Abstract
Aim:
The study was designed to explore the changes in oral health-related quality of life (QoL) in the immediate postoperative period following routine (non-surgical) dental extraction.
Setting and Design:
A prospective study carried out at the Oral and Maxillofacial Surgery clinic of the Lagos University Teaching Hospital, Nigeria.
Materials and Methods:
Subjects attending who required non-surgical removal of one or two teeth under local anesthesia were included in the study. A baseline QoL questionnaire (oral health impact profile-14 [OHIP-14]) was filled by each patient just before surgery, and only those who were considered to have their QoL “not affected” (total score 14 or less) were included in the study. After the extraction, each subject was given a modified form of “health related QoL” [OHIP-14]-instrument to be completed by the 3rd day-after surgery, and were given the opportunity to review the questionnaire on the 7th day postoperative review.
Results:
Total OHIP-14 scores ranged between 14 and 48 (mean ± SD, 26.2 ± 8.3). Majority of the subjects (60%) reported, “a little affected.” Only few subjects (5.8%) reported, “not at all affected,” and about 32% reported, “quite a lot.” Summation of OHIP-14 scores revealed that QoL was “affected” in 41 subjects (34.2%) and “not affected” in 79 subjects (65.8%). More than 30% of subjects reported that their ability to chew, ability to open the mouth and enjoyment of food were affected following tooth extraction. Few subjects (14-34%) reported deterioration in their speech and less than 20% of subjects reported that change in their appearance was “affected.” Only few subjects (12.5-15.1%) reported sleep and duty impairment. Thirty-percent of subjects reported their inability to keep social activities, and 41% were not able to continue with their favorite sports and hobbies. Multiple regression analysis revealed no significant association between age, sex, indications for extraction, duration of extraction, intra-operative complications, and deterioration in QoL (P < 0.05). Consumption of analgesics beyond postoperative day 1 (POD1) was more common in subjects with socket healing complications than those without (P = 0.000). About 33% of subjects reported, “inability to work” (1-3 days).
Conclusion:
About a third of subjects experienced significant deterioration in QoL. The most affected domains were eating/diet variation and speech variation. Therefore, patients should be informed of possible deterioration in their QoL following non-surgical tooth extraction.
Keywords: Intra-alveolar, quality of life, tooth extraction
Introduction
Extraction of teeth is the most common procedure carried out in oral surgery clinics. The final consequence of most dento-alveolar diseases is tooth loss, mostly through routine tooth extraction.[1] Reasons for routine tooth extractions have been widely reported in medical literature.[1–5] In addition, postoperative pain and discomfort, loss day at work as well as healing complications have been well reported in the immediate postoperative period following non-surgical (routine) tooth extraction.[6–8] Despite the fact that these are all indicators of quality of life (QoL) affectation, QoL after routine tooth has not yet been reported in the literature.
Extensive studies on QoL after third molar surgery have shown that the aspects often of more concern to the patient include limited mouth opening, impaired ability to masticate and swallow; changes in diet, enjoyment and taste of food, sleep disturbances, altered vocal functions, time off work and inability to socialize.[9–13] By implication, patients attach more importance to the functional handicap, whereas, the surgeon believes pain would be the main problem foremost in the patient's mind.[9–13] The understanding of the impact of QoL provides a more comprehensive assessment of physical, social and psychological consequences of treatment at personal and societal levels.[11]
Patients are increasingly asking medical practitioners the effect of a surgical procedure on their daily routine. Patients have often asked whether they would be able to return to work after extraction, when the effect of anesthesia would wear off, when to resume normal diet, how long they would feel pain and sometimes possible complications after non-surgical tooth extraction. Therefore, it is important to explore the effect of routine tooth extraction on QoL in the immediate postoperative period.
The present pilot study was designed to explore the oral health-related QoL in the immediate postoperative period following non-surgical (routine) tooth extraction.
