Abstract
Aim:
This prospective randomized clinical study (1) investigated the prevalence of post-obturation pain after single visit root canal treatment and (2) evaluated the influence of factors affecting the pain experience.
Materials and Methods:
One thousand three hundred and twenty eight (1328) patients were included in this study. Conventional single visit root canal treatment was carried out. The chemicomechanical preparation of root canals was done by a rotary protaper system with a combination of hand instruments. Post-operative pain was recorded by each patient by using visual analogue scale in well-defined categories at three time intervals, 12 h, 24 h, and 48 h. The data were analyzed using Fisher's exact test.
Results:
The prevalence of post-obturation pain (severe) within 48 h after treatment was 4% (n = 54) but less as compared to the pain experienced after 12 h (9%) and 24 h (8.6%). The factors that significantly influenced post-obturation pain experience were: Age (Fishers exact test = 46.387, P = 0.0), gender (Fishers exact test = 23.730, P = 0.0), arch (Fishers exact test = 11.710, P = 0.001), and presence of pre-operative pain (Fishers exact test = 67.456, P = 0.0).
Conclusion:
The presence of post-operative pain was low (4%). The important prognostic determinants of post-obturation pain were: Old age, female, mandibular teeth, and presence of pre-operative pain. The vital condition of the tooth does not affect the intensity and frequency of post-obturation pain.
Keywords: Molars, postoperative pain, single visit root canal treatment
Introduction
The basic principles of root canal treatment are the eradication of root canal irritant, obturation of the root canal system and preservation of the natural dentition. The root canal procedure can be done in single visit or multiple visits.[1] Traditionally root canal treatment was performed in multiple visits, with medication between root canal preparation and obturation, which mainly aims to reduce or eliminate microorganisms and their by-products from the root canal system before obturation. However, with various advances in endodontics, single visit root canal treatment is commonly performed.
However, despite advances in endodontic therapy, studies have shown that pain frequency and intensity vary after root canal treatment. There is no consistency in the literature, the frequency of postoperative pain is mentioned to be lower in single visit or multiple visits or to have similar results.[2]
Post-operative pain after endodontic procedures is an undesirable occurrence for both patients and clinicians.[3] Pain affects patient's quality of life and the success of dentist patient relationship.[2] Patients might consider post-operative pain as a benchmark against which the clinician's skills are measured. It might undermine patient's confidence in their dentist or patient satisfaction with their treatment.[1] The occurrence of mild pain is relatively common even when the treatment has followed the highest standards and should be expected and anticipated by patients.[3]
Numerous studies with post-operative pain after root canal treatment have been published, with the incidence of post-operative pain ranging from 1.9% to 48%, and they showed conflicting findings.[1] Pain associated with root canal therapy is a poor indicator of pathosis and an even more unreliable predictor of long-term success.[4]
Prospective, randomized studies are generally believed to provide the highest level of support for evidence-based clinical practice. Thus, a prospective, randomized study was carried out to evaluate the incidence and severity of post-operative pain following single sitting root canal therapy in Indian population. The relationship of certain factors (age, gender, pulpal status, arch, and presence of pre-operative pain) with post-operative pain was also analyzed.
Materials and Methods
One thousand three hundred and twenty eight patients were included in the study. Of the 1328 patients, 593 (44.7%) were women and 735 (55.3%) were men. Of all the teeth 1097 (82.6%) were vital and 231 (17.4%) teeth were non-vital. Age range was 15-65 years. 606 (45.6%) treated teeth were in the maxilla and 722 (54.4%) teeth were in the mandible. All the teeth were molars, either first molar (783) or second molar (545). Single sitting root canal therapy was explained to the patient and oral and written informed consent was obtained.
Patients who were pregnant, need retreatment, having complications during treatment (calcification, impossibility to achieve apical patency), taking antibiotics or steroids at the time of treatment, immuno-compromised or under 15-year-old were excluded from this study.
