Abstract
Addison's disease is a rare endocrinal disorder, with several oral and systemic manifestations. A variety of pathological processes may cause Addison's disease. Classically, hyperpigmentation is associated with the disease, and intraoral pigmentation is perceived as the initial sign and develops earlier than the dermatological pigmentation. The symptoms of the disease usually progress slowly and an event of illness or accident can make the condition worse and may lead to a life-threatening crisis. In this case, several oral as well as systemic manifestation of the Addison's disease was encountered.
Keywords: Addison's disease, adrenoleukodystrophy, hemochromatosis, hyperpigmentation, prednisolone
Introduction
Addison's disease is rare endocrinal disorder that affects 1 in 100,000 people. It is seen in all age groups and affects male and female equally. This disease is named after Thomas Addison, who first described patients affected by this disorder in 1855, in the book titled “On the constitutional and local effects of the disease of supra renal capsule.”[1,2] Addison's disease can present as a life-threatening crisis, because it is frequently unrecognized in its early stages. The basis of Addison's disease has dramatically changed from an infectious cause to autoimmune pathology since its initial description. However, tuberculosis is still the predominant cause of Addison's disease in developing countries.[3]
The symptom of Addison's disease begins gradually, chronic worsening fatigue, loss of appetite, generalized weakness, hypotension, and weight loss. The clinical features of hypoadrenocorticism do not actually begin to appear until at least 90% of the glandular tissue has been destroyed. Generalized hyperpigmentation of skin is seen, which is classically described as “bronzing” the hyperpigmentation is generally more prominent on sun-exposed skin and over pressure points, such as the elbows and knees which are caused by increased levels of beta-lipotropin or Adrenocorticotropic hormone, each of which can stimulate melanocyte production. Hyperpigmentation of the mucous membrane and skin usually proceeds over other symptoms by month to year. Vitiligo may also be seen in association with hyperpigmentation in idiopathic Addison's disease due to autoimmune destruction of melanocytes.[4–6]
Hyponatremia and hyperkalemia are commonly associated with Addison's disease, while hypoglycaemia uncommon. The patient usually complains of gastrointestinal upset with anorexia, nausea, vomiting, diarrhea, and a peculiar craving for salt. Adrenal calcification and enlargement are commonly seen in Addison's disease associated with tuberculosis.[7–9]
The symptoms of Addison' disease progress slowly and are usually ignored, an event of illness or accident can make the condition worsen and lead to Addisonian crisis. Sudden penetrating pains in the lower back region, abdomen or legs are symptoms of Addisonian crisis with severe vomiting and diarrhea, which is followed by dehydration, low blood pressure and loss of consciousness.[6,9]
The current case not only presents with the typical features of the disorder but also with the extra and particularly unique extensive intraoral pigmentation which is often considered as the initial presentation of the Addison's disease.
Case Report
A 26-year-old female came with the complaint of bleeding gum and bad breath, since last 10 months. Patient was anxious, but evidently fatigued, weakened, and easily irritable. Patient also gave a history of occasional abdominal pain, amenorrhea, nausea, and vomiting, dysphagia, weight loss and hypotension. She also gave history of sleep disturbances occasionally, which is usually accompanied by the exacerbation of abdominal pain. On clinical examination thin and brittle nail, scanty body hair, hyperpigmentation of skin in the neck [Figure 1] and in the lower abdominal region was present. There was a pulse of 106 bpm, and blood pressure 90/65 mmHg supine. Extraoral examination showed browny pigmentation affecting the perioral region. Intraoral examination demonstrated pigmentation with bilateral involvement of buccal mucosa, gingival, mucosal surface of lower lip, alveolar mucosa, and hard palate [Figure 2]. Tongue appears to be smooth with loss of the papilla with pigmentation on the posterior surface [Figure 3]. The gingiva appears to be blunt with apical positioning of gingival margins, significant loss of attachment with pocket depth between 3 and 5 mm.
Figure 1.

Hyperpigmentation in the neck and chest region
Figure 2.
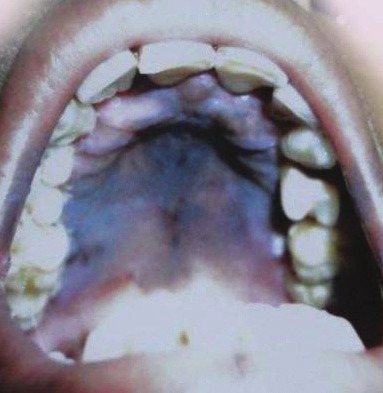
Hyperpigmentation in the palate
Figure 3.