Materials and Methods
Healthy subjects attending the oral and maxillofacial surgery clinic of the Lagos University Teaching Hospital, Nigeria between January and June 2010, who required intra-alveolar extraction of one or two teeth under local anesthesia were included in the study. Data obtained from each subject included: Age and sex, indication extraction, type and number of teeth extracted, duration of extraction, intra-operative, and postoperative complications. Exclusion criteria from participation in the study included: Elective surgical extraction, difficult intra-alveolar extraction necessitating a switch to trans-alveolar extraction. A preoperative QoL questionnaire (oral health impact profile-14 [OHIP-14]) (a modified form of Colorado Bonnin et al,[14] was filled by each subject just before surgery, and only those who were considered to have their QoL “not affected” (total score less than or equal to 14) were included in the study. Extraction of teeth was done under local anesthesia (2% lignocaine with 1:80,000 adrenaline). Extraction of teeth was either carried out by residents in training or dental students under the supervision of senior doctors. After the extraction, each subject was given a modified form of “health related QoL” [OHIP-14]-instrument to be completed by the 3rd day-after surgery, and were given the opportunity to review the questionnaire on the 7th day postoperative review. OHIP-14 questionnaire employed was a modification of Colorado-Bonnin et al.[14] Other data included in the analysis were age and sex of subjects, indications for extraction, duration of extraction (minutes), intra-operative complications, socket healing complications. Postoperative pain was assessed using a 4 point verbal rating scale (1 = no pain; 2 = mild pain; 3 = moderate pain; 4 = severe pain) to be completed for each postoperative day for 7 days.
The approval for the study was obtained from the Health and Research Ethics Committee of the hospital. Written informed consent was obtained from each subject before entry into the study.
Quality of life outcome measurement
Scores were derived from QoL questionnaire, by summating responses to each of the individual questions within a domain. For the modified OHIP-14 scores, each item was scored; not at all – score 1, a little – score 2, quite a lot – score 3, very much – score 4. Possible OHIP-14 scores ranged from 14 (no problems) to 56 (experienced all the problems very much). Scores 1 and 2 were considered together as little or not affected, while scores 3 and 4 were considered moderately/severely affected. The minimum score possible was 14 and maximum score was 56.
OHIP was categorized into four:
Category 1: Not at all affected (Score 14)
Category 2: A little affected (Score 15-28)
Category 3: Quite a lot affected (Score 29-42)
Category 4: Very much affected (Score 43-56).
Categories 1 and 2 were considered as “Not affected” (Score 14-28), and categories 3 and 4 considered as “Affected” (Score 29-56).
Subjects were placed on paracetamol tablets 1000 mg, 2 h after the extraction, and then 1000 mg 8 hourly for 24 h. No antibiotics were prescribed. Subjects were reviewed on postoperative day (POD) 3 and POD7. They were also instructed to report to the clinic at any other time during the postoperative period if there was any increased or persistent pain in the extraction socket.
Data analysis
Data was processed using the SPSS for Windows (version 16; SPSS Inc., Chicago, IL, USA) statistical software package. OHIP scores were computed using simple proportions and percentages. Simple frequency distribution was completed for item (question) of the measures and descriptive statistics was used to describe subjects’ responses to all items. Association between independent variables (age, sex, indications for extraction, duration of extraction, and intra-operative complications) and dependent variable (QoL) was explored using Chi-square and multiple regression analysis, and P value was set at P ≤ 0.05.
