Abstract
Coronal fractures of the anterior teeth are a common form of dental trauma that mainly affects children and adolescents. One of the options for managing coronal tooth fractures when the tooth fragment is available and there is no or minimal violation of the biological width is the reattachment of the fragment. This article presents a novel technique for reattachment of oblique fractured fragment of vital maxillary central and lateral incisor with pulp exposure. Pulp capping was done using mineral trioxide aggregate. Orthodontic extrusion was done to expose the sub gingival fractured site. Polyethylene fiber (ribbond) and panavia F cement were used to reattach the fractured fragment using an internal groove technique to provide high fracture strength to restored tooth. Ribbond fibers can be used to give additional strength to the reattached tooth fragment so that the tooth obtains fracture resistance equal to an intact tooth.
Keywords: Panavia F, ribbond, tooth fragment re-attachment, vital tooth
Introduction
Coronal fractures of the anterior teeth are a common form of dental trauma that mainly affects children and adolescents.[1] The majority of dental injuries involves the anterior teeth, especially the maxillary central incisors (because of its position in the arch), whereas the mandibular central incisors and the maxillary lateral incisors are less frequently involved.[2]
Enamel/dentin fractures, with or without pulp exposure and with invasion of biological width, are exceptionally challenging. The clinician has to determine whether to maintain the exposed vital pulp, employing a conservative treatment, or to sacrifice the pulp and perform the endodontic treatment.[3]
Although direct pulp capping with adhesive systems is a controversial technique, reports exist of successful clinical cases with direct adhesive restorations on vital teeth, where the pulp had been exposed for several days.[4] This article discusses the reattachment of the tooth fragments to the fractured maxillary central and lateral incisor with pulp exposure using a novel technique.
Case Report
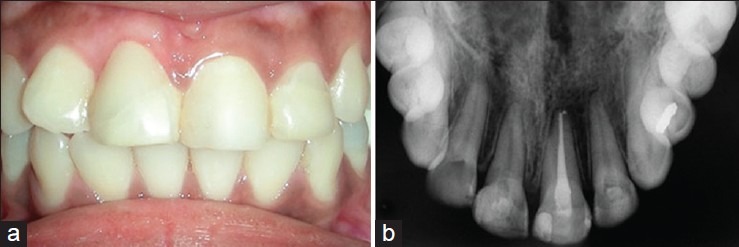
A 16-year-old female patient reported to the Department of Conservative Dentistry and Endodontics with a history of an automobile accident and injury to the upper front teeth. The patient had reported to the department within half an hour after injury. Initial examination revealed an oblique fracture on permanent maxillary right central incisor (MRCI) and permanent maxillary left lateral incisor (MLLI) involving three-fourths of the clinical crown with associated exposure of the pulp [Figure 1a]. Diagnosis of Ellis's class 3 fractures on both tooth were made. Maxillary left central incisor (MLCI) had a 3-year-old composite restoration. On clinical examination, the fracture line extended from labial to lingual in an apical direction. Radiographic examination revealed an oblique fracture with MRCI and MLLI [Figure 1b]. While MRCI exhibited fracture line extending 2 mm above the bony crest, the MLCI exhibited some periapical changes. The treatment options presented to the patient and to her legal guardians were: (1) Crown build-up restoration with a resin based composite, (2) reattachment of the tooth fragment (3) root canal therapy, post and core and lastly, the least desired (4) extraction. After some deliberation about the advantages, disadvantages, prognosis, and cost of each treatment option, the patient opted to have the tooth fragment reattached. It is important to note that the reattachment option was presented only after confirming that the fragment was in good condition and that it fit reasonably well on the fractured tooth.
Figure 1.
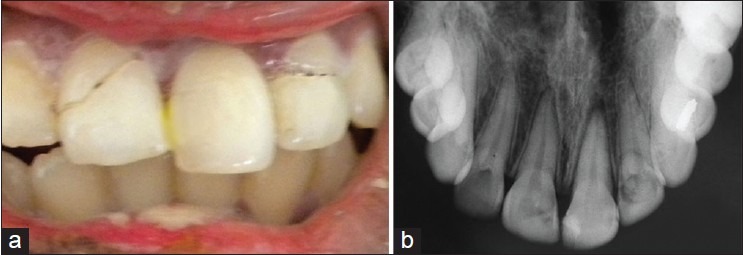
(a) Pre‑operative photograph and (b) Radiograph
The fragments of MRCI and MLLI were still attached by a soft-tissue junction at the palatal aspect [Figure 1a]. After local anesthesia, the coronal fragments were separated with minimum force [Figure 2a and b] and was stored in saline to prevent dehydration. Since the pulpal exposure was fresh, the exposed site was disinfected with chlorhexidine and saline and direct pulp capping was done with mineral trioxide aggregate (MTA) (Dentsply, Tulsa Dental, Tulsa, OK, USA) [Figure 3a and b]. Glass ionomer cement (Fuji IX GC Corporation Tokyo, Japan) was placed as the final restoration. After 2 weeks orthodontic extrusion was planned with MRCI to expose the fractured site supragingivally, using a custom-made appliance [Figure 4]. Vitality test was performed to check for the vitality of the teeth after 6 weeks. Both MRCI and MLLI tested positive for vitality, but MLCI showed delayed response. The procedure of reattachment of fragment was carried out.
