Abstract
Loss of interdental papilla predisposes to phonetic, functional, and esthetic problem. Surgical techniques are manifold, but are challenging and very unpredictable. The purpose of this case report is to present the use of platelet rich fibrin (PRF) in the reconstruction of papilla in the maxiallry anterior region of a forty year old woman who presented with loss of interdental papillae in 11, 12 and 11, 21 region. PRF was tucked in to the pouch created with a semilunar pedicle flap and the entire gingivopapillary unit was displaced coronally. Optimal fill was noted at 3 and 6 months postoperatively. Use of PRF may thus be the panacea for interdental papilla augmentation.
Keywords: Interdental papilla, periodontal plastic surgery, platelet rich fibrin
Introduction
Esthetic awareness has improved vastly in the last decade. The advent of periodontal plastic surgery has made it possible to address the common esthetic concern of receded gums. However, till date, the most challenging scenario lies in enhancement of lost interdental papillae in the maxillary anterior region. Loss of Interdental papilla (IDP) causes not only an esthetic and phonetic dilemma but also a functional impairment as it predispose to food accumulation.
The interdental papilla of the incisor region is usually pyramidal in shape. Factors which influence the presence or absence of interdental papilla are crestal alveolar bone height, dimensions of the interproximal space, soft tissue appearance (thick or thin biotype), minimal buccal plate thickness, type of contact area (triangular versus square), and the biologic width.[1] The papillary form and the corresponding interproximal embrasure share a special and intricate relationship. An ideal embrasure will house the entire papillae without impinging it with a pointed end extending to the top of the contact point, leaving no space in between the two, thus not favoring food entrapment or being esthetically displeasing. Interdental papillae behave differently than the facial gingival margin. The free gingival margin averaged 2-3 mm above underlying facial bone, whereas the tip of the papillae is about 4.5-5 mm above the interproximal bone.[2] Tarnow et al.,[3] proposed that the interdental papillae filled the space when the distance between the contact point and the crest of interdental bone is ≤ 5 mm. When the contact was 6 mm and 7 mm from bone, only 56% and 37% of the papillae could fill the space respectively.
Interdental area is the main site where dental caries and periodontitis can occur. The complex anatomy combined with the vascular supply allows for periodontal disease to progress rapidly and is the most common cause for appearance of black triangles. Nevertheless, it may also be absent in cases of naturally occurring diastema or can be encountered in teeth with tapered tooth form, where the papillae does not fill the space completely or in case of divergent roots, which places the contact point too coronally. Iatrogenically, surgical reflection of interproximal tissues in areas where the distance between the contact and interdental bone is ≥ 5 mm, also results in partial loss of interdental papillae. While the former can be corrected by shifting the contact point either restoratively or orthodontically, loss due to periodontal disease can be treated surgically.
Platelet rich fibrin (PRF) is a form of platelet gel; a matrix of autologous fibrin, which has scored over platelet rich plasma by virtue of its properties, easier preparation, and cost effectiveness. It promotes wound healing, wound sealing, and hemostasis. The platelet cytokines, platelet-derived growth factor (PDGF), transforming growth factor beta (TGF-β), and insulin-like growth factor-1 (IGF-1) are gradually released as the fibrin matrix is resorbed, aiding the process of healing. The presence of leukocytes and cytokines in the fibrin network can play a significant role in the self-regulation of inflammatory and infectious phenomena.[4] It can be used as a membrane or in conjunction with a bone graft, and is shown to promote bone density. It has been extensively used in hard and soft tissue augmentation, but not tried for augmenting interdental papilla. In this case report, we describe a surgical technique using PRF combined with advanced papillary flap for total papilla reconstruction in the maxillary anterior region.
Case Report
A 40 year old healthy, nonsmoking female presented to the department of periodontics, Thai Moogambigai Dental College and Hospital, Mogappair, Chennai, in November 2011. Her chief complaint was unaesthetic appearance of her gums in the upper front teeth region. Clinical examination revealed, esthetically displeasing black triangles between 11, 12 and 11, 21 [Figure 1]. No facial recession was evident on 11, 12, and 21. The soft tissues appeared to be healthy without overt inflammation. Preoperative examination included papilla contour measurements based on modification of Papilla Index Score (PIS) described by Jemt.[5] Papilla was absent with no curvature of soft tissue contour, which was observed in between 11, 12 and 11, 21, and therefore was assigned a PIS score of 0. The distance between the contact point and the crest of alveolar bone was determined under local anesthesia with 2% lignocaine hydrochloride. A William's periodontal probe was used and a distance of 9 mm between 11 and 21 and 9.5 mm between 11 and 12 was recorded.