Results
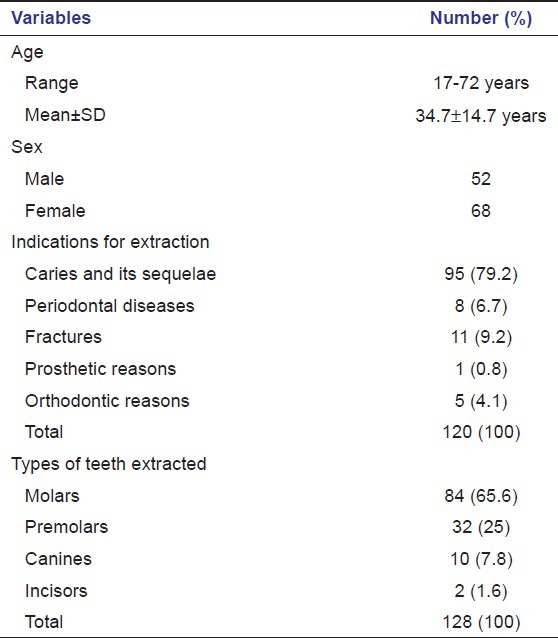
A total of 120 subjects who participated in the study and returned the questionnaires were included in the analysis. There were 52 males and 68 females with age ranged between 17 and 72 years (mean ± SD = 34.7 ± 14.7 years). The most common reasons for tooth extraction were caries and its sequelae, and these were recorded in 79% of the subjects [Table 1]. Technique of extraction in 45 subjects (37.5%) was forceps alone, elevator in 14 subjects (11.7%) and a combination of the forceps and elevator in 61 subjects (50.8%). A total of 128 teeth were extracted, and molar teeth (65.6%) were the most commonly extracted [Table 1]. Duration of extraction ranged between 1 and 3 min (mean ± SD, 1.97 ± 0.9 min). Intra-operative complications were recorded in 29 subjects (crown fracture, n = 19; root fracture, n = 9; alveolar bone fracture, n = 1). Socket healing was uneventful in 98 subjects, and in 22 subjects socket healing complications were diagnosed (dry socket, n = 6; acutely infected socket, n = 5; acutely inflamed socket, n = 11).
Table 1.
Characteristics of the subjects
Total OHIP-14 scores ranged between 14 and 48 (mean ± SD, 26.2 ± 8.3). Majority of the subjects (60%) reported “a little affected.” Only few subjects (5.8%) reported, “not at all affected,” and about 32% reported, “quite a lot” [Table 2]. Summation of OHIP-14 scores revealed that QoL was “affected” in 41 subjects (34.2%) and “not affected” in 79 subjects (65.8%) [Table 2]. Tables 3 and 4 show the percentage of subjects who reported, “affected” and “not affected” in their QoL in different domains of OHIP-14. For eating ability and diet variations, those who reported that their QoL was “not affected” were more than those who reported that their QoL was affected [Table 3]. More than 30% of subjects reported that their ability to chew, ability to open the mouth and enjoyment of food were affected following tooth extraction [Table 3]. Speech was reported to be affected by 14-34% of subjects, whereas less than 20% of subjects reported that change in their appearance was “affected.” Only few subjects (12.5-15.1%) reported, sleep and duty impairment [Table 4]. About 33% of subjects reported, “inability to work” (1-3 days) following tooth extraction [Table 4].
Table 2.
Summation oral health impact profile-14 scores in subjects who had tooth extraction
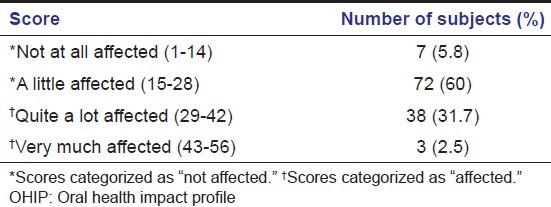
Table 3.
