Abstract
Objectives:
The aim of this study was to observe the tooth loss over age in a sample of Brazilian patients and analyze their ability to chew, relating it to how much is the loss of oral function impact over the quality of life (QoL).
Materials and Methods:
This is a single center, observational study and the data were collected through clinical examination followed of questionnaires to obtain sociodemographic information, the ability to chew (through the index of chewing ability [ICA]) and QoL (through Oral Health Impact Profile, OHIP-14).
Results:
The sample was composed by 171 random volunteers with mean age of 47 (SD 15.2). Low number of natural teeth was associated with an increase of age (Spearman's rho correlation coefficient-0.7, P < 0.001, 2-tailed) and chew disability (ICA: chew's ability vs. disability) (Mann-Whitney U-Test, P < 0.001). Chew disability showed a negative impact over the QoL (overall OHIP; Mann-Whitney U Test P < 0.001) and in five of seven OHIP domains (Functional Limitation, Physical Pain, Psychological Discomfort, Physical Disability, Psychological Disability). Age over than 40 years, was also associated with chewing disability (Pearson Chi-Square P < 0.001) and poorer QoL (Mann-Whitney U test P = 0.01).
Conclusion:
This study observed that the chewing disability produces a significant and negative impact over oral-health related QoL and both, poor QoL and chewing disability are related with the decrease of the number of natural teeth.
Keywords: Chew's ability, oral health impact profile-14, oral health-related quality of life, quality of life, tooth loss
Introduction
The World Health Organization (WHO)[1] has defined quality of life (QoL) as “an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.” It is increasingly recognized that clinical indicators only are not sufficient to describe health status and this is also true for oral diseases. Therefore, models and measures have been developed to assess the impact of oral disease on QoL.[2–4]
Tooth loss implies in loss of several orofacial structures, such as bone tissues, nerves, receptors and muscles and consequently, most orofacial functions are diminished. Studies have indicated that the decrease of number of teeth and for complete denture wearers the chew's ability is significantly less efficient and this may have consequences over general health and QoL of those patients. The negative impact on oral health-related quality of life (OHRQoL) may also be due to poor speech, pain, and dissatisfaction with appearance.[4–7]
The aim of this study was to observe the tooth loss over age in a sample of low income Brazilian patients and analyze their ability to chew, relating it to how much is the loss of oral function impact over OHRQoL.
Materials and Methods
This is a single center observational study. It was submitted and approved in the University Ethical Committee for Human Research and all participants signed an informed consent form before information collection. The data were collected between June 2010 and June 2011.
Clinical questionnaire and clinical examination
The questionnaire included questions to obtain basic socio demographic information (gender, age, working activity, etc.), habits and the oral clinical condition. The socio demographic questions were applied by the researcher and answered by the subject. The clinical examination was performed by trained and calibrated dental students enrolled in the study and it was performed in consulting room with potent illumination and under direct supervision by the principal researcher, who could resolve any doubts. Dental mouth mirror and dental and periodontal probe were used. Additional X-ray image was taken whenever necessary.
A natural teeth were defined as a tooth with the ability to chew or functional with or without dental restoration (amalgam or composite), but teeth with a fixed prosthesis or dental implants were not considered. Exodontia indicated was defined as the situation, where the tooth cannot be recovered due to any condition and exclude intact third molars surgeries.
Chew's ability
The ability to chew was measured by the index of chewing ability (ICA) developed by Leake (1990).[8] The ICA is a very simple, five-item yes/no questions based in the ability of chew foods like, boiled vegetables, salads, raw carrots/celery, steaks or chops and fresh apples, in a crescent difficulty to chew. The answers generate a 0-5 index-score (no = 0 and yes = 1), meaning that if you are able to chew all the five items you have a competent ability to chew and a single “no” put you in the disability group. So, to conduct the analysis the responders were assigned to one of two categories: (a) those with chewing competence, scoring 5 on the index and; (b) those deficient in chewing ability, scoring 0-4 on the index.