Treatment procedure
Conventional RCT was carried out in single visit. After adequate anesthesia, rubber dam was applied and access opening was done. The working length of each canal was determined by an electronic apex locator and 2 or more angled radiographs. Canals were prepared with a combination of hand files (K file, Mani, Japan) and rotary protaper system (Dentsply Maillefer, Ballalgues, Switzerland) by using RC Prep (Premier Dental Product Co. King of Prussia, PA, USA). Intermittent copious irrigation was done with 5.25% sodium hypochlorite solution. The canals were obturated with protaper gutta percha points (Dentsply Maillefer) using AH plus sealer (Dentsply, Konstanz, Germany). Temporary restoration with cavit (ESPE, Germany) was given for 2 weeks. Then the post-obturation restoration was done with amalgam to maintain a good coronal seal.
Post-operative pain was measured by using a visual analogue scale (VAS) of 0 (no symptom) to 3 (severe pain and/or swelling). VAS was taught to the participants as well as reporting the post-operative pain after 12 h, 24 h, and 48 h. Patients were contacted by telephone if they did not return the VAS form. The post-operative evaluation was recorded as 0 (no pain), 1 (slight pain/discomfort), 2 (moderate pain relived by analgesics) and 3 (severe pain/swelling not relieved by analgesics and required unscheduled visit). All patients were given a prescription for 50 mg of diclofenac potassium, with the dose of 1 tablet every 8 h taken only if they experienced moderate pain.
Results were statistically analyzed using Fishers exact test. Differences were considered significant when the probabilities were equal to or less than 0.05.
Results
Results are shown in Tables 1-6: The overall incidence of post-operative pain after RCT during the follow-up period of 12 h, 24 h, and 48 h was assessed according to patient's record in the VAS [Table 1]. 1190 (89.6%) patients had no pain, 14 (1.1%) patients had mild pain, 5 (0.4%) patients had moderate pain, and 119 (9.0%) patients experienced severe pain after 12 h. After 48 h the number of patients with severe pain was drastically reduced to 54 (4%), and there was no patient with mild pain, and only 1 (0.1%) patient with moderate pain.
Table 1.
Overall incidence of post-operative pain after 12 h, 24 h, and 48 h
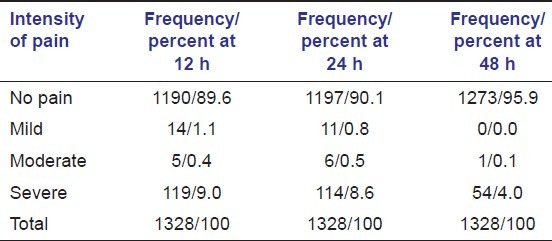
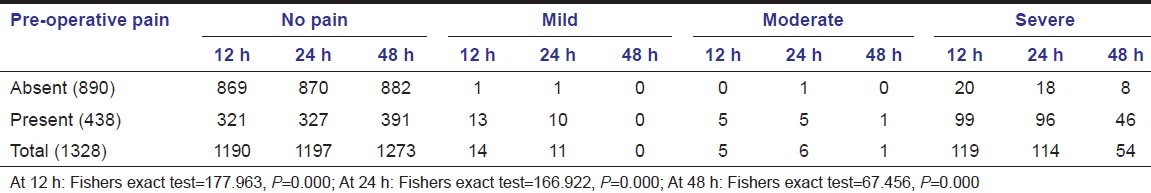
Table 6.
Incidence of post-operative pain in relation to the pre-operative pain at 12 h, 24 h, and 48 h
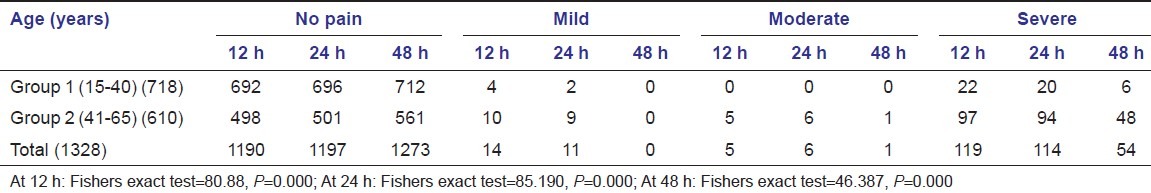
Post-operative pain related to the age: Differences were statistically significant (P = 0.0) between both the groups. Incidence of post-operative pain is high in group 2 (41-65 years) at all the three-time intervals [Table 2].