Eating ability/diet variation, speech variation, and physical appearance
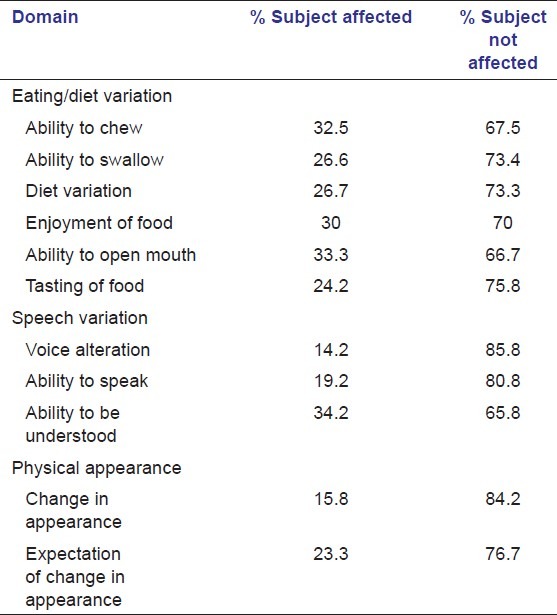
Table 4.
Sleep and duty impairment and lost days at work
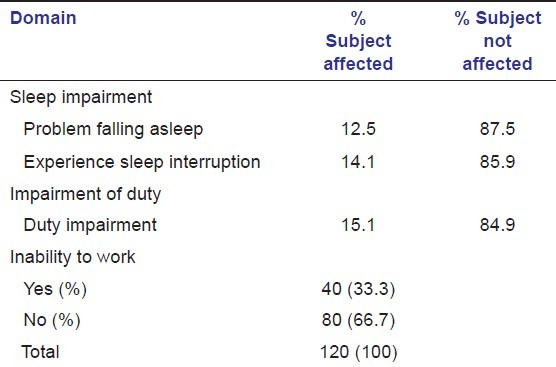
Table 5 shows a multiple regression analysis of the effect of independent variables (age and sex of subjects, intra-operative complications, duration of extraction, and socket healing complications) on QoL (dependent variable). No significantly association was found between these variables and deterioration in QoL (P > 0.05). Thirty-percent of subjects reported their inability to keep social activities during immediate postoperative period following extraction, and 41% were not able to continue with their favorite sports and hobbies during the period [Table 6]. The most common reason for social isolation was malaise and pain.
Table 5.
Multiple regression analysis of effect of independent variables on dependent variable (quality of life)
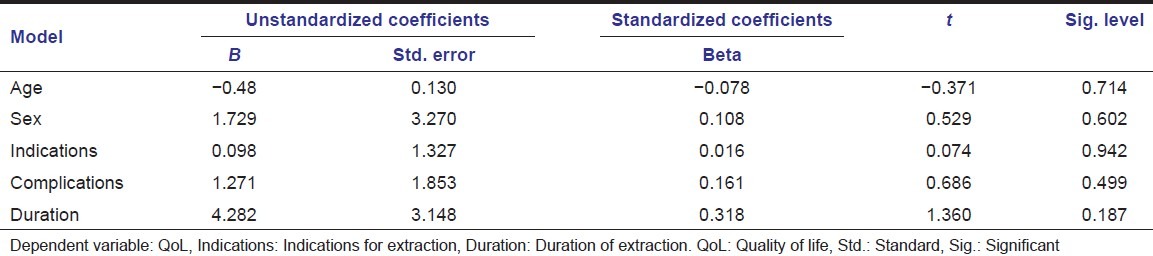
Table 6.
Subjects response to queries on social activities and favorite sports/hobbies
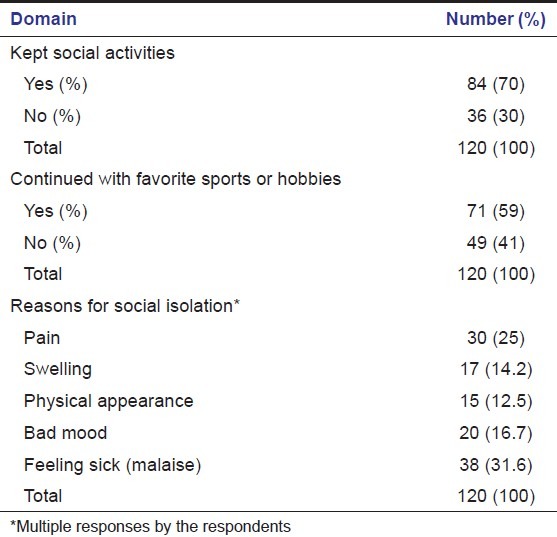
Table 7 shows pattern of pain experience following tooth extraction. Percentage number of subjects who experienced severe pain decreased from POD1 to POD7, and those who experienced no pain increased from POD1 to POD7. Prescribed analgesic regimen was adequate in 86.7% of subjects. Only 13.3% of subjects required additional analgesics beyond POD1. Consumption of analgesics beyond POD1 was more common in subjects with socket healing complications than those without (P = 0.000). About 96% of subjects were satisfied with the treatment and about 91% would recommend the treatment [Figure 1]. Although about 92% of the participants believed that the preoperative symptoms were resolved by the treatment, less than 50% of them would like to repeat the experience [Figure 1].