Oral Health Impact Profile-14
The Oral Health Impact Profile (OHIP) was developed by Slade and Spencer[2] and later a shortened version of the OHIP was validated (OHIP-14).[3] The Portuguese version of the OHIP-14, was adapted to the Brazilian-Portuguese language and culture by Almeida et al.[9] The questionnaire was conceived to measure how different oral conditions affect QoL in an overall sense. It is organized into 14 questions or items distributed into seven conceptual impact dimensions (two items within each of the seven dimensions): “functional limitations,” “physical pain,” “psychological discomfort,” “physical disability,” “psychological disability,” “social disability,” and “handicap.” The answers were assessed using a Likert type evaluation scale with 5 points: never = 0; rarely = 1; sometimes = 2; repeatedly = 3; always = 4. The impact over the QoL can be measurable through sum of the ordinal values of the 14 items and/or summoning the two items within each of the seven dimensions. Higher scores indicate a worse OHRQoL state.
Results
The sample was composed by 171 random volunteers that searched dental treatment in the Dental School of Oeste de Santa Catarina University (Brazil). Female patient comprised 54.4% (93) of the sample. Mean age was 47 (SD 15.2). The sample was composed by low-income families and daily activities most cited were housekeeping, small propriety farming, bricklayer's mate and general services.
Periodontal disease was present in 39 (22.8%) patients, while active tooth decay was observed in 67 (39.2%) subjects and 36 (21.1%) patients had, at least, one tooth with exodontia indicated. The number of natural teeth in the mouth ranged from 0 to 32, mean of 13.3 (SD 10.6). The mean number of natural teeth in mouth according to the age group (in years-y) observed was: 16-20 (y), 27.1; 21-30 (y), 24.2; 31-40 (y), 21.5; 41-50 (y), 12.5; 51-60 (y), 10.4; 61-70 (y), 3.6; 71 (y) or more.,1 [Figure 1]. Table 1 describes the clinical situation and functionality of the maxilla and mandible.
Figure 1.
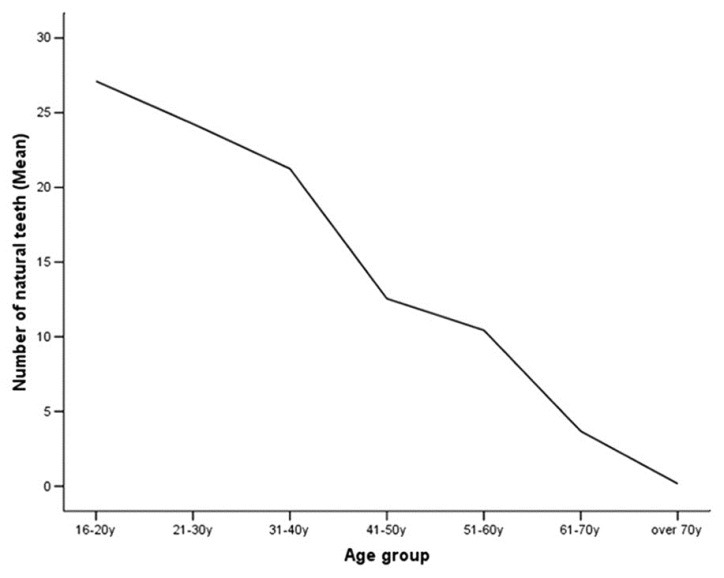
Graph showing the gradual and constant (mean) decrease of natural teeth in mouth according to age group (years)
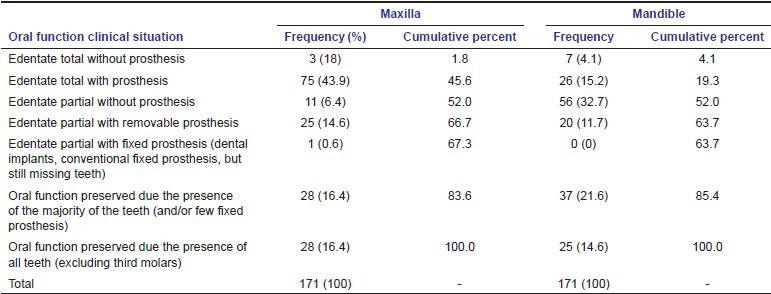
Table 1.