Table 2.
Incidence of post-operative pain in relation to age at 12 h, 24 h and 48 h
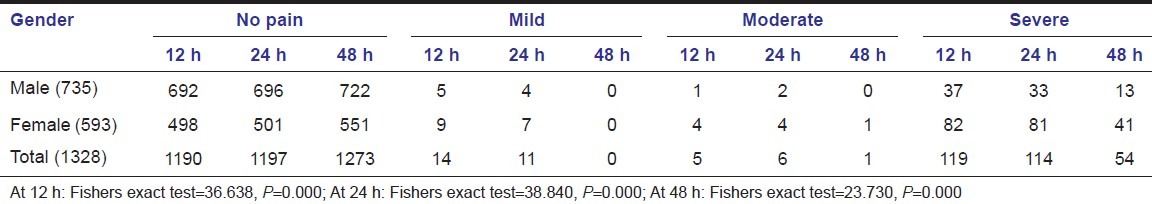
Post-operative pain related to the gender: Statistically significant (P = 0.0) difference was present between both the genders. More number of women experienced severe pain as compared to men, at all the three-time intervals [Table 3].
Table 3.
Incidence of post-operative pain in relation to gender at 12 h, 24 h, and 48 h
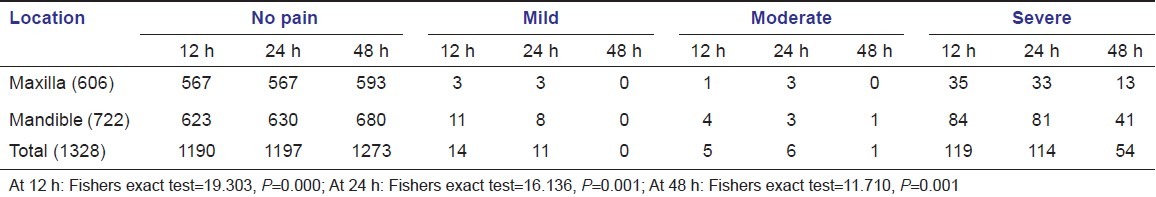
Post-operative pain related to the arch: In lower teeth post-operative pain was significantly higher (P = 0.001) at all the three time intervals [Table 4].
Table 4.
Incidence of post-operative pain in relation to arch at 12 h, 24 h, and 48 h
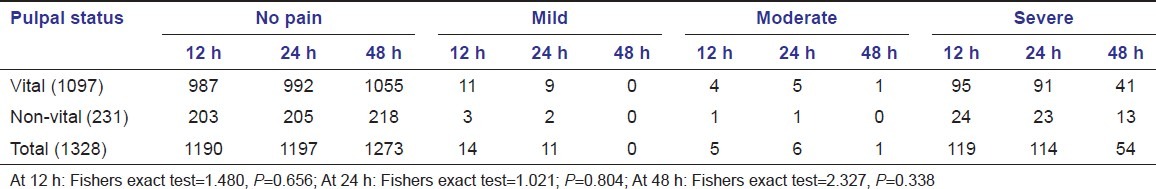
Post-operative pain related to the vital status of the tooth: There was no statistically significant difference (P = 0.338) in post-operative pain, between both the groups at all the three time intervals [Table 5].
Table 5.
Incidence of post-operative pain in relation to the vitality at 12 h, 24 h, and 48 h
Post-operative pain related to the pre-operative pain: In cases with reported presence of pre-operative pain, the presence of post-operative pain was significantly more (P = 0.0) [Table 6].