Figure 2.
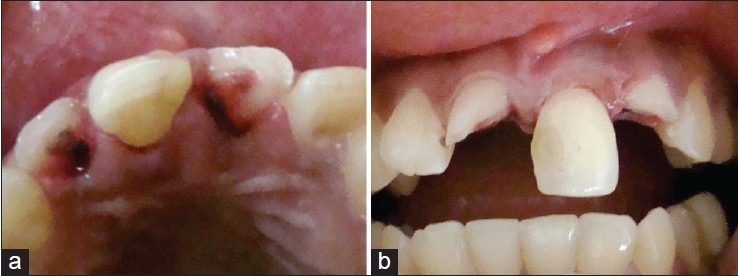
(a) Palatal view after separation of fragment. (b) Anterior view after fragment separation
Figure 3.
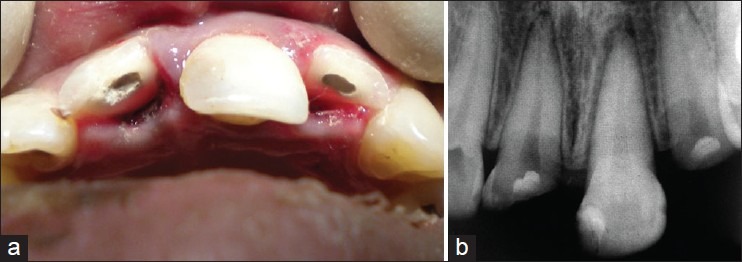
(a) Photograph and (b) Radiograph after pulp capping with mineral trioxide aggregate
Figure 4.

Customized appliance in place for orthodontic extrusion
The pulp chamber of the respective fragments (MRCI and MLLI), which were stored in saline and anti-fungal agent thymol for 8 weeks, were debrided of pulp and a groove was made with a long flat ended tapered fissure bur to act as a retentive area (Mani, Japan) [Figure 5a]. Etching (37% phosphoric acid gel, Prime Dent, New Delhi, India) and bonding (Bond I, Pentron Technologies LLC, Wallingford, CT, US) of the MRCI and MLLI and the respective fragments were done. A small pre-measured piece (2 mm) of ribbond (Ribbond Inc., Seattle, WA, USA) was selected, bonding agent applied (Bond I, Pentron Technologies LLC) and cured for 20 s. The ribbond was placed vertically in the groove prepared in the fractured fragments along with panavia F dual cure cement (Kuraray, Osaka, Japan) [Figure 5b]. The fragments were then verified for a fit with the teeth surface to ensure proper adaptation. Excess cement was removed and light cured from both buccal and palatal side.
Figure 5.
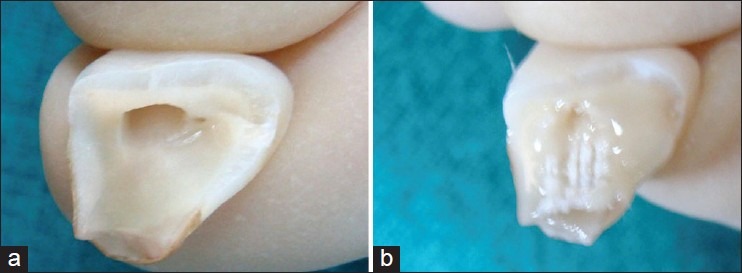
(a) Tooth fragment after pulp debridement and groove preparation. (b) Ribbond placement vertically in the groove along with panavia F dual cure cement
The occlusion was carefully adjusted and the patient was instructed to avoid exerting heavy function on the reattached teeth. Patient was recalled after 6 months, vitality test was done with electric and cold test. The MRCI and MLLI responded positively but MLCI showed no response. Root canal therapy was done with MLCI. An 18-month recall showed good esthetics and function of the reattached teeth and vitality of both MRCI and MLLI was confirmed [Figure 6a and b].
Figure 6.
(a, b) An 18‑month recall photograph and radiograph of maxillary right central incisor and maxillary left lateral incisor
Discussion
One of the options for managing the coronal tooth fractures, especially when there is no or minimal violation of the biological width, is the reattachment of the dental fragment when it is available.[5] The availability of the fragment does not necessarily indicate that the reattachment to the tooth remnant is indicated. To perform the reattachment with a predictable prognosis, several requisites must be achieved.
The fragment must be adaptable to the remaining tooth, the fragment and the remaining tooth must demonstrate color compatibility and dental composition to prevent aesthetic compromise.[3]
In the present case, the fragment fulfilled all the criteria mentioned above. Presence of pulp exposure is another decisive factor. The case presented had fresh pulpal exposure and thus teeth were immediately disinfected and capped with MTA and final restoration was done with glass ionomer cement.