Figure 1.

Preoperative view showing loss of interdental papillae in 11, 12 and 11, 21 region
Platelet Rich Fibrin Preparation
The preparation of PRF was carried out before the start of the surgery as per the protocol developed by Choukron et al.[6] en milliliter of intravenous blood (antecubital site) was collected in sterile 10 ml tubes without the addition of an anticoagulant and centrifuged at 3000 revolutions (≈400 × g) per minute for 10 minutes. PRF settles down between the platelet poor plasma (PPP) at the top and the red blood cells (RBC) at the bottom of the tube [Figure 2].
Figure 2.
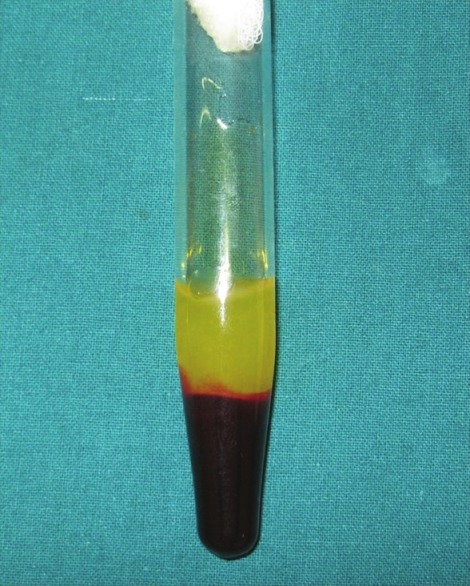
Platelet rich fibrin at the center with platelet poor plasma at the top and red blood cells at the bottom of the test tube
Surgical Procedure
Intraoral antisepsis was performed by rinsing with 0.12% chlorhexidine digluconate for 30 seconds. Adequate local anesthesia was achieved with 2% lignocaine hydrochloride (HCL). A split thickness semilunar incision was given about 1 mm coronal to the mucogingival junction in the interdental region of 11, 12 and 11, 21. Through the semilunar incision toward the interdental papillae, the split thickness flap was continued to create a pouch in the interdental area. A curette was used around the necks of 11, 12 and 21 to free the tissue attachment from the root surface, facilitating the displacement of gingivopapillary unit coronally.
The prepared PRF was removed using sterile tweezers and trimmed with scissors and transferred on to sterile gauze. A thick fibrin membrane was obtained by squeezing the serum out of the PRF clot. This membrane was eased in to the pouch and pushed coronally, enabling to fill the bulk of the interdental papillae [Figure 3]. The incisions were secured using absorbable sutures [Figure 4]. The surgical area was protected with a periodontal dressing. Analgesics (ibuprofen 400 mg twice daily for 3 days) along with chlorhexidine digluconate (0.12%) rinse twice daily were prescribed for 10 days. Postoperative healing was uneventful with minimal pain. Review of the patient on 10th day revealed partial fill of the interdental region, with the conversion of PIS from 1 to 3 – papilla fills the interproximal embrasure to the same level as in the proximal teeth and is in complete harmony with the adjacent papillae.
Figure 3.

Platelet rich fibrin being tucked in to the pouch created
Figure 4.

Incisions closed with absorbable sutures
Discussion
An assortment of surgical procedures has been tried out in papilla reconstruction. Shapiro et al.[7] advocated use of repeated curettage to stimulate the regrowth of interdental papillae in necrotizing ulcerative gingivitis. The roll technique[8] and the use of pedicle graft with coronal displacement of the gingivopapillary unit and subepithelial connective tissue grafting has been presented.[9] Interpositional subepithelial connective tissue grafting and use of buccal and palatal split thickness have been tried out.[10] Interdental papilla augmentation along with reconstruction of interdental bone to create appropriate support for gingival papilla has been reported.[11]
However, even with these different surgical techniques with different flap designs, results are elusive, not predictable and long-term stability are lacking. A major drawback associated with all these techniques is the lack of sufficient blood supply. Any graft placed in this small anatomic area will have to thrive in an unfavorable environment, walled on both sides by the nonvascularized tooth surfaces. Thus many authors have advocated the use of pedicle/advanced flap for better results than free grafts.