Clinical situation and functionality of the maxilla and mandible
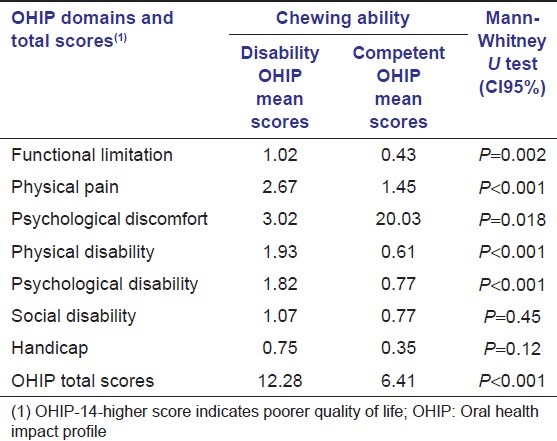
The results about QoL and chew's ability evaluated by the ICA and OHIP-14 can be viewed in Tables 2 and 3 respectively. Chew disability showed a negative impact over the QoL (overall OHIP) and in five of seven OHIP domains. The impact of ICA over the QoL can be viewed in Table 4.
Table 2.
Distribution of the chewing ability index (ICA) and the characterization of its scores into chewing competence and chewing disability
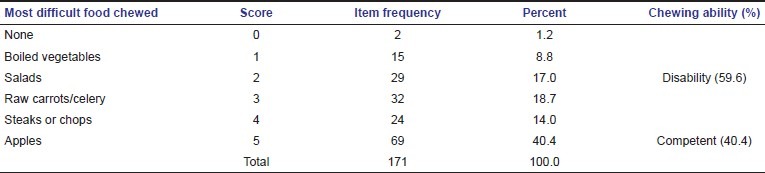
Table 3.
Scores of the oral health impact profile questionnaire according to its domains and total scores
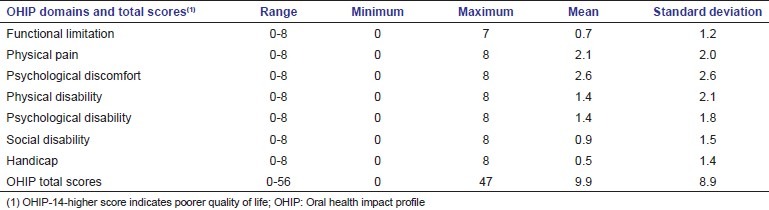
Table 4.
The impact of the index of chewing ability classified into two categories, chewing competence and chewing disability, over the quality of life measured by the oral health impact profile (OHIP-14) questionnaire
The analysis also showed a negative correlation between the number of natural teeth in mouth and the total scores of the OHIP-14 (Spearman's rho correlation coefficient-0.26, P = 0.001, 2-tailed), and this is interpreted as lower number of natural teeth, higher the scores of OHIP-14 or poorer QoL. These results can be viewed in the scatter-dot distribution graph [Figure 2]. The number of natural teeth also decrease with the increase of the age (Spearman's rho correlation coefficient -0.7, P < 0.001, 2-tailed) and as expected, low number of natural teeth was also associated with chew disability (ICA: chew's ability vs. disability) (Mann-Whitney U-Test, P < 0.001). Consequently, age in this sample, over than 40 years, was also associated with chew disability (Pearson Chi-Square P < 0.001) and poorer QoL (Mann-Whitney U test P = 0.01).
Figure 2.