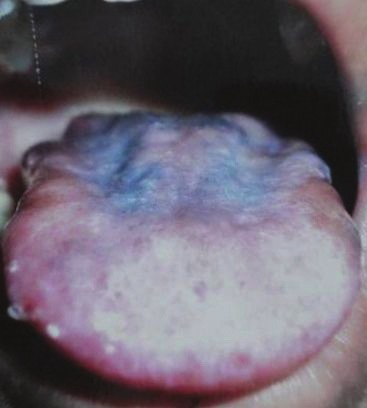
Hyperpigmentation and depapillation of the tongue
Laboratory investigations revealed anemia with hemoglobin level 7.8 g/dl, with normal red blood cell morphology, erythrocyte sedimentation rate (ESR) 59 mm/h, fasting blood sugar 70 mg/dl. The metabolic profile, including serum urea, creatinine and electrolyte all were within the normal range. Early morning cortisol level was well below normal level 2.2 μg/dl. Anti-HIV, anti hepatitis C virus hepatitis B surface antigen (HCV HBsAg) factors were negative. Mantoux tuberculin skin test was negative and chest radiograph also ruled out tuberculosis. Based on patient history, clinical findings and laboratory investigations, we reached to the diagnosis of Addison's disease. Initially, scaling was done and instruction was given to maintain oral hygiene. Cortisol replacement in from of methyl prednisolone 10 mg in morning and 5 mg in evening is started, as her condition improved the dose of methyl prednisolone is reduced to 7.5 mg per day. She had an episode of Addisonian crisis 3 months after the initial visit and admitted to the hospital, where acute malarial attack was diagnosed to be the precipitating factor. She was managed intravenous fluids, parental supplement glucose, hydrocortisone, and anti-malarial drugs. She had full recovery after 20 days of hospitalization and is maintained on prednisolone.
Discussion
A variety of pathological processes may cause Addison's disease, which was first described by Thomas Addison.[1–3] The commonest causes of Addison's disease are autoimmune and tuberculosis. Several autoimmune processes can lead to adrenal insufficiency affecting exclusively the adrenal glands or be part of a more complex inherited autoimmune polyglandular syndrome.[2,3,6,10] Tuberculosis is the most common cause of Addison's disease in developing countries. Fungal infection, hemochromatosis, metastatic neoplasm, and X-linked adrenoleukodystrophy are other causes of Addison's disease.[2,11] Several investigators have found dysphagia, fatigue, weight loss and hypotension, abdominal pain, amenorrhea, nausea, and vomiting, thin and brittle nail, scanty body hair in Addison's disease, which is also present in this study.[2–5,7–9,11,12] Psychiatric symptoms such as mood disturbances, decreased motivation, and behavior changes are frequently associated with Addison's disease. According to Anglin et al., the etiology of neuropsychiatric symptoms associated with Addison's disease is unknown, but may be related with the disturbances in the electrophysiological, electrolyte, and metabolic activity. In this case, positive history of mood disturbances and behavior changes is also present.[13] Sleep disturbances on periodic exacerbation is present in this case, which is according to the study by Løvås et al.[14] One of the hallmark signs of Addison's disease is cutaneous and mucosal hyperpigmentations related to ACTH melanogenesis action.[3–5] Soule reported that the presenting features among 50 patients seen over a 17-year period, as including hyperpigmentation (86%), weight loss (67%), abdominal pain (20%), and diarrhea (16%).[7] Pigmentation can be homogeneous or blotchy. The pigmentation may involve skin, oral cavity, conjunctiva, and genitalia.[3,5] Brown patches of gingival, vermillion border of the lips, buccal mucosa, palate, and tongue may represent the first signs of Addison's disease.[5] In this study, pigmentation was present in the neck [Figure 1] and in the lower abdominal region with bilateral involvement of buccal mucosa, gingival, mucosal surface of lower lip, and alveolar mucosa. Tongue appears to be smooth with loss of the papilla with pigmentation on the posterior surface [Figure 3]. Lab investigation in this case presented hemoglobin value of 7.8 g/dl, with normal morphology of the erythrocyte, ESR was 59 mm/h, and fasting blood sugar level was 70 mg/dl. Serum urea, creatinine, and electrolyte levels were within the normal range. Grinspoon and Biller[15] observed decrease hemoglobin percentage, decrease blood sugar level, which is also present in this study. This case is managed by methyl prednisolone initially and later she developed Addison crisis and fully recovered after brief hospitalization. The patient is now maintained with methyl prednisolone.