Table 7.
Pattern of pain experience following tooth extraction
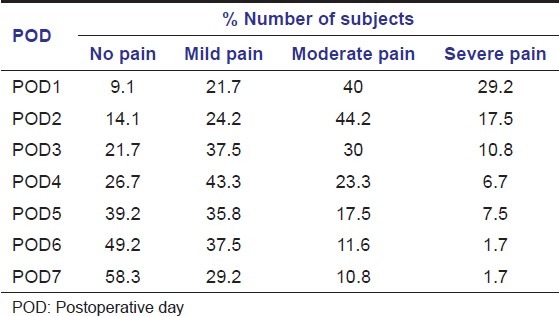
Figure 1.
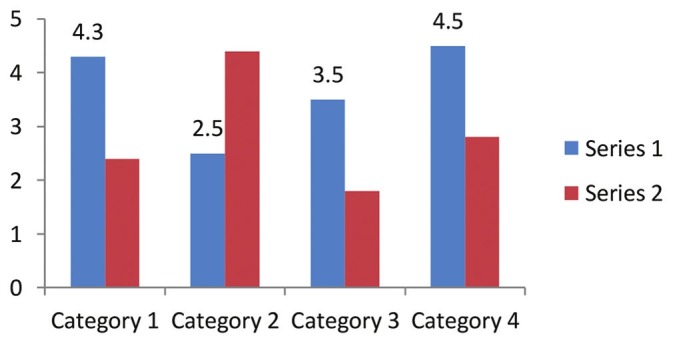
Responses to questions about the treatment
Discussion
Patients today demand more participation in their health care decisions, and require a higher level of understanding before consenting to treatment.[15] Most surgeons generally provide advice to their patients based on the surgeon's previous clinical experiences, and they rarely base such recommendations on the impact that surgery may have on the patients’ QoL.[10,13] Patients seeking dental surgeons to extract their teeth should be informed about the recovery period, potential complications, and of the possibility that their lifestyles could be negatively affected in their early postoperative days may improve satisfaction after surgery.[15]
While QoL is a term mostly used in oncology to assess social well-being and the effects of treatment upon patients with cancer in any region of the body, it has also become widely applied to other fields in health care - including dental and oral and maxillofacial surgery.[9–14] Extraction of teeth is the commonest procedure carried out in oral surgery clinics. Before consenting to surgery, patients should be informed of the risks of retention of a tooth already indicated for removal and should also be informed of risks of surgery. Today's patients demand more choice in their health care decisions and require a higher level of understanding before consenting to surgery. Patients want to know about the surgical procedure itself, possible complications and what they should expect during the post-operative period. They also want to know if they will be able to continue with their work, social activities, favorite sports or hobbies. In essence, patients are beginning to ask: How will this procedure affect my QoL?
Assessment and documentation of the physical, social and psychological consequences of surgical intervention using a well validated QoL questionnaire will afford the surgeon the opportunity to include the findings in the “written consent form” prior to surgical procedure, and therefore, prevent possible litigation. Several studies have addressed QoL especially following removal of impacted lower third molars.[9–16] To the best of our knowledge, QoL following non-surgical dental extraction has not been previously reported.