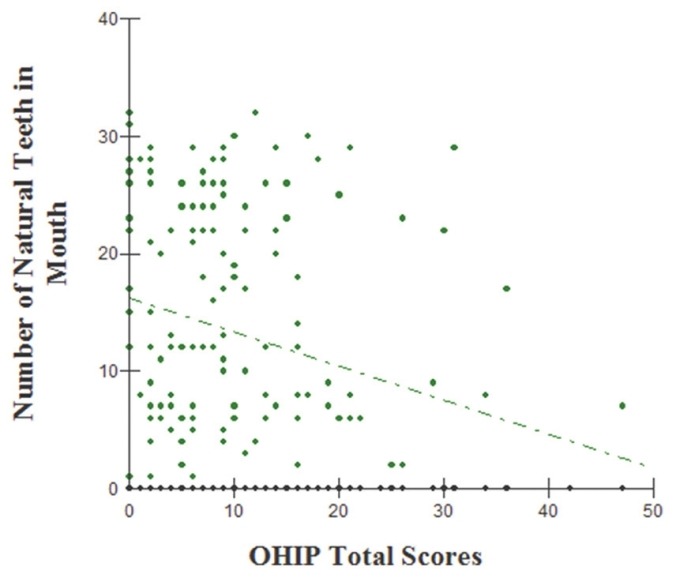
Scatter-dot graph showing that the negative correlation between the number of natural teeth in mouth and the scores of OHIP-14 (Spearman's rho correlation coefficient -0.26, P = 0.001, 2-tailed)
Discussion
Brazil has a long and sad history about poor quality of oral health, which renders internally the title of “edentates’ country,” besides the good technical and educational quality and an elevate number of dental schools (around 200). Brazil has actually around 216.000 dentists in activity, but it does not seem to ameliorate the oral conditions of the Brazilians. Worse, no news about serious federal preventive dental policy to change this scenario and as we observed in this study, patients as young as 40 years, still suffer with loss of teeth with consequent chew's disability and impairment of QoL, similar to what was found by Silva et al.[10] A study conducted in Taiwan by Hsu et al.,[7] observed as well that the increase of age also increases the number of tooth loss. That study concluded that the number of healthy remaining teeth, including natural teeth and fixed prostheses are key factors in chewing ability.
Besides this study has not an epidemiological design, our sample of patients showed a very concerning situation about losing teeth and its impact over chew ability and QoL, mainly if we compare these losses of natural teeth with those of the Swedish population which showed at the age of 70 years old an average of 20.7 natural teeth.[11] We also must take into consideration that the present study included, with no exception, low-income families and this highlight also the socioeconomic influence over oral health conditions for Brazilians. To our experience[12] is very common allegation for the patient to ask for tooth extraction since they could not afford for endodontic and prosthesis.
According to Preshaw et al.,[13] teeth are extracted as a consequence of oral disease, the interaction between the patient and dentist, the dentist's ability to provide care that will sustain a tooth in function, and the patient's preferences. The patient's decisions are likely to be influenced by variables such as the strategic location of the tooth, the importance they place on retaining teeth, their ability (and willingness) to pay for the necessary care that is required if a tooth can be saved, their willingness to undergo treatment, and the availability of specialist cares to resolve complex issues.
Chew's ability may also have influence in dietary preferences and this may contribute for the patients’ nutritional status, however, this is a matter of discussion since masticatory ability and efficiency are not the only factors affecting nutrition.[14,15]
Other studies have confirmed the association between prosthetic status/tooth loss and impair of the QoL measured by different instruments.[4,16,17] Related to the oral health status in older patients, Wφstmann et al.,[15] did not observe a significant improvement in QoL (OHIP-G14) after improvement of their oral condition, and that may indicate that QoL may be permanently worsened after losing teeth. Furthermore, Preshaw et al.,[13] declared that the use of removable partial dentures increase plaque and gingivitis and increases the risk for caries, particularly root caries. However, Nickenig et al.,[6] observed that, for partially edentulous patients, implant therapy had a positive effect on the OHRQoL (OHIP-G21), nevertheless, the scores of QoL never reach the quality of those fully dentate. The most frequently reported problems for that group of patients (partially edentulous) were difficulty in chewing, psychological disappointment related to dental problems and dissatisfaction with appearance due to problems with teeth, mouth, or dentures. As we observed within the subscales or domains of the OHIP-14, psychological discomfort and psychological disability are increased in patients with chew's disability as well as, functional limitation, physical pain and disability (impact in five of seven domains of OHIP-14).
It is difficult to explain why the OHIP-14 domain “social disability” was not affected in chew’ disability since the psychological status was. It is possible to speculate that two main reasons may be implicated. The first is the cultural aspect, since Brazilians are described as very sociable people and “his dental problems are quite similar as of his friends, relatives and coworkers” so, no reason to do not socialize. The second is related to complex sample itself, which brings a large age range and a different number of teeth loss, teeth positions, prosthesis condition and presence.