Discussion
One of the main problems in studying pain is the patient's subjective evaluation and its measurement. For this reason, design of the questionnaire is critical and must ensure that it will be fully understood by patients and easily interpreted by researchers.[5]
In this report, a simple verbal categorization was used in the feedback form with 4 categories: 0 - no pain, 1 - mild pain, 2 - moderate pain, and 3 - severe pain. These categories were easily understood by the patients.
It is well known that pain perception is a highly subjective and variable experience modulated by multiple physical and psychological factors.[4] Postobturation pain is considered to be related with several factors, including pre-operative pain, infection, retreatment, intracanal medications, and physical and chemical damage to periapical tissue. The lower incidence of post-operative pain in single visit root canal treatment might be attributed to immediate obturation, thereby to avoid passage of medications, repeated instrumentation and irrigation.
The reported prevalence of post obturation pain ranges widely from 0% (at 30 days) to 65% (at 1 day), generally declines over time and should therefore be qualified by duration after last treatment episode.[6]
In this investigation, overall incidence of post-operative (severe) pain in RCT was 9% after 12 h, which was reduced to 8.6% after 24 h and drastically to 4% after 48 h. Thus, under sound biological principles and by using contemporary scientifically based techniques, a low incidence of post-operative pain can be expected.[1] The pain was more frequent during the first 24 h of the observation period and quickly decreased thereafter. These findings were in agreement with those of some authors.[2,7–11]
In this study, five variables (age, gender, arch, vitality, and presence of pre-operative pain) were considered separately to explore the potential influence on the prevalence of post-obturation pain. Except for one variable (i.e., vital status of the tooth), the remaining four variables were significantly associated with presence of post-obturation pain.
Prevalence of post-operative pain is significantly higher (P = 0.0) in old patients (7.8%) as compared to young patients (0.8%), at all the three time intervals. This may be because of less pain tolerance, less blood flow and delayed healing.
The prevalence of post-operative pain is very high in women (7.4%) as compared to men (1.8%) (P0 = 0.0). This finding is in agreement with Ryan et al.,[12] who presented gender (women) as a factor that significantly influenced post-operative pain. Various hypotheses have been proposed to explain women predominance in pain prevalence. A more legitimate explanation is based on emerging evidence that biological differences between genders may explain increased pain prevalence in women. There are two possible explanations:[6]
Differences in pelvic and reproductive organs may provide an additional portal of entry of infection in females leading to possible local and distant hyperalgesia.
Fluctuating female hormonal levels may be associated with changing levels of serotonin and noradrenaline leading to increased pain prevalence during the menstrual period and in women receiving hormonal replacement therapy or oral contraceptives.
In mandibular molars post-obturation pain is significantly higher (6%) as compared to maxillary molars (2.2%) (P = 0.001). This might be because mandible has a dense trabeculae pattern, thus there is reduced blood flow and more localization of infection and inflammation, which might lead to delay healing. Analysis of post-obturation pain shows no statistically significant difference between vital (3.7%) and non-vital teeth (5.6%) (P = 0.338). This finding is in agreement with DiRenzo et al.,[4] Harrison et al.,[10] and Roane et al.[13]
In cases with presence of pre-operative pain, frequency, and degree of postoperative pain were significantly more (P = 0.0) (10.5%) as compared to patients with absence of pre-operative pain (0.9%). This finding is in agreement with ElMubarak et al.,[1] and Siqueira et al.[3] This finding could be explained by the presence of infection of the root canal system and periapical region pre-operatively. This tissue being initially irritated may become secondarily irritated during treatment.[2]
Conclusion
Thus, within the limitation of this study, it is concluded that post-obturation pain is likely to occur in first 24 h which further reduces as time passes. Thus, it is a strong indication that clinician should not overreact to early post-obturation pain by immediately initiating endodontic retreatment procedures or extraction of the involved tooth.