In this study, a modified 14-item OHIP was used to evaluate QoL perception by patients. The OHIP-14 is based on the World Health Organization (WHO) model of disease-impairment-disability-handicap. OHIP-14 is considered to be one of the most appropriate instruments for measuring QoL and is the most widely used means of scoring QoL, especially following lower third molar disimpaction.[9,10,16]
This study revealed that 1 out 3 subjects who had undergone non-surgical tooth extraction reported that their QoL was “affected.” However, if the preoperative QoL (not at all affected) of these subjects were taken into consideration, it can be deduced that about 94% of these subjects reported a deterioration in their QoL, though, majority of these (60%) claimed, “little affected.” These findings though not surprising, is in sharp contrast to QoL experience following third molar surgery.[9–14,16] The fact that there is no need to raise a surgical flap or to drill the bone during routine extraction may be responsible for this observation. Surgical removal of third molar is associated with inflammatory sequelae of surgery (postoperative swelling, trismus, and moderate to severe pain). Deterioration in QoL following surgical removal of third molar has been linked to the inflammatory sequelae of surgery.[10,13,16] Several pharmacological approaches to reduce these postoperative sequelae following third molar surgery have resulted in the improvement of QoL.[17–20]
The most commonly affected OHIP-14 domain following routine extraction was eating/diet variation, as about 24-32% of subjects reported that their eating/diet abilities were affected. The factors stated by the subjects necessitating dietary change were the experience of difficulty with chewing and swallowing as well as lack of enjoyment of food. Therefore, patients should be warned they may experience some level of difficulty in chewing and swallowing during immediate postoperative period following tooth extraction. Savin and Ogden[21] associated change in diet after third molar surgery with a lack of enjoyment of food, and stressed that appetizing alternatives that are ingestible without too much masticatory efforts be recommended to the patients.
Voice alteration and ability to speak and to be understood were not as affected as diet variation after tooth extraction. This maybe so because tooth extraction neither causes restriction of tongue mobility nor volume obliteration of the oral cavity, therefore, little or no interference in speech is expected. This finding is similar to that experience by patients after third molar surgery.[21] In our study, only a few subjects experienced a change in appearance. Unlike third molar surgery which is usually accompanied by postoperative swelling with subsequent change in appearance in the immediate postoperative period, routine uncomplicated dental extraction rarely causes postoperative swelling.
Sleep impairment was not a common experience among subjects who had their teeth extracted non-surgically as shown in this study. Colorado-Bonnin et al.[14] observed that sleep impairment associated with third molar extraction could result from a prolonged surgical extraction and to drowsiness induced by postoperative medication. They, therefore, advocated that patients should be warned of these side effects and the impact this would have on their ability to drive and use machines.[14]
Patients often ask the dental practitioner before tooth extraction whether the procedure will affect their ability to work. Berge[22] reported that 57% of patients who had undergone third molar surgery indicated their inability to work during the immediate postoperative period. Inability to work ranged between 1 and 6 days (mean 1.07 days).[22] In this study, impairment of duty (1-3 days) was reported by 15% of subjects. Berge[22] reported that duration of surgery more than 14 min, heavy smoking and female sex were associated with prolonged inability to work after third molar surgery. However, in our study no association was found between age and sex of subjects and inability to work.
Between 30% and 41% of subjects in the present study were not able to continue with their sporting activities and hobbies in the immediate postoperative period following non-surgical tooth extraction. Reasons for the social isolation included malaise, pain and bad mood. Therefore, patients should be warned that they may not be able to engage in their sporting activities and hobbies.