In conclusion, this study observed that the chew's disability measured by the ICA produce a significant and negative impact over OHRQoL (OHIP-14) and both poor QoL and chew's disabilities are related with the decrease of the number of natural teeth, therefore, oral health may influence the QoL.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
References
- 1.Study protocol for the World Health Organization project to develop a quality of life assessment instrument (WHOQOL) Qual Life Res. 1993;2:153–9. [PubMed] [Google Scholar]
- 2.Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 3.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 4.Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual Life Outcomes. 2010;8:126. doi: 10.1186/1477-7525-8-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, Van 'T Hof MA, Witter DJ, Kalk W, et al. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res. 2000;79:1519–24. doi: 10.1177/00220345000790071501. [DOI] [PubMed] [Google Scholar]
- 6.Nickenig HJ, Wichmann M, Andreas SK, Eitner S. Oral health-related quality of life in partially edentulous patients: Assessments before and after implant therapy. J Craniomaxillofac Surg. 2008;36:477–80. doi: 10.1016/j.jcms.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Hsu KJ, Yen YY, Lan SJ, Wu YM, Chen CM, Lee HE. Relationship between remaining teeth and self-rated chewing ability among population aged 45 years or older in Kaohsiung City, Taiwan. Kaohsiung J Med Sci. 2011;27:457–65. doi: 10.1016/j.kjms.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Leake JL. An index of chewing ability. J Public Health Dent. 1990;50:262–7. doi: 10.1111/j.1752-7325.1990.tb02133.x. [DOI] [PubMed] [Google Scholar]
- 9.Almeida A, Loureiro CA, Araujo VE. A transcultural study of heath values using the short-form of OHIP (oral health impact profile). Part I: Cultural and liguistic adaptation [Um estudo transcultural de valores de saúde utilizando o instrumento OHIP-14 (Oral Health Impact Profile) na forma simplificada-Parte I: Adaptação cultural e lingüística] UFES Rev Odontol. 2004;6:6–15. [Google Scholar]
- 10.Silva ME, Villaça EL, Magalhães CS, Ferreira EF. Impact of tooth loss in quality of life. Cien Saude Colet. 2010;15:841–50. doi: 10.1590/s1413-81232010000300027. [DOI] [PubMed] [Google Scholar]
- 11.Hugoson A, Koch G, Göthberg C, Helkimo AN, Lundin SA, Norderyd O, et al. Oral health of individuals aged 3-80 years in Jönköping, Sweden during 30 years (1973-2003). II. Review of clinical and radiographic findings. Swed Dent J. 2005;29:139–55. [PubMed] [Google Scholar]
- 12.Bortoluzzi MC, Manfro R, De Déa BE, Dutra TC. Incidence of dry socket, alveolar infection, and postoperative pain following the extraction of erupted teeth. J Contemp Dent Pract. 2010;11:E033–40. [PubMed] [Google Scholar]
- 13.Preshaw PM, Walls AW, Jakubovics NS, Moynihan PJ, Jepson NJ, Loewy Z. Association of removable partial denture use with oral and systemic health. J Dent. 2011;39:711–9. doi: 10.1016/j.jdent.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 14.Kossioni A, Bellou O. Eating habits in older people in Greece: The role of age, dental status and chewing difficulties. Arch Gerontol Geriatr. 2011;52:197–201. doi: 10.1016/j.archger.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 15.Wöstmann B, Michel K, Brinkert B, Melchheier-Weskott A, Rehmann P, Balkenhol M. Influence of denture improvement on the nutritional status and quality of life of geriatric patients. J Dent. 2008;36:816–21. doi: 10.1016/j.jdent.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 16.John MT. Prosthetic status is related to quality of life. J Evid Based Dent Pract. 2006;6:222–3. doi: 10.1016/j.jebdp.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 17.Saintrain MV, de Souza EH. Impact of tooth loss on the quality of life. Gerodontology. 2012;29:e632–6. doi: 10.1111/j.1741-2358.2011.00535.x. [DOI] [PubMed] [Google Scholar]