In the present situation, the subgingival location of the fracture line could not allow an optimal sealing besides oral hygiene could have been difficult to maintain. In such a case, two main factors must be addressed:
The fracture margin access and the possibility of performing a tight seal restoration.[6]
An orthodontic extrusion of fractured tooth will maintain the periodontal tissues at the same level and restore a physiological attachment. A 3-4 mm distance from the alveolar crest to the coronal extension of the remaining tooth structure has been recommended for optimal periodontal health.[7] In our case, a custom-made appliance was fabricated for the patient and the forced eruption was limited to 3 mm (maximum 5 mm as suggested by Ingle)[8] and was achieved with minimal force (Only 0.2-0.3 N).[9]
Various clinicians have employed an assortment of bevel designs, chamfers, dentinal and enamel grooves, and choices of resin composite materials and techniques for the reattachment of tooth fragments. In the present case report, an internal groove was placed in the fractured fragment using a flat ended tapered fissure bur, to provide space for placement of ribbond and panavia F cement. This technique provides high fracture strength to the restored tooth due to the incorporation of ribbond fibers. Further studies are required to assess the amount of increase in fracture resistance.
Panavia F has modulus of elasticity same as that of dentin. It has been demonstrated that elastic modulus is one of the important parameters to evaluate property of the cements. When cement with an elastic modulus close to the dentin was selected, optimal combination and mechanical compatibility of the cement and dentin could be achieved; this enhanced the ability to resist external force together. Stress in dentin was reduced due to the cement sharing parts of the stress.[10]
In the present case, surface area for retention for the fiber was provided by groove preparation on the fragment and by the concavity of the pulp chamber on the tooth side. The use of natural tooth substance clearly eliminated problems of differential wear of restorative material, unmatched shades and difficulty of contour and texture reproduction associated with other restorative techniques.[1] An 18-month recall showed good esthetic and function of the reattached teeth, vitality of both MRCI and MLLI was retained. The patient would be observed for the success of the material and technique used for reattachment procedure during recall visits.
Conclusion
The present case reports a novel method of using ribbond fibers to strengthen the fractured fragments and the multidisciplinary management of dental trauma that leads to conservation of the tooth.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
References
- 1.Dietschi D, Jacoby T, Dietschi JM, Schatz JP. Treatment of traumatic injuries in the front teeth: Restorative aspects in crown fractures. Pract Periodontics Aesthet Dent. 2000;12:751–8. [PubMed] [Google Scholar]
- 2.Andreasen JO, Andreasen F, Andersson L. In: Textbook and Color Atlas of Traumatic Injuries to the Teeth. 4th ed. Oxford, Blackwell; 2007. Classification Epidemiology Etiology; pp. 227–44. [Google Scholar]
- 3.Terry DA. Adhesive reattachment of a tooth fragment: The biological restoration. Pract Proced Aesthet Dent. 2003;15:403–9. [PubMed] [Google Scholar]
- 4.Baratieri LN, Ritter AV, Monteiro Júnior S, de Mello Filho JC. Tooth fragment reattachment: An alternative for restoration of fractured anterior teeth. Pract Periodontics Aesthet Dent. 1998;10:115–25. [PubMed] [Google Scholar]
- 5.Baratieri LN, Monteiro S, Jr, Andrada MAC. Tooth fracture reattachment; case reports. Qintessence Int. 1990;21:261–70. [PubMed] [Google Scholar]
- 6.Kocadereli I, Taºman F, Güner SB. Combined endodontic-orthodontic and prosthodontic treatment of fractured teeth. Case report. Aust Dent J. 1998;43:28–31. doi: 10.1111/j.1834-7819.1998.tb00148.x. [DOI] [PubMed] [Google Scholar]
- 7.Ingle JI, Bakland LK. In. Endodontics. 5th ed. Ontario Canada: BC Decker Inc; 2006. Endodontic considerations in dental trauma; pp. 804–11. [Google Scholar]
- 8.Vitale MC, Caprioglio C, Martignone A, Marchesi U, Botticelli AR. Combined technique with polyethylene fibers and composite resins in restoration of traumatized anterior teeth. Dent Traumatol. 2004;20:172–7. doi: 10.1111/j.1600-4469.2004.00201.x. [DOI] [PubMed] [Google Scholar]
- 9.Reis A, Francci C, Loguercio AD, Carrilho MR, Rodriques Filho LE. Re-attachment of anterior fractured teeth: Fracture strength using different techniques. Oper Dent. 2001;26:287–94. [PubMed] [Google Scholar]
- 10.Diangelis AJ, Jungbluth M. Reattaching fractured tooth segments: An esthetic alternative. J Am Dent Assoc. 1992;123:58–63. doi: 10.14219/jada.archive.1992.0222. [DOI] [PubMed] [Google Scholar]


