01.ede.0000142149.34095.88. [DOI] [PubMed] [Google Scholar]
- 17.O’Neill MS, Jerrett M, Kawachi I, et al. Health, wealth, and air pollution: advancing theory and methods. Environ Health Perspect. 2003;111:1861–70. doi: 10.1289/ehp.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilhelm M, Ritz B. Residential proximity to traffic and adverse birth outcomes in Los Angeles County, California, 1994-1996. Environ Health Perspect. 2003;111:207–16. doi: 10.1289/ehp.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ritz B, Yu F, Chapa G, et al. Effect of air pollution on preterm birth among children born in southern California between 1989 and 1993. Epidemiology. 2000;11:502–11. doi: 10.1097/00001648-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Roberts EM. Neighborhood social environments and the distribution of low birthweight in Chicago. Am J Public Health. 1997;87:597–603. doi: 10.2105/ajph.87.4.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Bureau of the Census . Census of population and housing, 1990. Summary tape file 3: technical documentation. (CD-ROM) Bureau of the Census; Washington, DC: 1990. [Google Scholar]
- 22.US Department of Health and Human Services poverty guidelines. Federal Register 2001. 2001;66:10695–7. [Google Scholar]
- 23.Lipfert FW. Air pollution and poverty: does the sword cut both ways? J Epidemiol Community Health. 2004;58:2–3. doi: 10.1136/jech.58.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gunier RB, Hertz A, Von Behren J, et al. Traffic density in California: socioeconomic and ethnic differences among potentially exposed children. J Expo Anal Environ Epidemiol. 2003;13:240–6. doi: 10.1038/sj.jea.7500276. [DOI] [PubMed] [Google Scholar]
- 25.National Climatic Data Center . Monthly average maximum & minimum temperatures, 2004. National Climatic Data Center; Asheville, NC: 2004. [Google Scholar]
- 26.Woodruff TJ, Parker JD, Kyle AD, et al. Disparities in exposure to air pollution during pregnancy. Environ Health Perspect. 2003;111:942–6. doi: 10.1289/ehp.5317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smedley BD, Stith AY, Nelson AR. Unequal treatment: confronting racial and ethnic disparities in health care. National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- 28.Ahern J, Pickett KE, Selvin S, et al. Preterm birth among African American and white women: a multilevel analysis of socioeconomic characteristics and cigarette smoking. J Epidemiol Community Health. 2003;57:606–11. doi: 10.1136/jech.57.8.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berkowitz GS, Papiernik E. Epidemiology of preterm birth. Epidemiol Rev. 1993;15:414–43. doi: 10.1093/oxfordjournals.epirev.a036128. [DOI] [PubMed] [Google Scholar]
- 30.Currie J, Hyson R. Is the impact of health shocks cushioned by socioeconomic status? The case of low birthweight. Am Econ Rev. 1999;89:245–50. [Google Scholar]
- 31.Guillory VJ, Samuels ME, Probst JC, et al. Prenatal care and infant birth outcomes among Medicaid recipients. J Health Care Poor Underserved. 2003;14:272–89. doi: 10.1353/hpu.2010.0734. [DOI] [PubMed] [Google Scholar]
- 32.Long SH, Marquis MS. The effects of Florida’s Medicaid eligibility expansion for pregnant women. Am J Public Health. 1998;88:371–6. doi: 10.2105/ajph.88.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ray WA, Mitchel EF, Jr, Piper JM. Effect of Medicaid expansions on preterm birth. Am J Prev Med. 1997;13:292–7. [PubMed] [Google Scholar]
- 34.Marquis SM, Long SH. The role of public insurance and the public delivery system in improving birth outcomes for low-income pregnant women. Med Care. 2002;40:1048–59. doi: 10.1097/00005650-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Phelps CE. Health economics. Addison Wesley; Boston, MA: 2003. [Google Scholar]
- 36.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783–9. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morenoff JD. Neighborhood mechanisms and the spatial dynamics of birth weight. Am J Sociol. 2003;108:976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- 38.About the California Health Interview Survey. UCLA Center for Health Policy Research; Los Angeles, CA: 2004. www.chis.ucla.edu. [Google Scholar]
- 39.Raudenbush S. The quantitative assessment of neighborhood social environments. Oxford University Press; New York, NY: 2003. [Google Scholar]
- 40.Zhu Y, Hinds WC, Shen S, et al. Seasonal trends of concentration and size distribution of ultrafine particles near major highways in Los Angeles. Aerosol Sci Technol. 2004;38:5–13. [Google Scholar]
- 41.Flachsbart PG. Long-term trends in United States highway emissions, ambient concentrations, and in-vehicle exposure to carbon monoxide in traffic. J Expo Anal Environ Epidemiol. 1995;5:473–95. [PubMed] [Google Scholar]
- 42.Hartert TV, Neuzil KM, Shintani AK, et al. Maternal morbidity and perinatal outcomes among pregnant women with respiratory hospitalizations during influenza season. Am J Obstet Gynecol. 2003;189:1705–12. doi: 10.1016/s0002-9378(03)00857-3. [DOI] [PubMed] [Google Scholar]
- 43.Dowell SF, Whitney CG, Wright C, et al. Seasonal patterns of invasive pneumococcal disease. Emerg Infect Dis. 2003;9:573–9. doi: 10.3201/eid0905.020556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cooperstock M, Wolfe RA. Seasonality of preterm birth in the Collaborative Perinatal Project: demographic factors. Am J Epidemiol. 1986;124:234–41. doi: 10.1093/oxfordjournals.aje.a114381. [DOI] [PubMed] [Google Scholar]
- 45.Matsuda S, Kahyo H. Geographic differences in seasonality of preterm births in Japan. Hum Biol. 1998;70:919–35. [PubMed] [Google Scholar]
- 46.Russell D, Douglas AS, Allan TM. Changing seasonality of birth—a possible environmental effect. J Epidemiol Community Health. 1993;47:362–7. doi: 10.1136/jech.47.5.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weinberg CR, Moledor E, Baird DD, et al. Is there a seasonal pattern in risk of early pregnancy loss? Epidemiology. 1994;5:484–9. [PubMed] [Google Scholar]