Pain is known to be a natural bodily response to noxious stimuli.[23] Pain during the immediate postoperative period after tooth extraction is an expected consequence of the surgical procedure.[6,23] However, increased or persistent pain should alert the surgeon to the possibility of socket healing complication.[6,7,23] In this study, the percentage number of subjects who experienced severe pain decreased from POD1 to POD7. Pain affects most domains of QoL, which depends on the extent, duration, acuteness, intensity, affectivity, and meaning of the pain, as well as the underlying disease and the individual's characteristics.[24] In addition, pain experience was one of the major reasons for social isolation in the studied subjects. Therefore, effective pain management may go a long way in improving QoL after non-surgical tooth extraction.
This is a finding of a pilot study; further studies on QoL in the immediate postoperative period following routine (intra-alveolar) extraction with a larger sample size are therefore encouraged.
Conclusion
About a third of subjects experienced significant deterioration in QoL. The most affected domains were eating/diet variation and speech variation. About one-third of the participants also reported lost days at work ranging between 1 and 3 days following tooth extraction. Most subjects were satisfied with the treatment, believed their symptoms were resolved by the treatment and recommend the treatment. However, less than half of them would like to repeat the experience. Therefore, patients should be informed of possible deterioration in their QoL after non-surgical extraction.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
References
- 1.Kay EJ, Blinkhorn AS. The reasons underlying the extraction of teeth in Scotland. Br Dent J. 1986;160:287–90. doi: 10.1038/sj.bdj.4805837. [DOI] [PubMed] [Google Scholar]
- 2.Angelillo IF, Nobile CG, Pavia M. Survey of reasons for extraction of permanent teeth in Italy. Community Dent Oral Epidemiol. 1996;24:336–40. doi: 10.1111/j.1600-0528.1996.tb00872.x. [DOI] [PubMed] [Google Scholar]
- 3.Murray H, Locker D, Kay EJ. Patterns of and reasons for tooth extractions in general dental practice in Ontario, Canada. Community Dent Oral Epidemiol. 1996;24:196–200. doi: 10.1111/j.1600-0528.1996.tb00841.x. [DOI] [PubMed] [Google Scholar]
- 4.McCaul LK, Jenkins WM, Kay EJ. The reasons for extraction of permanent teeth in Scotland: A 15-year follow-up study. Br Dent J. 2001;190:658–62. doi: 10.1038/sj.bdj.4801068. [DOI] [PubMed] [Google Scholar]
- 5.Aida J, Ando Y, Akhter R, Aoyama H, Masui M, Morita M. Reasons for permanent tooth extractions in Japan. J Epidemiol. 2006;16:214–9. doi: 10.2188/jea.16.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adeyemo WL, Ladeinde AL, Ogunlewe MO. Clinical evaluation of post-extraction site wound healing. J Contemp Dent Pract. 2006;7:40–9. [PubMed] [Google Scholar]
- 7.Adeyemo WL, Ladeinde AL, Ogunlewe MO. Influence of trans-operative complications on socket healing following dental extractions. J Contemp Dent Pract. 2007;8:52–9. [PubMed] [Google Scholar]
- 8.Oginni FO, Fatusi OA, Alagbe AO. A clinical evaluation of dry socket in a Nigerian teaching hospital. J Oral Maxillofac Surg. 2003;61:871–6. doi: 10.1016/s0278-2391(03)00248-9. [DOI] [PubMed] [Google Scholar]
- 9.McGrath C, Comfort MB, Lo EC, Luo Y. Changes in life quality following third molar surgery ߝ The immediate postoperative period. Br Dent J. 2003;194:265–8. doi: 10.1038/sj.bdj.4809930. [DOI] [PubMed] [Google Scholar]
- 10.McGrath C, Comfort MB, Lo EC, Luo Y. Can third molar surgery improve quality of life. A 6-month cohort study? J Oral Maxillofac Surg. 2003;61:759–63. doi: 10.1016/s0278-2391(03)00150-2. [DOI] [PubMed] [Google Scholar]