Conclusion
Addison disease is rare endocrinal disorder, in the developed nations it usually related to auto-immune disorder but in the developing nations it is widely associated with tuberculosis. Addison disease is usually associated with dysphagia, fatigue, weight loss, hypotension, abdominal pain, amenorrhea, nausea, vomiting, thin and brittle nail, scanty and body hair. Addison disease is classically seen with hyperpigmentation due to ACTH melanogenesis. Intraorally pigmentation over the gingival, vermillion border of lip, buccal mucosa, palate tongue, is evident and perceived as first sign. As the oral manifestation of the Addison's disease, particularly oral pigmentation may develop earlier than their dermatological counterpart, dental surgeon may be the first medical professional to encounter disease and early diagnosis of the disease essential for proper medical management.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
References
- 1.Grossman AB. Thomas Addison and his disease. Grand Rounds. 2004;4:L8–9. [Google Scholar]
- 2.Hiatt JR, Hiatt N. The conquest of Addison's disease. Am J Surg. 1997;174:280–3. doi: 10.1016/s0002-9610(97)00136-0. [DOI] [PubMed] [Google Scholar]
- 3.Stewart PM, Krone NP. The adrenal cortex. In: Kronenburg HM, Melmed S, Polonsky KS, Reed Larson P, editors. Williams Textbook of Endocrinology. 12th ed. Philadelphia PA: Saunders Elsevier; 2011. pp. 515–20. Ch. 15. [Google Scholar]
- 4.Zargar AH, Laway BA, Masoodi SR, Bashir MI, Wani AI, Salahuddin M. A critical evaluation of signs and symptoms in the diagnosis of Addison›s diseases. J Assoc Physicians India. 2001;49:523–6. [PubMed] [Google Scholar]
- 5.Lanza A, Heulfe I, Perillo L, Dell'Ermo A, Cirillo N. Oral manifestation as a sign of Addison's disease: A brief reappraisal. Open Dermatol J. 2009;3:3–6. [Google Scholar]
- 6.Ten S, New M, Maclaren N. Clinical review 130: Addison's disease 2001. J Clin Endocrinol Metab. 2001;86:2909–22. doi: 10.1210/jcem.86.7.7636. [DOI] [PubMed] [Google Scholar]
- 7.Soule S. Addison’ disease in Africa: A teaching hospital experience. Clin Endocrinol (Oxf) 1999;50:115–20. doi: 10.1046/j.1365-2265.1999.00625.x. [DOI] [PubMed] [Google Scholar]
- 8.Chakera AJ, Vaidya B. Addison disease in adults: Diagnosis and management. Am J Med. 2010;123:409–13. doi: 10.1016/j.amjmed.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 9.O'Connell S, Siafarikas A. Addison disease – Diagnosis and initial management. Aust Fam Physician. 2010;39:834–7. [PubMed] [Google Scholar]
- 10.Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003;361:1881–93. doi: 10.1016/S0140-6736(03)13492-7. [DOI] [PubMed] [Google Scholar]
- 11.Oelkers W. Adrenal insufficiency. N Engl J Med. 1996;335:1206–12. doi: 10.1056/NEJM199610173351607. [DOI] [PubMed] [Google Scholar]
- 12.Mason AS, Meade TW, Lee JA, Morris JN. Epidemiological and clinical picture of Addison's disease. Lancet. 1968;2:744–7. doi: 10.1016/s0140-6736(68)90948-3. [DOI] [PubMed] [Google Scholar]
- 13.Anglin RE, Rosebush PI, Mazurek MF. The neuropsychiatric profile of Addison's disease: Revisiting a forgotten phenomenon. J Neuropsychiatry Clin Neurosci. 2006;18:450–9. doi: 10.1176/jnp.2006.18.4.450. [DOI] [PubMed] [Google Scholar]
- 14.Løvås K, Husebye ES, Holsten F, Bjorvatn B. Sleep disturbances in patients with Addison's disease. Eur J Endocrinol. 2003;148:449–56. doi: 10.1530/eje.0.1480449. [DOI] [PubMed] [Google Scholar]
- 15.Grinspoon SK, Biller BM. Clinical review 62: Laboratory assessment of adrenal insufficiency. J Clin Endocrinol Metab. 1994;79:923–31. doi: 10.1210/jcem.79.4.7962298. [DOI] [PubMed] [Google Scholar]