The case presented here with the use of PRF and pedicle flap offers a reliable solution as PRF membrane has both mechanical adhesive properties and biologic functions like fibrin glue; it maintains the flap in stable position, enhances neoangiogenesis, reduces the necrosis and shrinkage of the flap and stabilization of the gingival flap in the highest covering position.[12] The PRF is easy to procure, not expensive and can be prepared in few minutes. PRF provides ideal healing properties. This fibrin matrix inclusive of its platelets, leucocytes, and cytokines allow remodeling of interdental papilla to occur. It has been found PRF organized as a dense fibrin scaffold with a specific release of growth factors (TGF-1β, PDGF-AB, and vascular endothelial growth factor (VEGF) and glycoproteins (thrombospondin -1) during ≥ 7 days,[13] is critical for the “take” of the grafted PRF membrane.
Case selection also plays a pivotal role in the success of the procedure. No improper root angulation or disproportional crown size was present in our case, but the interdental bone loss was high thus making this not a very ideal, but still optimal fill of the interdental space was noted. Additionally, harvesting PRF just prior to surgery, advocating an atraumatic procedure, with primary closure is likely to contribute to the overall success. Another advantage of this procedure is that a second site for graft harvest is avoided, vastly improving the patient compliance and reducing the post operative morbidity.
In conclusion, the case report shows a novel surgical procedure using PRF to regenerate a lost interdental papilla. The reconstructed papilla in the new position was stable when reviewed at 3 and 6 months postoperatively [Figure 5]. However, studies with a longer study period are required to determine the success rate and the predictability of this procedure. Moreover, of all methods, genuine and stable papillary reconstruction results only when the regeneration of interdental bone occurs, therefore, PRF combined with bone graft may improve the clinical success.
Figure 5.

Postoperative view after 6 months
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
References
- 1.Zetu L, Wang HL. Management of inter-dental/inter-implant papilla. J Clin Periodontol. 2005;32:831–9. doi: 10.1111/j.1600-051X.2005.00748.x. [DOI] [PubMed] [Google Scholar]
- 2.Spear Frank M, Joseph P. Cooney Restorative Interrelationships. In: Newman, Takei, Klokkevold, Carranza, editors. Carranza's Clinical Periodontology. 10th ed. 2006. p. 1059. [Google Scholar]
- 3.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–6. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 4.Simonpieri A, Del Corso M, Sammartino G, Dohan Ehrenfest DM. The relevance of Choukroun's platelet-rich fibrin and metronidazole during complex maxillary rehabilitations using bone allograft. Part I: A new grafting protocol. Implant Dent. 2009;18:102–11. doi: 10.1097/ID.0b013e318198cf00. [DOI] [PubMed] [Google Scholar]
- 5.Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997;17:326–33. [PubMed] [Google Scholar]
- 6.Choukroun J, Adda F, Schoeffler C, Vervelle A. A opportunite’ in parp-implantology: The PRF (in French) Implantodontie. 2000;42:55–62. [Google Scholar]
- 7.Shapiro A. Regeneration of interdental papillae using periodic curettage. Int J Periodontics Restorative Dent. 1985;5:26–33. [PubMed] [Google Scholar]
- 8.Beagle JR. Surgical reconstruction of the interdental papilla: Case report. Int J Periodontics Restorative Dent. 1992;12:145–51. [PubMed] [Google Scholar]
- 9.Han TJ, Takei HH. Progress in gingival papilla reconstruction. Periodontol 2000. 1996;11:65–8. doi: 10.1111/j.1600-0757.1996.tb00184.x. [DOI] [PubMed] [Google Scholar]
- 10.Azzi R, Etienne D, Carranza F. Surgical reconstruction of the interdental papilla. Int J Periodontics Restorative Dent. 1998;18:466–73. [PubMed] [Google Scholar]
- 11.Azzi R, Takei HH, Etienne D, Carranza FA. Root coverage and papilla reconstruction using autogenous osseous and connective tissue grafts. Int J Periodontics Restorative Dent. 2001;21:141–7. [PubMed] [Google Scholar]
- 12.Del Corso M, Sammartino G, Dohan Ehrenfest DM. Re: Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6-month study. J Periodontol. 2009;80:1697–9. doi: 10.1902/jop.2009.090253. [DOI] [PubMed] [Google Scholar]
- 13.Dohan Ehrenfest DM, de Peppo GM, Doglioli P, Sammartino G. Slow release of growth factors and thrombospondin-1 in Choukroun's platelet-rich fibrin: A gold standard to achieve for all surgical platelet concentrates technologies. Growth Factors. 2009;27:63–9. doi: 10.1080/08977190802636713. [DOI] [PubMed] [Google Scholar]