- 11.Ogden GR, Bissias E, Ruta DA, Ogston S. Quality of life following third molar removal: A patient versus professional perspective. Br Dent J. 1998;185:407–10. doi: 10.1038/sj.bdj.4809827. [DOI] [PubMed] [Google Scholar]
- 12.Conrad SM, Blakey GH, Shugars DA, Marciani RD, Phillips C, White RP., Jr Patient's perception of recovery after third molar surgery. J Oral Maxillofac Surg. 1999;57:1288–94. doi: 10.1016/s0278-2391(99)90861-3. [DOI] [PubMed] [Google Scholar]
- 13.Slade GD, Foy SP, Shugars DA, Phillips C, White RP., Jr The impact of third molar symptoms, pain, and swelling on oral health-related quality of life. J Oral Maxillofac Surg. 2004;62:1118–24. doi: 10.1016/j.joms.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 14.Colorado-Bonnin M, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Quality of life following lower third molar removal. Int J Oral Maxillofac Surg. 2006;35:343–7. doi: 10.1016/j.ijom.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Sato FR, Asprino L, de Araújo DE, de Moraes M. Short-term outcome of postoperative patient recovery perception after surgical removal of third molars. J Oral Maxillofac Surg. 2009;67:1083–91. doi: 10.1016/j.joms.2008.09.032. [DOI] [PubMed] [Google Scholar]
- 16.Negreiros RM, Biazevic MG, Jorge WA, Michel-Crosato E. Relationship between oral health-related quality of life and the position of the lower third molar: Postoperative follow-up. J Oral Maxillofac Surg. 2012;70:779–86. doi: 10.1016/j.joms.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 17.Snyder M, Shugars DA, White RP, Phillips C. Pain medication as an indicator of interference with lifestyle and oral function during recovery after third molar surgery. J Oral Maxillofac Surg. 2005;63:1130–7. doi: 10.1016/j.joms.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Tiwana PS, Foy SP, Shugars DA, Marciani RD, Conrad SM, Phillips C, et al. The impact of intravenous corticosteroids with third molar surgery in patients at high risk for delayed health-related quality of life and clinical recovery. J Oral Maxillofac Surg. 2005;63:55–62. doi: 10.1016/j.joms.2004.01.029. [DOI] [PubMed] [Google Scholar]
- 19.Majid OW, Mahmood WK. Effect of submucosal and intramuscular dexamethasone on postoperative sequelae after third molar surgery: Comparative study. Br J Oral Maxillofac Surg. 2011;49:647–52. doi: 10.1016/j.bjoms.2010.09.021. [DOI] [PubMed] [Google Scholar]
- 20.Limeres J, Sanromán JF, Tomás I, Diz P. Patient's perception of recovery after third molar surgery following postoperative treatment with moxifloxacin versus amoxicillin and clavulanic acid: A randomized, double-blind, controlled study. J Oral Maxillofac Surg. 2009;67:286–91. doi: 10.1016/j.joms.2008.06.061. [DOI] [PubMed] [Google Scholar]
- 21.Savin J, Ogden GR. Third molar surgery: A preliminary report on aspects affecting quality of life in the early postoperative period. Br J Oral Maxillofac Surg. 1997;35:246–53. doi: 10.1016/s0266-4356(97)90042-5. [DOI] [PubMed] [Google Scholar]
- 22.Berge TI. Inability to work after surgical removal of mandibular third molars. Acta Odontol Scand. 1997;55:64–9. doi: 10.3109/00016359709091944. [DOI] [PubMed] [Google Scholar]
- 23.Cheung LK, Chow LK, Tsang MH, Tung LK. An evaluation of complications following dental extractions using either sterile or clean gloves. Int J Oral Maxillofac Surg. 2001;30:550–4. doi: 10.1054/ijom.2000.0128. [DOI] [PubMed] [Google Scholar]
- 24.Niv D, Kreitler S. Pain and quality of life. Pain Pract. 2001;1:150–61. doi: 10.1046/j.1533-2500.2001.01016.x. [DOI] [PubMed] [Google Scholar]