Analysis of the influence of patient's age, gender, arch, vitality of the tooth, and presence of pre-operative pain, on prevalence of the post-operative pain showed that it is higher in the old age group (group 2: 41-65 years), women, mandibular teeth, and with presence of pre-operative pain. The vital condition of the tooth does not affect the intensity and frequency of post-obturation pain. Other factors reported to be significantly related to post-obturation pain such as apical periodontitis, retreatment, irrigating solution, intracanal medicament, tooth positions were not analyzed in this study.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
References
- 1.El Mubarak AH, Abu-bakr NH, Ibrahim YE. Post-operative pain in multiple-visit and single-visit root canal treatment. J Endod. 2010;36:36–9. doi: 10.1016/j.joen.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 2.Risso PA, Cunha AJ, Araujo MC, Luiz RR. Postobturation pain and associated factors in adolescent patients undergoing one- and two-visit root canal treatment. J Dent. 2008;36:928–34. doi: 10.1016/j.jdent.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Siqueira JF, Jr, Rôças IN, Favieri A, Machado AG, Gahyva SM, Oliveira JC, et al. Incidence of Post-operative pain after intracanal procedures based on an antimicrobial strategy. J Endod. 2002;28:457–60. doi: 10.1097/00004770-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 4.DiRenzo A, Gresla T, Johnson BR, Rogers M, Tucker D, BeGole EA. Post-operative pain after 1- and 2-visit root canal therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:605–10. doi: 10.1067/moe.2002.121900. [DOI] [PubMed] [Google Scholar]
- 5.Arias A, Azabal M, Hidalgo JJ, de la Macorra JC. Relationship between postendodontic pain, tooth diagnostic factors, and apical patency. J Endod. 2009;35:189–92. doi: 10.1016/j.joen.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Ng YL, Glennon JP, Setchell DJ, Gulabivala K. Prevalence of and factors affecting post-obturation pain in patients undergoing root canal treatment. Int Endod J. 2004;37:381–91. doi: 10.1111/j.1365-2591.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- 7.Albashaireh ZS, Alnegrish AS. Postobturation pain after single- and multiple-visit endodontic therapy. A prospective study. J Dent. 1998;26:227–32. doi: 10.1016/s0300-5712(97)00006-7. [DOI] [PubMed] [Google Scholar]
- 8.Al-Negrish AR, Habahbeh R. Flare up rate related to root canal treatment of asymptomatic pulpally necrotic central incisor teeth in patients attending a military hospital. J Dent. 2006;34:635–40. doi: 10.1016/j.jdent.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 9.Yesilsoy C, Koren LZ, Morse DR, Rankow H, Bolanos OR, Furst ML. Quintessence Int. 1988. Post-endodontic obturation pain: A comparative evaluation; pp. 431–8. [PubMed] [Google Scholar]
- 10.Harrison JW, Baumgartner JC, Svec TA. Incidence of pain associated with clinical factors during and after root canal therapy. Part 2. Postobturation pain. J Endod. 1983;9:434–8. doi: 10.1016/S0099-2399(83)80259-3. [DOI] [PubMed] [Google Scholar]
- 11.Fox J, Atkinson JS, Dinin AP, Greenfield E, Hechtman E, Reeman CA, et al. Incidence of pain following one-visit endodontic treatment. Oral Surg Oral Med Oral Pathol. 1970;30:123–30. doi: 10.1016/0030-4220(70)90021-6. [DOI] [PubMed] [Google Scholar]
- 12.Ryan JL, Jureidini B, Hodges JS, Baisden M, Swift JQ, Bowles WR. Gender differences in analgesia for endodontic pain. J Endod. 2008;34:552–6. doi: 10.1016/j.joen.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 13.Roane JB, Dryden JA, Grimes EW. Incidence of Post-operative pain after single- and multiple-visit endodontic procedures. Oral Surg Oral Med Oral Pathol. 1983;55:68–72. doi: 10.1016/0030-4220(83)90308-0. [DOI] [PubMed] [Google Scholar]


